Abstract
Objective
The aim of this study is to assess the latent profile types of marital adjustment in patients with breast cancer and to analyze the factors influencing these various profiles.
Methods
Patients with breast cancer who visited the Breast Surgery Department from January to June 2023 were selected using convenience sampling. These patients were surveyed using a general data questionnaire, the Revised Dyadic Adjustment Scale (RDAS), the Interpersonal Reactivity Index-C (IRI-C), and the Emotional Regulation Self-Efficacy Scale (RESS). Latent profile analysis (LPA) was used to determine different types of marital adjustment among patients, and influencing factors for the various profiles were identified through univariate analysis and multivariate logistic regression analysis.
Results
Marital adjustment in patients with breast cancer was categorized into three latent profiles: the “low marital adjustment-low cohesion group” (20.2%), the “midlevel marital adjustment group” (35.3%), and the “high marital adjustment-satisfaction group” (44.4%). The influencing factors included age, marital status, primary caregiver, type of surgical intervention, empathy, and emotional regulation self-efficacy (P < 0.05).
Conclusion
The marital adjustment levels of patients with breast cancer exhibited significant heterogeneity. Medical staff can implement targeted interventions based on the distinct characteristics of each marital adjustment profile, thereby enhancing the marital adjustment of these patients.
Keywords: breast cancer, emotional regulation self-efficacy, empathy, influencing factors, latent profile analysis, marital adjustment
Background
According to the 2022 global cancer data from the International Agency for Research on Cancer (IARC), breast cancer ranks second in global cancer incidence and is the most common malignancy among women.1 Advances in early screening and precision treatments have significantly improved survival rates, with the 5-year survival rate reaching as high as 80%,2 resulting in an increasing number of families living with cancer each year. Women undergoing breast cancer treatment often experience changes in body image, premature ovarian failure, and sexual dysfunction due to the impairment or loss of secondary sexual characteristics. These changes can significantly impact the marital relationship between patients having breast cancer and their spouses.3,4 Marital adjustment—the process by which couples establish common goals, achieve mutual satisfaction, and adapt to each other while maintaining their individual personalities over time—is a crucial metric for objectively assessing conjugal satisfaction and relationship quality.5,6 A healthy marital relationship serves as a vital resource and strategy, enhancing the physical and mental well-being of patients and their spouses, as well as their overall quality of life.7,8
As indicated by prior research, the marital status of breast cancer patients is concerning.9 The marital adjustment of breast cancer patients undergoing adjuvant chemotherapy in South Korea is reported to be low,9 and among Italian breast cancer patients, it was significantly lower than the global baseline.4 A systematic review highlights that the marital adjustment of breast cancer patients is closely related to their personality characteristics and psychosocial factors.6
Empathy10 encompasses an individual’s cognitive understanding and experiential grasp of others’ emotions, alongside the capacity to perceive, comprehend, and empathize with these emotions. The Relational-Focused Coping Model11 underscores the significance of emotional resonance and empathy between spouses as pivotal to enhancing joint coping mechanisms and marital quality. McDonald’s research12 demonstrates that empathy facilitates mutual understanding and encourages partners to express their negative emotions, thereby fostering intimacy. Emotional regulation self-efficacy, derived from self-efficacy theory, represents an individual’s confidence in effectively regulating their emotional states.13 According to Izard’s differentiated emotion theory,14 emotion constitutes a fundamental element of emotional experience, playing a critical role in the affective-cognitive system. Studies have indicated15 that emotional regulation self-efficacy is closely associated with interpersonal relationships. Individuals possessing higher emotional regulation self-efficacy are adept at regulating their own emotions, understanding others’ emotions, experiencing fewer interpersonal issues, and maintaining better intimate relationships.
However, the relationship between marital adjustment, empathy, and emotional regulation self-efficacy in breast cancer patients remains underexplored. Furthermore, most existing studies3,4 concentrate on aggregate scale scores, overlooking individual differences, which leads to suboptimal intervention outcomes16 and resource wastage.17 The aim of latent profiling18 is to categorize patients with similar traits into distinct subgroups to maximize inter-group differences and minimize intra-group variations. By analyzing the potential distribution ratios of categories, the study further investigates the characteristics of different groups. This study aims to: (1) identify diverse potential profiles of marital adjustment in breast cancer patients; and (2) examine the relationship between these profiles and empathy and emotional regulation self-efficacy.
Subjects and Methods
Subjects
Patients with breast cancer, who had visited the Breast Surgery Department of a tertiary class A hospital between January and June 2023, were selected through convenience sampling. Inclusion criteria comprised of patients who: (1) received a pathological diagnosis of breast cancer; (2) were married and cohabiting with their spouses; (3) were in stable health, defined as no major organ diseases, no new or recurrent tumors, good psychological well-being, and the ability to live independently and understand the questionnaire; and (4) expressed willingness to sign the informed consent. Exclusion criteria comprised of patients: (1) diagnosed with other malignancies; (2) concurrently enrolled in other scientific research endeavors during the same timeframe. A minimum of 240 samples were deemed necessary, considering a loss rate of 20%, as per the sample size calculations for LPA and logistic regression.19 A total of 272 questionnaires were distributed, of which 20 invalid questionnaires were excluded. Ultimately, 252 valid questionnaires were collected, resulting in a valid recovery rate of 92.6%. Approval of the study was obtained from the Ethics Committee of the hospital (2023-K066-01).
