Abstract
Background and Aims:
The conventional CE clamp technique may not effectively provide bag-mask ventilation (BMV) in the hands of inexperienced providers. Hence, we compared the efficacy of two-handed CE versus a hybrid technique.
Methods:
One hundred thirty-two American Society of Anesthesiologists (ASA) I–II adult patients were randomised into groups A and B. After induction of anaesthesia and neuromuscular blockade, Group A received BMV by using the double-handed CE technique. Group B received BMV by using dominant-hand CE and non-dominant-hand thenar eminence (TE) hybrid technique. The primary outcome was two minute (24 breaths) mean exhaled tidal volume. Secondary outcomes were the number of failed breaths and the comfortability level of airway providers using a 5-point Likert scale. Data were analysed using the Mann-Whitney U test, Student t-test, Chi-square test, and Fisher’s exact test.
Results:
The mean exhaled tidal volume and end-tidal carbon dioxide observed in Group A were significantly lower than in Group B (P = 0.001 and P = 0.001, respectively). The number of failed breaths and comfort level of both techniques were comparable in both groups (P = 0.310. and P = 0.584, respectively).
Conclusion:
The dominant-hand CE and non-dominant-hand TE techniques provide higher exhaled tidal volumes with comparable provider comfortability and may be considered an alternate BMV technique.
Keywords: Bag-mask ventilation, double-handed CE technique, end-tidal carbon dioxide, exhaled tidal volume, hybrid bag-mask ventilation technique
INTRODUCTION
Bag-mask ventilation (BMV) is a critical airway management skill that needs to be proficiently acquired by all airway providers. All healthcare providers, including new trainees, must be trained in the most efficient techniques of BMV as ineffective ventilation can result in irreversible hypoxia.[1]
Effective BMV necessitates proper patient positioning, a patent upper airway, and an adequate mask seal.[2] Various predictors of difficult BMV have been elucidated from many studies, such as edentulous patients, presence of beard, old age, body mass index (BMI) >26 kg/m2, history of snoring, and improperly sized mask.[3] These issues can be resolved by switching to a two-handed BMV technique with a properly fitting mask. Though a skilled provider may be able to adapt and overcome difficulties in BMV efficiently, a novice provider may face failure in BMV due to inadequate mastery of the essential components of the techniques of BMV.[4] Despite the popularity of the traditional EC clamp technique, significant failure rates have been reported due to air leaks that result in inadequate chest rise. Hence, many alternative techniques for efficient BMV have been investigated. The two-handed thenar eminence (TE) technique is one such alternate technique that involves downward pressure on the mask with the thenar eminence of the airway provider to create an air-tight seal on the face of the patient, while the four fingers of each hand pull the jaw upwards towards the mask.[5] The TE technique enhances airway patency due to all fingers’ advancement of the lower jaw, with an accompanying lack of compression on the submandibular tissue.[5,6] Various studies have compared two-handed CE techniques with two-handed TE techniques of BMV in novices and experienced airway providers, mainly on manikins, with conflicting results.[2,5,6]
The primary objective of this study was to compare the 2-minute (24 breaths) mean exhaled tidal volume between the two-handed CE versus the dominant-hand CE with the non-dominant-hand TE mask-holding technique on human subjects without difficult bag-mask ventilation predictors. The secondary objective was to compare the number of failed breaths reflected by no exhaled tidal volume amongst both methods. The comfort level of airway providers using both techniques using a 5-point Likert scale was also evaluated as a secondary outcome. We hypothesised that combining the traditional CE technique with a novel hybrid technique, which amalgamates the CE technique with the dominant hand and the TE technique with the non-dominant hand, might result in a higher degree of effectiveness and comfortability for relatively novice airway providers.
