In 2007, Tuschl et al. reported the world's first case of partial trisomy of chromosome 1 and monosomy of chromosome 211). In 2017, Aleksiuniene et al. reported the second case of partial trisomy of chromosome 1 and monosomy of chromosome 212). According to a review by Dupont et al, partial trisomy of chromosome 1 has only been reported in approximately 100 cases3). Similarly, a few cases of partial monosomy of chromosome 21 have been published4), indicating that this disease, in which both chromosomes are present, is extremely rare. This case report describes the world's first case of scoliosis in a patient with trisomy 1 and monosomy 21 genetic mutations, who was surgically treated using a vertical expandable prosthetic titanium rib (VEPTR) and posterior correction and fusion.
The patient was referred to the clinic at the age of 8 years with the chief complaint of trunk deformity. During the initial surgery, the patient's weight and height were 16.5 kg and 89 cm, respectively, and the standard deviations were −7.07 and −3.98, respectively. Spinal deformities have been observed since birth. At of the age of 1 month, she experienced respiratory failure, decreased appetite, and laryngomalacia. At the age of 1 year, she underwent genetic testing by fluorescence in situ hybridization and was diagnosed with partial trisomy of chromosome 1 in the q41-qter region and partial monosomy of chromosome 21 in the q22.2-qter region. At the age of 3 years, she was diagnosed with left ureteral stricture and right vesicoureteral reflux following a urinary tract infection. She had a history of cleft palate and mental retardation. Radiographs taken during consultation showed a T6-L3 Cobb angle of 72° and kyphosis of 63° (Fig. 1). Other features included arachnodactyly of the fingers, clinodactyly of the first toe, and a broad nasal bridge.
Figure 1.
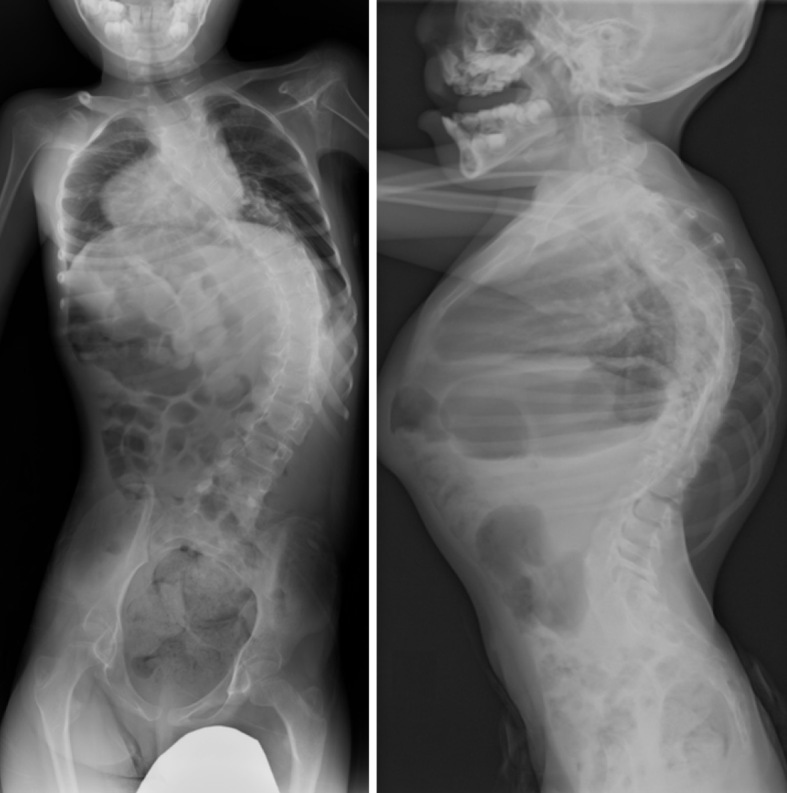
X-ray images upon referral to the hospital.
