Abstract
Cerebral hyperperfusion syndrome is a rare complication that can occur following carotid artery revascularization procedures in patients with chronic carotid artery stenosis. Cases of hyperperfusion syndrome resulting solely from intravenous tissue plasminogen activator administration, without a history of revascularization, are extremely rare. Only four of such cases have been reported with imaging evidence. This report presents a case of early neurological deterioration in acute ischemic stroke, identified as a form of hyperperfusion syndrome. Imaging evidence supports this diagnosis, and highlights the occurrence of hyperperfusion syndrome after intravenous tissue plasminogen activator administration.
Keywords: Cerebrovascular Circulation, Perfusion Imaging, Reperfusion Injury, Stroke, Tissue Plasminogen Activator
Abstract
과관류증후군은 만성적인 경동맥 협착이 있는 환자에서 주로 경동맥의 재개통시술 이후 발생하는 부작용으로 알려져 있다. 특히 재개통시술의 이력 없이 단순 정맥내 조직플라스미노겐활성제 사용만으로 발생하는 과관류증후군은 매우 드물며, 영상의학적 근거가 뒷받침되는 증례는 단 4례만이 보고되어 있다. 본 논문은 정맥내 조직플라스미노겐활성제 사용 후 과관류증후군 형태로 조기 신경학적 악화가 발생한 급성 뇌경색 환자에 관한 증례보고 논문으로 영상의학적으로 명백한 과관류증후군의 소견이 관찰되어 해당 증례를 보고하고자 한다.
INTRODUCTION
Cerebral hyperperfusion syndrome (CHS) is a rare complication that manifests with clinical symptoms, including headache, vomiting, seizures, altered consciousness, and neurological deficits following revascularization procedures or bypass surgery in patients with chronic cerebrovascular occlusive disease (1). The occurrence of CHS exclusively owing to the administration of intravenous tissue plasminogen activator (t-PA) without any prior revascularization procedures is extremely rare. To the best of our knowledge, only four cases of this specific condition, supported by imaging evidence have been reported in the literature (2). The term “early neurological deterioration (END),” defined as rapid neurological worsening within the first day after the onset of acute ischemic stroke, is typically associated with ischemic progression, brain edema, or intracranial hemorrhage rather than CHS. Therefore, the diagnosing CHS in cases with END is challenging (3). However, it is crucial to highlight the imaging manifestations of abnormal blood flow and blood-brain barrier (BBB) disruption, which are pathophysiologic features of CHS (4). These imaging findings, though infrequent, can serve as potential imaging markers that aid in the identification and management of clinically subtle but diagnostically challenging complications.
This study aims to report a case of END attributed to CHS, where no other factors contributing to neurological worsening were evident in a patient undergoing intravenous t-PA treatment for acute ischemic stroke. This case highlights the radiological manifestations of cerebral hyperperfusion and BBB disruption.
CASE REPORT
An 80-year-old male patient presented to the emergency department with a complaint of right-hand weakness that began 90 min earlier. The patient had a history of diabetes and previously underwent percutaneous coronary intervention for unstable angina, for which he was treated with clopidogrel. No history of cerebrovascular diseases was observed. Upon arrival, the blood pressure of the patient was 150/62 mmHg. The patient was alert with Glasgow Coma Scale (GCS) score of 14. Neurological examination showed right central facial palsy, with the motor power grade of the right upper and lower extremities graded as III and IV, respectively. Based on these findings, the National Institutes of Health Stroke Scale (NIHSS) score was determined to be 11 at the time of admission to the emergency room.
Upon arrival at the emergency department, brain imaging was performed, including CT angiography (CTA), CT perfusion (CTP), and diffusion weighted imaging (DWI) via MRI. Brain CTA and CTP revealed moderate stenosis in the left common carotid artery and proximal internal carotid artery, without any perfusion abnormalities in both cerebral hemispheres (Fig. 1A, B). Brain DWI revealed multiple lesions with diffusion restriction in the left frontoparietal cortex, left occipital cortex, and basal ganglia (Fig. 1C).
