Abstract
Background and Aims:
Three phases (dissection, anhepatic, and neohepatic) exist for propofol pharmacokinetics during liver transplantation (LT), resulting in varying cardiac output, volume of distribution, and drug metabolism. The primary objective was to compare the mean target concentration of propofol required to maintain the bispectral index (BIS) between 40 and 60 during three phases of LT by using a target-controlled infusion of total intravenous anaesthesia (TCI-TIVA).
Methods:
In this prospective, observational study, 20 adult patients diagnosed with chronic liver disease scheduled for live-donor LT were included. After anaesthesia induction and tracheal intubation, BIS-guided propofol infusion was started using TCI-TIVA with target plasma concentration (TPC) set initially at 2.5 μg/mL in all patients using the Marsh model. The TPC was decreased or increased by 0.2 μg/mL whenever the BIS values were persistently below 40 or above 60 for 15 minutes. Data were analysed using ANOVA and repeated measure ANOVA, followed by a post-hoc test.
Results:
The mean TPC was significantly higher during dissection [2.12 (Standard deviation (SD): 0.63 μg/mL)] as compared to anhepatic and neohepatic phases [1.29 (SD: 0.65) μg/mL and 1.35 (SD: 0.54) μg/mL], respectively (P < 0.001). A significant difference was observed between dissection and anhepatic (mean difference: −0.87 (95% confidence interval (CI): −0.98, −0.75) or dissection and neohepatic phase (mean difference: −0.77 (95% CI: −1.02, −0.53). The propofol dose was significantly higher in dissection compared to the anhepatic and neohepatic phases (P < 0.001).
Conclusion:
The propofol’s mean TPC when using TCI-TIVA decreased in the anhepatic and neohepatic phases to 61% and 63.7% of the dissection phase, respectively.
Keywords: Cardiac output, entropy, haemodynamic, liver cirrhosis, liver transplantation, pharmacokinetics, propofol, target control infusion, target plasma concentration, total intravenous anaesthesia
INTRODUCTION
Propofol has been successfully used in liver transplants for induction and maintenance of anaesthesia. It begets more haemodynamic stability than inhalational anaesthetics.[1] Due to its anti-inflammatory properties and free radicle scavenging properties, propofol protects from ischaemia-reperfusion injury, namely hepatoprotection, cardioprotection, renoprotection, and neuroprotection.[2]
Liver transplantation consists of three phases, namely dissection, anhepatic and neohepatic phases, which present three different pharmacokinetic situations for propofol. During the dissection phase of liver transplantation, acute haemorrhage can result in elevated plasma concentrations of propofol compared to a euvolemic state at the same dosage, necessitating a reduction in propofol dosage.[3] Moreover, cross-clamping of the inferior vena cava and portal vein leads to decreased venous return, reducing cardiac output and hepatic blood flow. The diminished hepatic perfusion impairs propofol clearance, thereby reducing its dosage requirements.[1] However, fluid and blood resuscitation to address the effects of haemorrhage and compromised venous return may necessitate an increased dose of propofol during this phase. In the anhepatic phase, a significant reduction in propofol clearance occurs due to the absence of hepatic function following liver removal.[4] This reduction necessitates careful adjustment of propofol dosing. Upon the implantation of a new liver during the neohepatic phase, hepatic function begins to be restored almost immediately, enhancing propofol clearance. This restoration implies that propofol dosing must be adjusted to account for the increased clearance capacity of the newly implanted liver. Thus, optimal propofol dosing strategies for each phase are important to improve anaesthetic management and patient outcomes.
In patients with cirrhosis, the pharmacokinetics of propofol are further complicated by factors such as ascites, endotoxemia, hypoalbuminemia, and haemodynamic disturbances. Evidence suggests that chronic liver disease (CLD) patients, particularly those with a Child-Turcotte-Pugh score (CTP) B or C, may experience drug overshoot when using a constant target-controlled infusion (TCI) concentration of propofol.[5]
Given the existing lack of studies on propofol dosing across the various phases of living donor liver transplantation, we hypothesise that the target concentration of propofol would be different in the dissection, anhepatic, and neohepatic phases of the transplant. The primary objective of our study was to compare the mean target concentration of propofol (TPC) required to maintain the BIS between 40-60 during three phases of live donor liver transplantation using a target-controlled infusion of total intravenous anaesthesia (TCI-TIVA). The secondary objective was to study the effect of increasing the model for end-stage liver disease (MELD) score on the propofol dose requirement during liver transplantation.
