Abstract
Background
Many patients with type 2 diabetes mellitus (T2DM) face barriers to maintain a healthy lifestyle. This study investigated the perceived barriers to healthy eating and physical activity and compared them by demographic and diabetes-related characteristics among patients with T2DM.
Methods
A cross-sectional study was conducted among 534 patients with T2DM attending primary healthcare centers in Hail City from January to June 2023. Data analyzed at a significance level of <0.05.
Results
Barriers to healthy eating and physical activity were perceived by 34.9% and 28% of patients, re-spectively. Personal and environmental barriers to healthy eating were perceived more frequently than social barriers (43.0% and 26.9%, respectively). Personal and environmental barriers to physical activity were perceived by 28.0% of patients, followed by social barriers (27.9%). The most frequently perceived barrier to healthy eating was a lack of motivation (61.6%), followed by insufficient information about healthy diets (32.2%). Regarding physical activity, a lack of motivation was the most frequently perceived personal barrier (32.0%), while a lack of a supportive work environment was the most frequently perceived social barrier (33.7%). Patients who were aged between 30 and 40 years, were highly educated, were diagnosed with DM within less than five years, and used insulin injections as a strategy to manage DM reported significantly higher levels of perceived barriers to healthy eating compared to their counterparts. In contrast, patients who were female, married, had poor financial status, and used insulin injections reported significantly higher levels of perceived barriers to physical activity compared to their counterparts.
Conclusion
Over one-third of patients with T2DM seeking medical care in Hail City perceive barriers to healthy eating, mainly a lack of motivation, insufficient diet information. Educational programs that consider the unique characteristics of patients should be developed.
Keywords: Healthy lifestyle, healthy eating, physical activity, barrier, adherence, type 2 diabetes mellitus, Saudi Arabia
Introduction
Diabetes mellitus (DM), particularly type 2 DM (T2DM), is a major global health challenge, affecting millions of people and associated with considerable morbidity and mortality.1 According to the World Health Organization (WHO), an estimated 422 million people are afflicted with DM worldwide, mostly in low- and middle-income countries.2 It also contributes to approximately 1.5 million deaths annually, making it one of the top 10 causes of death globally.2 Saudi Arabia ranks among the top 10 countries in the world with the highest prevalence of DM, with a reported rate of 23.7%.3
DM presents a significant financial burden on individuals, national health systems, and entire countries worldwide. In 2011, diabetes-related expenses constituted 11% of the total global healthcare expenditure. Notably, in Saudi Arabia, the national financial burden of diabetes was $0.87 billion in 2010 and was projected to reach $6.5 billion by 2020, excluding the indirect costs associated with the disease.4
Effective management of T2DM requires a holistic approach to lifestyle changes, including diet, physical activity, medication adherence, smoking cessation, blood pressure control, lipid management and psychological well-being. The WHO describes a healthy lifestyle as a mode of living that reduces the risk of severe illness or early mortality.5 Pender’s Health Promotion Model identifies barriers to a healthy lifestyle as factors that directly prevent the execution of health-promoting behaviors or indirectly by diminishing the commitment to a behavioral change plan.6 For instance, engaging in regular physical activity, adopting healthier eating habits and quitting smoking can positively impact various anthropometric parameters.7,8 These include reductions in body weight, body mass index (BMI) and waist circumference, as well as improvements in blood markers linked to glucose and lipid levels.7,8 Regular physical activity can reduce the quantity and dosage of antidiabetic medications, including insulin.9,10 Dietary knowledge can largely contribute to healthier eating habits.11 In Saudi Arabia, the marked increase in unhealthy dietary choices, larger portion sizes and sedentary lifestyles has led to a higher risk of obesity and complications among patients with T2DM.12,13 Fast food consumption has also been on the rise in the country, contributing to the obesity epidemic and exacerbating the concerning T2DM figures.14 Despite the evident advantages of adopting a healthy lifestyle to manage T2DM, many patients face substantial barriers to maintaining such a lifestyle. WHO and various diabetes associations worldwide recommend a combination of dietary management, regular physical activity and adherence to medication regimens for optimal diabetes control. However, the adherence of patients to these recommendations is often suboptimal. For instance, dietary management in diabetes is complex and requires a deep understanding of carbohydrate counting, glycemic index and meal planning, which can be overwhelming for patients.9 Socio-economic factors, such as income levels and access to healthy food options, also play a critical role in dietary choices.15,16 Physical activity is recommended at levels similar to those of the general population, but patients with diabetes often face barriers to regular exercise such as physical limitations due to diabetic complications, a lack of motivation, time constraints and environmental factors.17 Recent evidence shows that diabetes stigma leads individuals to conceal their condition, avoiding necessary actions for effective management. This stigma demotivates self-care behaviors, such as healthy eating, physical activity, and treatment adherence, worsening health outcomes.18 Additionally, medication adherence is critical for maintaining glycemic control and preventing complications. Nevertheless, it can be affected by several factors, including medication regimen complexity, side effects, patient beliefs about the medication and the psychological impact of managing a chronic disease.19,20
The Socio-Ecological Model (SEM) is extensively applied in understanding the intricate interplay among personal, social, and environmental factors that determine lifestyle behaviors.21 This model is particularly compelling because it encompasses a range of influences, from intrapersonal or personal factors (including biological and psychological aspects) to interpersonal/cultural dynamics, organizational structures, physical environments (both built and natural), and policy elements (such as laws and regulations). In our study, we adopted the SEM framework to guide the study and to explore the barriers to a healthy lifestyle within the context of Saudi Arabia. This approach allowed us to examine how these multifaceted factors collectively impact lifestyle choices, providing valuable insights into the specific challenges encountered in promoting healthier living in this setting. Barriers to adopting a healthy lifestyle can vary significantly based on the population, culture and socio-economic conditions across different countries. For instance, lack of time and enjoyment were identified as the main barriers to physical activity among Australian adults,22 while hot weather and occupational commitments were the primary barriers to physical activity among Kuwaiti adults.23 Consequently, it is necessary to investigate and understand barriers to adopting healthy lifestyles in contexts where the environment promotes an unhealthy lifestyle and a culture is inclined towards poor eating habits. This understanding can enable healthcare professionals to identify and prioritize these barriers, develop effective strategies to address them, and implement targeted interventions aimed at helping DM patients embrace healthier living habits that improve the overall management of diseases.24 Therefore, this study aimed to investigate the perceived barriers to healthy eating and physical activity among patients with T2DM in Hail City, Saudi Arabia. In addition, these barriers were compared according to the demographic and diabetes-related characteristics of the patients.
Methods
Study Design, Setting and Population
A cross-sectional descriptive design was conducted at primary healthcare centers (PHC) in Hail City among patients with T2DM who attended follow-up appointments from January to June 2023. Patients were included in the study if they were Saudi nationals over 18 years of age, cognitively capable of understanding and answering the questionnaire and willing to voluntarily participate in the study. Exclusion criteria included patients with diagnosed cognitive impairments or psychiatric conditions that could interfere with their ability to respond accurately, as well as pregnant individuals or those with other chronic conditions beyond T2DM that might independently affect health outcomes.