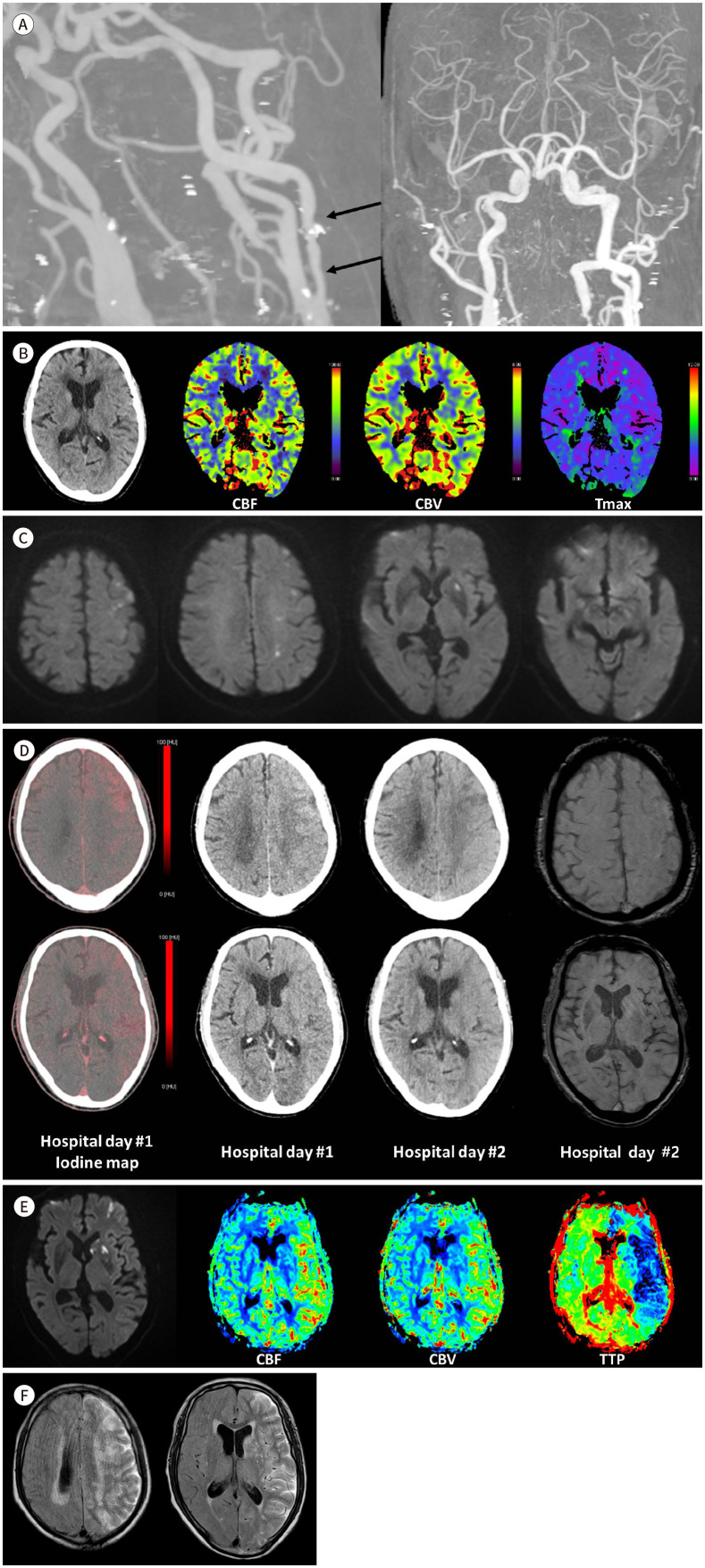
Fig. 1. An 80-year-old man with END as a form of CHS in acute ischemic stroke.
A. Brain CTA at the initial visit to the emergency department reveals moderate segmental stenosis in the left proximal internal carotid artery (arrows). Notably, there is patent flow to intracranial arteries with no evidence of occlusion or significant stenosis in intracranial arteries.