METHODS
In this prospective observational study, institutional ethics committee approval (vide approval number IEC/2022/94/MA10 dated 09-06-2022) was obtained, and the trial was registered with the Clinical Trials Registry-India (vide registration number CTRI /2023/01/049206, accessible at www.ctri.nic.in). The study was conducted over six months in accordance with the Helsinki Declaration (2013) and Good Clinical Practice (GCP) guidelines. Written informed consent was obtained from patients to participate in the study and use patient data for research and educational purposes.
Twenty CLD patients, aged between 18 and 65 years, undergoing elective live donor liver transplantation, were included in the study. A single surgeon and anaesthesia team performed the surgery with no veno-venous bypass intraoperatively. A detailed pre-anaesthetic checkup was done one day before surgery, and patients’ denying consent, allergy to egg or propofol or known psychiatric or neurologic disease, chronic kidney disease, previous spontaneous bacterial peritonitis, portal thrombosis, deviation from the protocol of anaesthesia, and hepatic encephalopathy were excluded from the study. None of the patients were premedicated in the preoperative period.
In the operation theatre, after attaching American Society of Anesthesiologists standard monitors viz. electrocardiogram, non-invasive blood pressure, pulse oximetry, a 20-G cannula was secured for propofol infusion. After noting the initial BIS (Aspect Medical System, Inc., Norwood, MA) value, general anaesthesia using TIVA was administered with 1.5–2 mg/kg propofol, 2 μg/kg fentanyl and 0.5 mg/kg atracurium, and the trachea was intubated. After 10–15 minutes of induction and when the BIS regained to more than 60, propofol via TCI pump (B Braun Perfusor® Space Infusion System, Melsungen, Germany) @ 2.5 μg/mL using Marsh Model with TPC set initially at 2.5 μg/mL was initiated in all patients. The TPC was decreased or increased by 0.2 μg/mL whenever the BIS values were persistently below 40 or above 60 for 15 minutes.
Under all aseptic precautions, the left radial artery, right femoral artery, and right internal jugular vein were canulated (8.5 F, Multicath 4, Vygon Ref 158.167 and 7 F sheath [Avanti +, Cordis Corporation Ref 504-610X.08, 10Fr]). Core body temperature was measured with an oesophageal probe, and to prevent hypothermia, a warming gel pad, a warming blanket, and warm fluid and blood were used.
Propofol via the TCI pump was continued throughout surgery to maintain the BIS value between 40 and 60 to ensure adequate depth of anaesthesia. The BIS value was monitored every 15 minutes. The propofol TPC was decreased or increased by 0.2 μg/mL whenever the BIS value persistently remained below 40 or increased above 60, respectively. Analgesia was provided with an intravenous infusion of fentanyl 2 μg/kg/h, and the neuromuscular blockade was maintained with an intravenous infusion of atracurium at 0.5 mg/kg/h throughout the surgery. Fluids were administered @ 10 mL/kg/h during surgery, and a bolus of 250–500 mL was given whenever blood pressure fell below the mean arterial pressure of 55 mmHg. Vasopressors (norepinephrine/vasopressin) were initiated when arterial hypotension (mean arterial pressure below 55 mmHg) persisted despite adequate fluid and blood replacement. Arterial blood gas was recorded 2 hourly. Haemoglobin value was maintained between 7 and 9 g/dL. During surgery, thromboelastography-guided platelets/fresh frozen plasma/cryoprecipitate were transfused whenever the surgeon complained of clinically significant ooze in the surgical field. All patients were overnight shifted to the intensive care unit for elective ventilation and extubated the following day.
