Abstract
Purpose
Myocardial perfusion imaging (MPI) procedures from single photon emission computed tomography and positron emission tomography imaging have been registered in the Western Denmark Heart Registry (WDHR) since 2017 as a sub-registry (WDHR-MPI). The aim was to review the content, quality, and research potential of the WDHR-MPI and assess the completeness and validity of its key variables.
Patients and Methods
Using the Danish National Patient Registry (DNPR) as a reference, we calculated the completeness of procedure registration as the proportion of procedures registered in the WDHR-MPI from 2017 to 2021. We defined completeness of variable registration as the proportion of non-missing values for a given variable and examined it for 38 key variables. We assessed validity by estimating the positive predictive values (PPV) and negative predictive values (NPV) with 95% confidence intervals (CI) for 26 selected key variables using corresponding extracted information from 300 randomly selected patient records.
Results
We identified 19,084 procedures in 17,871 patients from all seven cardiac centers performing nuclear cardiology procedures in the WDHR uptake area. The registry accumulated 4000–6000 procedures each year from 2019 to 2021. The overall completeness of procedure registration was 72% (95% CI 72–73), increasing from 14% (95% CI 13–15) in 2017 to 98% (95% CI 98–98) in 2021. The mean completeness of variable registration was 89%. The validity of entered data was high, with an overall PPV for the selected key variables of 95% (95% CI 94–95) and NPV of 94% (95% CI 93–96).
Conclusion
The WDHR-MPI is one of the largest systematic MPI cohorts. The overall high completeness and validity of the data support its potential for cardio-epidemiological research.
Keywords: ischemic heart disease, chronic coronary syndromes, cardiac imaging, database, registries, validation
Plain language summary
If you have ischemic heart disease, you may experience symptoms such as chest tightness and shortness of breath due to decreased blood supply to the heart muscle. To help identify decreased blood supply to the heart muscle, doctors can use a specialized scan which involves the injection of low doses of radioactive tracers into the bloodstream. Since 2017, doctors in Denmark have been recording these scans in the Western Denmark Myocardial Perfusion Imaging Registry (WDHR-MPI). This study found a high completeness and validity of the registry. With 19,084 scans recorded from 2017 to 2021, this registry provides a high-quality resource that could improve diagnosis and treatment for people with heart disease.
Introduction
Ischemic heart disease remains a highly prevalent disease in Western countries and an emerging disease in other parts of the world.1 European guidelines recommend the use of non-invasive imaging with eg single-photon emission computerized tomography (SPECT) or positron emission tomography (PET) myocardial perfusion imaging (MPI) in the diagnosis and management of patients with chest pain.2 Worldwide, 15–20 million SPECT procedures are performed annually, but PET-based MPI is increasingly utilized and has become the non-invasive reference standard for absolute measurements of myocardial perfusion.3
Since 2017, nuclear MPI procedures have been registered in the Western Denmark Heart Registry (WDHR) as a sub-registry (WDHR-MPI). The WDHR is a semi-national, multicenter-based registry with longitudinally obtained detailed patient and procedure data since 1999.4 The WDHR has been extensively used in large population-based studies and continues to influence patient care.4 While the cardiac computed tomography (CT) and coronary interventional data of the registry have been reviewed and validated, the MPI data have not.5
In general, if the data quality of the WDHR-MPI is sufficient, these data would allow for large-scale population-based studies of different domains of MPI. This study aims to review the content, data quality, and research potential of the WDHR-MPI.
Material and Methods
Setting and Data Sources
Western Denmark consists of three of the five regions in Denmark and holds a population of 3.2 million people as of 2024 (53% of the total population). Free access to general practitioners, outpatient specialty clinics, and hospitals, and partial reimbursement of prescribed medications for the entire Danish population is provided through the tax-supported Danish National Health System.6 All admissions, outpatient specialty clinic visits, and diagnostic procedures are registered in the Danish National Patient Registry (DNPR) according to the International Classification of Disease 10th Revision and Nordic Medical Statistics Committee’s Classification of Surgical Procedures.7 Upon birth or immigration, all residents are assigned a unique 10-digit Civil Personal Register (CPR) number with daily updates on residents’ emigration and vital status, enabling the linkage of individual patients across all Danish registries.8,9
As of 1999, the WDHR has longitudinally collected detailed patient and procedural data from diagnostic and treatment-related cardiac procedures.4 Data are entered via a web-based data entry form by the treating physician or their delegate. Each procedure type is recorded in a distinct dataset in the WDHR, and a common population dataset identifies each unique patient in the register with a CPR number, date of birth, date of death (if applicable), and municipality. The WDHR-MPI dataset consists of 187 variables covering pre-procedural data such as risk factors and previous cardiac interventions, procedural data such as isotope dose and type of vasodilator, and the procedure results.