B. Brain CT and CTP at the initial visit to the emergency department. Non-enhanced brain CT shows no signs of intracranial hemorrhage and no clear hypodense area indicative of acute infarction. Brain CTP indicates symmetrical perfusion in both cerebral hemispheres, with no distinct perfusion abnormalities.
C. DWI during the initial visit to the emergency department. Multifocal tiny lesions with restricted diffusion, indicating acute infarction, are observed in the left frontoparietal cortex and white matter, left basal ganglia and left occipital cortex.
D. Dual-energy brain CT performed after trans-femoral cerebral angiography on the day of admission, follow-up brain CT and SWI on day 2 of hospitalization. The dual-energy CT obtained on the day of admission shows diffuse hyperdensities in the cortex of the left cerebral hemisphere, predominantly in the frontoparietal lobes. The follow-up brain CT, conducted on day 2 of hospitalization, reveals a reduction in the extent of diffuse hyperattenuation. In contrast, no hyperdense lesions are observed in the cortex of the right cerebral hemisphere, indicating that only the BBB in the left cerebral hemisphere is disrupted. Furthermore, the SWI performed on day 2 of hospitalization reveals no evidence of hemorrhage.
E. DWI and perfusion MRI on the 2nd day of hospitalization. DWI reveals a slight increase in the extent of acute infarction in the left cerebral hemisphere. Perfusion MRI demonstrates significantly increased CBF and CBV, along with decreased TTP in the left cerebral hemisphere compared to the right, indicating hyperperfusion.
F. FLAIR images on day 3 of hospitalization. FLAIR images show a high signal intensity along the cerebrospinal fluid space in the left cerebral hemisphere. This high signal intensity is presumed to be associated with the gadolinium contrast agent administered the previous day for the perfusion MRI.
BBB = blood-brain barrier, CBF = cerebral blood flow, CBV = cerebral blood volume, CHS = cerebral hyperperfusion syndrome, CTA = CT angiography, CTP = CT perfusion, DWI = diffusion weighted imaging, END = early neurological deterioration, FLAIR = fluid-attenuated inversion recovery, SWI = susceptibility weighted imaging, Tmax = time-to-maximum, TTP = time to peak
Since the onset of the symptoms was well-defined, intravenous t-PA was administered 2 h and 30 min after the symptoms onset. After administration, the patient was transferred to the neurointensive care unit for further intensive care. Approximately 2 h and 40 min after intravenous t-PA administration, a decrease was observed in the level of consciousness of the patient with worsening of right-hand weakness, leading to a GCS score reduction from 14 to 11 and an increase in the NIHSS score from 11 to 17. Meanwhile, the blood pressure of the patient rose to 192/71 mmHg. Owing to clinically suspected ischemia progression, a transfemoral cerebral angiography was performed. However, no signs of severe stenosis or thrombosis were observed, leading to the decision not to proceed with intra-arterial thrombectomy, and the procedure was concluded.
On the dual-energy CT images obtained after the procedure, diffuse hyperdensities were observed along the cortex of the left cerebral hemisphere. By the following day, a brain CT showed a reduction in the extent of these hyperdense lesions. The susceptibility weighted imaging (SWI) sequence of the brain MRI obtained on day 2 of hospitalization showed no hypointense lesion indicative of hemorrhage in the cortex of the left cerebral hemisphere, where hyperdense lesions had previously been observed on CT. Hence, these densities were presumed to result from the enhancement of the contrast agent used in the earlier procedure, suggesting BBB disruption (Fig. 1D).