Demographic data (age, weight, and body mass index), MELD, CTP score, and decompensations (ascites, hepatic hydrothorax, oesophageal varices, hepatorenal syndrome, hepatopulmonary syndrome) were noted preoperatively a day before surgery. TCI concentration of propofol, BIS, vasopressor dose (noradrenaline and vasopressin), haemodynamic parameters (mean arterial pressure, heart rate, stroke volume variation, and cardiac output using flowtrac), and temperature using an oesophageal probe were recorded every 15 minutes intraoperatively. The total propofol consumed in each phase was recorded at the end of each phase from the reading of the TCI pump. All patients were interviewed about intraoperative recall on the second or third day after extubation using the modified Brice interview. The study’s primary outcome was to compare the mean TPC of propofol required to maintain BIS between 40 and 60 during each of the three phases of liver transplantation. The study’s secondary outcome was to compare the total propofol requirement in each of the three phases of liver transplantation in patients of MELD 15–20, 21–25, and more than 25.
Two studies were reported by Tremelot et al. and Restoux et al. in 8 and 13 patients, respectively, in patients undergoing orthotopic liver transplantation using BIS-guided propofol infusion via a TCI pump (closed-loop anaesthesia in a study by Restoux et al.) in the European population.[6,7] Due to the scarcity of similar studies in live donor liver transplantation (orthotopic liver transplantation in the earlier two studies) and lack of data in the Asian population, we did a pilot study of 20 patients of CLD from January 2023 to May 2023 in the Asian population. In addition, Tremelot et al. did not note the propofol requirement in the neohepatic phase.[7]
The data entry was done in the Microsoft Excel spreadsheet. Statistical Package for the Social Sciences (SPSS) statistics software version 25.0 (Armonk, NY: IBM Corp, USA) was used for statistical analysis. The categorical variables, namely aetiology of liver disease, gender, CTP score, and MELD score, were presented as numbers and percentages (%), while the continuous variables, namely age, weight, GRWR, duration of each phase, mean arterial pressure, heart rate, cardiac output, temperature, BIS, noradrenaline, vasopressin, TPC of propofol, and propofol requirement in each phase, were presented as mean [standard deviation (SD) value. The quantitative variables (TPC and propofol requirement) were compared using ANOVA, and repeated measure ANOVA was used to compare dissection, anhepatic, and neohepatic phases, followed by a post-hoc test (Bonferroni correction). For statistical significance, a P value of less than 0.05 was considered statistically significant.
RESULTS
Twenty patients were enroled prospectively in the study [Figure 1]. The demographics are presented in Table 1. The mean age of study subjects was 45.15 (SD: 9.9) years, with the majority being male (93%).
Figure 1.
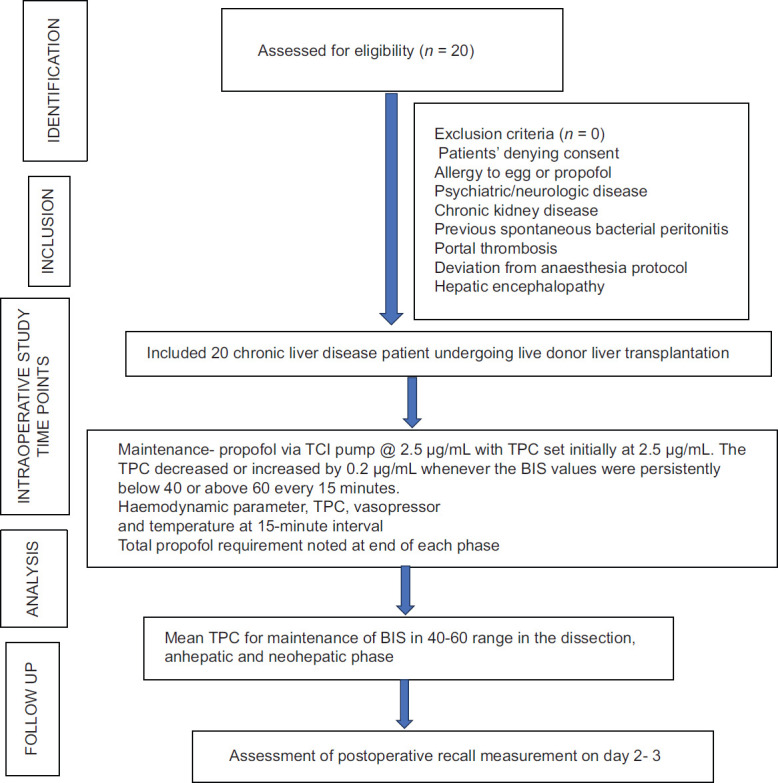
Patient flow diagram. TCI = Target controlled infusion, TPC = Target plasma
Table 1.