Survey Tools
General Data Questionnaire
The questionnaire, developed by the research team based on a comprehensive review of literature and group deliberations, encompassed social demographic data (such as age, marital status, education, employment status, monthly household income, place of residence, payment method, and primary caregiver) as well as disease-related information (including type of surgical intervention, disease duration, and cancer stage).
Revised Dyadic Adjustment Scale (RDAS)
The Revised Dyadic Adjustment Scale (RDAS), originally developed by Spanier5 and subsequently revised by Busby et al,20 comprises of 14 items categorized into three dimensions: marital consistency, marital cohesion, and marital satisfaction in its Chinese version. Using the Likert 6-level scoring method, each item (except for entry 11, which was scored on a 4–0 scale) was rated on a scale from 0 to 5 points. The total score ranged from 0 to 69 points, with higher scores indicating better marital adjustment capability in patients. The scale has strong internal consistency, with Cronbach’s α coefficient of 0.90 in the original study. This scale has been applied in Chinese breast cancer patients, and Cronbach’s α coefficient is 0.88.21 In our study, Cronbach’s α coefficient was 0.926.
Interpersonal Reactivity Index-C (IRI-C)
The Interpersonal Reactivity Index-Chinese version (IRI-C), as revised by Zhang et al, was used to assess the empathy levels of the participants.22 This scale comprises of 22 items distributed across four dimensions: perspective-taking, personal distress, fantasy, and empathic concern. Each item was rated on a Likert 5-level scale, ranging from “inappropriate” to “very appropriate”, with scores ranging from 0 to 4 points. The total score ranged from 0 to 88 points, with higher scores indicating greater levels of empathy among the subjects. This scale has been applied in Chinese breast cancer patients, and Cronbach’s α coefficient is 0.86.23 In this study, the Cronbach’s α coefficient for patients with breast cancer was 0.904.
Emotional Regulation Self-Efficacy Scale (RESS)
The Emotional Regulation Self-Efficacy Scale (RESS), translated into Chinese by Wen et al, was used to assess the emotional regulation abilities of the participants.24 This scale comprises of 12 items categorized into three dimensions: positive emotion expression efficacy, pain/depression regulation efficacy, and anger/irritability regulation efficacy. Participants rated each item on a Likert 5-level scale, ranging from “strongly disagree” to “strongly agree”, with scores ranging from 1 to 5 points. The total score ranged from 12 to 60 points, with higher scores indicating stronger emotional regulation abilities. This scale has been applied to patients with chronic diseases in China, and Cronbach’s α coefficient is 0.788.25 In our study, the Cronbach’s α coefficient for the scale was 0.803.
Data Collection Method
Prior to data collection, one project leader and three researchers underwent uniform training, during which 20 questionnaires were completed for a pre-survey. During the formal survey, researchers elucidated the objectives and significance of the study to the patients and emphasized the importance of maintaining confidentiality. Upon signing informed consent forms, patients were instructed to independently complete the questionnaire based on their actual circumstances. Researchers provided assistance and conducted interviews if patients encountered difficulties in completing the questionnaire. Completed questionnaires were immediately reviewed by the researchers, and patients were prompted to provide any missing information. The original data were meticulously verified by two researchers and entered into Excel, after which two more researchers conducted a secondary check.
Statistical Method
Data analysis was conducted using SPSS 27.0 and Mplus 8.3. Categorical data were presented as frequencies and percentages (%) and compared between groups using the chi-square test. Continuous data with a normal or approximately normal distribution were described as  and compared between groups using analysis of variance. By using the score for each item of marital adjustment as the manifest indicator, LPA was performed to fit 1–4 profile models sequentially. Model fit indices included the Akaike information criterion (AIC), Bayesian information criterion (BIC), and adjusted BIC (aBIC), as well as Entropy, Lo-Mendell-Rubin likelihood ratio (LMR), and Bootstrap likelihood ratio test (BLRT).26 Lower values of AIC, BIC, and aBIC indicated a better fit, while an Entropy value closer to 1 indicated more precise classification. LMR and BLRT (P < 0.05) indicated that the k models were superior to the k-1 models.27 However, the optimal model was determined based on the sample size of each profile and its actual significance. Multivariate logistic regression analysis was used to analyze the influencing factors of different marital adjustment classes in patients with breast cancer, with a significance level set at α = 0.05.
and compared between groups using analysis of variance. By using the score for each item of marital adjustment as the manifest indicator, LPA was performed to fit 1–4 profile models sequentially. Model fit indices included the Akaike information criterion (AIC), Bayesian information criterion (BIC), and adjusted BIC (aBIC), as well as Entropy, Lo-Mendell-Rubin likelihood ratio (LMR), and Bootstrap likelihood ratio test (BLRT).26 Lower values of AIC, BIC, and aBIC indicated a better fit, while an Entropy value closer to 1 indicated more precise classification. LMR and BLRT (P < 0.05) indicated that the k models were superior to the k-1 models.27 However, the optimal model was determined based on the sample size of each profile and its actual significance. Multivariate logistic regression analysis was used to analyze the influencing factors of different marital adjustment classes in patients with breast cancer, with a significance level set at α = 0.05.
Results
General Data of Patients with Breast Cancer and Current Status of Marital Adjustment
In this study, a total of 252 patients with breast cancer were included, and the general data of these patients are presented in Table 1. The average RDAS score among patients with breast cancer was (47.88 ± 10.85) points.
Table 1.
