Abstract
Background
Adjustment disorders are a frequent cause of sick leave and various interventions have been developed to expedite the return to work (RTW) of individuals on sick leave due to adjustment disorders.
Objectives
To assess the effects of interventions facilitating RTW for workers with acute or chronic adjustment disorders.
Search methods
We searched the Cochrane Depression, Anxiety and Neurosis Review Group's Specialised Register (CCDANCTR) to October 2011; the Cochrane Central Register of Controlled Trials (CENTRAL) to Issue 4, 2011; MEDLINE, EMBASE, PsycINFO and ISI Web of Science, all years to February 2011; the WHO trials portal (ICTRP) and ClinicalTrials.gov in March 2011. We also screened reference lists of included studies and relevant reviews.
Selection criteria
We selected randomised controlled trials (RCTs) evaluating the effectiveness of interventions to facilitate RTW of workers with adjustment disorders compared to no or other treatment. Eligible interventions were pharmacological interventions, psychological interventions (such as cognitive behavioural therapy (CBT) and problem solving therapy), relaxation techniques, exercise programmes, employee assistance programmes or combinations of these interventions. The primary outcomes were time to partial and time to full RTW, and secondary outcomes were severity of symptoms of adjustment disorder, work functioning, generic functional status (i.e. the overall functional capabilities of an individual, such as physical functioning, social function, general mental health) and quality of life.
Data collection and analysis
Two authors independently selected studies, assessed risk of bias and extracted data. We pooled studies that we deemed sufficiently clinically homogeneous in different comparison groups, and assessed the overall quality of the evidence using the GRADE approach.
Main results
We included nine studies reporting on 10 psychological interventions and one combined intervention. The studies included 1546 participants. No RCTs were found of pharmacological interventions, exercise programmes or employee assistance programmes. We assessed seven studies as having low risk of bias and the studies that were pooled together were comparable. For those who received no treatment, compared with CBT, the assumed time to partial and full RTW was 88 and 252 days respectively. Based on two studies with a total of 159 participants, moderate‐quality evidence showed that CBT had similar results for time (measured in days) until partial RTW compared to no treatment at one‐year follow‐up (mean difference (MD) ‐8.78, 95% confidence interval (CI) ‐23.26 to 5.71). We found low‐quality evidence of similar results for CBT and no treatment on the reduction of days until full RTW at one‐year follow‐up (MD ‐35.73, 95% CI ‐113.15 to 41.69) (one study with 105 participants included in the analysis). Based on moderate‐quality evidence, problem solving therapy (PST) significantly reduced time until partial RTW at one‐year follow‐up compared to non‐guideline based care (MD ‐17.00, 95% CI ‐26.48 to ‐7.52) (one study with 192 participants clustered among 33 treatment providers included in the analysis), but we found moderate‐quality evidence of no significant effect on reducing days until full RTW at one‐year follow‐up (MD ‐17.73, 95% CI ‐37.35 to 1.90) (two studies with 342 participants included in the analysis).
Authors' conclusions
We found moderate‐quality evidence that CBT did not significantly reduce time until partial RTW and low‐quality evidence that it did not significantly reduce time to full RTW compared with no treatment. Moderate‐quality evidence showed that PST significantly enhanced partial RTW at one‐year follow‐up compared to non‐guideline based care but did not significantly enhance time to full RTW at one‐year follow‐up. An important limitation was the small number of studies included in the meta‐analyses and the small number of participants, which lowered the power of the analyses.
Keywords: Adult; Humans; Return to Work; Absenteeism; Adjustment Disorders; Adjustment Disorders/therapy; Cognitive Behavioral Therapy; Cognitive Behavioral Therapy/methods; Problem Solving; Randomized Controlled Trials as Topic; Relaxation Therapy; Stress, Psychological; Stress, Psychological/prevention & control; Time Factors
Plain language summary
Improving return to work in adults suffering from symptoms of distress
Adjustment disorders, characterised by distress symptoms and emotional disturbance as a reaction to a significant life change or stressful life event, are a frequent cause of sick leave among workers. Apart from the negative consequences for the worker, sick leave poses a heavy burden on society due to the loss of productivity of the worker and work disability claims. Different treatments have been developed to help such workers return to work. Our study assessed how effective these treatments are at enabling the sick‐listed worker to return to partial or full‐time work. We searched databases containing articles from different scientific journals and looked for studies that tested whether a certain type of treatment helped the worker to return to work when on sick leave because of an adjustment disorder. We found nine relevant studies. In total, 10 psychological treatments were evaluated and one combined treatment consisting of a psychological treatment and relaxation techniques. We found no studies on pharmacological interventions, exercise programmes or employee assistance programmes. The nine studies included in this review reported in total on 1546 participants. Of the 10 psychological treatments, five consisted of cognitive behavioural therapy and five of problem solving therapy, which are commonly used types of treatment for patients with mental health problems. Our results showed that workers on sick leave because of an adjustment disorder can be helped with making their first step back to work (i.e. partial return to work) by treating them with problem solving therapy. On average, workers who are offered problem solving therapy start 17 days earlier with partial return to work compared to workers who receive no treatment or the usual treatment from their occupational physician or general practitioner. However, we also found that cognitive behavioural therapy or problem solving therapy does not help the worker return to work with full‐time hours any quicker than workers who receive no treatment or the usual treatment from their occupational physicians or general practitioners. These results are based on moderate‐quality evidence, which implies that further research is likely to have an important impact on our confidence in the results and may change the results.