Sampling Strategy and Sample Size
This study adopted a two-stage sampling strategy. In the first stage, eight PHC centers (Qufar, Aja, Sadyan, Sharaf, Alazizyah, Albadyah, Alnograh, and Alwasyta) were selected based on their pivotal role in the management of patients with T2DM in the city. A minimum sample size of 351 nurses was estimated using OpenEpi, Version 3.01 (www.openepi.com), a program used to calculate the sample size required to determine the frequency of a factor in a population.25 This was based on a population size of 4000, a 95% confidence level, and 5% absolute precision. In the second stage, all eligible patients from the selected PHC centers were approached and invited to participate in the study using convenience sampling. Ultimately, a total of 534 patients were included during the study period.
Instrumentation
The questionnaire included demographic data (including gender, age, height, weight, marital status, financial status and the level of education), diabetes-related data (including antidiabetic medication regimen and the time since T2DM diagnosis). The second section included 23 questions aimed at identifying barriers to healthy eating and physical activity. The section on the barriers was adapted from a questionnaire that had been previously developed and validated,26,27 besides being further validated in this study. Personal barriers included the lack of knowledge, motivation, time, and financial resources, while social barriers included the lack of support from family, friends and colleagues at work. On the other hand, environmental barriers included access to gym facilities, weather suitability for physical activities and cultural constraints. Participants were asked to rate each statement in the section about barriers using a scale of 0–2: (0) no barrier, (1) somewhat barrier, or (2) barrier. Consequently, the total score for barriers to healthy eating ranged from 0 to 20, while the total score for barriers to physical activity ranged from 0 to 26. The questionnaire has previously been utilized and demonstrated good content validity in the context of chronic diseases, including patients with diabetes.28 In this study, the content validity was established through an expert panel made up of two diabetic physicians, three PhD-holding nursing researchers for appropriateness, readability, clarity, and common terminology in order to determine the content validity index (CVI). Each item was given a rating of “essential” (3), “useful but not essential” (2), or “unnecessary” (1) by the panel members. In order to assess the expert panel’s agreement regarding the appropriateness, relevance, and clarity of the questionnaire items, both item CVIs (I-CVIs) and scale CVIs (S-CVIs) were computed (values ranged from 0.81 to 1). The reliability of the questionnaire was established to be good in a previous study,27 with Cronbach’s alpha coefficients of 0.686 and 0.762 for barriers to healthy eating and physical activity, respectively. Furthermore, the present study proved that the questionnaire reliability was good, with Cronbach’s alpha coefficients of 0.724 and 0.813 for barriers to healthy eating and physical activity, respectively.
Data Collection
Patients were invited to participate during their follow-up visits at the PHC. Interested patients received an information sheet with a Quick Response (QR) code. Scanning the QR code directed them to an online platform with comprehensive study information, including the study’s purpose, participant requirements, estimated survey completion time, potential benefits and risks, and the researcher’s contact number for further clarification. Participants could review the information, provide consent, and complete the questionnaire on the same platform.
Ethical Considerations
This study complies with the ethical principles outlined in the Declaration of Helsinki. The protocol of this study was approved by the Institutional Review Board (IRB) at the University of Hail (H-2023-029). Written informed consent was obtained from participants after being informed of the study objectives and that they had the option to withdraw from the study at any point. The privacy of participants and confidentiality of their data were prioritized, ensuring secure handling of their responses. No identifying details, such as names or contact information, were requested in the questionnaire.
Data Analysis
Data were analyzed using IBM SPSS Statistics, version 27.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics, including means and standard deviations (SD) for continuous variables and frequencies with percentages for categorical variables, were applied to summarize participant characteristics and responses.Body mass index (BMI) was calculated based on height and weight data, and categorized according to standard classifications: underweight (BMI <18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) and obese (≥30 kg/m2).29
To test for normality, the Kolmogorov–Smirnov test was used, indicating that the data were not normally distributed (p < 0.05). Consequently, nonparametric tests (the Mann–Whitney U-test and Kruskal–Wallis test) were used to examine how perceived barriers to healthy eating and physical activity differ between demographic and diabetes-related characteristics of the patients, as these tests are well-suited for ordinal data and non-normal distributions. A significance level of p < 0.05 was used to determine statistical significance throughout the analyses.
Results
Characteristics of Participants
Table 1 shows that the majority of patients with T2DM in the present study were females (62.9%). The average age of the patients was 34.4±15.5 years, with a relatively even age distribution between those aged less than 30 years (47.9%) and those above 40 years (32.0%). On average, the patients had been living with T2DM for 5.7±6.2 years, with the majority of patients having received their diagnosis within the past five years (60.9%). In addition, more than one third (39.1%) of patients reported relying on insulin injections as their chosen strategy for managing diabetes. The majority of patients reported having financial status ranged 5000–10000 RS (53.7%) and had attained higher education (59.7%). In terms of body weight, most patients were classified as normal body weight (40.3%), followed by those who were overweight (26.6%) and obese (26.4%). The level of hemoglobin A1c were more than or equal 6.5 for the majority of patients (75.1%).
Table 1.
Characteristics of Participants (n=534)
| Characteristics | n | (%) |
|---|---|---|
| Gender | ||
| Male | 198 | (37.1) |
| Female | 336 | (62.9) |
| Age (years) | ||
| <30 | 256 | (47.9) |
| 30–40 | 107 | (20.0) |
| >40 | 171 | (32.0) |
| Mean ± SD: 34.4±15.5 | ||
| Duration since diagnosis of DM (years) | ||
| <5 | 325 | (60.9) |
| ≥5 | 209 | (39.1) |
| Mean ± SD: 5.7±6.2 | ||
| Marital status | ||
| Married | 266 | (49.8) |
| Unmarried | 268 | (50.2) |
| Financial status | ||
| More than 5000 RS | 230 | (43.1) |
| 5000–10000 RS | 287 | (53.7) |
| Less than 5000 RS | 17 | (3.2) |
| Level of education | ||
| Illiterate | 55 | (10.3) |
| Primary | 36 | (6.7) |
| Secondary | 124 | (23.2) |
| Higher education | 319 | (59.7) |
| Weight categories | ||
| Underweight | 36 | (6.7) |
| Normal weight | 215 | (40.3) |
| Overweight | 142 | (26.6) |
| Obese | 141 | (26.4) |
| DM management strategy | ||
| Diet and a healthy lifestyle | 159 | (29.8) |
| Insulin injections | 209 | (39.1) |
| Oral medications | 166 | (31.1) |
| Hb A1c | ||
| ≤ 5.6 | 28 | (5.2) |
| 5.7–6.4 | 105 | (19.7) |
| ≥ 6.5 | 401 | (75.1) |
Abbreviations: SD, standard deviation; DM, diabetes mellitus; RS, Rial Saudi; Hb A1c, hemoglobin A1c.