Study Population
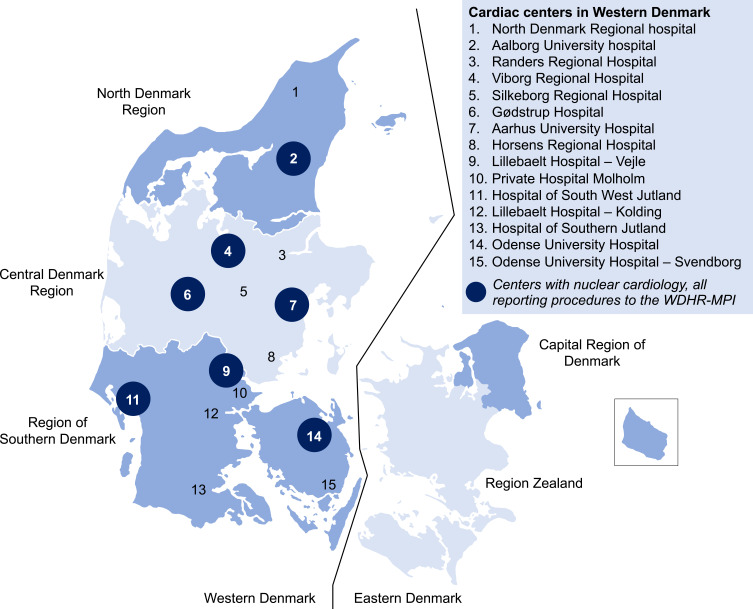
All 15 cardiac centers in Western Denmark report to the WDHR (Figure 1). Of these, three are university cardiac centers defined as centers performing coronary revascularization procedures, whereas the remaining are regional hospitals except for one private hospital. Nuclear MPI procedures are performed at nuclear departments at seven of the hospitals having a cardiac center, three university sites and four regional sites. Of the university sites, one is performing PET and two are performing SPECT. Of the regional sites, one is performing PET, two are performing SPECT, and one site switched from SPECT to PET in October 2020.
Figure 1.
Source Population and Cardiac Centers with Nuclear Cardiology Contributing Data to the Western Denmark Myocardial Perfusion Imaging Registry (WDHR-MPI). The Western Denmark Heart Registry covers the three Western regions of Denmark. All cardiac centers in the area are depicted, and centers performing nuclear myocardial perfusion imaging are highlighted in circles with all of them reporting procedures to the Western Denmark Myocardial Perfusion Imaging Registry (WDHR-MPI).
Abbreviation: WDHR-MPI, the Western Denmark Myocardial Perfusion Imaging Registry.
We included all patients registered in the WDHR-MPI registry between January 1st, 2017, and December 31st, 2021, in our review. We used the DNPR as a reference for the completeness of procedure registration.
Completeness
Completeness of data was evaluated both as procedure and variable registrations. We defined completeness of procedure registration as the number of procedures registered in the WDHR-MPI that could be matched to a procedure in the DNPR within ±31 days of the procedure date divided by the total number of procedures registered with any of the procedure codes listed in Supplementary Table 1 in the DNPR. Statistics Denmark created the DNPR reference population as all persons who had at one point in time lived in Western Denmark between 2008–2021. Thus, we removed patients investigated at hospitals in Western Denmark, but without residence in Western Denmark during the period required for inclusion in the DNPR cohort, from the WDHR-MPI cohort before analysis of procedural completeness. Likewise, in the DNPR, we removed procedures performed at hospitals outside of Western Denmark before analysis of the completeness of procedure registration as these hospitals are not reporting to the WDHR. As the rest and stress procedure of SPECT MPI is usually performed on different days, this will yield two procedure registrations, and therefore two procedure dates in the DNPR. However, the stress-rest SPECT examinations are only registered as one record and procedure date in the WDHR-MPI. Therefore, we assumed SPECT procedures in the DNPR performed in the same patient within 90 days to be a single rest/stress procedure.
Completeness of variable registration was defined as the number of procedures with registered information of a specific variable divided by the total number of procedures in the MPI cohort. We examined variable completeness for 38 specific variables that were considered to represent core elements of medical history, procedure, and imaging results.
Validity
We assessed the validity of MPI variables through a review of electronic medical records from a computer-generated random sample of 300 patients from all seven nuclear departments. The sample size (n=300) was based on previous experience from the sample of 250 patients used to validate cardiac CT data in the WDHR and no formal power calculation was done.5 We restricted the sample to procedures performed between January 1st, 2019, and December 31st, 2021, due to a five-year limit of medical record review imposed by several participating hospitals.
Before the generation of the sample population, we selected 26 key patient and procedural variables and defined their reference levels (Supplementary Table 2). One author (JHS) reviewed all electronic medical records with assistance from the local investigator at each site. If full electronic health records were not available, we collected information on medical history from referrals and procedure and image descriptions in the local radiology information system. We registered the results of the variables as one of three: confirmed by the electronic medical record, not confirmed by the electronic medical record, or missing in the electronic medical record. For each variable, we constructed a 2×2 contingency table with results for true positives, true negatives, false positives, and false negatives. We calculated positive predictive values (PPV) and negative predictive values (NPV) with 95% confidence intervals using the Wilson score interval method.10 True/false negatives and thus NPVs were only assessed in the nine variables that could attain a negative value, eg no history of myocardial infarction.
Sensitivity Analyses
During the study period, one study site switched from Rubidium-82 PET to [15O]H2O PET. As [15O]H2O is not retained in the myocardium when used as a tracer for PET MPI and the results are purely quantitative (myocardial blood flow in mL/g/min), no semi-quantitative segmental scores are obtained and thus no summed stress, rest, or difference scores can be calculated. However, the data entry form in the WDHR-MPI does not account for this. If no semi-quantitative segmental score is entered, the reported value will be zero which denotes normal perfusion, and thus all segments and sums of rest, stress, and difference scores for [15O]H2O will be zero. Thus, we excluded [15O]H2O procedures from the primary analysis of predictive values for segmental stress score and summed stress score. To assess the impact of this on predictive values, we performed a sensitivity analysis of predictive values for the segment stress score and summed stress score including [15O]H2O procedures.
As a sensitivity analysis of the impact of missing information in the electronic medical records on the predictive values, we constructed worst-case and best-case scenarios by calculating predictive values including all missing information as false and true positives/negatives, respectively.