Summary of findings
Summary of findings for the main comparison. CBT compared to no treatment for adjustment disorders.
| CBT compared to no treatment for adjustment disorders | ||||
| Patient or population: patients with adjustment disorders Settings: occupational health care Intervention: CBT Comparison: no treatment | ||||
| Outcomes3 | Illustrative comparative risks* (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | |||
| No treatment | CBT | |||
| Partial return to work Follow‐up: mean 1 year | The mean time to partial return to work in the control groups was 88 days | The mean time to partial return to work in the intervention groups was 8.78 days less (95% CI is ‐23.26 lower to 5.71 higher) | 201 (2 studies; 1 study with 2 treatment arms) | ⊕⊕⊕⊝ moderate1 |
| Full return to work Scale from: ‐180 to +180 days Follow‐up: 1 year (mean) | The mean time to full return to work in the control groups was 252 days | The mean time to full return to work in the intervention groups was 35.73 days less (95% CI is 113.15 lower to 41.69 higher) | 105 (1 study; 2 treatment arms) | ⊕⊕⊝⊝ low1,2 |
| Distress score DASS distress scale from: 0 to 42 points (worse) Follow‐up: 1 year (mean) | The mean distress score in the control groups was 14.1 points | The mean distress score in the intervention groups was 0.06 points higher (95% CI is 3.91 lower to 4.02 higher) | 89 (1 study; 2 treatment arms) | ⊕⊕⊕⊝ moderate1 |
| *The basis for the assumed risk when there was more than one study was the mean partial RTW in the control group across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1Fewer than 400 participants.
2Heterogeneity I² = 58% (moderate heterogeneity).
3CBT = cognitive behavioural therapy, DASS = Distress, Anxiety and Stress Scales.
Background
Description of the condition
In recent years, increasing attention has been paid to mental health problems and their consequences in terms of sick leave and work disability (Bültmann 2005; Hensing 2006; Michie 2003; Nieuwenhuijsen 2006). In many Western countries, mental health problems are the main cause of sick leave (Glozier 2002; Henderson 2005; Hensing 2004). Sick leave has major consequences for the subjective well‐being of an individual. Workers who are on sick leave can become isolated from family members and friends who are still working. Furthermore, they can become marginalised from their colleagues and the workplace (Eriksson 2008; Jansson 2007). Receiving compensation benefits is a possible source of stigma due to perceived laziness, leading to feelings of anger, shame and guilt in workers who are on sick leave (Eriksson 2008; Jansson 2007). Apart from the negative consequences for the individual worker, sick leave results in a heavy societal burden because of loss of productivity and work disability claims (Goetzel 2004; Lerner 2008; Lim 2000; Sanderson 2006).
Adjustment disorders are a common mental health problem among workers (Carder 2009). The Bristol Stress and Health at Work Study found that more than 50% of the respondents reported being extremely, very or moderately stressed at work (Smith 1998; Smith 2000). Furthermore, adjustment disorders are one of the most frequent causes of sick leave due to mental health problems (Koopmans 2011; Nielsen 2010). In the Netherlands, work disability as a result of mental health problems accounts for 30% of all disability benefits (Hartman 2004; Statistics Netherlands 2008). Moreover, a majority (69% to 79%) of the employees suffer from common mental health problems such as adjustment disorders (Lisv 2000; NCOD 2009).
Adjustment disorders are defined in both the Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV) (APA 1994) and the International Statistical Classification of Diseases and Related Health Problems (ICD‐10) (World Health Organization 1992). DSM‐IV has defined adjustment disorders as the occurrence of emotional and behavioural symptoms in response to an identifiable stressor occurring within three months after the onset of the stressor. Furthermore, the DSM‐IV states that:
The symptoms or behaviours are clinically significant as evidenced by either of the following:
marked distress that is in excess of what would be expected from exposure to the stressor;
significant impairment in social or occupational (academic) functioning.
The stress‐related disturbance does not meet the criteria for another specific Axis I disorder and is not merely an exacerbation of a pre‐existing Axis I or Axis II disorder.
The symptoms do not represent bereavement.
Once the stressor (or its consequences) has terminated, the symptoms do not persist for more than an additional six months.
Adjustment disorders can be classified as acute if the disturbance lasts less than six months and as chronic if the disorder lasts longer than six months. The specification 'chronic' is only applicable when the disorder lasts longer then six months as a reaction to a chronic stressor or a stressor with lasting consequences.