Patients’ Perceptions of Barriers to Healthy Diet and Physical Activity
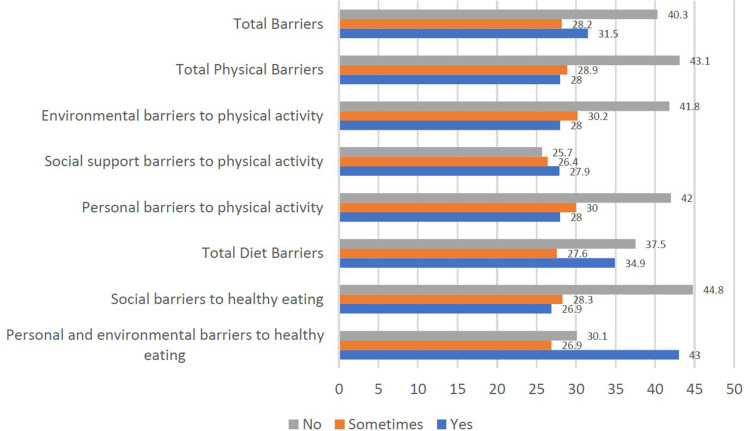
Overall, barriers to healthy eating and physical activity were perceived by 34.9% and 28% of patients, respectively. Personal and environmental barriers to healthy eating were perceived more frequently than social barriers (43.0% and 26.9%, respectively). However, personal and environmental barriers to physical activity were perceived by 28.0% of patients, followed by social barriers (27.9%) (Figure 1).
Figure 1.
Perceived barriers to healthy diet and physical activity among patients with T2DM.
Table 2 shows that a lack of motivation to eat a healthy diet (61.6%) was the most frequently perceived personal and environmental barrier to healthy eating, followed by insufficient information about healthy diets (55.2%). The lack of time to prepare or eat healthy foods (32.2%) and the absence of a work environment that promotes healthy eating (31.3%) were the most frequently perceived social barriers to healthy eating. On the other hand, a lack of motivation to do physical activity, exercise, or sport was the most frequently perceived personal barrier to physical activity, being reported by 32.0% of patients. However, the absence of a work environment that supports physical activity was the most frequently perceived social barrier to physical activity, being reported by 33.7% of patients. Regarding the environmental barriers to physical activity, weather unsuitability for practicing exercise was the most frequently perceived (37.8%), followed by a lack of affordable facilities for physical activity (37.5%).
Table 2.
Perceived Barriers to Healthy Eating and Physical Activity Among Patients with T2DM (n=534)
| Barrier Items | Perception of Barriers n (%) | ||||||
|---|---|---|---|---|---|---|---|
| Yes | Sometimes | No | |||||
| Personal and Environmental Barriers to Healthy Eating | |||||||
| 1 | Do not have enough information about healthy diet | 295 | 55.2 | 160 | 30.0 | 79 | 14.8 |
| 2 | Do not have motivation to eat a healthy diet | 329 | 61.6 | 122 | 22.8 | 83 | 15.5 |
| 3 | Do not enjoy eating healthy food | 265 | 49.6 | 154 | 28.8 | 115 | 21.5 |
| 4 | Do not have skills to plan and shop for preparing or cooking healthy foods | 284 | 53.2 | 143 | 26.8 | 107 | 20.0 |
| 5 | Do not have access to healthy foods | 114 | 21.3 | 158 | 29.6 | 262 | 49.1 |
| 6 | Not able to buy healthy foods that are inexpensive | 90 | 16.9 | 125 | 23.4 | 319 | 59.7 |
| Social barriers to healthy eating | |||||||
| 7 | No family support to eat a healthy diet | 101 | 18.9 | 144 | 27.0 | 289 | 54.1 |
| 8 | No friends’ support to eat a healthy diet | 135 | 25.3 | 144 | 27.0 | 255 | 47.8 |
| 9 | No work environment to eat a healthy diet | 167 | 31.3 | 129 | 24.2 | 238 | 44.6 |
| 10 | Not having time to prepare or eat healthy foods | 172 | 32.2 | 188 | 35.2 | 174 | 32.6 |
| Personal barriers to physical activity | |||||||
| 11 | Do not have motivation to do physical activity, exercise, or sport | 171 | 32.0 | 164 | 30.7 | 199 | 37.3 |
| 12 | Not enjoying physical activity, exercise, or sport | 133 | 24.9 | 176 | 33.0 | 225 | 42.1 |
| 13 | Do not have the skills to do physical activity, exercise, or sport | 152 | 28.5 | 152 | 28.5 | 230 | 43.1 |
| Social barriers to physical activity | |||||||
| 14 | No family support to be physically active | 123 | 23.0 | 151 | 28.3 | 260 | 48.7 |
| 15 | No friends’ support to be physically active | 144 | 27.0 | 143 | 26.8 | 247 | 46.3 |
| 16 | No work environment to be physically active? | 180 | 33.7 | 129 | 24.2 | 225 | 42.1 |
| Environmental barriers to physical activity | |||||||
| 17 | Do not have enough information about how to increase physical activity | 140 | 26.2 | 175 | 32.8 | 219 | 41.0 |
| 18 | Not having access to places to do physical activity, exercise, and sport | 174 | 32.6 | 174 | 32.6 | 186 | 34.8 |
| 19 | Not being able to find physical activity facilities that are inexpensive | 200 | 37.5 | 145 | 27.2 | 189 | 35.4 |
| 20 | Not having the time to be physically active | 160 | 30.0 | 214 | 40.1 | 160 | 30.0 |
| 21 | Feeling shy when practicing exercise outdoors | 79 | 14.8 | 128 | 24.0 | 327 | 61.2 |
| 22 | The weather is not suitable for practicing exercise | 202 | 37.8 | 181 | 33.9 | 151 | 28.3 |
| 23 | Not being able to practice physical activity due to cultural factors | 91 | 17.0 | 112 | 21.0 | 331 | 62.0 |
Abbreviation: T2DM, type 2 diabetes mellitus.
Comparison Between Perceived Barriers to Healthy Eating and Physical Activity According to Demographic and Diabetes-related Characteristics
Table 3 shows that patients in the age range of 30 to 40 years showed significantly higher levels of perceived personal and environmental barriers to healthy eating (p = 0.024) and total dietary barriers (p = 0.003), personal and social barriers to physical activities (p=0.017), as well as the total barriers to healthy eating and physical activity (P=0.043) compared to both younger and older patients. On the other hand, female patients had significantly higher levels of perceived personal, social, and environmental barriers to physical activity (P <0.05) and overall dietary and physical barriers (p = 0.002) compared to males. Married patients had significantly higher levels of perceived personal (p = 0.009), social (p =0.009), environmental (p = 0.002) and total physical barriers (p = 0.001) to physical activity and overall dietary and physical barriers (p = 0.006) compared to unmarried ones.
Table 3.