On day 2 of hospitalization, the level of consciousness of the patient worsened from confusion to stupor. Given that the patient had a cerebral infarction, the target blood pressure was set at 180 mmHg, and the systolic blood pressure of the patient was maintained between 160 and 180 mmHg. Following this, a brain MRI with dynamic contrast-enhanced perfusion imaging was performed. The result of DWI showed a slight increase in the extent of multiple acute infarctions in the left cerebral hemisphere. However, brain perfusion MRI demonstrated significantly increased relative cerebral blood flow (CBF) and relative cerebral blood volume (CBV) in the left cerebral hemisphere, along with a decreased time to peak (TTP). This indicates a substantial increase in perfusion compared to the contralateral hemisphere (Fig. 1E). On day 3 of hospitalization, the fluid-attenuated inversion recovery (FLAIR) sequence of brain MRI showed sulcal hyperintensity along the sulcal cerebrospinal fluid space of the left cerebral hemisphere (Fig. 1F), suggesting the ongoing disruption of the BBB. Based on the clinical presentation of the patient and radiological findings, CHS was suspected. However, since the patient already had a cerebral infarction, blood pressure was managed using a calcium channel blocker (CCB), which allows for easy titration, with a target systolic blood pressure below 140 mmHg. Following the administration of the CCB, the systolic blood pressure of the patient remained below the target of 140 mmHg. No changes were observed in the mental status or motor power of the patient immediately after the CCB administration. However, on day 8 of hospitalization, the patient regained consciousness, and the NIHSS score decreased from 17 to 11. On day 15 of hospitalization, a brain perfusion MRI revealed symmetrical perfusion in both cerebral hemispheres, with no signs of newly developed acute infarction. On day 22 of hospitalization, the condition of the patient, including vital signs and mental status, was stable. Consequently, the patient was transferred to the Department of Rehabilitation for further rehabilitation therapy.
DISCUSSION
CHS is a rare complication that can occur following revascularization procedures, including carotid endarterectomy, carotid artery stenting, or intracranial bypass surgery in patients with chronic cerebrovascular occlusive disease. It presents with clinical symptoms such as headache, vomiting, seizures, altered consciousness, and neurological deficits. CHS is typically defined as an increase in CBF by >100% in the cerebral hemisphere that has undergone revascularization procedures, as compared to preoperative levels on imaging studies, or as the emergence of the previously mentioned neurological symptoms following these procedures. The pathophysiology of CHS involves multiple factors, primarily owing to the inadequate adaptation of CBF to the increased flow after a procedure, especially when autoregulation of CBF is compromised due to chronic hypoperfusion (1). The occurrence of END in the form of CHS following the use of intravenous t-PA alone, without a revascularization procedure, is exceedingly rare in patients with acute ischemic stroke without other identifiable causes for END after intravenous t-PA administration.
END refers to a rapid deterioration in neurological function within the first day after onset of acute ischemic stroke. Definitions may vary among institutions; however, it is generally defined as an increase of >4 points from the baseline NIHSS score. The incidence of END after intravenous t-PA administration ranges from 6.7% to 13.8%, significantly increasing the risk of disability and mortality (3). Despite various known contributing mechanisms, a unified classification system, and established pathophysiology for END remain undocumented. Recently, Kim et al. (5) proposed categorizing END following thrombolysis into two types: ischemia and non-ischemia progression, which includes brain edema and symptomatic hemorrhagic transformation. This categorization is based on the distinct treatment approaches and outcomes related to each type. Brain edema-induced END is often understood as severe edema causing a mass effect on the infarcted brain parenchyma. However, there is a tendency to classify cases showing signs of CHS or BBB disruption as brain edema, which is primarily considered to be related to reperfusion injury (6).
In perfusion studies, CHS can be identified radiologically by a paradoxical increase in CBF or CBV, along with a decrease in TTP in regions where infarction has occurred (7). Additionally, other imaging findings may indicate disruption of BBB (4,8). A key imaging marker of BBB disruption is the hyperintense acute reperfusion marker (HARM), which emerges on post-contrast FLAIR sequences as an enhancement of the cerebrospinal fluid space in damaged cerebral regions (4). Similarly, on non-contrast CT imaging, the parenchyma of damaged cerebral regions may show high attenuation areas, possibly owing to the contrast agent employed in a prior procedure. This phenomenon, associated with BBB breakdown, is well-documented in the literature. These radiological findings can sometimes be challenging to differentiate from post-procedural hemorrhage. Dual-energy CT can help distinguish between simple contrast staining and brain hemorrhage. Additionally, in cases of contrast staining, the extent tends to decrease over time, unlike hemorrhage (8). In our case, brain MRI with FLAIR sequence clearly revealed the HARM sign and diffuse hyperdensities were observed in the cortex of the left cerebral hemisphere. However, dual-energy CT and follow-up brain CT findings suggest contrast staining rather than hemorrhage. The absence of brain hemorrhage on SWI taken the next day also supports this claim. Thus, the hyperdensities observed in the left cerebral cortex on CT can be attributed to contrast staining. This finding aligns with the HARM sign on MRI, which also results from BBB breakdown.