The ICD, a detailed description of known diseases and injuries published by the World Health Organization, is revised periodically (last revision in 1992) and is currently in its 10th edition. The ICD‐10 defines the following diagnostic criteria for adjustment disorders:
States of subjective distress and emotional disturbance, usually interfering with social functioning and performance, arising in the period of adaptation to a significant life change or a stressful life event. The stressor may have affected the integrity of an individual's social network (bereavement, separation experiences) or the wider system of social supports and values (migration, refugee status), or represented a major developmental transition or crisis (going to school, becoming a parent, failure to attain a cherished personal goal, retirement). Individual predisposition or vulnerability plays an important role in the risk of occurrence and the shaping of the manifestations of adjustment disorders, but it is nevertheless assumed that the condition would not have arisen without the stressor. The manifestations vary and include depressed mood, anxiety or worry (or mixture of these), a feeling of inability to cope, plan ahead, or continue in the present situation, as well as some degree of disability in the performance of daily routine.
Notwithstanding these clear definitions of adjustment disorder in the DSM‐IV and the ICD‐10, this diagnosis is not frequently used in the research literature. More often, mental health problems such as 'sub‐threshold symptoms of depression', 'stress‐related mental disorder', 'burnout', 'emotional distress' or 'distress' are investigated, which are not included in the DSM‐IV or ICD‐10 (Bakker 2010; Nielsen 2010; Rai 2010). However, the definitions of the DSM‐IV and the ICD‐10 show that distress or sub‐threshold symptoms (e.g. depressed mood or anxiety) accompanied by a stressful life event, coincide with the diagnosis of adjustment disorder as long as no other mental disorders can be diagnosed according to the DSM‐IV or ICD‐10. Although adjustment disorders are considered mild compared to major psychiatric disorders, at least 20% of Dutch patients with such a disorder do not return to work (RTW) within a year (Schröer 1993). In line with this, Nielsen 2011b showed that 19% of a cohort of workers on sick leave because of stress and burnout complaints had not returned to work after 40 weeks of sick leave.
Description of the intervention
Interventions have been developed to facilitate RTW of workers on sick leave because of adjustment disorders. A broad range of interventions is available, such as pharmacotherapy, psychological interventions, relaxation therapy, exercise programmes, employee assistance programmes or a combination of these. Interventions can be developed for the individual worker or for a group of workers. Commonly used interventions to address adjustment disorders and RTW are psychological interventions, such as cognitive behavioural therapy (CBT) or problem solving therapy (PST). Cognitive behavioural interventions focus on behavioural activation strategies (e.g. rehearsing activities before executing them, assertiveness or communication training), restructuring maladaptive thoughts, and identifying and challenging automatic thoughts (Longmore 2007). For example, Stenlund 2009 studied the effectiveness of cognitively oriented behavioural rehabilitation in combination with relaxation exercises on reducing sick leave. Problem solving interventions are primarily focused on identifying problems, generating and selecting solutions, developing an action plan and evaluating the solution (Cuijpers 2007). Other examples of psychological interventions are psychodynamic therapy, behavioural therapy, counselling and interpersonal therapy. Employee assistance programmes are offered by the employer and were originally developed from occupational alcohol programmes. Currently, employee assistance programmes are also designed to address other health problems that have a negative impact on workers' well‐being or job performance (Merrick 2007). Relaxation therapy can consist of any method to help relax a person and reduce levels of anxiety or stress (e.g. yoga), while exercise programmes are aimed at increasing physical activity.
How the intervention might work
Studies on prognostic factors for RTW of workers on sick leave because of mental health problems have shown that ongoing mental health problems are a negative predictor for RTW (Blank 2008; Brouwers 2009). We hypothesised that pharmacological interventions may improve RTW by the reduction of mental health complaints such as depressive and anxiety symptoms, related to the adjustment disorder, caused by the medication (Wagstaff 2001). When the symptoms of the adjustment disorder are reduced, a worker on sick leave will be able to resume social roles, such as work (Brouwers 2009). The effect of psychological interventions, especially CBT and PST, on RTW is hypothesised to be established through one (or both) of two routes. Firstly, by addressing cognitions, behaviours and problems related to the adjustment disorder, psychological intervention may improve mental health. The improved mental health could then facilitate RTW (Israel 1996; van der Klink 2001). Secondly, psychological interventions may specifically focus on cognitions, behaviours and problems that are work‐related and may induce more adaptive cognitions and find solutions for the work‐related problems to enhance RTW (van Rhenen 2008). Also, when a graded activity approach for RTW is part of a psychological intervention, RTW could be facilitated by gradually building up exposure to the work environment and work tasks (Blonk psychologist 2006). Relaxation techniques and exercise programmes may have an effect on RTW by introducing enjoyable activities (i.e. relaxation or exercise) which create an understanding of the importance of a balance between work and leisure (Eriksson 2010).