Reporting followed reporting guidelines.11 All statistical analyses were conducted using the statistical software R version 4.3.1.12 The study was approved by the Central Denmark Region (1–45-70-65-23) and registered at Aarhus University (2022–0367531).
Results
Study Population
From 2017 through 2021, we identified 19,084 procedures in the WDHR-MPI. These procedures were performed on 17,871 unique individuals. A total of 1845/19,084 (9.7%) of the procedures were performed within 90 days after a cardiac CT, while 2862/19,084 (15%) of the procedures were followed by invasive coronary angiography within 90 days after the procedure. Revascularization within 90 days was performed following 1463/19,084 (7.7%) of the procedures with percutaneous coronary intervention in 1225/1,463 (84%) and coronary artery bypass grafting in 238/1463 (16%) of the revascularization procedures. Characteristics of the study population, procedures, and imaging results are listed in Tables 1–3.
Table 1.
Completeness of Cohort Variables in the Western Denmark Myocardial Perfusion Imaging Registry. Selected Key Patient Characteristics Variables of the Western Denmark Myocardial Perfusion Registry. Frequencies are in Absolute Numbers with Proportions in Parentheses if Nothing Else is Stated for the Variable. All Frequencies, Proportions, and Descriptive Statistics Refer to Only Complete Cases of the Variable
| Variable | Frequency, % | Completeness, %a |
|---|---|---|
| Age median (IQR) | 71 (62, 77) | 100 |
| Female sex | 7007 (37) | 100 |
| Referral diagnosis | – | 100 |
| Family history of premature coronary artery disease | 7026 (45) | 82 |
| Smoking status (active or former) | 11,270 (69) | 86 |
| Diabetes | 3666 (21) | 92 |
| Medically treated dyslipidemia | 12,337 (71) | 92 |
| Medically treated hypertension | 12,811 (73) | 92 |
| Previous heart surgery | 2567 (15) | 91 |
| Previous coronary artery bypass graft surgery | 1776 (11) | 87b |
| Previous myocardial infarction | 3768 (22) | 89 |
| Previous percutaneous coronary intervention | 5654 (32) | 91 |
| Previous revascularization | 7075 (39) | 95 |
| Ejection fraction (%) on echocardiography (IQR) | 60 (50, 60) | 39 |
| Height (cm) | 172 (165, 179) | 98 |
| Weight (kg) | 84 (72, 96) | 98 |
| Body mass index (kg/m2) | 28 (25, 32) | 98 |
Notes: aCompleteness of variable registration is the proportion of observations without missing values in each variable. bPrevious coronary artery bypass graft surgery is a drop-down field of previous heart surgery. The completeness of previous coronary artery bypass graft surgery refers to the combined completeness of the two variables.
Abbreviation: IQR, inter-quartile range.
Table 2.
Completeness of Procedure Variables in the Western Denmark Myocardial Perfusion Imaging Registry. Selected Key Procedure Variables of the Western Denmark Myocardial Perfusion Registry. Frequencies are in Absolute Numbers with Proportions in Parentheses if Nothing Else is Stated for the Variable. All Frequencies, Proportions and, Descriptive Statistics Refer to Only Complete Cases of the Variable
| Variable | Frequency, % | Completeness, %a |
|---|---|---|
| Date of procedure | – | 100 |
| Procedure during admission | 100 (0.6) | 94 |
| Indication | – | 100 |
| Angina/angina equivalent | 16,279 (85) | – |
| Asymptomatic electrocardiogram changes | 704 (3.7) | – |
| Heart failure | 828 (4.3) | – |
| Other inconclusive diagnostic cardiac procedure | 527 (2.8) | – |
| Anomalous coronary artery | 42 (0.2) | – |
| Microvascular disease | 42 (0.2) | – |
| Research | 150 (0.8) | – |
| Transplant evaluation | 91 (0.5) | – |
| Other clinical indication | 421 (2.2) | – |
| Symptom description | – | 28b |
| Typical angina | 1631 (37) | – |
| Atypical angina | 944 (21) | – |
| Non-anginal chest pain | 562 (13) | - |
| Dyspnea | 1337 (30) | - |
| Viability procedure | 438 (2.3) | 99 |
| Type of myocardial perfusion imaging | - | 100 |
| SPECT | 9600 (50) | - |
| PET | 9484 (50) | - |
| SPECT tracerc | - | 100c |
| Sestamibi | 879 (9.2) | - |
| Tetrofosmin | 8,719 (91) | - |
| Other | 2 (0.0) | - |
| SPECT radiation exposure, mSv (IQR)c | 8.1 (5.1, 11)c | 99c |
| PET tracerc | - | 100c |
| Rubidium-82 | 7410 (78) | - |
| [13N]NH3 | 6 (0.1) | - |
| [15O]H2O | 2064 (22) | - |
| Other | 4 (0.0) | - |
| PET radiation dose, mSv (IQR)c | 2.3 (1.9, 2.8)c | 100c |
| Stress protocol | - | 100 |
| Ergometer | 197 (1.0) | - |
| Adenosine | 11,538 (61) | - |
| Regadenoson | 7276 (38) | - |
| Dobutamine | 30 (0.2) | - |
| Other | 38 (0.2) | - |
| Any complication | 130 (0.7) | 100 |
| Complicationd | - | 93d |
| Atrioventricular block | 15 (12) | − |
| Arrhythmia | 2 (1.7) | - |
| Bronchospasm | 29 (24) | - |
| Vasovagal reaction | 14 (12) | - |
| Other | 61 (50) | - |
Notes: aCompleteness of variable registration is the proportion of observations without missing values in each variable. bSymptom description is a drop-down field when angina/angina equivalent is selected as indication. The completeness of symptom description refers only to procedures with the indication angina/angina equivalent. cFrequencies and completeness are only based on SPECT and PET procedures, respectively. dComplication description is a drop-down field of any complication. Frequencies and completeness refer to the number of procedures registered with any complication.