Demographic parameters of study subjects
| Parameter | Values |
|---|---|
| Age (years) | 45.15 (9.9) |
| Gender (Female/Male) | 1/19 |
| Weight (kg) | 67.88 (11.38) |
| Aetiology of Chronic Liver Disease | |
| Autoimmune hepatitis | 3 |
| Budd-Chiari syndrome | 1 |
| Cryptogenic | 3 |
| Alcohol | 5 |
| Hepatitis B Virus | 4 |
| Non-alcoholic steatohepatitis | 3 |
| Hepatocellular carcinoma | 1 |
| Model for End-stage Liver Disease Score (MELD) - 15–20/21–25/>26 | 4/10/6 |
| Child Turcotte Pugh (CTP) score- A/B/C | 3/4/13 |
| Graft versus Weight Ratio (GRWR) | 0.94 (0.14) |
Data expressed as mean (standard deviation) or numbers
The mean value of the MELD score of the study subjects was 23.6 (SD: 5.54). Haemodynamic parameters were maintained within normal limits during the three phases of liver transplant surgery [Table 2]. The mean TPC were significantly different (P < 0.001) in the three phases of liver transplantation [Table 2]. On further comparison by the Bonferroni test, the mean TPC differed significantly between the anhepatic and dissection phase (P < 0.001) and the dissection and neohepatic phase (P < 0.001). Still, it was comparable in the anhepatic and neohepatic phases (P = 1).
Table 2.
Intraoperative parameters and dose of propofol during the three phases of Liver Transplantation
| Dissection Phase Mean (SD) | Anhepatic Phase Mean (SD) | Neohepatic Phase Mean (SD) | Mean difference (95% Confidence Interval) [P] |
|||
|---|---|---|---|---|---|---|
| Dissection vs anhepatic phase | Dissection vs neohepatic phase | Anhepatic phase vs neohepatic phase | ||||
| Duration of phase (min) | 303 (59.33) | 116.25 (44.3) | 258 (38.5) | 186.75 (147.2, 226.29) 0.009 | 45 (12.38, 77.61) <0.001 | −141.75 (−172.17, −111.32) <0.000 |
| Mean arterial pressure (mmHg) | 78.13 (7.69) | 72.83 (8.23) | 73.65 (4.45) | −5.29 (−8.49, −2.09) 0.001 | −4.47 (−7.68, −1.26) 0.006 | −0.82 (−4.26, 2.62) 0.641 |
| Heart rate (per min) | 86.39 (15.9) | 102.67 (16.69) | 99.01 (15.55) | 15.47 (11.5, 19.6) <0.001 | 11.86 5.68, 18) <0.001 | 3.60 (−1.69, 8.91) 0.183 |
| Cardiac output (L/min) | 8.43 (1.99) | 8.43 (2.64) | 8.56 (2.16) | 0.02 (−1.0, −1.1) 0.968 | 0.14 (−0.49, 0.78) 0.657 | −0.12 (−1, 0.75) 0.784 |
| Temperature (°C) | 36.71 (0.5) | 36.26 (0.44) | 36.55 (0.36) | 0.40 (0.08, 0.72) 0.012 | 0.69 (0.39, 1.00) <0.001 | −0.29 (−0.45, −0.12) 0.001 |
| BIS | 45.64 (3.78) | 42.29 (3.04) | 48.95 (4.02) | −3.38 (−5.54, −1.22) 0.002 | 3.27 (0.99, 5.55) 0.002 | −6.6 (−8.42, −4.89) <0.001 |
| Noradrenaline (μg/kg/min) | 0.05 (0.04) | 0.14 (0.08) | 0.15 (0.08) | 0.09 (0.06, 0.11) <0.001 | 0.10 (0.06, 0.12) <0.001 | −0.09 (−0.02, 0.02) <0.00 |
| Vasopressin (unit/h) | 0.37 (0.22) | 1.11 (0.66) | 0.96 (0.71) | 0.74 (0.50, 0.98) <0.001 | 0.58 (0.304, 0.87) <0.001 | 0.15 (−0.109, 0.421) 0.250 |