Why it is important to do this review
For those on sick leave from work due to adjustment disorders, various interventions for improving RTW have been developed; it is important to evaluate which types of intervention are effective and to quantify the effect size. To date, no systematic review has investigated the effectiveness of interventions aimed at improving RTW of workers on sick leave due to adjustment disorders. Therefore, this is the topic of the current review. Recently, three Cochrane reviews have been published in the same research area (Marine 2006; Nieuwenhuijsen 2008; van Oostrom 2009). However, the review by Marine 2006 was only performed for healthcare workers and focused on the reduction of symptoms of occupational stress, while the present review is focused on all workers on sick leave because of an adjustment disorder and has RTW as primary outcome measure. The review by Nieuwenhuijsen 2008 also focused on RTW (i.e. by looking at the reduction of sick leave), but within a working population suffering from depression, not adjustment disorders. Finally, the review of van Oostrom 2010 included all workers on sick leave and, therefore, also those on sick leave because of an adjustment disorder. Nevertheless, the review included only workplace interventions whereas the present review describes a broader array of interventions.
Objectives
The objective of this review was to assess the effects of interventions facilitating RTW for workers with acute or chronic adjustment disorders.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials (RCTs), including cluster RCTs, that evaluated an intervention to facilitate RTW of workers on sick leave due to adjustment disorders were considered.
Types of participants
Participant characteristics
Workers (18 to 65 years of age) with work disability related to an adjustment disorder causing sick leave.
Sick leave status
If the study population consisted of a mix of workers who were working and who were on sick leave, studies were included if the distribution of workers on sick leave was comparable between study groups. Furthermore, we would only use the number of workers that were on sick leave in the analyses and thus 'at risk' for the outcome (which was RTW). This was a post‐hoc decision (i.e. made after the development of the review protocol).
Diagnosis ‐ inclusion
Adjustment disorders were defined as acute significant emotional or behavioural problems in response to an identified stressor, as described in the DSM‐IV (APA 1994) and ICD‐10 (World Health Organization 1992) criteria. Studies were included when participants had a main diagnosis of adjustment disorder based on the DSM‐IV or ICD‐10 criteria. Studies were also included when the authors stated that a diagnosis of adjustment disorder, burnout or neurasthenia was made by a qualified medical or psychological professional based on a classification system or by excluding other psychiatric disorders based on the DSM‐IV or ICD‐10. Moreover, studies were included when participants reported a distinct level of (di)stress‐related symptoms or burnout‐related symptoms assessed by a (di)stress or burnout scale of a validated self report questionnaire such as the Four‐Dimension Symptom Questionnaire (4DSQ) (Terluin 2006), the Depression, Anxiety and Stress Scales (DASS) (Lovibond 1995) or the Maslach Burnout Inventory (MBI) (Maslach 1996).
Diagnosis ‐ exclusion
Studies were excluded if it was clear that more than 30% of the participants (a) suffered from moderate to severe depression or anxiety disorder, (b) were diagnosed with other psychiatric disorders than adjustment disorder, or (c) were diagnosed with physical disorders. This criterion allowed us to include studies in which some participants (maximum 30%) were misclassified, in line with the misclassifications that sometimes occur in practice.
Types of interventions
All interventions were included that aimed at facilitating RTW of workers on sick leave because of adjustment disorders, using individual or group approaches. We grouped interventions into the following categories:
1. Pharmacological interventions
Pharmacological interventions could consist of any psychotropic medication.
2. Psychological interventions
Psychological interventions could consist of any form of psychological therapy such as cognitive therapy, behaviour therapy, cognitive behavioural therapy (CBT), problem solving therapy (PST), psychodynamic therapy or individual psychotherapy. However, we only found interventions that consisted of CBT or PST. Interventions were considered to be CBT when at least one of the components was cognitive restructuring (Beck 1979). Interventions were considered to be PST when at least one of the components was identifying problems and solutions by the patient/worker (Cuijpers 2007).
Treatment providers could be any type of healthcare professional trained in the therapy being investigated in the study.
3. Relaxation techniques
Relaxation techniques could consist of techniques to learn to relax muscles and breathing exercises to accomplish a state of calmness.
4. Exercise programmes
Exercise programmes could consist of enhancing physical fitness by muscle training, endurance training, aerobics, etc.
5. Employee assistance programmes
Employee benefit programmes could consist of programmes offered by the employer to help employees deal with problems that may have a negative impact on their work performance and health.
6. A combination of two or more of these interventions
We grouped interventions in different comparison groups when the type of control group differed. We grouped the following control groups together.
No treatment or waiting list condition
Care as usual
A similar alternative treatment
Types of outcome measures
Primary outcomes
The primary outcome was RTW and we considered the following measures of RTW for this review:
Time until partial RTW. Time to partial RTW was operationalised as (a) number of days of sick leave until partial RTW, (b) total number of days of partial sick leave during follow‐up, or (c) rate of partial RTW at follow‐up measurements.