Differences in Perceived Barriers to Healthy Eating and Physical Activity Among Patients with T2DM According to Their Demographic and Diabetes-Related Characteristics (N=534)
| Variables | N | Barriers to Healthy Eating | Barriers to Physical Activity | Overall Barriers | |||||
|---|---|---|---|---|---|---|---|---|---|
| Personal and Environmental | Social | Total Dietary | Personal | Social | Environmental | Total Physical | |||
| Age (years) | |||||||||
| <30 | 256 | 7 (5–8) | 3 (1–5) | 10 (8–12) | 2 (0–4) | 2 (0–4) | 6 (3–8) | 11 (6–15) | 21 (14–26) |
| 30–40 | 107 | 7 (6–9) | 4 (1–6) | 11 (8–13) | 3 (0–4) | 3 (0–4) | 7 (3–9) | 13 (6–17) | 23 (15–30) |
| >40 | 171 | 6 (5–8) | 3 (1–5) | 9 (7–12) | 2 (0–4) | 2 (0–4) | 7 (3–9) | 12 (4–16) | 21 (11–27) |
| P-value | 0.024 | 0.175 | 0.003 | 0.017 | 0.017 | 0.719 | 0.099 | 0.043 | |
| Gender | |||||||||
| Male | 198 | 7 (5–8) | 3 (1–5) | 9 (8–12) | 2 (0–4) | 2 (0–4) | 6 (2–8) | 10 (3–15) | 19 (12–26) |
| Female | 336 | 7 (5–8) | 3 (1–5) | 10 (8–12) | 3 (0–4) | 3 (0–4) | 7 (4–9) | 12 (6–16) | 22 (14–28) |
| P-value | 0.430 | 0.343 | 0.150 | 0.026 | 0.026 | 0.007 | 0.008 | 0.007 | |
| Marital status | |||||||||
| Married | 266 | 7 (7–8) | 3 (1–6) | 10 (8–13) | 3 (0–4) | 3 (0–4) | 7 (4–9) | 13 (5–17) | 23 (13–29) |
| Unmarried | 268 | 7 (5–8) | 3 (1–5) | 10 (8–12) | 2 (0–4) | 2 (0–4) | 6 (2–8) | 10 (4–15) | 20 (12–26) |
| P value | 0.550 | 0.256 | 0.675 | 0.009 | 0.009 | 0.002 | 0.001 | 0.006 | |
| Financial status | |||||||||
| Excellent | 230 | 7 (6–8) | 3 (0. 75–5) | 10 (8–12) | 2 (0–4) | 2 (0–4) | 6 (2–9) | 10 (3–16) | 20 (12–27) |
| Acceptable | 287 | 7 (6–8) | 3 (1–5) | 10 (8–12) | 3 (0–4) | 3 (0–4) | 6 (4–8) | 12 (5–16) | 22 (13–27) |
| Poor | 17 | 5 (4–7) | 5 (1–8) | 11 (8–13) | 6 (1–6) | 6 (1–6) | 11 (8–13) | 23 (11–25) | 31 (20–37) |
| P-value | 0.006 | 0.029 | 0.596 | 0.023 | 0.023 | 0.002 | 0.006 | 0.010 | |
| Level of education | |||||||||
| Illiterate | 55 | 6 (5–7) | 2 (0–5) | 8 (6–11) | 2 (0–4) | (0–4) | 7 (4–10) | 12 (4–20) | 20 (11–28) |
| Primary | 36 | 7 (5–8) | 3 (0–4) | 8.5 (8–11) | 1.5 (0–4) | 1.5 (0–4) | 6 (3–8) | 11 (3–16) | 21 (11–27) |
| Secondary | 124 | 7 (5–9) | 3 (1–5) | 10 (8–12) | 2 (0–4) | 2 (0–4) | 6 (2–8) | 11 (4–15) | 21 (12–27) |
| Higher education | 319 | 7 (5–8) | 4 (1–5) | 10 (8–13) | 3 (0–4) | 3 (0–4) | 6 (3–8) | 12 (6–16) | 22 (14–28) |
| P-value | 0.011 | 0.043 | <0.001 | 0.775 | 0.775 | 0.472 | 0.877 | 0.596 | |
| Duration since diagnosis of DM (years) | |||||||||
| <5 | 325 | 7 (6–9) | 3 (1–5) | 10 (8–13) | 3 (0–4) | 3 (0–4) | 6 (3–8) | 11 (5–16) | 22 (14–28) |
| ≥5 | 209 | 6 (5–8) | 3 (1–5) | 9 (7–12) | 3 (0–4) | 3 (0–4) | 7 (3–9) | 12 (4–16) | 21 (12–27) |
| P-value | <0.001 | 0.135 | <0.001 | 0.791 | 0.791 | 0.306 | 0.772 | 0.269 | |
| DM management strategy | |||||||||
| Diet and a healthy lifestyle | 159 | 8 (6–8) | 3 (1–5) | 10 (8–12) | 2 (0–3) | 2 (0–3) | 6 (3–8) | 11 (6–14) | 21 (14–26) |
| Insulin injections | 209 | 7 (5–8) | 4 (1–6) | 10 (8–13) | 3 (0.5–5) | 3 (0.5–5) | 7 (4–9) | 13 (6–18) | 23 (16–29) |
| Oral medications | 166 | 6 (5–8) | 2 (0–5) | 9 (8–11) | 2 (0–4) | 2 (0–4) | 6 (2–8) | 10 (2–16) | 19 (11–26) |
| P-value | 0.012 | 0.003 | <0.001 | 0.001 | 0.001 | 0.042 | 0.003 | <0.001 | |
| BMI | |||||||||
| Underweight | 36 | 7 (5–8) | 2 (0=4) | 8 (7–12) | 2 (0–4) | 2 (0–4) | 5 (1–7) | 9 (1–14) | 18 (10–26) |
| Normal | 215 | 7 (5–8) | 3 (1–5) | 10 (8–12) | 2 (0–3) | 2 (0–3) | 6 (3–8) | 10 (5–15) | 20 (14–25) |
| Overweight | 142 | 7 (6–8) | 3 (1–5) | 9 (8–12) | 2 (0–4) | 2 (0–4) | 6 (2–8) | 11 (4–16) | 21 (12–29) |
| Obese | 141 | 7 (5–8) | 4 (2–6) | 10 (8–13) | 3 (1.5–5) | 3 (1.5–5) | 7 (5–9) | 13 (8–18) | 24 (18–30) |
| P-value | 0.708 | 0.013 | 0.215 | 0.003 | 0.003 | 0.002 | <0.001 | 0.001 | |
| HbA1c | |||||||||
| ≤ 5.6 | 28 | 7 (5–8) | 2 (0–4) | 9 (7–11) | 2 (1–3) | 2 (1–3) | 6 (2–8) | 10 (6–13) | 20 (14–23) |
| 5.7–6.4 | 105 | 7 (5–9) | 3 (1–6) | 10 (8–13) | 3 (0.5–5) | 3 (0.5–5) | 7 (4–9) | 13 (6–17) | 23 (15–30) |
| ≥ 6.5 | 401 | 7 (5–8) | 3 (1–5) | 10 (8–12) | 2 (0–4) | 2 (0–4) | 6 (2–8) | 11 (4–16) | 21 (12–27) |
| P-value | 0.777 | 0.059 | 0.123 | 0.018 | 0.018 | 0.370 | 0.037 | 0.032 | |
Notes: N= number of patients, p < 0.05 level. Bold text represents significant values.
Abbreviation: T2DM, type 2 diabetes mellitus.
In terms of financial status, patients with excellent status had a significantly higher level of perceived personal and environmental barriers to healthy eating (p = 0.006) compared to patients with lower financial status. Conversely, patients with poor financial status had significantly higher levels of perceived personal (p = 0.023), social (p = 0.023) and environmental (p <0.002) barriers to physical activity compared to patients with different financial status. Significantly higher levels of perceived personal and environmental barriers and social barriers to healthy eating were observed among patients with a higher educational level (p <0.05) and those diagnosed with DM within less than five years (p <0.05) compared to their counterparts (Table 3).
