Abstract
Dermoid cysts originate from embryonic tissues trapped in the cranial fusion lines and typically manifest extra-axially. However, intradiploic dermoid cysts are rare among cranial tumors, and their rupture has been sparsely documented. We present a case showcasing a remarkable phenomenon—the spontaneous rupture of an intradiploic dermoid cyst into the subarachnoid space, displaying a distinct “volcano-like” appearance on CT and MRI scans. This case represents the first documented instance of spontaneous intracranial rupture of an intradiploic dermoid cyst into the subarachnoid space. Although uncommon, this rupture poses a risk of severe complications, such as chemical meningitis and vasospasm. This extraordinary presentation of an uncommon lesion at an atypical location may contribute to a better understanding of the potential mechanisms of rupture, thereby emphasizing the importance of recognition and exploration.
Keywords: Dermoid Cyst, Case Report, MRI, Subarachnoid Space, Embryonic Development
INTRODUCTION
Dermoid cysts are rare congenital intracranial tumors that result from the ectopic inclusion of embryonic ectoderm into the neural tube during early embryonic development (third to fifth weeks). These cystic lesions comprise of stratified squamous epithelium and skin adnexal structures, such as hair follicles, sebaceous glands, and sweat glands (1). Typically, they manifest in midline locations, particularly in the suprasellar and parasellar regions; however, their occurrence within intradiploic sites is exceptionally rare and sparsely documented (2).
The literature extensively documents the rupture of intracranial dermoid cysts, which can lead to symptoms of increased intracranial pressure due to mass effect. Patients may experience worsening headaches and seizures due to the dissemination of dermoid contents into the subarachnoid space and ventricles (3). This current report presents an unprecedented case of spontaneous rupture of an intradiploic cyst into the subarachnoid space. Notably, imaging revealed a distinct “volcano-like” appearance, a unique finding not previously documented in the literature. This extraordinary presentation of an uncommon lesion at such an atypical location may offer valuable insights into potential mechanisms underlying the rupture of these cysts.
CASE REPORT
A 50-year-old female presented with episodes of acute-onset headache and partial complex seizures followed by generalization over the past two months. On examination, vital signs were within normal limits. There was no reported history of weakness, cranial nerve deficits, fever, trauma, or surgery. The patient denied current medication use, smoking, alcohol abuse, or illicit drug consumption. Her past history was notable for a single episode of generalized tonic–clonic seizures at the age of 16 years, which had not undergone further evaluation.
Neurological examination revealed normal cognitive function and cranial nerve response. Motor and sensory examinations revealed no deficits, and deep tendon reflexes were within normal limits bilaterally. The gait and coordination were unremarkable. Laboratory investigations, including complete blood count, comprehensive metabolic panel, and inflammatory markers, were within normal ranges.
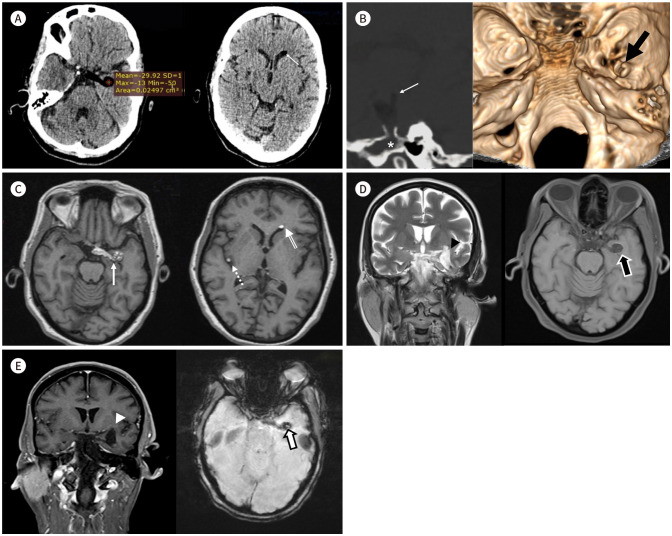
Non-contrast brain CT revealed a predominantly fat-density lesion (mean attenuation of -29.92 Hounsfield unit), measuring 4 × 1.5 × 1.2 cm in maximal transverse, craniocaudal, and antero-posterior orthogonal dimensions in the left suprasellar region, extending into the left temporal lobe (Fig. 1A, left). A fat–fluid level was observed in the frontal horn of the left lateral ventricle (Fig. 1A, right), with a fat droplet in the right Sylvian fissure. The bone window (Fig. 1B, left) revealed widening of the intradiploic space along the mandibular fossa of the left temporal bone. The inner table appeared elevated in a cinder shape with a vent-like opening through which the soft tissue-fat content was extruded. A volume-rendered image, providing a top-down view of the middle cranial fossa, demonstrated this vent-like opening (Fig. 1B, right). Subsequent brain MRI showed T1/T2 hyperintensity of the lesion in the suprasellar cistern extending into the left temporal lobe (Fig. 1C, left; Fig. 1D, left), with complete suppression on fat-saturated images (Fig. 1D, right). T1 hyperintense foci were also noted in the frontal horn of the left lateral ventricle and right Sylvian fissure (Fig. 1C, right). No enhancement was observed on post-contrast scans, and no meningeal enhancement was seen (Fig. 1E, left). However, the lesion showed blooming due to susceptibility artifacts on susceptibility-weighted imaging (Fig. 1E, right).