Abbreviations: IQR, inter-quartile range; PET, positron emission tomography; SPECT, single-photon emission computerized tomography.
Table 3.
Completeness of Result Variables in the Western Denmark Myocardial Perfusion Imaging Registry. Selected Key Results Variables of the Western Denmark Myocardial Perfusion Registry. Frequencies are in Absolute Numbers with Proportions in Parentheses if Nothing Else is Stated for the Variable. All Frequencies, Proportions, and Descriptive Statistics Refer to Only Complete Cases of the Variable. Completeness of Variable Registration is the Proportion of Observations Without Missing Values in Each Variable
| Variable | Frequency, % | Completeness, %a |
|---|---|---|
| Image quality | – | 100 |
| Evaluable | 18,383 (96) | – |
| Partially evaluable | 530 (2.8) | – |
| Not evaluable | 171 (0.9) | – |
| Any abnormal perfusion | 5955 (32) | 99 |
| Perfusion abnormalityb | – | 98b |
| Reversible ischemia >10% of myocardium | 1803 (31) | – |
| Irreversible ischemia | 1469 (25) | – |
| Irreversible ischemia and reversible ischemia >10% of myocardium | 745 (13) | – |
| Reversible ischemia <10% of myocardium | 645 (11) | – |
| Irreversible ischemia and reversible ischemia <10% of myocardium | 242 (4.1) | – |
| Balanced ischemia | 392 (6.7) | – |
| Other | 595 (10) | – |
| Agatston calcium score, median (IQR) | 174 (15, 685) | 14 |
| Ejection fraction stress, median (IQR) | 61 (51, 69) | 79 |
| Rest perfusion LAD, mL/g/min, median (IQR)c,d | – | 96c |
| Rubidium-82 | 1.1 (0.9, 1.4) | |
| [15O]H2O | 1 (0.8, 1.2) | |
| Stress perfusion LAD, mL/g/min, median (IQR)c,d | - | 96c |
| Rubidium-82 | 2.4 (1.9, 3) | - |
| [15O]H2O | 2.5 (1.8, 3.2) | - |
| Myocardial flow reserve LAD, median (IQR)c,d | - | 95c |
| Rubidium-82 | 2.1 (1.7, 2.6) | - |
| [15O]H2O | 2.6 (2, 3.2) | - |
| Global rest perfusion, mL/g/min, median (IQR)c | - | 97c |
| Rubidium-82 | 1.1 (0.9, 1.4) | |
| [15O]H2O | 1 (0.8, 1.2) | |
| Global stress perfusion, mL/g/min, median (IQR)c | - | 96c |
| Rubidium-82 | 2.4 (1.9, 3) | |
| [15O]H2O | 2.5 (1.8, 3.2) | |
| Global myocardial flow reserve, median (IQR)c | - | 95c |
| Rubidium-82 | 2.2 (1.7, 2.7) | |
| [15O]H2O | 2.6 (2, 3.2) | |
| Summed stress score, median (IQR) | 1 (1, 6) | 100 |
Notes: aCompleteness of variable registration is the proportion of observations without missing values in each variable. bPerfusion abnormality is a drop-down field of any abnormal perfusion. Frequencies and completeness refer to the number of procedures registered with any abnormal perfusion. cOnly reported for PET procedures, thus completeness refers to the total number of PET procedures. The six procedures with [13N]NH3 as the tracer and four procedures with the tracer reported as “other” are not listed. dTerritorial rest and stress perfusion and myocardial flow reserve is also available for the left circumflex artery and right coronary artery with similar completeness, but not included in the table to limit the size of the table.
Abbreviations: IQR, inter-quartile range; LAD, left anterior descending artery; PET, positron emission tomography; SD, standard deviation.
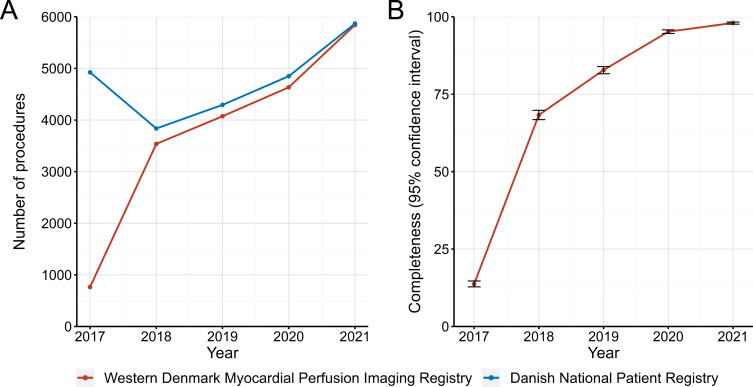
Completeness
For analysis of completeness of procedure registration, we excluded 233 procedures as these CPR numbers were not present in the reference population (ie, they did not live in Western Denmark at any time in the period 2008–2021) and thus were not available for analysis, leaving 18,851 procedures in the WDHR-MPI for analysis. In 2017, 740/765 procedures (97%) were registered by only one nuclear department, while six nuclear departments reported to the WDHR-MPI in 2018, and all seven nuclear departments reported procedures in 2019 and later. We identified a total of 24,876 procedures in the DNPR in the period 2017–2021. Of these procedures, we excluded 1105 procedures performed at hospitals outside of Western Denmark, leaving 23,771 procedures in the DNPR for comparison. The number of procedures per year in the WDHR-MPI and DNPR are presented in Figure 2A. We were able to match 17,217 procedures in the WDHR-MPI by CPR number and date ±31 days to one of the 23,771 procedures in the DNPR, yielding an overall completeness of procedure registration of 72% (95% CI 72–73). The completeness of procedure registration increased from 14% (95% CI 13–15) in 2017 to 98% (95% CI 98–98) in 2021 as illustrated in Figure 2B.