Time until full RTW. Time to full RTW was operationalised as (a) number of days of sick leave until full RTW, (b) total number of days of full‐time sick leave during follow‐up, or (c) rate of full RTW at follow‐up measurements.
When studies reported more than one measure of RTW including time to RTW, we only used time to RTW for data analysis because we considered this to be the most precise estimate of RTW.
Secondary outcomes
Symptoms related to an adjustment disorder as measured by a validated and reliable psychometric scale such as the distress scale of the Four‐Dimensional Symptom Questionnaire (4DSQ) (Terluin 2006), the stress scale of the Depression, Anxiety and Stress Scales (DASS) (Lovibond 1995) or the Maslach Burnout Inventory (MBI) (Maslach 1996); or by structured diagnostic interviews like the Composite International Diagnostic Interview (CIDI) (Kessler 2004).
Work functioning, which we defined as productivity (economic impact of health problems on work) or performance (impact of health problems on the execution of a job) of workers (Lagerveld 2010). Examples of validated work functioning measures are the Work Limitations Questionnaire (WLQ) (Lerner 2001) or the Stanford Presenteeism Scale (SPS) (Koopman 2002). Only total scores on questionnaires were used in this review.
Generic functional status (the overall functional capabilities of an individual, such as physical functioning, social function, general mental health) and quality of life as measured by validated and reliable questionnaires such as the Short Form 36 Health Survey (SF‐36) (Ware 1992) and EuroQol (EuroQol Group 1990). Only total scores on questionnaires were used in this review.
When studies used different questionnaires to measure the same concept, only the results of one questionnaire was reported. The choice for one of the questionnaires was based on the best reflection of the concept being measured according to the opinion of the review authors.
Timing of outcome assessment
We grouped follow‐up times into three categories that we considered to be sufficiently homogeneous; from zero to three months, from four to 12 months and from one to two years.
Search methods for identification of studies
Cochrane Depression, Anxiety and Neurosis Group (CCDAN) Specialised Register (CCDANCTR)
The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintain two clinical trials registers at their editorial base in Bristol, UK, a references register and a studies‐based register. The CCDANCTR‐References Register contains over 29,000 reports of randomised controlled trials in depression, anxiety and neurosis. Approximately 65% of these references have been tagged to individual, coded trials. The coded trials are held in the CCDANCTR‐Studies Register and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual. Please contact the CCDAN Trials Search Co‐ordinator for further details.
Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of MEDLINE (1950 ‐), EMBASE (1974 ‐) and PsycINFO (1967 ‐); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and review‐specific searches of additional databases. Reports of trials are also sourced from international trials registers c/o the World Health Organization’s trials portal (ICTRP), drug companies, the handsearching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses.
Details of CCDAN's generic search strategies can be found on the Group's website.
Electronic searches
The CCDANCTR (Studies and References) was searched by the Group's Trials Search Co‐ordinator (TSC), all years to 1 October 2011, using the following terms for POPULATION only (employees on sick leave):
Keywords = (“sick leave” or “medical leave” or absenteeism or (vocational and rehabilitation) or reemployment or “leave benefits”) OR Free‐text = ((sick and (leave or list* or absen*)) or ((sick* or absen*) and (workplace or (work and related) or occupation* or job)) or "return to work")
We ran complementary searches on the following databases:
Cochrane Central Register of Controlled Trials (CENTRAL) (all years to Issue 4, 2011, Appendix 1);
MEDLINE (1950 to 21 February 2011, Appendix 2) (search terms were based on those used by Gehanno et al (Gehanno 2009) in a study to identify RTW records in MEDLINE);
EMBASE (1980 to 21 February 2011, Appendix 3);
PsycINFO (all years to 21 February 2011, Appendix 4);
ISI Web of Science (all years to 21 February 2011, Appendix 5); and
WHO trials portal (ICTRP) and the ClinicalTrials.gov (29 March 2011, Appendix 6).
We applied no restriction on date or language.
An update search was conducted in October 2011. At this stage we took the decision to rely on the CCDANCTR alone as no extra studies were found by our complementary searches.
Searching other resources
We checked the reference lists of all reports retrieved as full‐text papers for other potentially relevant studies. We also screened systematic reviews and narrative literature reviews. We retrieved and assessed relevant articles for possible inclusion in the review.
Data collection and analysis
Selection of studies
We developed a standardised selection form to make a first selection of relevant studies, based on the following criteria: (1) study design is a RCT, (2) study population consists of a working population and (3) study population includes common mental disorders (adjustment disorders, depressive disorders, anxiety disorders). Two review authors (DB and DR, DB and IA, KN and IA, or UB and IA) screened all references on title, keywords and abstract independently by using the standardised form. Disagreements were resolved by consensus of opinion. If disagreements could not be resolved, a third review author (JV) was consulted. We documented a record of all rejected papers and the reasons for rejection.