General Data of Patients with Breast Cancer and Univariate Analysis of Their Latent Profiles of Marital Adjustment [Case (Percentage, %)]
| Variable | Case [Case (Percentage, %)] (n = 252) | Low Marital Adjustment-Low Cohesion Group (n = 51) | Middle Marital Adjustment Group (n = 89) | High Marital Adjustment-Satisfaction group (n = 112) | χ2 value | P | |
|---|---|---|---|---|---|---|---|
| Age | < 40 years | 77 (30.6) | 28 (54.9) | 22 (24.7) | 27 (24.1) | 20.974 | <0.001 |
| 40 years~ | 120 (47.6) | 12 (23.5) | 50 (56.2) | 58 (51.8) | |||
| ≥ 56 years | 55 (21.8) | 11 (21.6) | 17 (19.1) | 27 (24.1) | |||
| Marriageable age | < 10 years | 143 (56.7) | 22 (43.1) | 38 (42.7) | 83 (74.1) | 26.608 | <0.001 |
| 10 years~ | 44 (17.5) | 9 (17.6) | 21 (23.6) | 14 (12.5) | |||
| ≥ 21 years | 65 (25.8) | 20 (39.2) | 30 (33.7) | 15 (13.4) | |||
| Course of disease | < 1 year | 55 (21.8) | 22 (43.1) | 23 (25.8) | 10 (8.9) | 26.602 | <0.001 |
| 1 year~ | 101 (40.1) | 18 (35.3) | 33 (37.1) | 50 (44.6) | |||
| > 3 years | 96 (38.1) | 11 (21.6) | 33 (37.1) | 52 (46.4) | |||
| Education | Junior high school and below | 44 (17.5) | 21 (41.2) | 15 (16.9) | 8 (7.1) | 32.584 | <0.001 |
| Senior high school or junior college | 118 (46.8) | 23 (45.1) | 40 (44.9) | 55 (49.1) | |||
| Bachelor degree and above | 90 (35.7) | 7 (13.7) | 34 (38.2) | 49 (43.8) | |||
| Payment | Medical insurance | 168 (66.7) | 36 (70.6) | 59 (66.3) | 73 (65.2) | 0.47 | 0.791 |
| Agricultural insurance | 84 (33.3) | 15 (29.4) | 30 (33.7) | 39 (34.8) | |||
| Main caregiver | Other | 102 (40.5) | 41 (80.4) | 52 (58.4) | 9 (8.0) | 94.552 | <0.001 |
| Spouse | 150 (59.5) | 10 (19.6) | 37 (41.6) | 103 (92.0) | |||
| Residence | Rural area | 165 (65.5) | 38 (74.5) | 58 (65.2) | 69 (61.6) | 2.587 | 0.274 |
| Urban area | 87 (34.5) | 13 (25.5) | 31 (34.8) | 43 (38.4) | |||
| Per-capita income | < RMB 5000 | 90 (35.7) | 22 (43.1) | 34 (38.2) | 34 (30.4) | 3.895 | 0.42 |
| RMB 5000~ | 118 (46.8) | 19 (37.3) | 40 (44.9) | 59 (52.7) | |||
| ≥ RMB 8000 | 44 (17.5) | 10 (19.6) | 15 (16.9) | 19 (16.9) | |||
| Operation mode | Modified radical correction | 123 (48.8) | 32 (62.7) | 36 (40.4) | 55 (49.1) | 6.457 | 0.04 |
| Breast conserving/ reconstruction | 129 (51.2) | 19 (37.3) | 53 (59.6) | 57 (50.9) | |||
| Disease stage | Endocrine therapy | 80 (31.7) | 27 (52.9) | 28 (31.5) | 25 (22.3) | 18.799 | <0.001 |
| No therapy | 84 (33.3) | 16 (31.4) | 25 (28.1) | 43 (38.4) | |||
| Radiotherapy/ chemotherapy/ targeted therapy | 88 (34.9) | 8 (15.7) | 36 (40.4) | 44 (39.3) | |||
| Employment status | Unemployed | 113 (44.8) | 22 (43.1) | 37 (41.6) | 54 (48.2) | 4.332 | 0.363 |
| Retired | 77 (30.6) | 19 (37.3) | 24 (26.9) | 34 (30.4) | |||
| Employed | 62 (24.6) | 10 (19.6) | 28 (31.5) | 24 (21.4) | |||
LPA results of Marital Adjustment in Patients with Breast Cancer
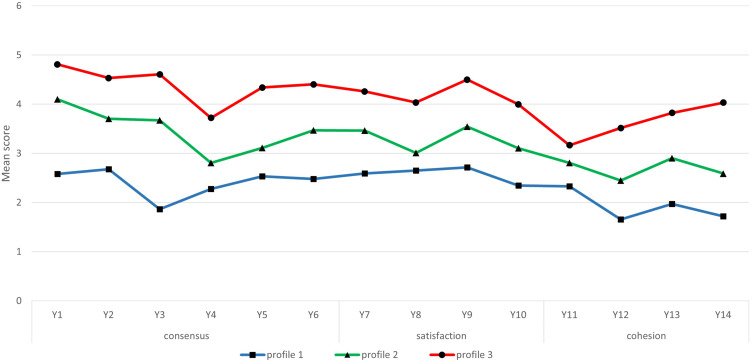
Four latent profile models were fitted in this study. Table 2 illustrates the potential profiles of marital adjustment among breast cancer patients. With an increasing number of categories, the values of AIC, BIC, and aBIC decrease. Although model 2 exhibits the highest Entropy value, the Entropy values of other models exceed 0.9, with model 4’s LMR presenting a P-value of 0.447. Therefore, upon comprehensive consideration of these metrics, it emerges as the optimal model. Figure 1 depicts a model comprising three profiles, with each category named according to the scoring outcomes of the scale items. The three identified profiles are: low marital adjustment-low cohesion group (Profile 1, 20.2%), moderate marital adjustment group (Profile 2, 35.3%), and high marital adjustment- satisfaction group (Profile 3, 44.4%).