Figure 2.
Trends in Registrations and Completeness of Procedures in the Western Denmark Myocardial Perfusion Imaging Registry. (A) Annual number of positron emission tomography and single-photon emission computerized tomography myocardial perfusion imaging procedures registered in the Western Denmark Myocardial Perfusion Imaging Registry and Danish National Patient Registry. (B) Completeness of procedure registration calculated as the proportion of procedures registered in the Western Denmark Myocardial Perfusion Imaging Registry using the number of procedures with corresponding Civil Personal Register number and date of MPI procedure ±31 days in the Danish National Patient Registry as a reference. Completeness estimates are depicted as points with 95% confidence intervals as error bars.
The mean completeness of variable registration of the 38 selected key variables was 89%, ranging from 14% for the Agatston calcium score to 100% for 11 (29%) out of the 38 variables. The completeness of variable registration was above 85% for 33/38 (87%) variables (Tables 1–3).
Validity
In the validation sample of 26 selected key variables from 300 randomly selected patients, a total of 6511/7800 (83%) variable values were relevant for validation. Of the 6511 relevant variable values, 544 (8.4%) values were missing in the WDHR-MPI and therefore not validated in the electronic medical records and thus not included in the calculation of predictive values, leaving 5967 variable values in the WDHR-MPI for validation. We were able to access full electronic medical records at five of seven centers corresponding to 250/300 patients (83%). The number of true and false positive and negative observations and calculated positive and negative predictive values are listed in Table 4.
Table 4.
Validity of Key Variables of the Western Denmark Myocardial Perfusion Imaging Registry During 2019–2021 Using Medical Record Review as Reference Standard. The Validation Sample Consists of 300 Randomly Selected Patients Who Underwent SPECT or PET Myocardial Perfusion Imaging at Three University and Four Regional Cardiac Centers in Western Denmark in the Period 2019–2021. In the Analyses of Predictive Values, Only Records with Complete Information on the Specific Variable in the Registry Were Included
| Variable | True Positive | True Negative | False Positive | False Negative | Positive Predictive Value, % (95% CI) | Negative Predictive Value, % (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Observed | Worst-Case Scenarioa | Best-Case Scenarioa | Observed | Worst-Case Scenarioa | Best-Case Scenarioa | |||||
| Medical history | ||||||||||
| Family history of premature coronary artery disease | 78 | 69 | 10 | 9 | 89 (80–94) | 45 (38–53) | 94 (90–97) | 89 (80–94) | 42 (35–50) | 95 (90–97) |
| Smoking status | 150 | 52 | 7 | 1 | 96 (91–98) | 71 (64–77) | 97 (94–98) | 98 (90–100) | 48 (39–58) | 99 (95–100) |
| Diabetes | 52 | 213 | 5 | 3 | 91 (81–96) | 81 (70–89) | 92 (83–97) | 99 (96–100) | 96 (92–98) | 99 (96–100) |
| Medically treated dyslipidemia | 199 | 65 | 2 | 15 | 99 (96–100) | 97 (94–99) | 99 (97–100) | 81 (71–88) | 77 (67–85) | 82 (73–89) |
| Medically treated hypertension | 202 | 68 | 3 | 9 | 99 (96–100) | 96 (93–98) | 99 (96–100) | 88 (79–94) | 83 (73–90) | 89 (80–94) |
| Myocardial infarction | 61 | 180 | 6 | 11 | 91 (82–96) | 82 (72–89) | 92 (83–96) | 94 (90–97) | 91 (86–94) | 94 (90–97) |
| Percutaneous coronary intervention | 99 | 156 | 5 | 14 | 95 (89–98) | 93 (86–96) | 95 (90–98) | 92 (87–95) | 90 (85–94) | 92 (87–95) |
| Ejection Fraction (%) on echocardiography | 83 | - | 15 | - | 85 (76–91) | 78 (69–84) | 86 (78–91) | - | - | - |
| Procedure | ||||||||||
| Procedure date | 298 | - | 2 | - | 99 (98–100) | 99 (98–100) | 99 (98–100) | - | - | - |
| Indication | 284 | - | 15 | - | 95 (92–97) | 95 (92–97) | 95 (92–97) | - | - | - |
| Imaging modality | 300 | - | 0 | - | 100 (99–100) | 100 (99–100) | 100 (99–100) | - | - | - |
| SPECT tracer | 146 | - | 2 | - | 99 (95–100) | 99 (95–100) | 99 (95–100) | - | - | - |
| PET tracer | 152 | - | 0 | - | 100 (98–100) | 100 (98–100) | 100 (98–100) | - | - | - |
| Stress protocol | 298 | - | 1 | - | 100 (98–100) | 99 (98–100) | 100 (98–100) | - | - | - |
| Any complication | 4 | 295 | 0 | 1 | -b | -b | -b | 100 (98–100) | 100 (98–100) | 100 (98–100) |
| Complication | 4 | - | 0 | - | -b | -b | -b | - | - | - |
| Results | ||||||||||
| Image quality | 300 | - | 0 | - | 100 (99–100) | 100 (99–100) | 100 (99–100) | - | - | - |
| Any abnormal perfusion | 111 | 164 | 7 | 12 | 94 (88–97) | 94 (88–97) | 94 (88–97) | 93 (89–96) | 93 (89–96) | 93 (89–96) |
| Perfusion abnormality | 107 | - | 9 | - | 92 (86–96) | 92 (86–96) | 92 (86–96) | - | - | - |
| Ejection fraction stress | 216 | - | 11 | - | 95 (92–97) | 93 (89–96) | 95 (92–97) | - | - | - |
| LVEDV stress | 179 | - | 13 | - | 93 (89–96) | 82 (77–87) | 94 (90–97) | - | - | - |
| LV mean volume stress | 94 | - | 17 | - | 85 (77–90) | 51 (44–58) | 91 (86–94) | - | - | - |
| Stress perfusion LAD | 126 | - | 8 | - | 94 (89–97) | 88 (81–92) | 94 (89–97) | - | - | - |
| Myocardial flow reserve LAD | 120 | - | 9 | - | 93 (87–96) | 83 (76–89) | 94 (89–97) | - | - | - |
| Stress score segment 13c | 229 | - | 12 | - | 95 (92–97) | 89 (85–92) | 95 (92–97) | - | - | - |
| Summed stress scorec | 203 | - | 38 | - | 84 (79–88) | 79 (74–84) | 85 (80–89) | - | - | - |
Notes: aWorst-case and best-case scenarios were calculated assuming that none (worst-case scenario) or all (best-case scenario) confirmed the data in the registry. bFrequencies are too low to provide meaningful estimates. c[15O]H2O procedures are excluded as the tracer is not retained in the myocardium.