| Mean target plasma concentration of propofol (μg/mL) | 2.12 (0.63) | 1.29 (0.65) | 1.35 (0.54) | −0.87−0.98, −0.75 <0.000 | −0.77−1.02, −0.53 <0.000 | −0.09−0.29, 0.09 0.332 |
| Dose requirement of Propofol (μg/kg/min) | 76.25 (24.21) | 27.88 (16.71) | 38.88 (15.85) | 48.36 37.73, 58.99 <0.001 | 37.36 27.39, 47.34 <0.001 | −11.00−16.21, −5.79 0.001 |
Data expressed as mean (standard deviation). BIS- Bispectral Index
The mean propofol requirement also differed significantly between the three phases (P < 0.001), and on further analysis, the difference in dose of propofol between the dissection and anhepatic phases (P < 0.001), anhepatic and neohepatic phases (P < 0.001), and between dissection and neohepatic phases (P < 0.001) were found to be significant [Table 2]. There was no difference in mean propofol consumption with increasing MELD score [propofol dosage was 119.13 (SD: 54.38) (95%CI: 32.59, 205.66), 134.25 (SD: 32.3) (95% CI: 111.14, 157.35), 173.49 (SD: 56.54) (95% CI: 114.15, 132.82) μg/kg/min for MELD 15-20, 21–25, >25 respectively, P = 0.148].
None of the patients had any history of recall after surgery.
DISCUSSION
In our study, the mean TPC of propofol in all the phases of live donor liver transplantation was notably lower compared to the maintenance dose of 2.5–4 μg/mL typically administered with opioids in standard surgical patients. Furthermore, this discrepancy highlights a reduced TPC in both the anhepatic and neohepatic phases relative to the dissection phase.
Propofol clearance depends on hepatic blood flow. In patients with cirrhosis, hepatic blood flow is diminished, leading to a reduced propofol dose requirement during the dissection phase compared to standard dosages for healthy individuals.[5] Cirrhotic patients often have collateral circulation, redirecting portal blood to the systemic circulation, thereby slowing propofol metabolism.[5] In addition, as only 1.2%–1.7% of propofol exists in its free fraction, with the remainder bound to albumin and red blood cells, cirrhotic patients’ hypoalbuminemia and anaemia characteristics lead to an increased free fraction of propofol.[8] Consequently, these patients require a lower propofol dose during the liver transplantation dissection phase. Chi et al.[5] also observed elevated plasma propofol concentrations at a target of 3 μg/mL in patients with CTP B and C CLD, suggesting a dose reduction based on liver disease severity. In our study, we employed BIS monitoring to titrate propofol dosing and mitigate risks of over- or under-dosage.
A series of eight patients by Tremelot et al.[7] recorded higher TPC values during the anhepatic and dissection phases [2.0 (SD: 0.8) μg/mL and 3.0 (SD: 0.9) μg/mL, respectively] compared to our findings [1.29 (SD: 0.65) μg/mL and 2.12 (SD: 0.63) μg/mL, respectively). This variance may be attributed to the worse CTP scores of the patients and the more equivalent opioid dosages in our study.