Fig. 1. Radiological features of intracranial rupture of intradiploic dermoid cyst in a 50-year-old female.
A. Left: non-contrast axial CT shows a predominantly fat-dense lesion (mean attenuation of -29.92 Hounsfield unit), measuring 4 × 1.5 × 1.2 cm (TR × CC × AP), at the basal cisterns in the left parasellar region extending into the left temporal lobe. Right: non-contrast axial CT reveals the presence of a fat droplet in the frontal horn of the left lateral ventricle (arrow).
B. Left: sagittal multiplanar reconstruction of CT image demonstrates a widened intradiploic space (*) with an evident fatty mass protruding (arrow) through a cinder-shaped vent in the inner table of the left temporal bone. Right: surface-shaded volume-rendered CT image of the middle cranial fossa provides an en-face perspective of the round opening of the defect in the inner table (arrow).
C. Left: T1-weighted axial MR image depicts a hyperintense mass protruding from the left temporal region into the parasellar region (arrow). Right: T1-weighted axial MR image indicates the presence of T1-hyperintense foci in the frontal horn of the left lateral ventricle (doubleline arrow) and the right Sylvian fissure (dashed arrow).
D. Left: T2-weighted MRI coronal image shows a T2-hyperintense lesion in the left temporal region (arrowhead). Right: T1-weighted fat-saturated pre-contrast axial image shows complete suppression of fat (arrow).
E. Left: T1-weighted fat-saturated post-contrast coronal image demonstrates no enhancement of the lesion or meninges (arrowhead). Right: susceptibility-weighted axial magnitude image shows blooming in the lesion due to susceptibility artifacts (arrow).
AP = anterioposterior, CC = craniocaudal, TR = transverse
These distinct imaging findings, presenting an unusual appearance akin to that of a volcano, raised the possibility of an intracranial rupture of an intradiploic dermoid cyst into the subarachnoid space. The patient chose not to undergo surgical intervention and was prescribed an antiepileptic medication. Follow-up appointments were scheduled, and the patient was advised to visit the emergency department if she experienced sudden neurological symptoms, such as seizures or weakness.
Written informed consent was obtained from the patient.
DISCUSSION
Dermoid cysts are thought to originate from dermal and epidermal tissues entrapped along the cranial fusion lines during embryogenesis. These lesions primarily occur in the extra-axial and midline locations, with the suprasellar cistern, posterior fossa, and frontonasal region being the most common sites (1). Intradiploic dermoid cysts represent between 0.04% and 0.7% of all cranial tumors and have been scarcely documented, with rupture being the rarest manifestation (2).
The clinical manifestations of these cysts typically remain dormant until rupture occurs. While rupture itself is not usually fatal, it can lead to severe complications, such as chemical meningitis, seizures, vasospasm, and infarction (3). Rupture of intradiploic dermoid cysts has been documented in a limited number of case reports. Gulsen et al. (4) reported a case of an intradiploic dermoid cyst adherent to the torcula herophili that eroded the overlying scalp and bone tissue. Mishra et al. (5) reported another case of a ruptured intradiploic following trauma, with content spillage into the underlying extradural hematoma as well as extracranially. The patient developed aseptic chemical meningitis and was treated with intravenous steroids.
Although the exact etiology of intradiploic dermoid cyst rupture is unclear, insights can be drawn from hypotheses regarding intracranial dermoid cyst ruptures. Potential mechanisms include age-related hormonal changes leading to rapid cyst expansion (3), sudden growth spurts in small dermoids (6), and mechanical stress from head movements or brain pulsation (7). However, the latter mechanism is less likely to occur in intradiploic dermoids due to their anatomical location. Therefore, our case supports theories emphasizing rapid cyst expansion as the primary factor in rupture. Further studies are required to definitively determine the precise pathophysiological mechanisms involved.
In our case, the intradiploic dermoid cyst expanded the intradiploic space, creating a “cinder-shaped” elevation of the inner table. Following rupture, a “vent-like” opening emerged, allowing the soft tissue-fat content to protrude, resembling a volcanic eruption. This visual representation bore a striking resemblance to a volcanic eruption, with the raised inner table likened to a “mound,” the predominantly fat-dense lesion resembling “lava,” and the widened intradiploic space evoking the concept of a “magma chamber”. In the radiological literature, the term “volcano sign” has been previously used by Prabhu (8) to characterize other extra-axial lesions, such as aggressive neoplastic epidural lesions with subdural extension. He described this phenomenon as having a distinctive appearance resulting from a localized rupture of the dural lining, leading to a notable subdural component due to the rapid growth of the lesion. This analogy compares an active volcano releasing an ash cloud and lava from its vent. In our case, the vent corresponds to the inner table rather than the dural lining.