METHODS
This randomised controlled study was conducted after approval by the institutional ethics committee (vide approval Number: BFUHS/2K21p-TH, dated 22-2-2021) and registered in the Clinical Trials Registry–India (vide registration number CTRI/2021/09/036598, accessible at www:/ctri.nic.in). The study duration was July 2021 to December 2021. The procedures followed were in accordance with the Helinski Declaration of 2003 and Good Clinical Practice guidelines. The study was conducted on patients scheduled to undergo general anaesthesia (GA) for elective surgical procedures. In these recruited patients, relatively novice airway providers (defined as those with less than 3 years of experience in BMV and other airway management procedures) performed BMV.[7] Written informed consent was obtained from the patients and airway providers for participation in the study and use of data for research and educational purposes.
The patients included were adult patients (18–55 years of age), American Society of Anesthesiologists (ASA) physical status I and II, with a Modified Mallampatti Score (MMPS) I and II, and the absence of any of the predictors of difficult mask ventilation (DMV) presenting for elective surgeries under GA. Patients who had a full stomach requiring rapid sequence intubation, those with predicted difficult airway including DMV [age >55 years, BMI >30 kg/m2, history of snoring, neck radiation, facial asymmetry, presence of beard, MMPS III and IV, upper lip bite test 2 and 3, edentulous, thyromental distance <6 cm, neck circumference >40/42 cm (female/male)],[8] pregnant, and haemodynamically unstable were excluded from the study.
Patients were randomly assigned equally into either of the two groups, A or B, by computer-generated randomised codes, and allocation concealment was ensured using sealed, sequentially numbered envelopes, which were opened by an anaesthesiologist who was not a part of the study. Group A comprised patients who underwent BMV with a two-handed CE mask ventilation technique for 2 minutes (24 breaths). Group B consisted of the patients who underwent BMV with the two-handed dominant-hand (CE) and non-dominant-hand (TE) technique of mask ventilation for 2 minutes (24 breaths). We could not blind the airway providers performing the method. However, bias was reduced by recording variables, especially exhaled tidal volumes from the anaesthesia workstation ventilator interface, by an unbiased observer not part of the study protocol.
An experienced anaesthesiologist (airway provider with more than 3 years of experience in BMV and airway management)[7] conducted a brief training session for all assigned novice airway providers before enrolment in the study. This comprised pictures demonstrating the techniques [Figure 1], video demonstration, and hands-on skill performance on manikins (Airway management trainer, Laerdal Co. Ltd.) for 30 minutes.
Figure 1.
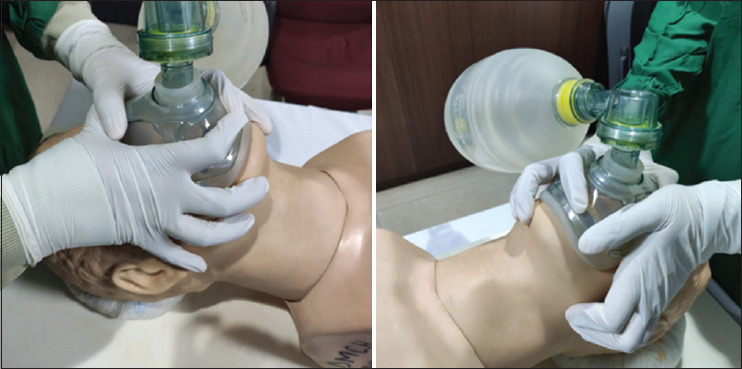
Two-handed CE technique of BMV and two-handed dominant-hand CE with non-dominant-hand TE technique
Two-handed CE technique of BMV: In this, the thumb and the index finger of both hands formed the shape of the letter ‘C’ around the mask, attempting to secure the mask tightly around the patient’s mouth and nose, and the other three fingers formed the letter ‘E’ on the inferior portion of the mandible where the little finger provided jaw thrust, and middle and ring finger rested on the rim of the mandible.[5,9]
Two-handed dominant-hand CE with non-dominant-hand TE technique: In this technique, the dominant hand was used to perform the CE technique and the non-dominant hand was used to perform the TE technique (in which downward pressure on the mask was applied with the thenar eminence while the four fingers of each hand pulled the jaw upwards towards the mask).[5]
All patients enroled in the study underwent routine, thorough pre-anaesthesia check-ups comprising a detailed history, a focused airway history, a general physical examination, and a focused airway examination. Relevant investigations were sent and reviewed. Demographic information and preoperative variables, including age, gender, height, weight, BMI, and ASA physical status, were recorded.