First, a Halo-gravity traction was applied for approximately 3 weeks5). Subsequently, a growth-friendly surgery using VEPTR was initiated (Fig. 2). Two cradles were placed between the left fifth rib and the iliac bone and between the left seventh rib and the third lumbar lamina. The patient was scheduled for lengthening once every 6 months, but 3 months after the initial surgery, redness and pain in the back wound and fever of 40°C were observed and diagnosed as surgical site infection. The initial surgical site infection occurred at the place where a hook was placed on the lamina at the third lumbar vertebra, and it extended across the entire implant. Since the patient was skinny, the prominent protrusion of the hook may have caused the ulcer and resulted in the surgical site infection. Because the patient had repeated deep wound infections, the patient underwent partial implant removal, vacuum-assisted closure therapy, and debridement several times. However, all the implants were required to be removed to control the infection. After confirming that the wound infection had completely healed, a posterior correction and fusion surgery with pedicle screws was performed from the Th2 to S1. The operative time was 3 hours and 26 minutes, and the intraoperative blood loss was 445 mL. Scoliosis and kyphosis were corrected to 54° and 85°, respectively (Fig. 3). The postoperative course was uneventful, and no recurrence of the deep wound infection was observed 2 years postoperatively without antibiotics.
Figure 2.

X-ray images after the first vertical expandable prosthetic titanium rib surgery at 8 years old.
Figure 3.
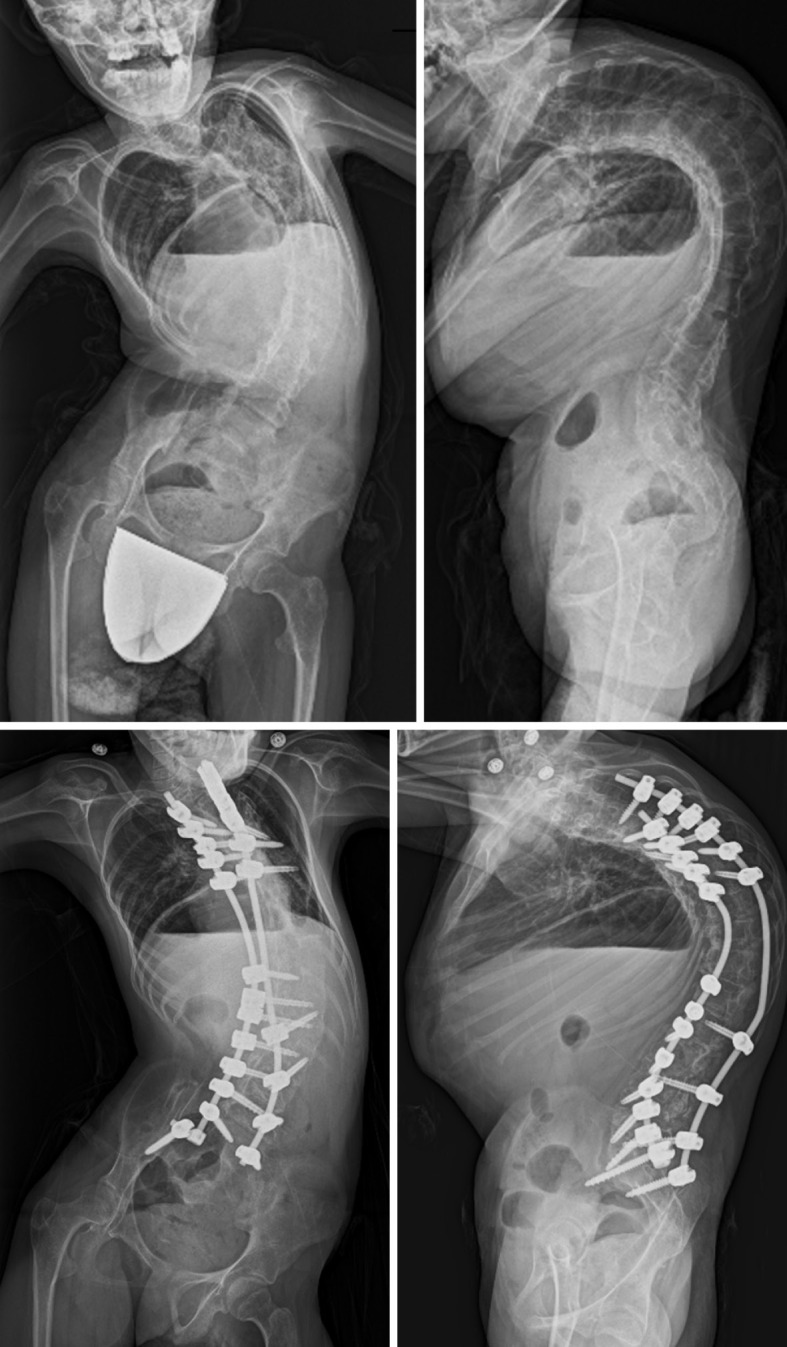
X-ray images before and after posterior spinal fixation at 17 years old.