In particular, this case demonstrated a close temporal association between END and t-PA administration, and the imaging findings of hyperperfusion and BBB disruption in the damaged left cerebral hemisphere were visually confirmed. Another condition that needs to be differentiated is luxury perfusion. However, luxury perfusion typically occurs in the subacute stage of cerebral infarction, which distinguishes it from the patient in this case (9).
Importantly, this case suggests that CHS can occur even when only t-PA is used. In clinical practice, the causes of END following t-PA administration are often attributed to intracranial hemorrhage or ischemia progression. Meanwhile, non-ischemia progression type of END, such as midline shifting or significant mass effect to the infarcted brain, tends to attract more attention. In contrast, cerebral edema expressed solely through BBB disruption without severe cerebral edema can be overlooked. Consequently, this type of cerebral edema might be missed if insufficient clinical suspicion exists or if imaging studies, such as perfusion studies or post-contrast FLAIR sequences, do not reveal it.
Zhang et al. (2) reported four cases where CHS was confirmed radiologically and was solely triggered by the use of t-PA. In these cases, t-PA administration was temporally correlated with END events—including confusion, seizures, and worsening hemiplegia. The radiological evidence presented in their study suggests findings consistent with CHS on CTP. Zhang et al. (2) observed that, in three of four cases, the intracranial arteries in the infarcted hemisphere were dilated compared to those in the contralateral side (2). In contrast, our case did not show a significant difference in the diameter of intracranial arteries between both hemispheres.
The pathophysiology and risk factors for CHS following endovascular therapies are relatively well understood; however, the mechanisms underlying CHS after t-PA administration remain largely unclear. The pathophysiology of CHS generally involves chronic impairment of cerebrovascular autoregulation, which fails to accommodate a sudden increase in blood flow (1). However, t-PA administration is less likely to cause a sudden surge in blood flow than endovascular therapies such as carotid artery stenting or carotid endarterectomy.
CHS following t-PA administration may not be caused by a significant increase in CBF but rather by severe impairment of cerebrovascular autoregulation, rendering the brain susceptible to even minor changes in blood flow. Individual patient risk factors or clinical predictors that severely impair autoregulation may play a crucial role in CHS development. Known clinical predictors of CHS after endovascular therapy include being female, having a history of chronic kidney disease, older age, and involvement of the left carotid artery. These factors are frequently associated with microvascular damage and alterations in intracranial vascular geometry and flow dynamics (10).
Meanwhile, the clinical predictors of CHS observed after endovascular therapy do not show a clear correlation with our case or the cases reported by Zhang et al. (2) When combining our case with those reported by Zhang et al. (2), the only shared factor was older age, ranging from 61 to 92 years. No apparent sex preferences were observed, and none of the patients had a history of chronic kidney disease. Most patients, with the exception of one, had underlying cardiovascular conditions such as hypertension, diabetes, atrial fibrillation, and unstable angina. This suggests that these patients may have had preexisting vulnerabilities in their cerebrovascular microvasculature, potentially exacerbating the failure of BBB autoregulation.
Three of four cases reported by Zhang et al. (2) had a history of cancer, which led to the hypothesis that cancer may influence the microvascular environment, although this is not applicable to our case. Additionally, both our case and those of Zhang et al. (2) (five cases) involved infarctions in the left cerebral hemisphere. Given that left cerebral hemisphere infarctions are generally more common than those on the right, the limited number of cases necessitates further research to draw definitive conclusions.