Subsequently, we retrieved the full papers of all remaining titles and abstracts. In addition, we retrieved all other potentially relevant articles identified by reference checking. Papers in all languages were included. The two authors independently reviewed all articles who completed a form for each study and scored the eligibility of the study (see Appendix 7). The reasons for exclusion were documented. When the same study had more than one article written on the outcomes, we treated all articles as one study and presented the results only once. Disagreements were resolved as before.
Data extraction and management
Two authors (DB and IA and AN and IA) completed the extraction of data from the papers to a data extraction form to elicit the following information:
General : published/unpublished, title, authors, source, contact address, country, language of publication, year of publication, duplicate publications
Methods : design, country, setting, randomisation procedure, recruitment, inclusion period, follow‐up, start/end dates, loss to follow‐up
Participants : number of participants, diagnosis, co‐morbidity, inclusion/exclusion criteria, age, sex, days of sick leave at baseline, ethnicity, marital status, educational level, social economic status
Interventions per treatment group : number of participants, treatment type/content, treatment provider, number of treatment providers, treatment frequency/duration, training/supervision of treatment providers
Outcomes: length of follow‐up, return to work, clinical outcomes, work functioning, generic functioning, quality of life and type of analysis for every outcome measured
Results : absenteeism, clinical outcomes, work functioning, generic functioning and quality of life (effect measure, standard deviation, test statistic, confidence interval)
If there were any disagreements about the data extraction, consensus was achieved by discussion between the two review authors. If disagreements could not be resolved, a third author was consulted (JV).
Assessment of risk of bias in included studies
Two authors (IA and UB) assessed the risk of bias of the included studies. We assessed risk of bias with the use of an adapted version of The Cochrane Collaboration's tool for assessing risk of bias as described in the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0. (Higgins 2011). We assessed the following nine criteria.
Random sequence generation
Allocation concealment
Blinding of participants
Blinding of care providers
Blinding of outcome assessment
Co‐interventions avoided or similar
Treatment fidelity
Incomplete outcome data
Selective outcome reporting
We scored the criteria as 'low risk of bias', 'high risk of bias' or 'unclear risk of bias'. When the two review authors disagreed about the risk of bias for one of the criteria, we tried to reach consensus. If disagreements could not be resolved by consensus of opinion, the judgement of a third review author (DB) was asked for. Where resolution was not possible, we contacted the study author to obtain more information and clarification. We pilot‐tested the 'Risk of bias' tool on two of the included studies in the review. When information to assess the risk of bias was lacking in a study article, we contacted the authors for additional information. If the authors did not reply, or if the information was no longer available, the criteria were judged as 'unclear risk'.
Measures of treatment effect
Dichotomous measures
For studies that reported on dichotomous data, such as RTW rates, we used risk ratios as a measure of treatment effect.
Continuous measures
For studies that reported on continuous data, such as the number of days until full RTW, we used the mean difference (MD) because the same measurement scale was used. All estimates included a 95% confidence interval (CI).
Unit of analysis issues
Cross‐over trials
We planned to include RCTs with a cross‐over design, but no studies of this kind were found.
Multiple‐armed trials
If studies had multiple treatment arms (i.e. two intervention arms and one control arm) and each treatment intervention could be used in the same meta‐analysis, we chose to compare each treatment intervention with the comparison intervention and divided the number of participants in the comparison intervention over the number of treatment interventions. This was done to prevent double‐counting of the participants in the comparison intervention. In case the number of participants in the comparison intervention could not be equally divided (e.g. there were 71 participants in the comparison intervention and there were two treatment interventions to make a comparison with), we chose to use the higher number of participants (36, following the example) for the comparison with the treatment intervention with the highest number of participants.
Cluster‐randomised controlled trials
For the two studies (Bakker 2007; van der Klink 2003) that employed a cluster‐randomised design but did not account for the design effect, we made the following adjustments. In one study, the cluster‐level results were reported for the primary outcome (days until partial and full RTW), which we used in the data‐analysis (van der Klink 2003). For the other study, no intra‐cluster correlation (ICC) was reported for the primary outcome (days until full RTW), but information was available on the intra‐cluster correlation for the scores on the four scales of the 4DSQ (which was one of the secondary outcome measures in this study). Therefore, to calculate the design effect for the primary outcome, we used the mean of the intra‐cluster correlations of the four 4DSQ scales (Bakker 2007). We assumed that differences between treatment providers would be comparable for the reduction of distress symptoms and the facilitation of return to work. Furthermore, ICCs for the level of treatment providers are generally low and do not have a big impact on the outcome data (i.e. the effect of individual differences between treatment providers on the outcome is often low). We used the intra‐cluster correlation reported by Bakker 2007 for the distress scale of the 4DSQ to calculate the design effect for this secondary outcome measure for both the studies of Bakker 2007 and van der Klink 2003.