The VEPTR is a curved metal rod attached to the ribs, spine, or pelvis. It helps straighten their spine and separate the ribs so that the lungs can grow and expand as they grow6). However, serious intraoperative and postoperative complications may occur. Intraoperative complications included rib fractures and atelectasis, whereas postoperative complications included implant prominence, junctional kyphosis, anchor dislocation, and surgical site infection.
Compared with the incidence of skin complications in a growing rod, which ranges from 7.1% to 33.3%7-11), the incidence in VEPTR surgery is between 17.2% and 84.0%11-16), suggesting a higher likelihood of skin complications in VEPTR surgery. The hook placed at the lamina will be prominent and may increase the risk of skin complications. The prominence of pedicle screws will be covered by the spinous processes, which may be a benefit of the growing rod from the standpoint of preventing surgical site infection.
However, it needs to be recognized that the indications may differ between VEPTR and growing rod, which may have caused the observed differences. VEPTR was used to correct the pelvic obliquity with the S hook, which cannot be done with the growing rod. Again, the reasons and surgical indications for each procedure are different. Thus, an analysis based on a large number of cases should be conducted to decide the appropriate indications for skinny patients as in the present case, to prevent surgical site infections.
Chromosome 1q43q44 deficiency is a chromosomal abnormality in this region17). 1q44 is located at the end of the long arm of chromosome 1, and its deletion results in a terminal (q44-qter) or intermediate (q43-q44) deletion. The 1q region contains several genes, and associated chromosomal disorders have a wide variety of symptoms. In general, the phenotypic effects of gene deletion and duplication occur at ratios of 2:1 to 3:1, with the loss being greater. The same result was obtained for chromosome 1. Many cases of 1q duplication syndrome have been reported in Japan, and patients commonly survive until middle or old age. However, in this case, the patient also had partial monosomy of chromosome 21, suggesting that the genetic mutations were diverse.
Comparing the clinical findings with those of two previous reports, the patient also had developmental delay and mental retardation as well (Table 1). In addition, abnormal findings have been observed in the extremities, such as arachnodactyly and syndactyly of the fingers and toes and clinodactyly and syndactyly of the toes. In two previous reports, other physical abnormalities, such as hypoplastic external ear, epilepsy, microcephaly, and macrocephaly were also reported. However, the patient in this study was the only case with scoliosis, and the condition was difficult to treat because of wound infection.
Table 1.
Previously Reported Cases of Partial Trisomy 1q and Partial Monosomy 21q.
| Clinical features | dup1q43q44 & del21q22.2q22.3(Beata et al.) | dup1q42.3qter & del21q22.3qter(Tuschl et al.) | dup1q41qter & del21q22.2qter(the present case) |
|---|---|---|---|
| Development delay | + | + | + |
| Intellectual disability | + | NA | + |
| Finger anomalies | Arachnodactyly | 5th finger clinodactyly | Arachnodactyly |
| Toe anomalies | NA | Syndactyly | 1st finger clinodactyly |
| Scoliosis | – | – | + |
| Kyphosis | – | – | + |
| Macrocephaly | + | – | – |
| Microcephaly | – | + | – |
| Broad nasal bridge | NA | + | + |
| Ear anomalies | Narrowing external auditory canal | Low set, hypoplastic ear | Normal |
| Joint hypermobility | + | NA | Normal |
| Seizures | + | + | – |
| Hypotonia | – | + | – |
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: None.
Author Contributions:
Conception and design: Yuta Fukase.
Acquisition of data: Yuta Fukase and Kota Watanabe.
Interpretation of data: Yuta Fukase and Kota Watanabe.
Study supervision: Kota Watanabe and Masaya Nakamura.
Drafting of the manuscript: Yuta Fukase and Kota Watanabe.
Critical revision of the manuscript: Kazuki Takeda, Toshiki Okubo, Satoshi Suzuki, Osahiko Tsuji, Narihito Nagoshi, Mitsuru Yagi and Masaya Nakamura.
The final version of the manuscript has been approved by all authors.
Ethical Approval: Ethical approval was waived due to the confidentiality and anonymity of this study.
Informed Consent: Informed consent for publication was obtained by parents of the patient in this study.