Patients who adopted the diet and a healthy lifestyle as a strategy to manage DM showed a significantly higher level of perceived personal and environmental barriers to healthy eating (p = 0.012) compared to those who used other management strategies. On the other hand, patients on Insulin injections had significantly higher levels of perceived social barriers to healthy eating (p=0.003) as well as personal (p = 0.001), social (p = 0.001), and environmental (p=042) barriers to physical activity compared to those using other strategies for managing DM. Patients who were obese had more barriers for personal, social, and environmental barriers than other groups (Table 3).
Discussion
The present study identified significant personal, social, and environmental barriers that hinder patients with T2DM in Hail City from adopting healthy eating habits and engaging in regular physical activity. Over one-third of patients with T2DM reported challenges to maintaining a healthy lifestyle. The most commonly perceived barriers to healthy eating were a lack of motivation and insufficient knowledge about healthy diets, while barriers to physical activity included a lack of motivation, unsupportive work environments, unfavorable weather conditions, and limited access to affordable exercise facilities. These barriers were influenced by various demographic and diabetes-related characteristics, including age, gender, marital status, financial status, educational level, and diabetes management strategies. The findings emphasize the importance of tailored interventions to effectively address these challenges and promote healthier lifestyles among patients with T2DM.
Barriers for Healthy Eating Habits
This study highlights that barriers such as lack of motivation and insufficient dietary knowledge significantly impact the ability of patients with diabetes to adhere to healthy eating habits.30 Motivation is crucial for establishing and maintaining healthy routines, as it helps individuals prioritize their health and wellness.31 A lack of motivation can hinder commitment to making healthy food choices, while insufficient knowledge about nutrition affects the ability to select and prepare meals that support diabetes management.32 Understanding nutrition, including food options, portion sizes, and meal planning, empowers patients to make informed decisions that enhance their well-being.33 The interplay between motivation and knowledge is essential for developing and sustaining long-term healthy eating habits.
This study also highlighted significant social barriers to healthy eating among patients with diabetes, particularly an unsupportive work environment and limited time availability. Many workplaces lack access to healthy food options, often offering unhealthy snacks or being located near fast food restaurants.34 Additionally, high-stress work cultures and long hours can discourage prioritizing health and making nutritious food choices.35 Time constraints further exacerbate the challenge, as busy lifestyles often leave individuals struggling to plan meals, shop for groceries, or cook, leading them to opt for convenient but less healthy options like fast food or pre-packaged meals,36 leading them to opt for convenient but less healthy options like fast food or pre-packaged meals.37 Addressing these barriers requires workplace policies that promote access to healthy food, foster a culture supportive of healthy eating, and encourage time-efficient strategies such as meal planning or exploring quick, nutritious meal options.
Environmental barriers, such as limited access to healthy food options and safe venues for physical activity, were significant challenges to healthy practices.38 While external factors influence lifestyle decisions, societal barriers like peer pressure or societal norms were perceived as less impactful by patients, contrasting with Kabir et al39 view that social settings are key determinants of healthy habits. Addressing personal and environmental barriers through targeted interventions can enhance motivation and provide supportive environments, enabling patients to adopt and maintain healthy eating and exercise routines.
Barriers to Engaging in Physical Activity
In this study, lack of motivation was the most frequently perceived personal barrier to engaging in physical activity among patients with diabetes, hindering the consistency needed for regular exercise routines. Without sufficient motivation, people may struggle to find the desire and consistency needed to incorporate regular physical exercise into their daily routines.40 Additionally, the absence of a supportive work environment was the most commonly reported social barrier.41 Sedentary jobs and long work hours limit opportunities for physical activity, highlighting the need for workplace policies that promote exercise through scheduled breaks, fitness facilities, or support for active transportation.42
The findings also highlight that the majority of patients identified unsuitable climate conditions, such as excessive heat, cold, rain, and pollution, as significant obstacles to physical activity.43 These adverse conditions discourage outdoor exercise and diminish motivation. Furthermore, the lack of affordable fitness facilities was the second most reported barrier, with high membership fees and limited access to low-cost options hindering participation, especially for those with financial constraints.44,45 Addressing these challenges involves promoting indoor exercise alternatives, utilizing community facilities offering low-cost or free programs, and advocating for the development of accessible and affordable fitness centers in local communities.46
Social barriers to physical activity include a lack of social support from friends, family, and the community, particularly for seniors who rely on others to participate in activities.47 Environmental barriers, such as limited access to safe, age-friendly spaces like parks and recreation centers, also hinder participation.48 Additionally, cultural norms may devalue exercise or restrict who can engage in physical activities and what types are considered appropriate.48
Factors Influencing Barriers: Demographic and Diabetes-Related Characteristics
Perceptions of barriers to healthy lifestyles varied by demographics and diabetes-related characteristics. Patients aged 30–40 years reported higher levels of barriers to healthy eating, while older individuals faced challenges like physical limitations and medication interactions but often had better nutritional knowledge.49 Tailored strategies are essential to address age-specific barriers and promote healthy eating.50
Female patients with T2DM in this study reported higher barriers due to socio-cultural factors, including gender norms and societal expectations that limit their time and activity options, as well as cultural beliefs discouraging certain physical activities.51 These sociocultural hurdles, in addition to individual and environmental difficulties, heighten the sense of impediments that these women encounter in pursuing an active lifestyle.
Married patients with T2DM in this study reported significantly higher perceptions of personal, social, and environmental barriers to physical activity. This may stem from time constraints due to family responsibilities,52 reduced social support for exercise amidst additional obligations,53 financial commitments limiting access to fitness facilities,44 and lifestyle changes favoring sedentary activities, such as watching television or dining out.54 These factors collectively contribute to decreased opportunities for physical activity.
This study found that patients with higher education levels perceived greater personal and environmental barriers to healthy eating, likely due to time constraints and stress from demanding jobs, leading to reliance on unhealthy food options.55,56 Conversely, patients with lower education levels reported higher barriers to physical activity, attributed to limited knowledge about exercise benefits, socioeconomic challenges, and work constraints. Financial limitations often restrict access to gyms or sports facilities57,58 while physically demanding jobs with long or irregular hours leave little energy or time for exercise.59 These factors highlight the need for tailored interventions to address educational disparities in healthy lifestyle practices.