When analysing propofol dosage across the different phases of liver transplantation, the requirement was reduced to 61% in the anhepatic phase and 63.7% in the neohepatic phase compared to the dissection phase. The lower dosage in the anhepatic phase is expected due to the absence of liver function and reduced cardiac output resulting from portal and inferior vena cava clamping, which diminishes hepatic blood flow and peripheral distribution of propofol. Takizawa et al.[4] also reported a 42% decrease in apparent systemic clearance of propofol during the anhepatic phase relative to the dissection phase. Restoux et al. and Tremelot et al. noted reduced propofol requirements during the anhepatic phase.[6,7] Based on a pig model study, the results presented appear to contradict the findings of Murayama et al.,[9] who proposed that the extrahepatic metabolism of propofol might lower propofol blood concentration in the absence of the liver. The exact location of extrahepatic clearance for propofol remains a topic of debate, particularly regarding the role of the kidneys.[10,11] In addition, while there is some suggestion that the small intestine could be involved in propofol metabolism, the involvement of the lungs in this process remains contentious.[4,11,12]
The increased propofol requirement observed in the neohepatic phase compared to the anhepatic phase can be attributed to the clearance of propofol by the newly implanted allograft, which is reflected in the increased BIS values and consequent higher propofol requirements in this phase.[6] Our study showed a 63.9% reduction in propofol requirements in the neohepatic phase compared to the dissection phase. This differs from the findings of Restoux et al.,[6] who reported comparable doses in both phases. This discrepancy may be due to the smaller volume of the grafted liver in living donor liver transplantation compared to the whole liver transplant from a deceased donor used in orthotopic liver transplantation.
The pharmacokinetics of propofol follow a three-compartment model, wherein the drug is distributed among the central compartment (plasma) and the fast and slow equilibrating tissues following an initial bolus. The TCI pump operates on the bolus, elimination, and transfer principle, adjusting the maintenance dose to account for the elimination and distribution of the drug. We chose the Marsh model over the Schnider model due to the former’s lower propensity for plasma propofol overshoot (up to 150% of the target concentration) compared to the Schnider model (up to 300%). The Marsh model’s reduced overshoot minimises the risk of haemodynamic instability, which is crucial during liver transplantation, a procedure characterised by significant fluid shifts and blood loss.[13,14] In addition, the Marsh model allows dosing based on body weight, aligning with common clinical practices, whereas the Schnider model calculates an age-based initial rate of decline.[13,15] We mitigated the Marsh model’s limitation of larger bolus doses by starting TCI at a lower 2 μg/mL dose. Given our use of BIS monitoring for dose adjustment, either model could be effectively utilised for anaesthesia maintenance.
While our study observed statistically significant haemodynamic variations and temperature changes across the three phases, these variations did not result in clinically relevant outcomes. None of the patients suffered from massive haemorrhage. The findings may not apply to scenarios involving severe haemorrhage as propofol pharmacokinetics can vary significantly with different stages of haemorrhagic shock.[3]
Our study’s limitations include the lack of plasma propofol concentration measurements, which could have provided insights into the difference between measured and target concentrations. The small sample size limits the generalisability of our findings, and a larger sample size is necessary to accurately determine propofol dosing across the three phases of liver transplantation. In addition, closed-loop anaesthesia could have provided more precise titration of propofol dosage. We did not measure the blood loss and fluid administered in each phase separately, which might have provided valuable insights into the propofol dosage.
CONCLUSION
The mean target propofol concentration when using a TCI pump should be adjusted to 61% and 63.7% of the dissection phase levels during the anhepatic and neohepatic phases, respectively, to avoid overdosage and ensure optimal anaesthesia management.