Abbreviations: CAD, coronary artery disease; CI, confidence interval; LAD, left anterior descending artery; LV, left ventricular; LVEDV, left ventricular end‐diastolic volume; PET, positron emission tomography; SPECT, single-photon emission computerized tomography.
The PPVs ranged from 84% (95% CI 79–88) for summed stress score to 100% for four variables (Table 4). The estimated PPVs were above 90% in 22/26 (85%) variables and the overall PPV was 95% (95% CI 94–95). The NPVs ranged from 81% (95% CI 71–88) for medically treated dyslipidemia to 100% (95% CI 98–100) for any complication. The estimated NPVs were above 90% in 6/9 (67%) variables for which NPVs were meaningful parameters and the overall NPV was 94% (95% CI 93–96).
Of the 5967 available variable values in the WDHR-MPI, we could not verify 338 (5.7%) variable values in electronic medical records due to missing information. The proportion of missing information in the electronic medical records was highest for smoking status (21%), family history of premature coronary artery disease (34%), and left ventricular mean volume during stress (40%). This impacted the worst-case scenarios for these variables with PPVs for smoking status at 71% (95% CI 64–77), family history of premature coronary artery disease at 45% (95% CI 38–53), and left ventricular mean volume during stress at 51% (95% CI 44–58), while the impact of missing values on estimates of PPVs for the remaining variables were minor (Table 4). Similarly, the NPVs for smoking status at 48% (95% CI 39–58) and family history of premature coronary artery disease at 42% (95% CI 35–50) were decreased in the worst-case scenarios due to missing information, while the impact was small in the other variables (Table 4). When we included the 43/300 (14%) [15O]H2O procedures in a sensitivity analysis of predictive values, the PPV for stress score in segment 13 selected for validation decreased from 95% (95% CI 92–97) to 81% (95% CI 76–85) while the PPV for summed stress score decreased from 84% (95% CI 79–88) to 72% (95% CI 66–76).
Discussion
This study investigated the content and data quality of the WDHR-MPI. We found increasing completeness of procedure registration during the study period with high coverage of the registry from 2020. Furthermore, the completeness of variable registration was high for most variables. Importantly, we found high positive and negative predictive values for most of the selected key variables.
Previous Literature
The near-complete registration of all procedures in the WDHR-MPI in 2021 is comparable to the 99.5% completeness of procedure registration for invasive coronary angiography and percutaneous coronary intervention for 2022 in Western Denmark in the Danish Heart Registry to which the WDHR also provides data.13 Additionally, it matched the 93.4% completeness of registration of coronary CT angiography procedures.13 A similar pattern with increasing completeness of procedure registrations was observed in the first years after the inclusion of cardiac CT in the WDHR in the years from 2008 through 2012.5 We attribute the initial low completeness of procedure registration to the fact that only one center reported the vast majority of procedures in 2017, and it was not until 2019 that all centers began reporting to the WDHR-MPI. Likewise, the completeness of individual variables is similar to those observed for the cardiac CT procedures, invasive coronary angiography, and percutaneous coronary intervention domains of the WDHR, with the exceptions of ejection fraction on echocardiography and Agatston calcium score which both have low completeness in the WDHR-MPI.14 However, only two centers perform calcium scoring and only in patients without known ischemic heart disease. Thus, the observed 14% completeness of this variable is underestimated and the completeness referring to actual calcium score procedures performed would probably be considerably higher.