Radiological diagnosis of dermoid cysts depends on identifying the lipid content. They often appear as well-defined, lobulated midline masses on imaging, with high signal intensity on T1-weighted MR images and low attenuation (indicative of fat density) on CT scans. They usually do not show contrast enhancement. Differential diagnoses based on imaging include epidermoid cysts, lipomas, craniopharyngiomas, and teratomas (1). Each presents distinct characteristics on imaging studies, such as CT and MRI, aiding in differentiation from dermoid cysts.
The optimal therapeutic approach for intracranial dermoid is complete surgical excision. However, it is advisable to deliberately retain residual tumor capsules adhered to neurovascular structures to mitigate potential complications (9). Small lesions can often be extracted as a whole entity, whereas large lesions may require intracapsular decompression. Vigilant postoperative monitoring is recommended after full resection due to the potential for tumor recurrence. There is also some evidence in favor of a non-operative approach for the managing ruptured intracranial dermoid cysts, particularly in patients presenting without any neurological deficits (10).
The widespread dispersal of lipid droplets into the subarachnoid space following cyst rupture makes complete removal impossible. Despite these fat particles persisting for years, long-term observations using MRI and clinical assessments have not shown any deterioration or movement of the fat. Cyst rupture is generally spontaneous and not life-threatening, and the remaining fat in the subarachnoid space often does not cause symptoms for years (9).
In conclusion, the calvarial intradiploic space is a rare location for dermoid cysts, and spontaneous rupture into the subarachnoid space through a breach in the inner table is exceptionally uncommon. The imaging feature of the presented case gives a very unique “erupting volcano” appearance. This unprecedented presentation not only highlights the rarity of such occurrences but also underscores the importance of heightened recognition and understanding of this rare phenomenon involving intracranial dermoid cysts.
Footnotes
- Conceptualization, A.A., S.S.
- formal analysis, A.A., S.S., G.V.
- investigation, A.A., B.S.
- methodology, A.A., S.S.
- supervision, S.S.
- validation, G.V., B.S.
- writing—original draft, A.A.
- writing—review & editing, S.S., G.V., B.S.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Funding: None
References
- 1.Smirniotopoulos JG, Chiechi MV. Teratomas, dermoids, and epidermoids of the head and neck. Radiographics. 1995;15:1437–1455. doi: 10.1148/radiographics.15.6.8577967. [DOI] [PubMed] [Google Scholar]
- 2.Vega RA, Hidlay DT, Tye GW, Fuller CE, Rhodes JL. Intradiploic dermoid cyst of the lateral frontotemporal skull: case report and review of the literature. Pediatr Neurosurg. 2013;49:232–235. doi: 10.1159/000363329. [DOI] [PubMed] [Google Scholar]
- 3.Stendel R, Pietilä TA, Lehmann K, Kurth R, Suess O, Brock M. Ruptured intracranial dermoid cysts. Surg Neurol. 2002;57:391–398. doi: 10.1016/s0090-3019(02)00723-1. discussion 398. [DOI] [PubMed] [Google Scholar]
- 4.Gulsen S, Yilmaz C, Serhat C, Altinors N. Ruptured intradiploic dermoid cyst overlying the torcular herophili. Neurol Neurochir Pol. 2010;44:308–313. doi: 10.1016/s0028-3843(14)60047-5. [DOI] [PubMed] [Google Scholar]
- 5.Mishra SS, Das D, Das S, Panigrahi S. Ruptured intradiploic dermoid cyst into an extra dural hematoma in a traumatic brain injury patient. Indian J Neurotrauma. 2014;11:175–177. [Google Scholar]
- 6.Shashidhar A, Sadashiva N, Prabhuraj AR, Narasingha Rao K, Tiwari S, Saini J, et al. Ruptured intracranial dermoid cysts: a retrospective institutional review. J Clin Neurosci. 2019;67:172–177. doi: 10.1016/j.jocn.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 7.Lunardi P, Missori P. Supratentorial dermoid cysts. J Neurosurg. 1991;75:262–266. doi: 10.3171/jns.1991.75.2.0262. [DOI] [PubMed] [Google Scholar]
- 8.Prabhu SP. “Volcano sign”—description of a sign of aggressive neoplastic epidural lesions with subdural extension. Childs Nerv Syst. 2009;25:399–402. doi: 10.1007/s00381-009-0818-6. [DOI] [PubMed] [Google Scholar]
- 9.Liu JK, Gottfried ON, Salzman KL, Schmidt RH, Couldwell WT. Ruptured intracranial dermoid cysts: clinical, radiographic, and surgical features. Neurosurgery. 2008;62:377–384. doi: 10.1227/01.neu.0000316004.88517.29. discussion 384. [DOI] [PubMed] [Google Scholar]
- 10.Alsallamin I, Choudhury R, Somoza-Cano FJ, Makadia A, Mudrieddy M, Weiland A, et al. An unusual presentation of spontaneous rupture of dermoid cyst. Cureus. 2022;14:e21976. doi: 10.7759/cureus.21976. [DOI] [PMC free article] [PubMed] [Google Scholar]