Abstract
A Temporomandibular joint (TMJ) effusion is an accumulation of fluid components in the articular space. It represents an inflammatory process which can be associated with trauma, arthritis or internal derangement of TMJ such as disc displacement. In this study, we present the case of a 48-year-old patient presented with TMJ effusion, diagnosed as resulting from disc displacement without reduction and osteoarthrosis. The case report details the diagnostic and therapeutic strategies employed.
Keywords: Temporomandibular joint, Joint effusion, Magnetic resonance imaging, Pain, Disc displacement, Corticoids
Introduction
Temporomandibular joint (TMJ) effusion is defined as an accumulation of fluid components specifically synovial fluid in the articular space. It represents an inflammatory process which can be associated with trauma, arthritis or internal derangement of TMJ. Radiologically it is identified by hyperintense signal on a T2 weighted magnetic resonance (MRI) images. Clinically TMJ effusion causes moderate to severe TMJ pain making patients seek treatment emergently [1,2]. Treatment included medical management based on drugs therapy (nonsteroidal anti-inflammatory agents, corticoids) and occlusal splints. If these previous conservative treatments fail, a surgical intervention may be indicated [2]. The aim of this article was to describe the diagnostic and therapeutic approaches to TMJ effusion secondary to a disc displacement without reduction (DDWoR) and TMJ osteoarthrosis in a 48-year old male Tunisian patient.
Case report
A 48-year old Tunisian man was referred to the department of functional exploration, pain and orofacial dysfunction of the dental clinic of Monastir with a severe pain in the right hemiface evolving over 2 months.
A history of spontaneous pain in the right preauricular region was reported. Patient had no history of trauma or infection of the TMJ. Pain was spontaneous, continuous, present at rest with a score on visual analogic scale (VAS) evaluated at 4.2/10, and it got worse with activity and when lying down (VAS= 8.2/10) or at night keeping the patient awake. As pain was experienced first of all as an otalgia, an otorhinolaryngological exam by a specialist was carried out and it revealed no pathology. The patient was referred to a maxillo-facial surgeon. A prefabricated bimaxillary flexible splint and an anti-inflammatory non steroid drug were prescribed for 4 days. As there was no improvement of symptoms, the patient was referred to the department of functional exploration, pain and orofacial dysfunction of the dental clinic of Monastir.
Clinical examination of the orofacial region revealed an acute pain in the right preauricular region with TMJ lateral palpation, intra-auricular palpation, during motion and during maximum assisted mouth opening. A pain at the right masseter was also detected at palpation. The range of motion was restricted by pain with a positive endfeel. The maximum assisted mouth opening was equal to 40 mm causing a severe pain especially in the right masseter muscle.
The intraoral examination showed nothing abnormal except a superficial decay on the mesial side of the second upper left molar which could not explain these severe continuous pains. In fact, all clinical tests (cold test, percussion) were normal.
A conventional tomography in open and closed mouth positions was performed. It depicted a narrowing of the articular space of the right TMJ with a slightly restricted condylar transitional motion (Fig. 1). Degenerative bone alterations in the condylar right head were also suspected. Based on clinical data (spontaneous, continuous, present at rest and aggravated by function, causing insomnia), the inflammatory origin of pain was confirmed and a TMJ effusion was suspected. A magnetic resonance imaging (MRI) in open and closed mouth positions was performed to evaluate articular surfaces, disc morphology and position and to evaluate the synovial fluid.
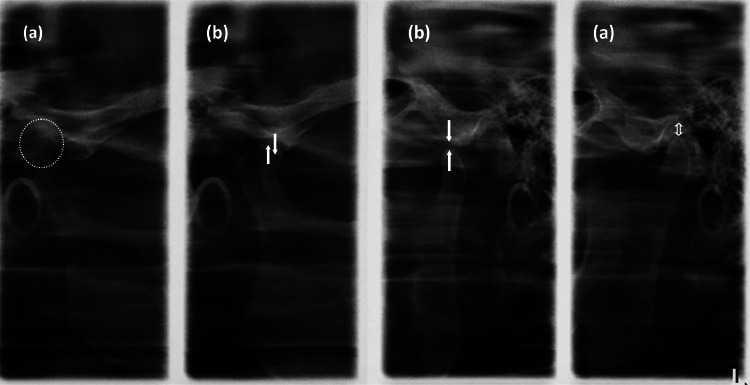
Fig. 1.
A conventional tomography in open and closed mouth positions showing a narrowing of the articular space of the right TMJ with a slightly restricted condylar transional motion.(a: closed mouth; b: open mouth).