For the calculation of the design effect we used the method described in the Cochrane Handbook in chapter 16.3.4 (Higgins 2011).
Dealing with missing data
We contacted the authors of all nine studies to obtain data missing from their study report which we needed for the 'Risk of bias' assessment and/or input for the meta‐analysis. For a detailed description of the information asked from each author, see the Characteristics of included studies table. We received a response from all authors, except for Stenlund 2009. For the studies of van der Klink 2003 and Willert 2011, we calculated the standard deviations (SDs) for the primary outcome measure based on the 95% CI using the calculation tool provided by RevMan 5.1 (RevMan 2011). For calculating the SD, only one of the two sides of the 95% CI needs to be entered in the calculation tool (next to the group mean and the group N). Therefore, we chose to enter the left side of the 95% CI since this results in a more conservative (i.e. larger) SD.
Assessment of heterogeneity
For judging clinical similarity between studies, we followed the algorithm provided by Verbeek 2011. We deemed interventions similar if the mechanism by which they were believed to achieve RTW was similar, such as a cognitive behavioural or a problem solving mechanism. For RTW outcomes, we considered both number of days until RTW and number of days on sick leave during follow‐up as sufficiently similar. Studies with study populations consisting of working age participants were deemed similar enough, because studies generally include a broad range of participants. Thus, we expected characteristics such as age, gender and job type to be heterogeneous in all studies alike.
For judging statistical heterogeneity, we inspected graphical representations of the data. In addition, we quantified statistical heterogeneity with the I2 statistic. We judged statistical heterogeneity as not important when the I2 was less than 40%, moderate if it was between 30% and 60%, substantial if between 50% and 90%, and considerable if between 75% and 90% (Higgins 2011).
Assessment of reporting biases
We intended to assess publication bias with funnel plots, if 10 or more studies had been available for each of the seven data analyses. If there had been an indication of publication bias we would have used Egger's test to assess this (Egger 1997).
Data synthesis
We pooled studies into different comparisons with RevMan 5.1 software when they were judged to be clinical homogeneous and had sufficient and adequate data. The data allowed us to make comparisons according to the interventions mentioned under the heading Types of interventions. We expected that possible observed differences between study results might not be solely due to chance, because of differences in bias or treatment provider. Therefore, we used random‐effects models. If small studies were included in a comparison group, we compared the random‐effects model with the fixed‐effect meta‐analysis to see whether the small studies increased the estimate of the beneficial effect of the intervention in the random‐effects model. If small studies significantly increased the estimate of the effect of the intervention (i.e. from a non‐significant effect in a fixed‐effect meta‐analysis to a significant effect in a random‐effects analysis), we chose to present the results of the fixed‐effect meta‐analysis.
For studies with continuous outcomes, we used the mean number of days until RTW/on sick leave and the SD of each study group to calculate the mean difference (MD). For studies with a dichotomous outcome measure (rate of RTW), we used risk ratios (RR) and combined them in the meta‐analysis.
We combined continuous measures, such as number of days until RTW, using the mean difference as implemented in the RevMan 5.1 software. For dichotomous outcomes such as rate of RTW we used the Mantel‐Haenzel method to combine the risk ratios.
We assessed the overall quality of the evidence for each outcome using the GRADE approach as recommended by the Cochrane Handbook (Higgins 2011). The quality of the evidence on a specific outcome was based on the following five domains: limitations of the study design, inconsistency of results, indirectness of results, imprecision of results and publication bias across all studies that measured that particular outcome. At the start of the GRADE assessment process we assumed high quality for all studies and we downgraded the quality of the evidence for each comparison by one to three levels depending on the seriousness of the violations of each domain. For limitations in study design, we considered a majority of studies with high risk of bias as a serious limitation leading to downgrading of the quality. For consistency, we considered an I2 value of 30% to 60% as moderate inconsistency, 50% to 90% as substantial inconsistency and of 75% to 90% as considerable inconsistency, which would lead to downgrading quality. For imprecision of results, we judged serious imprecision leading to downgrading by a number of fewer than 400 participants or, for a non‐significant effect, a confidence interval that included an effect size (ES) of 0.5. We judged publication bias with funnel plots when enough studies were available. If not, we looked at the characteristics (e.g. only studies with a positive result) of the studies that were available, to get an indication of possible publication bias. The interpretation of the quality level of evidence that resulted from these judgements was as follows:
High: further research is very unlikely to change our confidence in the estimate of effect.
Moderate: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low: any estimate of effect is very uncertain.
Subgroup analysis and investigation of heterogeneity
We intended to carry out subgroup analyses on: (1) organisational setting, (2) type/level of job undertaken, (3) group versus individual therapy and (4) the setting of treatment providers. It could be possible that the effects of interventions are altered by these study features. For example, bigger organisations might be better able to create an infrastructure for executing an intervention, workers with a higher job level might have better cognitive abilities to understand intervention assignments and treatment providers that are more closely related to the workplace (e.g. occupational physicians (OPs)) might have more influence on the RTW process. Furthermore, differences in effectiveness between individual and group therapy are not frequently investigated for adjustment disorders but it is interesting for practice since group therapy can be more cost‐effective (Jónsson 2011; Sobell 2009). However, we did not find enough studies for these analyses. One study did make a direct comparison between an individual and a group intervention (de Vente individual 2008), and we decided to compare both interventions in a separate data‐analysis.