The present study revealed that patients with excellent financial status had a significantly higher level of perception regarding personal and environmental barriers to healthy eating. In contrast, American people with lower incomes were found to have distinct challenges that make it more difficult for them to get and maintain a healthy diet than those with higher incomes.60 The perceived barriers to healthy eating by those with higher incomes could be related to time constraints, bad dietary choices and marketing influences. Despite the high income in Saudi Arabia, the dietary practices of the majority of the country’s adult population do not comply with official dietary standards.61 A previous study highlighted that lower-income people may have limited access to exercise facilities, leisure centers, or sports clubs due to financial restraints.62 Gym memberships, sports equipment and participation fees for organized sports can be expensive, making them unaffordable for people with low incomes. Moreover, lower-income people often face challenging work schedules, multiple jobs, or caregiving duties, reducing their free time.59
This study found that patients diagnosed within the past five years reported significantly higher personal and environmental barriers to healthy eating. Newly diagnosed patients often face challenges in adopting dietary changes required for effective blood sugar management.14 They may feel overwhelmed or uncertain about food choices, portion sizes, and meal planning, requiring guidance on reading food labels and understanding the impact of foods on their condition.13 Emotional responses like fear or dissatisfaction, along with social challenges such as dining out, can further hinder adherence to a healthy diet.63–65
Obese individuals often face significant barriers to engaging in physical activity and maintaining a nutritious diet due to environmental, societal, and personal factors. Social stigma and judgment can discourage participation in public dining or physical activity settings, while psychological challenges like low self-esteem and body image issues further hinder healthy lifestyle adoption.66 A recent systematic review by Akyirem and Ekpor18 highlights that diabetes stigma can exacerbate these challenges, leading individuals to conceal their condition, avoid necessary self-care actions, and feel demotivated to engage in healthy eating and physical activity. Physical limitations related to size, such as difficulty finding suitable clothing or exercise equipment, also restrict activity options. These combined obstacles make it challenging for obese individuals to adopt and sustain healthy lifestyle practices.67
Strengths and Limitations
This study has several strengths that enhance its relevance and impact. It provides a comprehensive analysis of personal, social, and environmental barriers to healthy lifestyle adherence among patients with T2DM, offering a well-rounded view of the challenges faced in diabetes management. Conducted in Hail City, the study brings culturally specific insights that support tailored interventions for the Saudi population. With a large sample size of 534 participants, the study’s findings are robust and more generalizable to similar populations. However, the present study has several limitations. First, the study adopted a cross-sectional design with a structured questionnaire that does not reflect the changes in perceived barriers over time. To gain a deeper understanding of these perceived barriers, it is recommended to conduct longitudinal studies and incorporate qualitative methods. Second, the study was health facility-based, possibly affecting the generalizability of its findings to the broader diabetic population in the community. Therefore, the study findings should be interpreted cautiously, and large-scale com-munity-based studies are recommended. Third, the use of convenience sampling, whereby participants are selected based on their availability and accessibility, introduces the possibility of bias and may affect the representativeness of the sample. However, given the absence of a defined sampling frame, it is not feasible to employ random sampling in this particular situation.
Conclusions
Over one-third of patients with T2DM in Hail City face barriers to healthy eating, primarily due to lack of motivation, insufficient dietary information, an unsupportive work environment, and limited time for healthy meal preparation. Similarly, barriers to physical activity include lack of motivation, an unsupportive work environment, unfavorable weather, and limited access to affordable exercise facilities. These barriers vary by demographic and diabetes-related factors, highlighting the need for tailored approaches.
Acknowledgments
We thank all patients for their participation in this study.
Funding Statement
This research has been funded by the Scientific Research Deanship at the University of Ha’il, Saudi Arabia, through project number (GR-23021).
Abbreviations
T2DM, type 2 diabetes mellitus; WHO, World Health Organization; BMI, body mass index; SEM, Socio-Ecological Model; PHC, Primary healthcare centers.
Data Sharing Statement
The corresponding author can be contacted for access to the data presented in this study.
Institutional Review Board Statement
This study complies with the ethical principles outlined in the Declaration of Helsinki. The protocol of this study was approved by the Institutional Review Board (IRB) at the University of Hail (H-2023-029). Written informed consent was obtained from participants after being informed of the study objectives and that they had the option to withdraw from the study at any point. The privacy of participants and confidentiality of their data were prioritized, ensuring secure handling of their responses. No identifying details, such as names or contact information, were requested in the questionnaire.
Informed Consent Statement
All participants who took part in the study gave written, informed consent.
Implications for Practice and Policy
To address these challenges, healthcare providers should incorporate motivational counseling and targeted education into routine diabetes care, emphasizing the benefits of healthy lifestyle adherence. Workplaces could implement wellness programs and supportive policies to facilitate healthy eating and physical activity for employees with diabetes. Additionally, local governments and healthcare agencies should consider improving access to affordable exercise facilities and creating community environments that support healthier lifestyle choices, such as parks or climate-controlled activity spaces. Developing educational programs that address specific barriers by demographic group may enhance the effectiveness of self-care interventions, ultimately improving health outcomes for people with diabetes in this region.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
- 1.Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of Type 2 Diabetes - Global Burden of Disease and Forecasted Trends. J Epidemiol Glob Health. 2020;10(1):107–111. doi: 10.2991/jegh.k.191028.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin X, Xu Y, Pan X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10(1):14790. doi: 10.1038/s41598-020-71908-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naeem Z. Burden of Diabetes Mellitus in Saudi Arabia. Int J Health Sci. 2015;9(3):V–VI. doi: 10.12816/0024690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alhowaish AK. Economic costs of diabetes in Saudi Arabia. J Family Community Med. 2013;20(1):1–7. doi: 10.4103/2230-8229.108174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chudasama YV, Khunti K, Gillies CL, et al. Healthy lifestyle and life expectancy in people with multimorbidity in the UK Biobank: a longitudinal cohort study. PLoS Med. 2020;17(9):e1003332. doi: 10.1371/journal.pmed.1003332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pender NJ, Murdaugh CL, Parsons MA. Health Promotion in Nursing Practice. 2006. [Google Scholar]
