Abstract
Sinusitis is a common condition that can lead to various neurological complications due to the spread of infection to the intracranial and orbital regions. Fortunately, the availability of antibiotics has significantly improved the prognosis of sinusitis-associated intracranial complications. As a result, the overall incidence of neurological complications arising from sinusitis remains low. We present a rare case of a 13-year-old male who developed epidural empyema and orbital cellulitis as a complication of acute sinusitis. The patient initially exhibited signs and symptoms of orbital cellulitis, including eyelid swelling, erythema, and pain. Subsequently, the patient's condition worsened, with the development of fever and an intensifying headache. Imaging revealed an epidural empyema, necessitating urgent medical intervention. This case highlights the importance of early recognition and prompt management of sinusitis-related intracranial and orbital complications to prevent potentially life-threatening outcomes
Keywords: Orbital cellulitis, Periorbital cellulitis, Epidural empyema, Sinusitis, Maxillary sinusitis, Orbital abscess
Introduction
Sinusitis is a common condition that can lead to various neurological complications by spreading infection to the intracranial and orbital regions, such as epidural empyema and orbital cellulitis. Antibiotic and surgical interventions have significantly reduced the risk of complications associated with sinusitis. Imaging plays a crucial role in the early detection of these complications. We report a rare case of a 13-year-old male who presented to our radiology department from the Emergency Room with orbital cellulitis. A noncontrast head and brain computed tomography (NCCT) scan and a noncontrast head and brain magnetic resonance imaging (NCMRI) scan were performed, revealing acute sinusitis and epidural empyema. The patient underwent antibiotic therapy and surgical intervention, leading to full recovery without permanent sequelae.
Case report
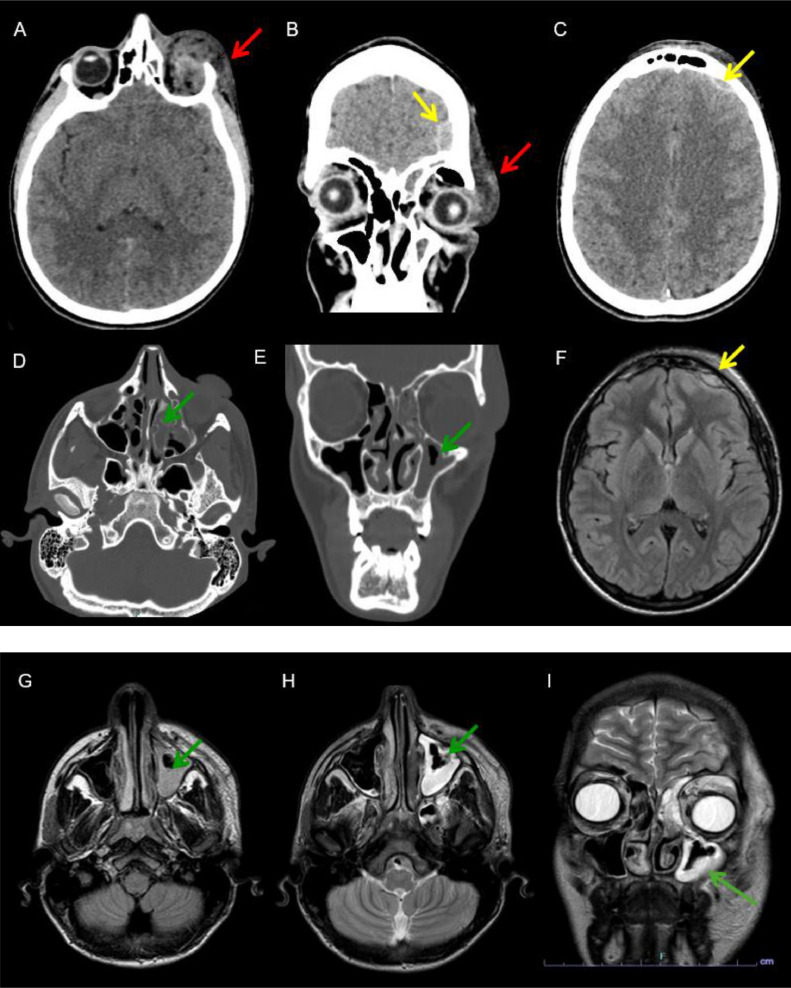
A 14-year-old male presented to our emergency department with severe left eye pain, accompanied by eyelid edema, erythema, and localized warmth. His medical history included recent episodes of severe nasal congestion and headaches. On initial evaluation, the patient was febrile (39.5°C), and laboratory findings showed elevated C-reactive protein (CRP) levels (306.9 mg/L), leukocytosis (15.30 × 10^3/µL), and neutrophilia (13.16 × 10^3/µL). An NCCT scan of the head revealed significant thickening and inhomogeneity of the soft tissues in the left orbital and periorbital regions, along with a noticeable air pocket along the lower margin of the orbital roof. There was near-complete inflammatory obliteration of the left maxillary sinus, as well as a small frontal extra-axial epidural empyema (Figs. 1A-E). Empirical antibiotic therapy was initiated. A subsequent NCMRI scan of the head confirmed left maxillary sinusitis with subtotal inflammatory obliteration of the left maxillary sinus, ipsilateral periorbital cellulitis, and extra-axial frontal epidural empyema (Figs. 1F-I). The patient underwent sinus surgery to drain the retained mucus in the paranasal sinuses. After symptom resolution and normalization of laboratory parameters, the patient was discharged.