Table 2.
Fitting Index for the Latent Profile Model of the Marital Adjustment of Patients with Breast Cancer
| Class Model | AIC | BIC | aBIC | Entropy | P (LMR) | P (BLRT) | Class Proportion |
|---|---|---|---|---|---|---|---|
| 1 | 10403.562 | 10502.386 | 10413.622 | – | – | – | – |
| 2 | 9121.222 | 9272.988 | 9136.671 | 0.957 | <0.001 | <0.001 | 46%/54% |
| 3 | 8790.981 | 8995.688 | 8811.819 | 0.925 | 0.006 | <0.001 | 20.2%/35.3%/44.4% |
| 4 | 8631.631 | 8889.280 | 8657.859 | 0.945 | 0.447 | <0.001 | 7.5%/29.8%/17.1%/45.6% |
Figure 1.
Item-response mean scores for the 3-profile marriage adjustment model. The X-axis represents the marital adjustment items. Items 1–6 belong to consensus, items 7–10 belong to satisfaction, and items 11–14 belong to cohesion.
Profile 1: Patients in this category scored lower across all marital adjustment items compared to the other two groups and exhibited significantly lower scores in the “cohesion” dimension relative to the “consistency” and “satisfaction” dimensions. Accordingly, this category was named the “low marital adjustment-low cohesion group”, encompassing 51 individuals (20.2%).
Profile 2: Patients in this category had marital adjustment scores intermediate between the other groups, leading to its designation as the “moderate marital adjustment group”, comprising 89 patients (35.3%).
Profile 3: Patients in this category scored higher on all marital adjustment items compared to the other groups and demonstrated significantly higher scores in the “satisfaction” dimension. Thus, this category was termed the “high marital adjustment - satisfaction group”, including 112 individuals (44.4%).
Univariate Analysis on the LPA of Marital Adjustment in Patients with Breast Cancer
The marital adjustment score of breast cancer patients in the “low marital adjustment-low cohesion group” was (40.12±10.72), the score in the “medium marital adjustment group” was (46.17±9.17), and the score in the “high marital adjustment - satisfaction group” was (52.92±9.64), with statistically significant differences observed between the groups (F=32.79, P<0.001). There were also statistically significant differences in age, age at marriage, disease duration, education level, primary caregiver, mode of operation, stage of disease, empathy, and emotional regulation self-efficacy among the three different potential profiles of breast cancer patients (P < 0.05). Further details are provided in Tables 1 and 3.
Table 3.
Comparing the Regulatory Emotional Self-Efficacy and Empathy of Patients with Breast Cancer Across Various Latent Profiles  , n = 252, Point
, n = 252, Point
| Variable | Low Marital Adjustment-Low Cohesion Group (C1) | Midlevel Marital Adjustment Group (C2) | High Marital Adjustment-Satisfaction Group (C3) | Pairwise Comparison | F | P |
|---|---|---|---|---|---|---|
| Empathy | 43.25±12.19 | 55.13±9.52a | 70.12±6.89a,b | C1<C2<C3 | 82.97 | <0.001 |
| Regulatory emotional self-efficacy | 32.69±6.77 | 38.56±6.87a | 42.21±4.99a,b | C1<C2<C3 | 36.99 | <0.001 |
Notes: arepresents compared with layer 1, P < 0.05; brepresents compared with layer 2, P < 0.05.
Multivariate Analysis on the Latent Profiles of Patients with Breast Cancer
Three potential profiles of breast cancer patients were taken as dependent variables (with “low marital adjustment-low cohesion group” as reference), and variables with statistical significance in the univariate analysis were taken as independent variables. The values of independent variables were shown in Table 4. Logistic regression analysis results showed that, Age, age of marriage, primary caregiver, mode of surgery, empathy, emotional regulation self-efficacy were the factors influencing the potential profile of marital adjustment in breast cancer patients. Age < 40 years old, marriage age < 10 years, primary caregiver is non-spouse and modified radical surgery is more likely to belong to the “low marital adjustment-low cohesion group”. The higher the scores of empathy and emotion regulation self-efficacy, the more likely they are to be classified into the medium marital adjustment group and the high marital adjustment satisfaction group. The results are shown in Table 5.
Table 4.
Mode of Assignment of Independent Variables
| Variable | Assignment Mode |
|---|---|
| Age | < 40 years = 1, 40 years~ =1, ≥ 56 years = 3, taking “≥ 56 years” as reference |
| Marriageable age | < 10 years = 1, 10 years~ = 2, ≥ 21 years = 3, taking “≥ 21 years” as reference |
| Course of disease | < 1 year = 1, 1 year~ = 2, > 3 years = 3, taking “≥ 3 years” as reference |
| Education | Junior high school and below = 1, senior high school or junior college = 2, bachelor’s degree and above = 3, taking “bachelor’s degree and above” as reference |
| Main caregiver | Other = 1, spouse = 3, taking “spouse” as reference |
| Operation mode | Modified radical correction = 1, breast conserving/reconstruction = 3, taking “breast conserving/reconstruction” as reference |
| Disease stage | Endocrine therapy = 1, no therapy = 2, radiotherapy/chemotherapy/targeted therapy = 3, taking “radiotherapy/chemotherapy/targeted therapy” as reference |
Table 5.