Monitors including pulse oximeter, non-invasive blood pressure, and 5-lead electrocardiography (ECG) were attached, and continuous monitoring of heart rate, ECG rhythm, and oxygen saturation (SpO2) was done. An experienced consultant anaesthesiologist who did not participate in the study was assigned to manage the anaesthesia for the case. After securing an intravenous (IV) cannula, an IV midazolam 0.05 mg/kg was given as premedication. An appropriately sized, well-fitting transparent face mask was used for each patient. Pre-oxygenation with 100% oxygen at a flow rate of 10 L/min was done for 3 minutes. General anaesthesia was induced with IV propofol 2–3 mg/kg, IV lidocaine 1.5 mg/kg, and IV fentanyl 1–2 μg/kg. Neuromuscular (NM) blockade was established with IV atracurium 0.5 mg/kg. The anaesthesia machine was preset in pressure control mode (PCV) to deliver 12 breaths/min, peak inspiratory pressure of 15 cm of H2O, and an inspiratory to expiratory ratio (I: E) ratio of 1:2, with no positive end-expiratory pressure. The anaesthesiologist assigned to the case performed BMV to confirm adequate BMV for an initial 1 minute before handing over the mask to the designated airway provider to ensure patient safety. The patient was excluded from the study if this experienced consultant anaesthesiologist encountered inadequate BMV [defined as exhaled tidal volume (VTe) less than 4 mL/kg of predicted body weight or less than 150 mL per breath with clinical signs such as inadequate chest rise, no fogging in the mask, no positive tracing of end-tidal carbon dioxide (EtCO2), and lack of measurable VTe on anaesthesia ventilator display].[9,10]
Each airway provider performed the assigned technique for 2 minutes (24 breaths) [Figure 1]. An observer who was neither part nor aware of the study recorded all data manually from the anaesthesia machine ventilator display. The protocol was to be aborted in case of any observed decrease in SpO2 to less than 94% or the event of any haemodynamic instability. In that case, the consultant anaesthesiologist was requested to intervene and manage the patient. The data of zero was planned to be entered for the remaining breaths of the patient. In case of complex or failed bag ventilation, the airway adjuncts and laryngeal mask airway were kept as rescue measures. After the completion of the study, the consultant anaesthesiologist assigned to the case continued with further management of the patient as per standard protocol.
The exhaled tidal volume (VTe), oxygen saturation (SpO2), and end-tidal carbon dioxide (EtCO2) for each breath during bag-mask ventilation were recorded. The primary outcome of our study was the 2-minute (24 breaths) mean exhaled tidal volume between both mask-holding techniques, while the number of failed breaths as reflected by no exhaled tidal volume recorded by the anaesthesia machine display and the comfortability of both methods to airway providers were analysed as secondary outcomes. The comfortability of the technique was assessed using a 5-point Likert scale by asking the airway providers to grade the technique as very comfortable, comfortable, neutral, uncomfortable, and very uncomfortable.
The sample size was calculated based on the primary objective, that is, the mean difference in VTe using the study results of Gerstein et al.,[5] where the mean VTe of the TE grip group was 379 mL. In comparison, the mean VTe of the EC grip group was 269 mL, with a mean difference (MD) of 110 mL. Assuming an α-error (significance) of 0.05 and power (1 - β) of 90%, the adequate sample size based on 2-minute (24 breaths) mean VTe came out to be 60 in each group. This number was increased to 66 per group, allowing for a predicted 10% dropouts from treatment. A post-hoc power analysis also reflected 99% power calculated using Gstar power software. Statistical Package for the Social Science (SPSS) 21 version (SPSS Inc., Chicago, IL, USA) statistical program for Microsoft Windows was used for statistical calculations. For statistical analysis, data were described in terms of range, mean [(standard deviation (SD)], frequencies (number of cases), and relative frequencies (percentages) as appropriate. A Kolmogorov-Smirnov test was used to determine whether the data were normally distributed (normal distributed data were vital parameters; non-normally distributed data were VTe and EtCO2). A comparison of quantitative variables (VTe and EtCO2) between the study groups was analysed using the Student t-test and Mann-Whitney U test for independent samples of parametric (vital parameters) and non-parametric data (VTe and EtCO2), respectively. For comparing categorical data (characteristics of airway providers such as gender, speciality, and experience in BMV) and number of failed breaths, the Chi-square (χ2) test was performed, and Fisher’s exact test was used when the expected frequency was less than 5. A probability value (P value) was considered statistically significant if it was less than 0.05.