Study data availability
De-identified data may be requested with reasonable justification from the authors (email to the corresponding author) and shall be shared upon request.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lu CH, Yeh CC, Huang YS, Lee MS, Hsieh CB, Cherng CH, et al. Hemodynamic and biochemical changes in liver transplantation: A retrospective comparison of desflurane and total intravenous anesthesia by target-controlled infusion under auditory evoked potential guide. Acta Anaesthesiol Taiwan. 2014;52:6–12. doi: 10.1016/j.aat.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Wu ZF, Lin WL, Lee MS, Hung NK, Huang YS, Chen TW, et al. Propofol vs desflurane on the cytokine, matrix metalloproteinase-9, and heme oxygenase-1 response during living donor liver transplantation: A pilot study. Medicine. 2019;98:e18244. doi: 10.1097/MD.0000000000018244. doi: 10.1097/MD.0000000000018244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Egan ED, Johnson KB. The influence of hemorrhagic shock on the disposition and effects of intravenous anesthetics: A narrative review. Anesth Analg. 2020;130:1320–30. doi: 10.1213/ANE.0000000000004654. [DOI] [PubMed] [Google Scholar]
- 4.Takizawa D, Sato E, Hiraoka H, Tomioka A, Yamamoto K, Horiuchi R, et al. Changes in apparent systemic clearance of propofol during transplantation of living related donor liver. Br J Anaesth. 2005;95:643–7. doi: 10.1093/bja/aei243. [DOI] [PubMed] [Google Scholar]
- 5.Chi X, Pan J, Cai J, Luo G, Li S, Yuan D, et al. Pharmacokinetic analysis of propofol target-controlled infusion models in Chinese patients with hepatic insufficiency. Med Sci Monit. 2018;24:6925–33. doi: 10.12659/MSM.910103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Restoux A, Grassin-Delyle S, Liu N, Paugam-Burtz C, Mantz J, Le Guen M. Pilot study of closed-loop anaesthesia for liver transplantation. Br J Anaesth. 2016;117:332–40. doi: 10.1093/bja/aew262. [DOI] [PubMed] [Google Scholar]
- 7.Tremelot L, Restoux A, Paugam-Burtz C, Dahmani S, Massias L, Peuch C, et al. Interest of BIS monitoring to guide propofol infusion during the anhepatic phase of orthotopic liver transplantation. Ann Fr Anesth Reanim. 2008;27:975–8. doi: 10.1016/j.annfar.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Mazoit JX, Samii K. Binding of propofol to blood components: Implications for pharmacokinetics and for pharmacodynamics. Br J Clin Pharmacol. 1999;47:35–47. doi: 10.1046/j.1365-2125.1999.00860.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murayama T, Sato Y, Wainai T, Enomoto A, Seo N, Yoshino H, et al. Effect of continuous infusion of propofol on its concentration in blood with and without the liver in pigs. Transplant Proc. 2005;37:4567–70. doi: 10.1016/j.transproceed.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 10.Takata K, Kurita T, Morishima Y, Morita K, Uraoka M, Sato S. Do the kidneys contribute to propofol elimination? Br J Anaesth. 2008;101:648–52. doi: 10.1093/bja/aen249. [DOI] [PubMed] [Google Scholar]
- 11.Hiraoka H, Yamamoto K, Miyoshi S, Morita T, Nakamura K, Kadoi Y, et al. Kidneys contribute to the extrahepatic clearance of propofol in humans, but not lungs and brain. Br J Clin Pharmacol. 2005;60:176–82. doi: 10.1111/j.1365-2125.2005.02393.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen YZ, Zhu SM, He HL, Xu JH, Huang SQ, Chen QL. Do the lungs contribute to propofol elimination in patients during orthotopic liver transplantation without veno-venous bypass? Hepatobiliary Pancreat Dis Int. 2006;5:511–4. [PubMed] [Google Scholar]
- 13.Nimmo AF, Absalom AR, Bagshaw O, Biswas A, Cook TM, Costello A, et al. Guidelines for the safe practice of total intravenous anaesthesia (TIVA) joint guidelines from the association of anaesthetists and the society for intravenous anaesthesia. Anaesthesia. 2019;74:211–24. doi: 10.1111/anae.14428. [DOI] [PubMed] [Google Scholar]
- 14.Absalom AR, Mani V, De Smet T, Struys MM. Pharmacokinetic models for propofol—defining and illuminating the devil in the detail. Br J Anaesth. 2009;103:26–37. doi: 10.1093/bja/aep143. [DOI] [PubMed] [Google Scholar]
- 15.Lee YH, Choi GH, Jung KW, Choi BH, Bang JY, Lee EK, et al. Predictive performance of the modified Marsh and Schnider models for propofol in underweight patients undergoing general anaesthesia using target-controlled infusion. Br J Anaesth. 2017;118:883–91. doi: 10.1093/bja/aex102. [DOI] [PubMed] [Google Scholar]