To our knowledge, no other population-based, multicenter nuclear MPI registries with continuing registration exist. The largest multicenter MPI registry is the Registry of Fast Myocardial Perfusion Imaging with Next Generation SPECT (REFINE SPECT) which is an international, multicenter registry recruiting patients with known or suspected coronary artery disease undergoing SPECT. From 2009 until 2014, 20,418 consecutive patients were included in a prognostic cohort with follow-up through national databases, chart review, and/or patient contact, and 2079 consecutive patients were included in a diagnostic cohort undergoing invasive coronary angiography after SPECT.15 Strengths of the REFINE SPECT registry include the collection of all image files and core lab quality control of all image analyses. The registry has been used to study prognosis after MPI and to develop machine-learning models to predict early coronary revascularization.16,17 Several PET MPI registries exist, with the largest being the Rubidium-82 PET registry from Saint Luke’s Health System (Greater Kansas City Area, Missouri, USA), which included 19,282 patients from 2010 through 2016 and has been extensively used to study associations of different domains of PET MPI with cardiovascular outcomes.18,19 However, the study of long-term prognosis using the registry is limited by the end of follow-up as of December 31st, 2017.
Strengths and Limitations
The population-based nature of the WDHR-MPI, the inclusion of all centers, and the high completeness of procedure registrations since 2020 reduce selection bias in future research. The WDHR prospectively collects detailed data on different diagnostic and treatment procedures.4 This allows for extensive studies of diagnostic and treatment pathways for acute and chronic coronary syndromes as well as studies of diagnostic procedures before cardiac surgery. Furthermore, the registered information on co-morbidity and risk factors for ischemic heart disease in the WDHR-MPI can be used as exposure or to control for confounding. Additional information on other comorbidities, medication use, subsequent diagnoses, and death can be obtained through individual-level linkage to other administrative, health, or clinical registries in Denmark.9 In particular, the major cardiovascular outcomes, such as myocardial infarction and stroke, can validly be assessed through the DNPR, while all-cause and cardiovascular mortality can be assessed through The Danish Register of Causes of Death.20,21 Complete follow-up with accurate censoring due to emigration or death is possible in Denmark owing to the Danish Civil Registration System.8 The observed PPVs and NPVs in our study suggest high validity of the selected key variables, comparable to those of cardiovascular diagnoses in the DNPR which is extensively used in clinical epidemiological research.20
While the findings of high completeness and validity in the current study support the use of the WDHR-MPI in research, several limitations must be considered before initiating such studies. The procedural completeness was low in the first year of the registry, largely attributable to only one center reporting to the WDHR-MPI. Although the WDHR encourages centers to report data prospectively, some centers have retrospectively reported past procedures to the WDHR-MPI until a certain time point and then started prospective reporting. The available variables do not explicitly provide information on whether data were reported prospectively or retrospectively. Importantly, all centers are now reporting prospectively.
Although the data in the validation sample is most consistent with high observed PPVs and NPVs, the worst-case scenarios cannot exclude that the predictive values of especially family history of premature coronary artery disease and smoking could be markedly lower. Furthermore, only 83% of the variable values selected for validation were available. However, this proportion resulted from some variables being registered according to drop-down fields of other variables, some variables are only relevant for PET procedures, and some variables were not relevant for [15O]H2O procedures.
As of March 2021, several variables underwent changes. The variable “Symptom description” was added for procedures with the indication angina/angina equivalent. In the “Perfusion abnormality”, the levels “Reversible ischemia <10% of myocardium” and “Irreversible ischemia and reversible ischemia <10% of myocardium” was added. For prospectively reported observations, these category levels were not available but may have been reported in the “Perfusion abnormality free text” variable. Retrospectively reported observations may have been reported using all available category levels irrespective of the time of procedure. Caution should be taken in future study designs and the interpretation of these variables.
The inclusion of [15O]H2O procedures in the calculation of PPVs for segmental scores and summed stress score resulted in lower PPVs for these variables. This is partly explained by the fact that all scores for [15O]H2O procedures are automatically reported as zero as stress scores are not generated for this tracer. Thus, great caution should be taken when using rest, stress, difference scores, and sums of these in future studies, and values for these in [15O]H2O procedures should instead be regarded as not appropriate. The observed PPV for summed stress score was lower than the PPV for the selected segmental value. Several factors may have contributed to this. First, the reporting practice of segment scores differs between centers. Some report the scores automatically generated by the analysis software while others report scores corrected by the reading physician, and others report scores by visual interpretation by the reading physician. The reference standard used in the analysis of validity was the scores available in the local picture archiving system and some misclassification may have been introduced. Second, the summed stress score in the WDHR-MPI is the sum of stress scores for the individual 17 myocardial segments. In some image software, stress scores can have decimals and the summed stress score can thus differ from the sum of rounded scores. Finally, as the summed stress score is a sum of 17 values, a typing error in only one of the segments would result in the summed stress score being false positive.
Conclusion
The WDHR-MPI is one of the largest cohorts of MPI patients and data are accumulating prospectively. Owing to the high completeness of procedure registration since 2020 and high validity of key variables, the WDHR-MPI could become a valuable tool for cardio-epidemiological research.
Acknowledgments
First, we acknowledge the tremendous effort by all centers and staff reporting procedures to the WDHR-MPI. Second, we would like to thank Søren Hess, MD, Chief Consultant, Clinical Associate Professor and Mie Holm Vilstrup MD, Chief Consultant for their kind assistance in obtaining permission to access electronic health records at Hospital South West Jutland. LDR acknowledges support in terms of a research grant (PD5Y-2023001-DCA) from the Danish Cardiovascular Academy, which is funded by the Novo Nordisk Foundation, grant number NNF20SA0067242, and The Danish Heart Foundation.
Funding Statement
This study was supported by a grant from the NIDO Research Fund. The funding source did not have a role in the design, conduct, analysis, or reporting of the study.