Fig. 1.
NCCT (A-D): brain window (A-C) axial (A-C) and coronal (B) view; bone window (D-E) axial (D) and coronal view. NCMRI Fluid Attenuated Inversion Recovery sequence FLAIR axial view (F-G) and T2W images axial and coronal view (H-I). Extensive thickening and inhomogeneity of the soft tissues of the left orbital and periorbital region with a coarse air nucleus along the lower margin of the orbital roof (red arrow), subtotal phlogistic obliteration of the left maxillary sinus (green arrow) and the presence of a small frontal extra-axial epidural empyema (yellow arrow).
Discussion
Sinusitis is the inflammation of the paranasal sinuses, which can be either infectious or noninfectious. Infectious sinusitis can be caused by bacteria, fungi, or viruses. Acute sinusitis is characterized by an infection lasting less than 4 weeks, while subacute sinusitis involves symptoms persisting for 4–12 weeks, and chronic sinusitis refers to infection lasting over 12 weeks. Sinusitis can lead to various neurological complications due to disease spread to the intracranial and orbital regions. Intracranial complications include suppurative conditions such as brain abscess, epidural abscess, and subdural empyema, as well as nonsuppurative conditions like meningitis and cerebral venous sinus thrombosis [3]. These complications often occur simultaneously, as seen in our case [4].
The spread of infection from the paranasal sinuses occurs through 2 primary pathways. The first is retrograde spread via valveless diploic veins, driven by thrombus propagation or the release of septic emboli. These veins drain the mucosa of the paranasal sinuses and communicate with the dural venous sinuses. The second mechanism involves direct extension through bone, potentially due to congenital or traumatic defects, sinus wall erosion or dehiscence, or existing foramina [6]. In paediatric patients, sinusitis most commonly affects the maxillary and anterior ethmoidal sinuses [5], as observed in our case (Fig. 1).
Epidural empyema is a rare but serious intracranial complication characterized by the accumulation of purulent material between the dura mater and the skull. It is often secondary to sinusitis and caused by bacteria from the upper respiratory tract. Symptoms can initially mimic those of the primary infection but may progress to altered consciousness and neurological deficits [1].
Orbital cellulitis is a severe infection of the soft tissues surrounding the eye, typically secondary to sinusitis or trauma, and most commonly caused by bacterial pathogens. Symptoms include proptosis, ophthalmoplegia, pain, and systemic manifestations like fever [2]. According to Chandler's staging system [7], orbital cellulitis can be classified into 5 stages:
-
1.