RESULTS
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram [Figure 2] depicts the flow of 132 enroled patients. Demographic data of all patients in groups A and B were comparable in age, gender, ASA physical status, weight, height, and BMI (P > 0.05). We recruited a total of 66 relatively novice airway providers [46 interns with experience of 10 months into internship after graduating and 20 junior residents (of which 15 were first-year residents with knowledge of less than 1 year and five third-year residents with an understanding of 2 years in airway management procedures). There was no significant difference in the age and level of experience between the two groups [Table 1].
Figure 2.
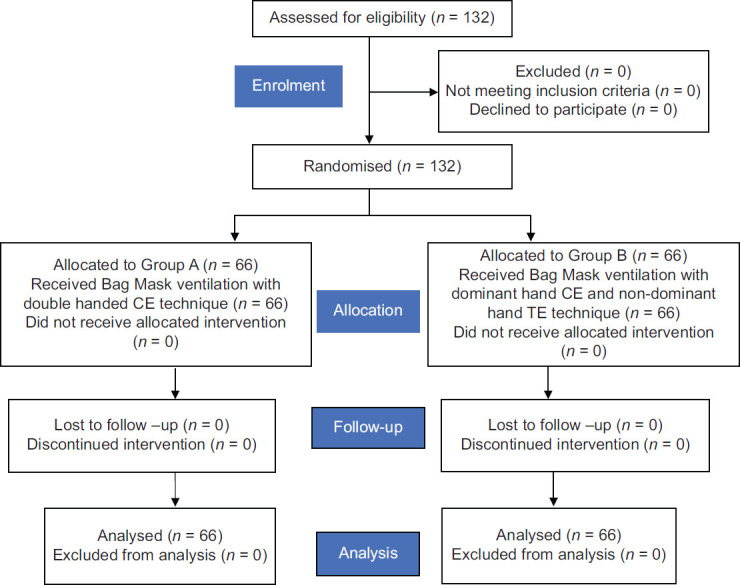
Consolidated Standards of Reporting Trials (CONSORT) flow diagram
Table 1.
Comparison of characteristics of airway providers in both groups
| Characteristics | Group A (n=66) | Group B (n=66) | P |
|---|---|---|---|
| Gender: Male/Female | 32/34 | 32/34 | 1 |
| Speciality and level of training: Intern/JR1/JR3 | 46/15/5 | 46/15/5 | 1 |
| Experience in BMV: 10 months/1 year/2 years | 46/15/5 | 46/15/5 | 1 |
Data expressed as number (n). JR 1=Junior resident first year, JR3=Junior resident third year, BMV=Bag-Mask Ventilation
The mean VTe in Group A was 377.51 (SD: 82.79) mL versus 476.71 (SD: 121.85) mL in group B [MD: 99.2 mL (95% CI: 63.34, 135.09). The mean EtCO2 in Group A was 28.83 (SD: 1.83) mmHg, which was significantly lower than in Group B with a value of 30.42 (SD: 2.59) mmHg (P = 0.001) [MD: 1.58; 95% CI: 0.80, 2.35) mmHg [Table 2].
Table 2.