Multivariate Logistic Regression Analysis on the Latent Profile of Marital Adjustment in Patients with Breast Cancer
| Item | Midlevel Marital Adjustment Groupa | High Marital Adjustment-Satisfaction Groupa | ||||
|---|---|---|---|---|---|---|
| β | P | OR (95% CI) | β | P | OR (95% CI) | |
| Constant term | −13.302 | <0.001 | – | −35.267 | <0.001 | – |
| Age | ||||||
| < 40 years | −3.171 | 0.016 | 0.042 (0.003–0.555) | −4.563 | 0.008 | 0.01 (0–0.301) |
| 40 years~ | 2.612 | 0.027 | 13.62 (1.342–138.355) | 1.482 | 0.293 | 4.4 (0.278–69.525) |
| Marriageable age | ||||||
| <10 years | −2.152 | 0.023 | 0.116 (0.018–0.74) | −0.876 | 0.476 | 0.417 (0.037–4.635) |
| Main caregiver | ||||||
| Not the spouse | −1.485 | 0.065 | 0.227 (0.047–1.098) | −4.602 | <0.001 | 0.01 (0.001–0.076) |
| Operation mode | ||||||
| Modified radical correction | −2.827 | 0.015 | 0.059 (0.006–0.583) | −1.969 | 0.137 | 0.140(0.010–1.872) |
| Empathy | 0.241 | <0.001 | 1.273 (1.135–1.428) | 0.481 | <0.001 | 1.617 (1.4–1.868) |
| Regulatory emotional self-efficacy | 0.185 | 0.002 | 1.203 (1.349–0.185) | 0.343 | <0.001 | 1.409 (1.218–1.631) |
Note: arepresents that the low marital adjustment-low cohesion group is taken as reference.
Discussion
Our study identified three distinct categories of marital adjustment in breast cancer patients through latent profile analysis, assessing the influencing factors of these categories and their associations with empathy and emotional regulation self-efficacy. Consistent with prior research, the majority of breast cancer patients exhibited moderate to low levels of marital adjustment.
This study classified 20.2% of breast cancer patients into the “low marital adjustment - low cohesion group” (Profile 1), where scores for each item were the lowest across all categories. This suggests that individuals in this group experience significant marital adjustment challenges, particularly in emotional connectivity and the alignment of thoughts and actions. For these patients, couple-based interventions are recommended to facilitate effective expression and understanding of each other’s feelings and needs, and to encourage sharing of interests and hobbies, thereby enhancing marital cohesion. 35.3% of patients fell into the “moderate marital adjustment group” (Profile 2), with item 12 receiving the lowest score, indicating that they were able to cope with the binary relationship after illness to some extent, but still faced insurmountable disease limitations. 44.4% of patients were categorized into the “high marital adjustment-satisfaction group” (Profile 3), with higher scores across all items, signifying superior overall marital adjustment. Therefore, through potential profile analysis, identifying patient subgroups, analyzing each category’s characteristics, formulating targeted intervention strategies, and implementing stratified interventions can enhance intervention precision and improve marital adjustment among breast cancer patients.
This study demonstrates that patients under 40 years of age are more likely to fall into the group characterized by “low marital adjustment-low cohesion”, a finding that aligns with the conclusions of Ganz et al.28 It is likely due to the fact that breast cancer treatment represents a long-term process, with surgery, chemoradiotherapy, and endocrine therapy resulting in changes to physical appearance and hormone levels. Younger breast cancer patients tend to be more susceptible to psychological and emotional stress.29 Furthermore, for younger patients, managing the disease while addressing career, family, and fertility issues30,31 can result in a heightened sense of burden within the marital relationship. Compared with the moderate marital adjustment group, patients whose marriage has lasted less than 10 years are more likely to be classified into the “low marital adjustment-low cohesion” group (P < 0.05), aligning with the findings of Avci et al.32 This may be attributed to the significant physical and emotional impacts associated with breast cancer diagnosis and treatment. Patients in relatively new marriages have often not yet established a stable family foundation. Marriage and family constitute the most critical sources of social support for breast cancer patients, with spouses offering companionship, understanding, and emotional support. This support plays a crucial role in enabling patients to actively confront disease challenges.33 For patients in shorter marriages, insufficient time to adapt to the changes induced by the disease renders coping with breast cancer stress more challenging, adversely affecting the marital. In addition, when compared to the high marital adjustment-satisfaction group, patients with a non-spouse as their primary caregiver are more likely to be categorized into the low marital adjustment-low cohesion group (P < 0.05), echoing the findings of Choi et al.34 Marital quality improves for individuals receiving care from their spouse, likely because spouses have a deeper understanding of each other through shared life experiences. A heightened sense of mutual understanding and shared experiences can deepen the bond and trust between partners, enhancing their collective resilience against the disease.35 During breast cancer treatment and rehabilitation, having a spouse as the primary caregiver usually facilitates more effective communication between partners, enabling a deeper understanding of each other’s needs and emotions,36 thereby fostering stronger emotional bonds. The results indicated that, in comparison to the medium marital adjustment group, patients undergoing modified radical surgery had a higher likelihood of being classified into the low marital adjustment-low cohesion group (P < 0.05). Consistent with Alinejad et al,37 breast-conserving or reconstructive surgery can assist in maintaining patients’ body image and minimizing the impact on their self-esteem. This approach helps keep patients positive;38 furthermore, it facilitates closer physical intimacy between patients and their spouses,38 contributing to the stability of the marital relationship. In summary, it is recommended that healthcare professionals focus on patients of younger age and those in earlier stages of marriage, tailoring health education and intervention programs to the diverse characteristics of patients, and offering psychological support and joint coping strategies for couples, emphasizing the significance of family support in aiding patients to more effectively confront the challenges posed by the disease. Additionally, healthcare professionals should offer support in treatment decisions to alleviate the dilemma of surgical method selection, thereby enabling the establishment of a positive body image and fostering positive marital adjustment.39