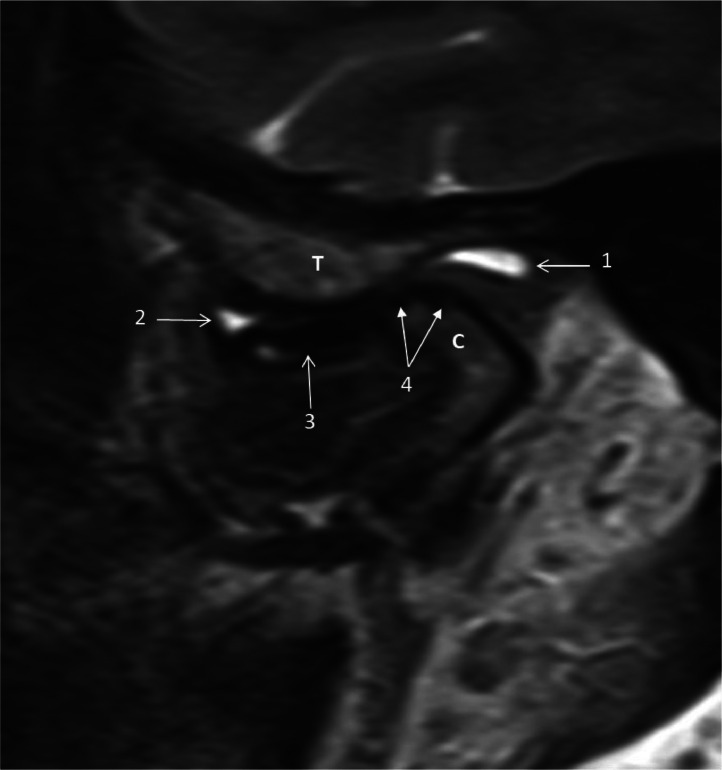
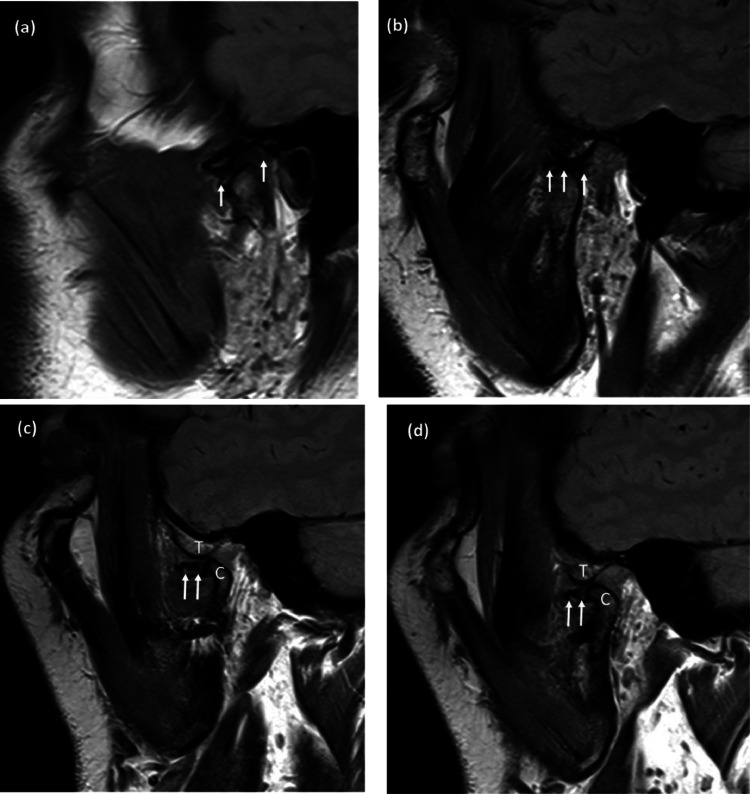
T-2 weighted MRI views showed a high hyperintense signal in the anterior and posterior compartments of the upper articular space of the right TMJ with an anterior disc displacement (ADD) in closed mouth position (Fig. 2). This signal was more abundant in the posterior area. This image corresponded to TMJ effusion. T-1 weighted MRI views showed an ADD in open mouth position (Fig. 3). Diagnosis of DDWoR with TMJ effusion in the right TMJ was retained. For the left TMJ, clinical and radiological examination revealed no patholgy (Fig. 3).
Fig. 2.
T-2 weighted MRI images of the right TMJ in closed mouth position showing a high hyperintense signal in the anterior and posterior compartments of the upper articular space, erosion of condylar head and anterior disc displacement (1;2: joint effusion, 3: articular disc, 4: bone erosion, C: mandibular condyle, T: temporal tubercle).
Fig. 3.