Comparison of mean exhaled tidal volume and mean EtCO2 in both groups
| Parameters | Group A n=66 Mean (SD) | Group B n=66 Mean (SD) | Mean difference (95% CI) | P |
|---|---|---|---|---|
| Exhaled tidal volume (ml) | 377.51 (82.79) | 476.71 (121.85) | 99.21 (63.34, 135.09) | 0.001 |
| EtCO2 (mmHg) | 28.83 (1.83) | 30.42 (2.59) | 1.576 (0.80, 2.35) | 0.001 |
CI=confidence interval, SD=standard deviation, n=number, EtCO2=End-tidal carbon dioxide
The BMV in Group A was comfortable to 51.5% of airway providers and very comfortable to 48.5%. In contrast, the BMV in Group B was very comfortable to 50% of providers and comfortable to 48.5%, and one of the airway providers found this technique uncomfortable (P = 0.584). None of the providers found any techniques to be neutral or very uncomfortable. Four patients (1 in Group A and 3 in Group B) experienced two failed breaths each. The total number of failed breaths was 8 (6 in Group B and 2 in Group A) (P = 0.31). However, during the study period, we did not encounter any drop in oxygen saturation below 94% or the need to use airway adjuncts amongst all our recruited patients.
DISCUSSION
We observed that the hybrid technique resulted in significantly higher tidal volume delivery with comparable comfortability scores to the traditional CE technique. This finding was further corroborated by higher EtCO2 levels observed in Group B, implying superior ventilation achieved using the dominant-hand CE and non-dominant-hand TE technique of BMV. This validates our hypothesis that a hybrid method of BMV can be considered notably better than the traditional CE clamp technique in terms of efficiency of delivering adequate tidal volume breaths, especially in the hands of relatively novice airway providers.
Our results corroborate the findings of a randomised crossover comparison study conducted by Gerstein et al.[5] with 60 novice clinicians (medics and paramedics) to perform two two-handed mask grip techniques, TE and EC clamp technique, in a crossover manner on the same patient undergoing GA for 1 minute (12 breaths). TE grip resulted in greater expired tidal volume (379 mL versus 269 mL) when the TE-EC sequence was used for BMV primarily by novice providers. The relatively higher tidal volumes observed in our study could be ascribed to using NM blocking agents that assisted us in overcoming poor chest wall compliance and ventilator desynchrony. Various studies have validated these findings of improved ventilation using NM blockade.[10,11]
The results of our study are also in accordance with a manikin study conducted by Soleimanpour et al.[7] in which they compared the efficacy of the four techniques (EC, thenar eminence, thenar eminence (dominant hand)–EC (non-dominant hand), and thenar eminence (non-dominant hand)–EC (dominant hand)) of mask ventilation amongst two groups of experienced and novice staff. The quality of ventilation adequacy was, however, subjective as it was assessed by observed chest expansion by blinded observers.
The hybrid technique used in our study provides effective jaw thrust displacing the mandible anteriorly, thus improving the patency of the airway whilst the CE grip ensures an air-tight seal at the mask-face interface. Various studies have postulated that positive pressure is generated by the TE technique, which pushes the submandibular tissue anteriorly, relieving upper airway obstruction and thus providing higher tidal volumes at lower pressures.[6,12]
We compared the comfortability levels of both techniques for airway providers. Our results of the comfortability level were in contrast to the study conducted by Althunayyan et al.[2] where the CE technique was superior to the VE technique in comfortability. However, their study participants were experienced respiratory therapists who performed BMV on simulated models, which explains the results using the traditional CE technique.
The number of failed breaths was compared as a secondary outcome, and we observed that this difference could not attain statistical or clinical significance in contrast with the study by Gerstein et al.[5] The fewer failed breaths in our study could be secondary to including patients without DMV predictors. Furthermore, our study was not powered adequately to detect differences for this secondary outcome.
Our study has limitations that may be addressed in future investigations of these techniques. Our study could not be blinded; a crossover design might have helped prevent this concern. Leak fraction was not measured, and a correlation of mean exhaled tidal volume with leak fraction would have further validated our findings. In addition, the results cannot be extrapolated to emergency scenarios or settings necessitating prolonged bag-mask ventilation in patients with DMV. Nevertheless, our study on human subjects does pave the way for evaluating alternative hybrid bag-mask ventilation techniques.
CONCLUSION
When used on human subjects by relatively inexperienced airway providers, the hybrid technique (dominant-hand CE and non-dominant-hand TE) resulted in higher mean tidal volume than the traditional CE technique.