References
- 1.Tuschl K, Fritz B, Herle M, et al. Trisomy 1q42.3-qter and monosomy 21q22.3-qter associated with ear anomaly, facial dysmorphology, psychomotor retardation, and epilepsy: delineation of a new syndrome. Am J Med Genet A. 2007;143A(17):2065-9. [DOI] [PubMed] [Google Scholar]
- 2.Aleksiuniene B, Matuleviciute R, Matuleviciene A, et al. Opposite chromosome constitutions due to a familial translocation t(1;21) (q43;q22) in 2 cousins with development delay and congenital anomalies. Medicine. 2017;96(16):e6521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DuPont BR, Huff RW, Ridgway LE, et al. Prenatal diagnosis of partial trisomy 1q using fluorescent in situ hybridization. Am J Med Genet. 1994;50(1):21-7. [DOI] [PubMed] [Google Scholar]
- 4.Pelleri MC, Cicchini E, Locatelli C, et al. Systematic reanalysis of partial trisomy 21 cases with or without Down syndrome suggests a small region on 21q22.13 as critical to the phenotype. Hum Mol Genet. 2016;25(12):2525-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hwang CJ, Kim DG, Lee CS, et al. Preoperative halo traction for severe scoliosis. Spine. 2020;45(18):E1158-65. [DOI] [PubMed] [Google Scholar]
- 6.Parnell SE, Effmann EL, Song K, et al. Vertical expandable prosthetic titanium rib (VEPTR): a review of indications, normal radiographic appearance and complications. Pediatr Radiol. 2015;45(4):606-16. [DOI] [PubMed] [Google Scholar]
- 7.Bess S, Akbarnia BA, Thompson GH, et al. Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg Am. 2010;92(15):2533-43. [DOI] [PubMed] [Google Scholar]
- 8.Poe-Kochert C, Shannon C, Pawelek JB, et al. Final fusion after growing-rod treatment for early onset scoliosis: is it really final? J Bone Joint Surg Am. 2016;98(22):1913-7. [DOI] [PubMed] [Google Scholar]
- 9.Dumaine AM, Yu J, Poe-Kochert C, et al. Surgical site infections in early onset scoliosis: what are long-term outcomes in patients with traditional growing rods? Spine Deform. 2022;10(2):465-70. [DOI] [PubMed] [Google Scholar]
- 10.Matsumoto H, Fields MW, Roye BD, et al. Complications in the treatment of EOS: is there a difference between rib vs. spine-based proximal anchors? Spine Deform. 2021;9(1):247-53. [DOI] [PubMed] [Google Scholar]
- 11.Crews JD, Mina M, Johnson E, et al. Risk factors for surgical site infections following vertical expandable prosthetic titanium rib (VEPTR) surgery in children. Spine Deform. 2018;6(6):791-6. [DOI] [PubMed] [Google Scholar]
- 12.Murphy RF, Moisan A, Kelly DM, et al. Use of vertical expandable prosthetic titanium rib (VEPTR) in the treatment of congenital scoliosis without fused ribs. J Pediatr Orthop. 2016;36(4):329-35. [DOI] [PubMed] [Google Scholar]
- 13.Hasler CC, Mehrkens A, Hefti F. Efficacy and safety of VEPTR instrumentation for progressive spine deformities in young children without rib fusions. Eur Spine J. 2010;19(3):400-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waldhausen JH, Redding G, White K, et al. Complications in using the vertical expandable prosthetic titanium rib (VEPTR) in children. J Pediatr Surg. 2016;51(11):1747-50. [DOI] [PubMed] [Google Scholar]
- 15.Lucas G, Bollini G, Jouve JL, et al. Complications in pediatric spine surgery using the vertical expandable prosthetic titanium rib: the French experience. Spine. 2013;38(25): E1589-99. [DOI] [PubMed] [Google Scholar]
- 16.Garg S, Cyr M, St Hilaire T, et al. Variability of surgical site infection with VEPTR at eight centers: a retrospective cohort analysis. Spine Deform. 2016;4(1):59-64. [DOI] [PubMed] [Google Scholar]
- 17.Mohamed A, EI-Bassyouni H, EI-Gerzawy A, et al. Cytogenomic characterization of 1q43q44 deletion associated with 4q32.1q35.2 duplication and phenotype correlation. Mol Cytogenet. 2018;11:57. [DOI] [PMC free article] [PubMed] [Google Scholar]