This study identified empathy and emotional regulation self-efficacy as protective factors in marital adjustment. Increased empathic abilities correlate with a higher likelihood of patients being classified into the moderate or high marital adjustment-satisfaction groups, aligning with findings from Todi et al.40 Patients possessing heightened empathic abilities can more thoroughly and deeply comprehend the emotional needs of both spouses, facilitating effective communication, thereby more readily receiving care, attention, and effective emotional support from their spouse. This enhancement in family cohesion aids patients in more effectively managing the emotional distress associated with the disease, thereby fostering stability in the marital relationship and enhancing marital satisfaction. Regression analysis results further indicate that emotional regulation self-efficacy significantly influences the potential profiles of marital adjustment among breast cancer patients. As emotional regulation self-efficacy improves, patients increasingly align with the moderate or high marital adjustment-satisfaction groups, mirroring observations by Javed et al.41 Facing the significant life event of cancer, breast cancer patients with high emotional regulation self-efficacy are apt to adopt positive emotional regulation strategies, proactively manage disease stress, mitigate negative emotional perceptions, and consequently enhance the family atmosphere, furthering marital coordination and stability.42 Consequently, family-based dual interventions for breast cancer patients can be implemented,43 including partner support groups, family rehabilitation initiatives, cognitive-behavioral therapy, and emotional regulation strategy training. Such as training in listening, feedback, expression, empathy skills, and emotional vocabulary education, assist in more precisely expressing and comprehending emotions. To promote effective emotional expression and empathy between breast cancer patients and their partners, thereby enhancing their ability to navigate cancer’s relational challenges.
Limitations and Future Research
First, the cross-sectional design of this study does not permit causal inference. Future studies should include longitudinal data for each stage of the disease to more fully explain the dynamic changes to marital adjustment. Second, the sample was taken from a single medical institution, which may limit the generalizability of the findings. Future studies should expand the sample size and conduct cross-cultural adaptation. Third, the data in this study were derived from patients’ self-reports. Although statistical analysis confirmed no methodological bias, reporting bias may still exist, potentially affecting the accuracy of the results. Various data collection methods, such as in-depth interviews and behavioral observations, could be used in the future to gain a more complete understanding of the marital relationships of breast cancer patients. Fourth, this study may not cover all variables that affect the marital relationship of breast cancer patients, such as data from spouses. Future studies should collect dyadic data to build a subjective and objective-dependent mediation model to more fully understand the interaction in the couple relationship.
Conclusion
This study highlights variations in marital adjustment among breast cancer patients, offering a more nuanced understanding of socio-demographic and disease-related factors. Using latent profile analysis, the study classified marital adjustment into three distinct groups: low marital adjustment-low cohesion, medium marital adjustment-low cohesion, and high marital adjustment-satisfaction. The high marital adjustment-satisfaction group accounted for the largest proportion, while the low marital adjustment-low cohesion group was the smallest. Notably, most patients in the latter group were younger and faced greater psychological pressure, warranting increased attention from healthcare providers. Furthermore, factors such as age at marriage, primary caregiver, mode of surgery, empathy, and emotional regulation self-efficacy were significant predictors of marital adjustment profile subgroups. Caregivers should recognize the distinct characteristics of patients in each group early on and apply targeted interventions based on relevant predictors. In particular, for patients with low levels of marital adjustment, enhancing various skills and implementing integrated couple-based interventions within the family unit are crucial.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff who implemented the intervention and evaluation components of the study.
Funding Statement
Science and Technology Project of Affiliated Hospital of Nantong University (Tfh2212); Research Project of Nantong Municipal Health Commission (QNZ2023016); Social and People’s Livelihood Science and Technology Projects of Nantong (MS22022063); Nantong “14th Five-Year Plan” Science and Education Health Enhancement Project Young Medical Key Talents Project.