Study data availability
De-identified data may be requested with reasonable justification from the authors (email to the corresponding author) and shall be shared after approval as per the authors’ Institution policy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chi JH, Knudson MM, Vassar MJ, McCarthy MC, Shapiro MB, Mallet S, et al. Prehospital hypoxia affects outcome in patients with traumatic brain injury: A prospective multicentre study. J Trauma. 2006;61:1134–41. doi: 10.1097/01.ta.0000196644.64653.d8. [DOI] [PubMed] [Google Scholar]
- 2.Althunayyan SM, Alotaibi RN, Aljanoubi MA, Alharthi MZ, Mubarak AM, Al-Otaibi AM. Comparison of the effectiveness and comfort level of two commonly used mask ventilation techniques in a model. Respir Care. 2021;66:460–5. doi: 10.4187/respcare.07949. [DOI] [PubMed] [Google Scholar]
- 3.Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–36. doi: 10.1097/00000542-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Umesh G, Krishna R, Chaudhuri S, Tim TJ, Shwethapriya R. E-O technique is superior to E-C technique in manikins during single-person bag mask ventilation performed by novices. J Clin Monit Comput. 2014;28:269–73. doi: 10.1007/s10877-013-9531-9. [DOI] [PubMed] [Google Scholar]
- 5.Gerstein NS, Carey MC, Braude DA, Tawil I, Peterson TR, Deriy L, et al. Efficacy of facemask ventilation techniques in novice providers. J Clin Anaesth. 2013;25:193–7. doi: 10.1016/j.jclinane.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 6.Fei M, Blair JL, Rice MJ, Edwards DA, Liang Y, Pilla MA, et al. Comparison of effectiveness of two commonly used two-handed mask ventilation techniques on unconscious apnoeic obese adults. Br J Anaesth. 2017;118:618–24. doi: 10.1093/bja/aex035. [DOI] [PubMed] [Google Scholar]
- 7.Soleimanpour M, Rahmani F, Ala A, Bagi HR, Mahmoodpoor A, Golzari SE, et al. Comparison of four techniques on the facility of two-hand Bag-valve-mask (BVM) ventilation: EC, Thenar Eminence, Thenar Eminence (Dominant hand)-EC (non-dominant hand) and Thenar Eminence (non-dominant hand)–EC (dominant hand) J Cardiovasc Thorac Res. 2016;8:147–51. doi: 10.15171/jcvtr.2016.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar R, Kumar S, Misra A, Kumar NG, Gupta A, Kumar P, et al. A new approach to airway assessment—”Line of Sight” and more. Recommendations of the Task Force of Airway Management Foundation (AMF) J Anaesthesiol Clin Pharmacol. 2020;36:303–15. doi: 10.4103/joacp.JOACP_236_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Umesh G, Gotur GV, Rao AK, Joseph TT. EO technique provides 20 better mask seal than the EC clamp technique during single handed mask holding by novices in anaesthetised and paralysed patients. Indian J Anaesth. 2018;62:780–5. doi: 10.4103/ija.IJA_228_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joffe AM, Hetzel S, Liew EC. A two-handed jaw-thrust technique is superior to the one-handed “EC-clamp” technique for mask ventilation in the apneic unconscious person. Anesthesiology. 2010;113:873–9. doi: 10.1097/ALN.0b013e3181ec6414. [DOI] [PubMed] [Google Scholar]
- 11.Ikeda A, Isono S, Sato Y, Yogo H, Sato J, Ishikawa T, et al. Effects of muscle relaxants on mask ventilation in anesthetized persons with normal upper airway anatomy. Anesthesiology. 2012;117:487–93. doi: 10.1097/ALN.0b013e3182668670. [DOI] [PubMed] [Google Scholar]
- 12.Sato Y, Ikeda A, Ishikawa T, Isono S. How can we improve mask ventilation in patients with obstructive sleep apnea during anesthesia induction? J Anesth. 2013;27:152–6. doi: 10.1007/s00540-012-1520-5. [DOI] [PubMed] [Google Scholar]