T-1 weighted MRI images of the right and left TMJ: (a, b ): T-1 weighted MRI images of the left TMJ in closed and open mouth positions showing a normal disc position. (a: closed mouth position, b: open mouth position); (c, d ): T-1 weighted MRI images of the right TMJ in open mouth position showing an anterior disc displacement.
A long term corticotherapy starting by a loading dose of 1mg / kg/ day for 10 days was prescribed. Then, a gradual reduction in the dosage was undertaken. A muscle relaxant drug was also indicated for 1 week.
After the fifth day of muscle relaxant and corticoid intake VAS had regressed from 8.2 to 3.2/10 at rest and the patient became able to have a good night sleep. Eight days later VAS decreased to 1.4/10. On the twentieth day of corticoid treatment, the patient described a mechanical type of pain that was worsened with activity, alleviated by rest and accompanied by morning stiffness.
After pain regression, dental impressions and bite registration were taken and a rigid occlusal splint for articular decompression was made.
After 1 month of constant use of the occlusal splint, there was a complete improvement of all symptoms. The patient was regularly reviewed for the next six months.
Discussion
TMJ effusion seemed to be related to internal derangement of TMJ. In this case report, effusion was associated with DDWoR . This association had been reported by many authors. In fact, Manfredini et al., described an association of joint effusion with DDWoR but not with disc displacement with reduction (DDWR) supporting the results founded by Huh et al., showing that TMJ effusion was more frequent in joint with DDWoR [3,4]. However, the etiopathogenic process underlaying this association still unclear. Two hypotheses have been proposed. The first one was that the accumulation of fluid in the posterior joint compartment might induce a mechanical displacement of the joint disc toward a more anterior position. The second one was that the disc displacement might induce an inflammatory process which had led to TMJ effusion [3]. In this case report, the presence of degenerative bone alterations traduced the long-term evolution of the disease and lent support to the hypothesis that disc displacement had led to effusion and not the opposite.
This hypothesis seemed to be more plausible. In fact, internal derangement results in an abnormal mechanical stress leading to the deterioration and abrasion of articular cartilage and disc surfaces. As a result, there is releasing of pro-inflammatory cytokines including tumor necrosis factor TNF-α, nitric oxide, bradykinin, Interleukins (IL) (IL-6, IL-1, IL-8) and leukotriene B4. These inflammatory cytokines lead to further joint destruction, creating a painful inflammatory effusion around the joint [[5], [6], [7]]. This may explain the association between TMJ effusion and degenerative joint changes [1,8,9]. In the other hand, TMJ effusion results in an increased articular pressure that may activate or sensitize nociceptive afferent neurons within the joint creating an arthralgia [2,8]. Furthermore, Manfredini et al., found that the most reliable predictors of TMJ effusion were respectively pain with lateral and posterior TMJ palpation and during mandibular movements. They found that the presence of clinically diagnosed pain was highly predictive of the presence of TMJ effusion [10]. In fact, the prevalence of TMJ effusion in patient with TMJ pain ranged from 13% to 88% whereas prevalence rates in TMJ without pain ranged from 0% to 38.5% [2,[11], [12], [13]]. So, it can be concluded that patients without TMJ pain may also exhibit TMJ effusion, but it tends to be less frequent and less severe. Asymptomatic effusion may be associated with minor conditions that don't cause noticeable inflammation like DDWR. However, the authors' conclusions regarding the relationship between joint effusion and pain in patients with DDWR are confusing. While Pinto et al. found no association, it has been suggested that TMJ pain is linked to significant effusion [2,[11], [14]].
As there are no specific clinical symptoms for TMJ effusion, the diagnosis is based on the radiological findings. MRI is considered as the gold standard for the analysis of soft tissues and fluids in the TMJ complex. In fact, it has shown a perfect validity in the diagnosis of TMJ effusion [2].
In this case report, corticotherapy and articular decompression were effective to relieve the symptoms. In fact, articular decompression reduces intra-articular pressure thus it reduces pain. Corticoid was indicated to stop the inflammatory process after the failure of nonsteroidal anti-inflammatory agents. Surgical approaches such as arthrocentesis with corticoid injection may be considered in case of failure of conservative treatments. Furthermore, arbashahi et al., reported that there was a significant improvement in TMJ effusion and TMJ pain after intraarticular corticosteroid injection in children with symptomatic TMJ arthritis [15].
Conclusion
This case supported the fact that disc displacement causes TMJ effusion and not the converse. Clinically TMJ effusion caused an acute inflammatory pain in the TMJ area which seemed to have a highly predictive value in the diagnosis. Thus, MRI might be considered for patients in which the exact disc- condyle relationship needs to be evaluated or in case of failure of conservative treatments.