Preseptal cellulitis: Inflammation confined within the orbital septum.
-
2.
Postseptal cellulitis: Inflammation extending into orbital tissues without abscess formation.
-
3.
Subperiosteal abscess: Abscess formation beneath the periosteum of the orbit.
-
4.
Orbital abscess: Abscess formation within the orbit.
-
5.
Cavernous sinus thrombosis.
Progression through these stages is not inevitable.
The causes of orbital cellulitis include both endogenous and exogenous factors. Endogenous factors, such as the absence of valves between the orbit and sinuses, allow retrograde spread of infections. Conditions like diabetes mellitus and immunosuppression also increase the risk. Exogenous causes include foreign bodies, trauma, eye surgeries, dacryocystitis, infected tumours, and mucormycosis. Orbital cellulitis is most commonly seen in children aged 1–7 years, as their immune systems are still developing [8].
Due to the potential for severe vision-threatening and life-threatening complications, prompt intravenous antibiotic administration is crucial in all cases of orbital cellulitis. Empiric antibiotic therapy typically targets common causative organisms, primarily gram-positive bacteria such as Staphylococcus and Streptococcus. However, cultures from the conjunctiva, nose, or throat may not reflect the pathogens present in abscesses. Age influences the bacteriology and treatment response; younger children usually present with simpler infections that respond to treatment, while older children and adults may experience more complex, polymicrobial infections that are harder to manage both medically and surgically, as seen in our case [9].
In most cases, epidural empyema requires both antibiotic therapy and surgery to prevent complications. However, in our case, due to the small size of the empyema, antibiotic therapy alone was sufficient.
In conclusion, early recognition and treatment of sinus-related intracranial and orbital complications are essential to prevent potentially life-threatening outcomes. Intracranial complications should be suspected in paediatric patients with sinusitis and orbital cellulitis. Accurate diagnosis is crucial for effective management and to prevent complications due to delayed treatment.
Patient consent
Written informed consent for publication of their clinical details and clinical images was obtained from the patients.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Sellick JA., Jr. Epidural abscess and subdural empyema. J Am Osteopath Assoc. 1989;89(6):806–810. [PubMed] [Google Scholar]
- 2.Harris GJ. Periorbital cellulitis: an analysis of its past, present, and future. J Pediatr Ophthalmol Strabismus. 2014;51(2):78–86. [Google Scholar]
- 3.Ziegler A, Patadia M, Stankiewicz J. Neurological complications of acute and chronic sinusitis. Curr Neurol Neurosci Rep. 2018;18(2):5. doi: 10.1007/s11910-018-0816-8. [DOI] [PubMed] [Google Scholar]
- 4.Tan R, Spector S. Pediatric sinusitis. Curr Allergy Asthma Rep. 2007;7(6):421–426. doi: 10.1007/s11882-007-0064-5. [DOI] [PubMed] [Google Scholar]
- 5.Lee S, Fernandez J, Mirjalili SA, Kirkpatrick J. Pediatric paranasal sinuses: development, growth, pathology, & functional endoscopic sinus surgery. Clin Anat. 2022;35(6):745–761. doi: 10.1002/ca.23888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stankiewicz JA, Newell DJ, Park AH. Complications of inflammatory diseases of the sinuses. Otolaryngol Clin North Am. 1993;26(4):639–655. [PubMed] [Google Scholar]
- 7.Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80(9):1414–1428. doi: 10.1288/00005537-197009000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Gupta S, Sharma S. orbital cellulitis: defining multidisciplinary approach as the need of the hour. Indian J Otolaryngol Head Neck Surg. 2019;71(4):464–469. doi: 10.1007/s12070-019-01632-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hornblass A, Herschorn BJ, Stern K, Grimes C. Orbital abscess. Surv Ophthalmol. 1984;29:169–178. doi: 10.1016/0039-6257(84)90202-9. [DOI] [PubMed] [Google Scholar]