In summary, for patients who experience unexplained END following the use of t-PA alone, considering the possibility of CHS is crucial. In these cases, conducting perfusion studies or post-contrast FLAIR imaging can help in making an accurate diagnosis. Owing to the limited number of cases and the incomplete understanding of the pathophysiology and risk factors, further research is warranted. The factors leading to END following t-PA administration can vary from common issues, including hemorrhagic transformation, to less common conditions, such as the rarer CHS. Consequently, considering clinical symptoms and radiological findings to develop an appropriate treatment plan is essential, as this has significant implications for patient prognosis.
Footnotes
- Conceptualization, K.S.S., J.J.
- supervision, K.S.S., K.S.
- visualization, K.N.H., K.S.S., O.H.Y., J.J.
- writing—original draft, K.N.H.
- writing—review & editing, all authors.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Funding: None
References
- 1.van Mook WN, Rennenberg RJ, Schurink GW, van Oostenbrugge RJ, Mess WH, Hofman PA, et al. Cerebral hyperperfusion syndrome. Lancet Neurol. 2005;4:877–888. doi: 10.1016/S1474-4422(05)70251-9. [DOI] [PubMed] [Google Scholar]
- 2.Zhang Y, Kumar A, Tezel JB, Zhou Y. Imaging evidence for cerebral hyperperfusion syndrome after intravenous tissue plasminogen activator for acute ischemic stroke. Case Rep Neurol Med. 2016;2016:8725494. doi: 10.1155/2016/8725494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seners P, Turc G, Oppenheim C, Baron JC. Incidence, causes and predictors of neurological deterioration occurring within 24 h following acute ischaemic stroke: a systematic review with pathophysiological implications. J Neurol Neurosurg Psychiatry. 2015;86:87–94. doi: 10.1136/jnnp-2014-308327. [DOI] [PubMed] [Google Scholar]
- 4.Warach S, Latour LL. Evidence of reperfusion injury, exacerbated by thrombolytic therapy, in human focal brain ischemia using a novel imaging marker of early blood-brain barrier disruption. Stroke. 2004;35(11 Suppl 1):2659–2661. doi: 10.1161/01.STR.0000144051.32131.09. [DOI] [PubMed] [Google Scholar]
- 5.Kim JM, Moon J, Ahn SW, Shin HW, Jung KH, Park KY. The etiologies of early neurological deterioration after thrombolysis and risk factors of ischemia progression. J Stroke Cerebrovasc Dis. 2016;25:383–388. doi: 10.1016/j.jstrokecerebrovasdis.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 6.Zhang YB, Su YY, He YB, Liu YF, Liu G, Fan LL. Early neurological deterioration after recanalization treatment in patients with acute ischemic stroke: a retrospective study. Chin Med J (Engl) 2018;131:137–143. doi: 10.4103/0366-6999.222343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin YH, Liu HM. Update on cerebral hyperperfusion syndrome. J Neurointerv Surg. 2020;12:788–793. doi: 10.1136/neurintsurg-2019-015621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoon W, Seo JJ, Kim JK, Cho KH, Park JG, Kang HK. Contrast enhancement and contrast extravasation on computed tomography after intra-arterial thrombolysis in patients with acute ischemic stroke. Stroke. 2004;35:876–881. doi: 10.1161/01.STR.0000120726.69501.74. [DOI] [PubMed] [Google Scholar]
- 9.Braileanu M, Weinberg BD, Hu R, Hoch MJ. Appearance of cerebral infarct fogging on CT perfusion. Radiol Case Rep. 2019;14:889–893. doi: 10.1016/j.radcr.2019.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.González García A, Moniche F, Escudero-Martínez I, Mancha F, Tomasello A, Ribó M, et al. Clinical predictors of hyperperfusion syndrome following carotid stenting: results from a national prospective multicenter study. JACC Cardiovasc Interv. 2019;12:873–882. doi: 10.1016/j.jcin.2019.01.247. [DOI] [PubMed] [Google Scholar]