Patient consent
We declare that written, informed consent for the publication of this case has been obtained from the patient. The patient was fully informed about the nature of the publication, including any potential risks and benefits, and his consent was given voluntarily.
Footnotes
Competing Interests: The authors declare that they have no conflict of interest.
References
- 1.Ahmad M, Hollender L, Anderson Q, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 2009;107:844–860. doi: 10.1016/j.tripleo.2009.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khawaja S-N, Crow H, Mahmoud RFG, et al. Is there an association between temporomandibular joint effusion and arthralgia? J Oral Maxillofac Surg. 2017;75:268–275. doi: 10.1016/j.joms.2016.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manfredini D, Basso D, Arboretti R, et al. Association between magnetic resonance signs of temporomandibular joint effusion and disk displacement. OOOOE. 2009;107:266–271. doi: 10.1016/j.tripleo.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 4.Huh JK, Kim HG, Ko JY. Magnetic resonance imaging of temporomandibular joint synovial fluid collection and disk morphology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:665–671. doi: 10.1067/moe.2003.159. [DOI] [PubMed] [Google Scholar]
- 5.Emshoff R, Puffer P, Rudisch A, et al. Temporomandibular joint pain: relationship to internal derangement type, osteoarthrosis, and synovial fluid mediator level of tumor necrosis factor-alpha. Oral Surg Oral Med. Oral Pathol. Oral Radiol.Endod. 2000;90:442–449. doi: 10.1067/moe.2000.108801. [DOI] [PubMed] [Google Scholar]
- 6.Takahashi T, Kondoh T, Fukuda M, et al. Proinflammatory cytokines detectable in synovial fluids from patients with temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:35–141. doi: 10.1016/s1079-2104(98)90415-2. [DOI] [PubMed] [Google Scholar]
- 7.Suenaga S, Abeyama K, Hamasaki A, et al. Temporomandibular disorders: relationship between joint pain and effusion and nitric oxide concentration in the joint fluid. Dentomaxillofac Radiol. 2001;30:214–218. doi: 10.1038/sj.dmfr.4600610. [DOI] [PubMed] [Google Scholar]
- 8.Oliveira JX, Rosa JA, Dutra ME, et al. Assessing joint effusion and bone changes of the head of the mandible in MR images of symptomatic patients. Braz Oral Res. 2013;27:37–41. doi: 10.1590/s1806-83242012005000028. [DOI] [PubMed] [Google Scholar]
- 9.Adame CG, Monje F, Offnoz M, et al. Effusion in magnetic resonance imaging of the temporomandibular joint: a study of 123 joints. J Oral Maxillofac Surg. 1998;56:314–318. doi: 10.1016/s0278-2391(98)90106-9. [DOI] [PubMed] [Google Scholar]
- 10.Manfredini D, Tognini F, Zampa V, et al. Predictive value of clinical findings for temporomandibular joint effusion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:521–526. doi: 10.1016/s1079-2104(03)00475-x. [DOI] [PubMed] [Google Scholar]
- 11.Larheim TA, Westesson PL, Sano T. MR grading of temporomandibular joint fluid: association with disk displacement categories, condyle marrow abnormalities and pain. Int J Oral Maxillofac Surg. 2001;30:104–112. doi: 10.1054/ijom.2000.0017. [DOI] [PubMed] [Google Scholar]
- 12.Schellhas KP. Temporomandibular joint inflammation: comparison of MR fast scanning with T1- and T2-weighted imaging techniques. Am J Neuroradiol. 1989;10:584–589. doi: 10.2214/ajr.153.1.93. [DOI] [PubMed] [Google Scholar]
- 13.Murakami K, Nishida M, Bessho K, et al. MRI evidence of high signal intensity and temporomandibular arthralgia and relating pain. Does the high signal correlate to the pain? Br J Oral Maxillofac Surg. 1996;34:220–224. doi: 10.1016/s0266-4356(96)90273-9. [DOI] [PubMed] [Google Scholar]
- 14.Pinto GNDS, Grossmann E, Filho LI et al. Correlation between joint effusion and morphology of the articular disc within the temporomandibular joint as viewed in the sagittal plane in patients with chronic disc displacement with reduction: a retrospective analytical study from magnetic resonance imaging. J Cranio Pract 39:1–6. DOI:10.1080/08869634.2019.1582166. [DOI] [PubMed]
- 15.Arabshahi B, Dewitt E M, Cahill AM, et al. Utility of corticosteroid injection for temporomandibular arthritis in children with juvenile idiopathic arthritis. Arthritis Rheumatol. 2005;52:3563–3569. doi: 10.1002/art.21384. [DOI] [PubMed] [Google Scholar]