Abbreviations
RDAS, Revised Dyadic Adjustment Scale; IRI-C, Interpersonal Reactivity Index-C; RESS, Emotional Regulation Self-Efficacy Scale; LPA, Latent profile analysis; AIC, Akaike information criterion; BIC, Bayesian information criterion; aBIC, adjusted BIC; LMR, Lo-Mendell-Rubin likelihood ratio; BLRT, Bootstrap likelihood ratio test.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of the Affiliated Hospital of Nantong University (2023-K066-01). This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74(3):229–263. doi: 10.3322/caac.21834 [DOI] [PubMed] [Google Scholar]
- 2.Ong SK, Haruyama R, Yip CH, et al. Feasibility of monitoring global breast cancer initiative framework key performance indicators in 21 asian national cancer centers alliance member countries. Eclinicalmedicine. 2024;67:102365. doi: 10.1016/j.eclinm.2023.102365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Telli S, Gurkan A. Examination of sexual quality of life and dyadic adjustment among women with mastectomy. Eur J Breast Health. 2020;16(1):48–54. doi: 10.5152/ejbh.2019.4969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Di Mattei VE, Perego G, Taranto P, et al. The long-term effects of cancer treatment on sexuality and couple relationships. Fam Process. 2021;60(3):853–865. doi: 10.1111/famp.12604 [DOI] [PubMed] [Google Scholar]
- 5.Spanier GB, Cole CL. Toward clarification and investigation of marital adjustment. Int J Sociol Family. 1976;6(1):121–146. [Google Scholar]
- 6.Brandão T, Pedro J, Nunes N, et al. Marital adjustment in the context of female breast cancer: a systematic review. Psychooncology. 2017;26(12):2019–2029. doi: 10.1002/pon.4432 [DOI] [PubMed] [Google Scholar]
- 7.Smith TW. Intimate relationships and coronary heart disease: implications for risk, prevention, and patient management. Curr Cardiol Rep. 2022;24(6):761–774. doi: 10.1007/s11886-022-01695-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruiz-Marin CM, Molina-Barea R, Slim M, et al. Marital adjustment in patients with cancer: association with psychological distress, quality of life, and sleep problems. Int J Environ Res Public Health. 2021;18(13):7089. doi: 10.3390/ijerph18137089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee H, Yoon HG. Body change stress, sexual function, and marital intimacy in Korean patients with breast cancer receiving adjuvant chemotherapy: a cross-sectional study. Asia Pac J Oncol Nurs. 2023;10(5):100228. doi: 10.1016/j.apjon.2023.100228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gambin M, Sharp C. The relations between empathy, guilt, shame and depression in inpatient adolescents. J Affect Disord. 2018;241:381–387. doi: 10.1016/j.jad.2018.08.068 [DOI] [PubMed] [Google Scholar]
- 11.O’Brien TB, DeLongis A. The interactional context of problem-, emotion-, and relationship-focused coping: the role of the big five personality factors. J Pers. 1996;64(4):775–813. doi: 10.1111/j.1467-6494.1996.tb00944.x [DOI] [PubMed] [Google Scholar]
- 12.McDonald JE, Olson JR, Lanning AH, et al. Effects of religiosity, forgiveness, and spousal empathy on marital adjustment. Marriage Fam Rev. 2018;54(4):393–416. doi: 10.1080/01494929.2017.1403992 [DOI] [Google Scholar]
- 13.Liu B, Yang T, Xie W. Emotional regulation self-efficacy influences moral decision making: a non-cooperative game study of the new generation of employees. Int J Environ Res Public Health. 2022;19(23):16360. doi: 10.3390/ijerph192316360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Izard CE, Malatesta CZ. Perspectives on emotional development. In: Osofsky JD, editor. Handbook of Infant Development. 2nd ed. New York: Wiley; 1987:494–554. [Google Scholar]
- 15.Zamir O, Lavee Y. Emotional regulation and revictimization in women’s intimate relationships. J Interpers Violence. 2016;31(1):147–162. doi: 10.1177/0886260514555125 [DOI] [PubMed] [Google Scholar]
- 16.Price-Blackshear MA, Pratscher SD, Oyler DL, et al. Online couples mindfulness-based intervention for young breast cancer survivors and their partners: a randomized-control trial. J Psychosoc Oncol. 2020;38(5):592–611. doi: 10.1080/07347332.2020.1778150 [DOI] [PubMed] [Google Scholar]
- 17.Fergus K, Ahmad S, Gardner S, et al. Couplelinks online intervention for young couples facing breast cancer: a randomised controlled trial. Psychooncology. 2022;31(3):512–520. doi: 10.1002/pon.5836 [DOI] [PubMed] [Google Scholar]
- 18.Yang Q, Zhao A, Lee C, et al. Latent profile/class analysis identifying differentiated intervention effects. Nurs Res. 2022;71(5):394–403. doi: 10.1097/NNR.0000000000000597 [DOI] [PubMed] [Google Scholar]
- 19.Wang M, Bi X. Latent Variable Modeling and Mplus Applications - Advanced Section. Chongqing: Chongqing University Press; 2018:13–15. [Google Scholar]
- 20.Busby DM, Christensen C, Crane DR, et al. A revision of the dyadic adjustment scale for use with distressed and nondistressed couples: construct hierarchy and multidimensional scales. J Marital Fam Ther. 1995;21(3):289–308. doi: 10.1111/j.1752-0606.1995.tb00163.x [DOI] [Google Scholar]
- 21.Yang J, Yuan X, Wu Y, et al. Current status and influencing factors of postoperative marital adjustment in patients with breast cancer. Chin J Mod Nurs. 2021;27(15):2039–2044. [Google Scholar]