- 7.Cannata F, Vadala G, Russo F, Papalia R, Napoli N, Pozzilli P. Beneficial Effects of Physical Activity in Diabetic Patients. J Funct Morphol Kinesiol. 2020;5(3):70. doi: 10.3390/jfmk5030070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garedow AW, Jemaneh TM, Hailemariam AG, Tesfaye GT. Lifestyle modification and medication use among diabetes mellitus patients attending Jimma University Medical Center, Jimma zone, south west Ethiopia. Sci Rep. 2023;13(1):4956. doi: 10.1038/s41598-023-32145-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saghir SA, Alhariri AE, Alkubat SA, Almiamn AA, Aladaileh SH, Alyousefi NA. Factors associated with poor glycemic control among type-2 diabetes mellitus patients in Yemen. Tropical J Pharma Res. 2019;18(7):1539–1546. doi: 10.4314/tjpr.v18i7.26 [DOI] [Google Scholar]
- 10.Teich T, Zaharieva DP, Riddell MC. Advances in Exercise, Physical Activity, and Diabetes Mellitus. Diabetes Technol Ther. 2019;21(S1):S112–S122. doi: 10.1089/dia.2019.2509 [DOI] [PubMed] [Google Scholar]
- 11.Almansour FD, Allafi AR, Al-Haifi AR. Impact of nutritional knowledge on dietary behaviors of students in Kuwait University. Acta Biomed. 2020;91(4):e2020183. doi: 10.23750/abm.v91i4.8716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Almoraie NM, Shatwan IM, Althaiban MA, Hanbazaza MA, Wazzan HA, Aljefree NM. Associations between dietary intake, physical activity, and obesity among public school teachers in Jeddah, Saudi Arabia. Front Nutr. 2023;10:1081928. doi: 10.3389/fnut.2023.1081928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Albagawi B, Alkubati SA, Abdul-Ghani R. Levels and predictors of nurses’ knowledge about diabetes care and management: disparity between perceived and actual knowledge. BMC Nursing. 2023;22(1):342. doi: 10.1186/s12912-023-01504-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sami W, Ansari T, Butt NS, Hamid MRA. Effect of diet on type 2 diabetes mellitus: a review. Int J Health Sci. 2017;11(2):65–71. [PMC free article] [PubMed] [Google Scholar]
- 15.Costa BVL, Menezes MC, Oliveira CDL, et al. Does access to healthy food vary according to socioeconomic status and to food store type? An ecologic study. BMC Public Health. 2019;19(1):775. doi: 10.1186/s12889-019-6975-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Domosławska-żylińska K, Łopatek M, Krysińska-Pisarek M, Sugay L. Barriers to Adherence to Healthy Diet and Recommended Physical Activity Perceived by the Polish Population. J Clin Med. 2024;13(1):22. doi: 10.3390/jcm13010022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vilafranca Cartagena M, Tort-Nasarre G, Rubinat Arnaldo E. Barriers and Facilitators for Physical Activity in Adults with Type 2 Diabetes Mellitus: a Scoping Review. Int J Environ Res Public Health. 2021;18(10):5359. doi: 10.3390/ijerph18105359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akyirem S, Ekpor E. Experience of stigma among persons with type 2 diabetes in Africa: a systematic review. Int Health. 2023;16(3):231–239. doi: 10.1093/inthealth/ihad045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sendekie AK, Netere AK, Kasahun AE, Belachew EA. Medication adherence and its impact on glycemic control in type 2 diabetes mellitus patients with comorbidity: a multicenter cross-sectional study in Northwest Ethiopia. PLoS One. 2022;17(9):e0274971. doi: 10.1371/journal.pone.0274971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alqarni AS, Pasay-an E, Saguban R, et al. Relationship between the Health Literacy and Self-Medication Behavior of Primary Health Care Clientele in the Hail Region, Saudi Arabia: implications for Public Health. Eur J Invest Health Psychol Educ. 2023;13(6):1043–1057. doi: 10.3390/ejihpe13060080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Subramaniam M, Devi F, AshaRani PV, et al. Barriers and facilitators for adopting a healthy lifestyle in a multi-ethnic population: a qualitative study. PLoS One. 2022;17(11):e0277106. doi: 10.1371/journal.pone.0277106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoare E, Stavreski B, Jennings GL, Kingwell BA. Exploring Motivation and Barriers to Physical Activity among Active and Inactive Australian Adults. Sports. 2017;5(3):47. doi: 10.3390/sports5030047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Baho AK, Al-Naar A, Al-Shuaib H, Panicker JK, Gaber S. Levels of physical activity among Kuwaiti adults and perceived barriers. Open Public Health J. 2016;9(1):77–87. doi: 10.2174/1874944501609010077 [DOI] [Google Scholar]
- 24.Alkubati SA, Albagawi B, Alharbi TA, et al. Nursing internship students’ knowledge regarding the care and management of people with diabetes: a multicenter cross-sectional study. Nurse Education Today. 2023;129:105902. doi: 10.1016/j.nedt.2023.105902 [DOI] [PubMed] [Google Scholar]
- 25.Sullivan KM, Dean A, Soe MM. OpenEpi: a web-based epidemiologic and statistical calculator for public health. Public Health Rep. 2009;124(3):471–474. doi: 10.1177/003335490912400320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andajani-Sutjahjo S, Ball K, Warren N, Inglis V, Crawford D. Perceived personal, social and environmental barriers to weight maintenance among young women: a community survey. Int J Behav Nutr Phys Act. 2004;1(1):15. doi: 10.1186/1479-5868-1-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Musaiger AO, Al-Mannai M, Tayyem R, et al. Perceived barriers to healthy eating and physical activity among adolescents in seven Arab countries: a cross-cultural study. ScientificWorldJournal. 2013;2013(1):232164. doi: 10.1155/2013/232164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alshammari SA, AlDhayan AZ, Saad Al-Essa OM, et al. Challenges to lifestyle modification of chronic disease patients attending primary health care centers in Riyadh. J Family Med Prim Care. 2020;9(12):6186–6193. doi: 10.4103/jfmpc.jfmpc_1037_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Y, Liu M, Liu J. Association of Body Mass Index with Risk of Household Catastrophic Health Expenditure in China: a Population-Based Cohort Study. Nutrients. 2022;14(19):4014. doi: 10.3390/nu14194014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schmidt SK, Hemmestad L, MacDonald CS, Langberg H, Valentiner LS. Motivation and Barriers to Maintaining Lifestyle Changes in Patients with Type 2 Diabetes after an Intensive Lifestyle Intervention (The U-TURN Trial): a Longitudinal Qualitative Study. Int J Environ Res Public Health. 2020;17(20):7454. doi: 10.3390/ijerph17207454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ljubičić M, Sarić MM, Klarin I, et al. Motivation for health behaviour: a predictor of adherence to balanced and healthy food across different coastal Mediterranean countries. J Funct Foods. 2022;91:105018. doi: 10.1016/j.jff.2022.105018 [DOI] [Google Scholar]
- 32.Silva P, Araujo R, Lopes F, Ray S. Nutrition and Food Literacy: framing the Challenges to Health Communication. Nutrients. 2023;15(22):4708. doi: 10.3390/nu15224708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gomez-Velasco DV, Almeda-Valdes P, Martagon AJ, Galan-Ramirez GA, Aguilar-Salinas CA. Empowerment of patients with type 2 diabetes: current perspectives. Diabetes Metab Syndr Obes. 2019;12:1311–1321. doi: 10.2147/DMSO.S174910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leung SL, Barber JA, Burger A, Barnes RD. Factors associated with healthy and unhealthy workplace eating behaviours in individuals with overweight/obesity with and without binge eating disorder. Obes Sci Pract. 2018;4(2):109–118. doi: 10.1002/osp4.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gupta CC, Coates AM, Dorrian J, Banks S. The factors influencing the eating behaviour of shiftworkers: what, when, where and why. Ind Health. 2019;57(4):419–453. doi: 10.2486/indhealth.2018-0147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ducrot P, Mejean C, Aroumougame V, et al. Meal planning is associated with food variety, diet quality and body weight status in a large sample of French adults. Int J Behav Nutr Phys Act. 2017;14(1):12. doi: 10.1186/s12966-017-0461-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van der Heijden A, Te Molder H, Jager G, Mulder BC. Healthy eating beliefs and the meaning of food in populations with a low socioeconomic position: a scoping review. Appetite. 2021;161:105135. doi: 10.1016/j.appet.2021.105135 [DOI] [PubMed] [Google Scholar]