Abbreviations
CT, computed tomography; CI, confidence interval; CPR, Civil Personal Register; DNPR, Danish National Patient Registry; IQR, inter-quartile range; LAD, left anterior descending artery; MPI, myocardial perfusion imaging; PET, positron emission tomography; REFINE SPECT, Registry of Fast Myocardial Perfusion Imaging with Next-Generation SPECT; SD, standard deviation; SKS, Sundhedsvæsenets klassifikations system, English: The Danish Medical Classification System; SPECT, single-photon emission computerized tomography; WDHR, Western Denmark Heart Registry.
Data Sharing Statement
Data are not readily publicly available and cannot be shared according to Danish legislation but can be applied for at one of the Regions of Denmark, the WDHR, and Statistics Denmark. Programming code can be retrieved by request to the corresponding author.
Ethics Approval and Informed Consent
The study was approved by the Central Denmark Region (permission number 1-45-70-65-23) and this approval waived ethics approval and informed consent per Danish legislation.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Morten Böttcher has participated in advisory boards for Astra-Zeneca, Bayer, Boehringer Ingelheim, Novartis, NOVO Nordisk, and Sanofi. The remaining authors have no conflicts of interest.
References
- 1.Global Burden of Diseases Causes of Death Collaborators Global. regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knuuti J, Wijns W, Saraste A, et al. ESC Guidelines for the diagnosis and management of chronic coronary syndromes: the Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J. 2019;41(3):407–477. doi: 10.1093/eurheartj/ehz425 [DOI] [PubMed] [Google Scholar]
- 3.International Atomic Energy Agency. Nuclear Cardiology: Guidance on the Implementation of SPECT Myocardial Perfusion Imaging. International Atomic Energy Agency; 2016. [Google Scholar]
- 4.Schmidt M, Maeng M, Madsen M, Sorensen HT, Jensen LO, Jakobsen CJ. The Western Denmark Heart Registry: its Influence on Cardiovascular Patient Care. J Am Coll Cardiol. 2018;71(11):1259–1272. doi: 10.1016/j.jacc.2017.10.110 [DOI] [PubMed] [Google Scholar]
- 5.Nielsen LH, Norgaard BL, Tilsted HH, et al. The Western Denmark Cardiac Computed Tomography Registry: a review and validation study. Clin Epidemiol. 2015;7:53–64. doi: 10.2147/CLEP.S73728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johannesdottir SA, Horvath-Puho E, Ehrenstein V, Schmidt M, Pedersen L, Sorensen HT. Existing data sources for clinical epidemiology: the Danish National Database of Reimbursed Prescriptions. Clin Epidemiol. 2012;4:303–313. doi: 10.2147/CLEP.S37587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmidt M, Pedersen L, Sorensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi: 10.1007/s10654-014-9930-3 [DOI] [PubMed] [Google Scholar]
- 9.Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591. doi: 10.2147/CLEP.S179083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown LD, Cai TT, DasGupta A. Interval Estimation for a Binomial Proportion. Stat Sci. 2001;16(2):101–117. doi: 10.1214/ss/1009213286 [DOI] [Google Scholar]
- 11.Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.R Core Team. R: A Language and Environment for Statistical Computing. 2021; 2021. [Google Scholar]
- 13.Danish Regions - The Danish Clinical Quality Program – national Clinical Registries Danish Heart Registry - Annual Report 2022. 2023. Accessed March 26, 2024. Available from: https://www.sundhed.dk/content/cms/72/4672_dhreg_aarsrapport-2022.pdf.
- 14.Western Denmark Heart Registry Annual Report 2021 [Danish]. 2022. Accessed March 26, 2024. http://vdh.csc.dsdn.dk/Configuration/VDH/Documents/%c3%85rsrapporter/VDH%c3%85rsrapport%202021.pdf.
- 15.Slomka PJ, Betancur J, Liang JX, et al. Rationale and design of the REgistry of Fast Myocardial Perfusion Imaging with NExt generation SPECT (REFINE SPECT). J Nucl Cardiol. 2020;27(3):1010–1021. doi: 10.1007/s12350-018-1326-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Otaki Y, Betancur J, Sharir T, et al. 5-Year Prognostic Value of Quantitative Versus Visual MPI in Subtle Perfusion Defects: results From REFINE SPECT. JACC Cardiovasc Imaging. 2020;13(3):774–785. doi: 10.1016/j.jcmg.2019.02.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu LH, Betancur J, Sharir T, et al. Machine learning predicts per-vessel early coronary revascularization after fast myocardial perfusion SPECT: results from multicentre REFINE SPECT registry. Eur Heart J Cardiovasc Imaging. 2020;21(5):549–559. doi: 10.1093/ehjci/jez177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas M, Spertus JA, Kennedy KF, et al. Reasons for discordance between positron emission tomography (PET) myocardial perfusion imaging (MPI) results and subsequent management. J Nucl Cardiol. 2022;29(3):1109–1116. doi: 10.1007/s12350-021-02695-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel KK, McGhie AI, Kennedy KF, et al. Impact of Positron Emission Tomographic Myocardial Perfusion Imaging on Patient Selection for Revascularization. J Am Coll Cardiol. 2023;82(17):1662–1672. doi: 10.1016/j.jacc.2023.08.027 [DOI] [PubMed] [Google Scholar]
- 20.Sundboll J, Adelborg K, Munch T, et al. Positive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: a validation study. BMJ Open. 2016;6(11):e012832. doi: 10.1136/bmjopen-2016-012832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Helweg-Larsen K. The Danish Register of Causes of Death. Scand J Public Health. 2011;39(7 Suppl):26–29. doi: 10.1177/1403494811399958 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are not readily publicly available and cannot be shared according to Danish legislation but can be applied for at one of the Regions of Denmark, the WDHR, and Statistics Denmark. Programming code can be retrieved by request to the corresponding author.