- 22.Zhang F, Dong Y, Wang K, et al. Reliability and validity of the Chinese version of the lnterpersonal reactivity index-c. Chin J Clin Psychol. 2010;18(02):155–157. [Google Scholar]
- 23.Li L, Chen L, Wu C. Interaction influence of conjugal empathy on self disclosure and intimate relationship in young breast cancer patients and spouses. J Nurs Sci. 2022;37(18):75–78. [Google Scholar]
- 24.Wen S, Tang D, Yu G. The characteristics of regulatory emotional self-efficacy in Chinese graduate students. J Psychol Sci. 2009;32(03):666–668. [Google Scholar]
- 25.Wang Y, Wang D. The status quo of experiential avoidance and the analysis of influencing factors in elderly patients with hypertension in rural areas. Chin Nurs res. 2022;36(03):408–412. [Google Scholar]
- 26.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a monte carlo simulation study. Struct Equ Model. 2007;14(4):535–569. doi: 10.1080/10705510701575396 [DOI] [Google Scholar]
- 27.Kim SY. Determining the number of latent classes in single- and multi-phase growth mixture models. Struct Equation Model. 2014;21(2):263–279. doi: 10.1080/10705511.2014.882690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ganz PA, Rowland JH, Desmond K, et al. Life after breast cancer: understanding women’s health-related quality of life and sexual functioning. J Clin Oncol. 1998;16(2):501–514. doi: 10.1200/JCO.1998.16.2.501 [DOI] [PubMed] [Google Scholar]
- 29.Hasan S, Chew KS, Balang RV, et al. Beyond the scars: a qualitative study on the experiences of mastectomy among young women with breast cancer in a country with crisis. Bmc Women's Health. 2023;23(1):596. doi: 10.1186/s12905-023-02734-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jäkel K, Richter D, Leuteritz K, et al. Sexuality, fertility, family planning, family life, and partnership in young breast cancer patients: a longitudinal study. Front Psychol. 2023;14:1127359. doi: 10.3389/fpsyg.2023.1127359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raque-Bogdan TL, Hoffman MA, Ginter AC, et al. The work life and career development of young breast cancer survivors. J Couns Psychol. 2015;62(4):655–669. doi: 10.1037/cou0000068 [DOI] [PubMed] [Google Scholar]
- 32.Avci IA, Kumcagiz H. Marital adjustment and loneliness status of women with mastectomy and husbands reactions. Asian Pac J Cancer Prev. 2011;12(2):453–459. [PubMed] [Google Scholar]
- 33.Boamah MA, Adamu B, Mensah KB, et al. Exploring the social stressors and resources of husbands of women diagnosed with advanced breast cancer in their role as primary caregivers in Kumasi, Ghana. Support Care Cancer. 2021;29(5):2335–2345. doi: 10.1007/s00520-020-05716-2 [DOI] [PubMed] [Google Scholar]
- 34.Choi H. Giving or receiving spouse care and marital satisfaction among older Korean individuals. Soc Sci Med. 2021;272:112071. doi: 10.1016/j.socscimed.2018.12.012 [DOI] [PubMed] [Google Scholar]
- 35.Noveiri M, Shamsaei F, Khodaveisi M, et al. The concept of coping in male spouses of Iranian women with breast cancer: a qualitative study using a phenomenological approach. Can Oncol Nurs J. 2021;31(3):314–321. doi: 10.5737/23688076313314321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krok D, Telka E, Moroń M. Marital satisfaction, partner communication, and illness acceptance among couples coping with breast cancer: a dyadic approach. Psychooncology. 2023;32(8):1240–1247. doi: 10.1002/pon.6174 [DOI] [PubMed] [Google Scholar]
- 37.Alinejad MS, Fernandez R, Lord H, et al. The impact of mastectomy on Iranian women sexuality and body image: a systematic review of qualitative studies. Support Care Cancer. 2021;29(10):5571–5580. doi: 10.1007/s00520-021-06153-5 [DOI] [PubMed] [Google Scholar]
- 38.Salafuddin MF, Yarso KY, Nugroho HA, et al. Breast conserving surgery is better for sexual satisfaction compared to a modified radical mastectomy for breast cancer. Asian Pac J Cancer Prev. 2023;24(6):2083–2088. doi: 10.31557/APJCP.2023.24.6.2083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tunç E, Sevcan OO, Işeri Ö. The effect of acceptance and commitment therapy-based psychoeducation on body image, quality of sexual life, and dyadic adjustment of women after breast cancer surgery. Oncol Nurs Forum. 2023;50(5):599–609. doi: 10.1188/23.ONF.599-609 [DOI] [PubMed] [Google Scholar]
- 40.Todić I, Šakotić-kurbalija J, Trifunović-Marinković B. The contribution of dyadic empathy to the perception of the relationship quality. Psiholoska Istrazivanja. 2022;25(1):21–35. doi: 10.5937/PSISTRA25-31604 [DOI] [Google Scholar]
- 41.Javed F, Ahmad M, Nasar Iqbal M. Resilience and emotional regulation predicting marital satisfaction in females diagnosed with polycystic ovarian syndrome (pcos). Pak-Euro J Med Life Sci. 2022;5(2):391–398. doi: 10.31580/pjmls.v5i2.2572 [DOI] [Google Scholar]
- 42.Horn AB, Zimmerli L, Maercker A, et al. The worse we feel, the more intensively we need to stick together: a qualitative study of couples’ emotional co-regulation of the challenge of multimorbidity. Front Psychol. 2023;14:1213927. doi: 10.3389/fpsyg.2023.1213927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nicolaisen A, Hagedoorn M, Hansen DG, et al. The effect of an attachment-oriented couple intervention for breast cancer patients and partners in the early treatment phase: a randomised controlled trial. Psychooncology. 2018;27(3):922–928. doi: 10.1002/pon.4613 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.