- 38.Goukens C, Klesse AK. Internal and external forces that prevent (vs. Facilitate) healthy eating: review and outlook within consumer Psychology. Curr Opin Psychol. 2022;46:101328. doi: 10.1016/j.copsyc.2022.101328 [DOI] [PubMed] [Google Scholar]
- 39.Kabir A, Miah S, Islam A. Factors influencing eating behavior and dietary intake among resident students in a public university in Bangladesh: a qualitative study. PLoS One. 2018;13(6):e0198801. doi: 10.1371/journal.pone.0198801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brand R, Cheval B. Theories to Explain Exercise Motivation and Physical Inactivity: ways of Expanding Our Current Theoretical Perspective. Front Psychol. 2019;10:1147. doi: 10.3389/fpsyg.2019.01147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rosenkranz SK, Mailey EL, Umansky E, Rosenkranz RR, Ablah E. Workplace Sedentary Behavior and Productivity: a Cross-Sectional Study. Int J Environ Res Public Health. 2020;17(18):6535. doi: 10.3390/ijerph17186535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Halling Ullberg O, Toivanen S, Tillander A, Balter K. Workplace health promotion to facilitate physical activity among office workers in Sweden. Front Public Health. 2023;11:1175977. doi: 10.3389/fpubh.2023.1175977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pröbstl-Haider U, Hödl C, Ginner K, Borgwardt F. Climate change: impacts on outdoor activities in the summer and shoulder seasons. J Outdoor Recreation Tourism. 2021;34:100344. doi: 10.1016/j.jort.2020.100344 [DOI] [Google Scholar]
- 44.Nikolajsen H, Sandal LF, Juhl CB, Troelsen J, Juul-Kristensen B. Barriers to, and Facilitators of, Exercising in Fitness Centres among Adults with and without Physical Disabilities: a Scoping Review. Int J Environ Res Public Health. 2021;18(14):7341. doi: 10.3390/ijerph18147341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kruszynska E, Poczta J. Difficulties Limiting Access to Sports and Recreational Facilities in the City in the Perceptions of Service Users. Sports and Recreational Infrastructure Management Policy-Poznan Case Study. Int J Environ Res Public Health. 2020;17(5):1768. doi: 10.3390/ijerph17051768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhong J, Liu W, Niu B, Lin X, Deng Y. Role of Built Environments on Physical Activity and Health Promotion: a Review and Policy Insights. Front Public Health. 2022;10:950348. doi: 10.3389/fpubh.2022.950348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zanjari N, Momtaz YA, Kamal SHM, Basakha M, Ahmadi S. The Influence of Providing and Receiving Social Support on Older Adults’ Well-being. Clin Pract Epidemiol Ment Health. 2022;18(1):e174501792112241. doi: 10.2174/17450179-v18-e2112241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yi H, Ng ST, Chang CM, Low CXE, Tan CS. Effects of neighborhood features on healthy aging in place: the composition and context of urban parks and traditional local coffeeshops in Singapore. BMC Geriatr. 2022;22(1):969. doi: 10.1186/s12877-022-03679-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yi H, Ng ST, Chang CM, Low CXE, Tan CS. Older Adults’ Understanding of Nutrition. Kompass Nutr Dietet. 2021;1(3):93–94. doi: 10.1159/000519342 [DOI] [Google Scholar]
- 50.Mattei J, Alfonso C. Strategies for Healthy Eating Promotion and Behavioral Change Perceived as Effective by Nutrition Professionals: a Mixed-Methods Study. Front Nutr. 2020;7:114. doi: 10.3389/fnut.2020.00114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mayes J, Castle EM, Greenwood J, Ormandy P, Howe PD, Greenwood SA. Cultural influences on physical activity and exercise beliefs in patients with chronic kidney disease: ‘The Culture-CKD Study’-a qualitative study. BMJ Open. 2022;12(1):e046950. doi: 10.1136/bmjopen-2020-046950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nemati M, Behmanesh F, Kheirkhah F, Geraili Z, Pasha H. Marital Commitment and Mental Health in Different Patterns of Mate Selection: a Comparison of Modern, Mixed, and Traditional Patterns. Iran J Psychiatry. 2022;17(4):418–427. doi: 10.18502/ijps.v17i4.10691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Arsh A, Afaq S, Carswell C, Coales K, Siddiqi N. Barriers & facilitators to physical activity in people with depression and type 2 diabetes mellitus in Pakistan: a qualitative study to explore perspectives of patient participants, carers and healthcare staff. Mental Health Phys Act. 2023;25:100542. doi: 10.1016/j.mhpa.2023.100542 [DOI] [Google Scholar]
- 54.Monin JK, Levy B, Chen B, et al. Husbands’ and Wives’ Physical Activity and Depressive Symptoms: longitudinal Findings from the Cardiovascular Health Study. Ann Behav Med. 2015;49(5):704–714. doi: 10.1007/s12160-015-9705-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee DW, Jang TW, Kim HR, Kang MY. The relationship between working hours and lifestyle behaviors: evidence from a population-based panel study in Korea. J Occup Health. 2021;63(1):e12280. doi: 10.1002/1348-9585.12280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Escoto KH, Laska MN, Larson N, Neumark-Sztainer D, Hannan PJ. Work hours and perceived time barriers to healthful eating among young adults. Am J Health Behav. 2012;36(6):786–796. doi: 10.5993/AJHB.36.6.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kari JT, Viinikainen J, Bockerman P, et al. Education leads to a more physically active lifestyle: evidence based on Mendelian randomization. Scand J Med Sci Sports. 2020;30(7):1194–1204. doi: 10.1111/sms.13653 [DOI] [PubMed] [Google Scholar]
- 58.Rawal LB, Smith BJ, Quach H, Renzaho AMN. Physical Activity among Adults with Low Socioeconomic Status Living in Industrialized Countries: a Meta-Ethnographic Approach to Understanding Socioecological Complexities. J Environ Public Health. 2020;2020:4283027. doi: 10.1155/2020/4283027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Zon SKR, Reijneveld SA, Mendes de Leon CF, Bultmann U. The impact of low education and poor health on unemployment varies by work life stage. Int J Public Health. 2017;62(9):997–1006. doi: 10.1007/s00038-017-0972-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.French SA, Tangney CC, Crane MM, Wang Y, Appelhans BM. Nutrition quality of food purchases varies by household income: the SHoPPER study. BMC Public Health. 2019;19(1):231. doi: 10.1186/s12889-019-6546-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sabur AM, Alsharief LA, Amer SA. Determinants of Healthy Food Consumption and the Effect of Saudi Food Related Policies on the Adult Saudi Population, a National Descriptive Assessment 2019. Curr Res in Nutr and Food Sci J. 2022;10(3):1058–1076. doi: 10.12944/CRNFSJ.10.3.21 [DOI] [Google Scholar]
- 62.Bantham A, Taverno Ross SE, Sebastiao E, Hall G. Overcoming barriers to physical activity in underserved populations. Prog Cardiovasc Dis. 2021;64:64–71. doi: 10.1016/j.pcad.2020.11.002 [DOI] [PubMed] [Google Scholar]
- 63.Kalra S, Jena BN, Yeravdekar R. Emotional and Psychological Needs of People with Diabetes. Ind J Endocrinol Metab. 2018;22(5):696–704. doi: 10.4103/ijem.IJEM_579_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bukhsh A, Goh BH, Zimbudzi E, et al. Type 2 Diabetes Patients’ Perspectives, Experiences, and Barriers Toward Diabetes-Related Self-Care: a Qualitative Study From Pakistan. Front Endocrinol. 2020;11:534873. doi: 10.3389/fendo.2020.534873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Alshammari B, Alkubati SA, Pasay-An E, et al. The influence of social support on sleep and fatigue level among patients receiving hemodialysis in Saudi Arabia: a cross-sectional correlational design. Front Psychol. 2023;14:1272500. doi: 10.3389/fpsyg.2023.1272500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fruh SM, Graves RJ, Hauff C, Williams SG, Hall HR. Weight Bias and Stigma: impact on Health. Nurs Clin North Am. 2021;56(4):479–493. doi: 10.1016/j.cnur.2021.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baillot A, Chenail S, Barros Polita N, et al. Physical activity motives, barriers, and preferences in people with obesity: a systematic review. PLoS One. 2021;16(6):e0253114. doi: 10.1371/journal.pone.0253114 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The corresponding author can be contacted for access to the data presented in this study.