Sensitivity analysis
Methodological heterogeneity can lead to differences between the results of individual studies. Therefore, we intended to undertake sensitivity analyses on the results by looking at the possible contribution of differences in methodological quality, for example by excluding studies with a high or unclear risk of bias for allocation concealment or acceptable compliance. However, the number of studies in each analysis was insufficient to perform these sensitivity analyses.
We performed sensitivity analyses on the diagnosis of adjustment disorder, by excluding studies from comparisons that did not diagnose adjustment disorder based on the DSM‐IV or ICD‐10.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Results of the search
Figure 1 presents a flow diagram of included and excluded studies. The initial search in the electronic databases identified 3546 references; 121 in the CCDANCTR, 299 in CENTRAL, 488 in EMBASE, 590 in MEDLINE, 264 in PsycINFO and 1784 in ISI Web of Science. After removing duplicate references, 1454 references remained. Based on title and abstract, we identified 59 eligible references and retrieved the full text of the references. Checking the references of all articles that were retrieved as full papers and two systematic reviews (Simon 2001; van Oostrom 2009) did not result in any additional studies. Following this, we screened the 59 full‐text articles with the help of the study eligibility form.
1.
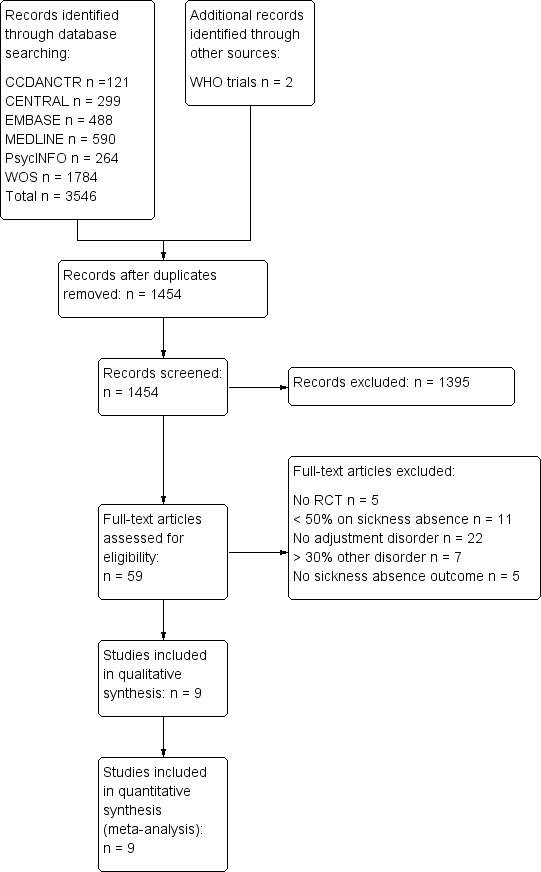
Study flow diagram.
Eight studies met the inclusion criteria and were included in the review (Bakker 2007; Blonk psychologist 2006; Brouwers 2006; de Vente individual 2008; Stenlund 2009; van der Klink 2003; van Oostrom 2010; Willert 2011). A study by Rebergen 2009 met all the inclusion criteria, except one: 32% of the study population had symptoms related to an anxiety or depressive disorder. The other 68% of the study population had symptoms related to adjustment disorders. Therefore, we contacted the author for outcome data on the subgroup of participants with adjustment disorders. The author was willing to provide these data, and because the distribution of participants with symptoms of adjustment disorders was equal for both study groups (86 participants in the trial and comparison intervention), the study was also included in the review (Rebergen 2009). In the study of Willert 2011, some of the participants were not on sick leave at baseline. Therefore, we contacted the author and asked them to provide separate data including only the participants that were on sick leave at baseline. The author was willing to provide the data and the distribution of the participants on sick leave at baseline was comparable between the trial and comparison intervention (29 and 31 respectively). Thus, this study was also included. Two study protocols were found for studies that are still ongoing (Arends 2010; Noordik 2009). With the additional search in the WHO trials portal, we found two other studies that are also still ongoing (Brouwers 2011; Netterstrøm 2011). Reasons for excluding the other 50 articles can be found in the Characteristics of excluded studies table.
Included studies
Characteristics of studies and participants
The main characteristics of the nine included studies are summarised in Table 2. Seven of the nine studies were performed in the Netherlands, one in Denmark and one in Sweden. Overall, 1546 participants were included. The average age of the participants ranged between 39 and 49 years; the percentage of female participants ranged between 19% and 71%. All studies recruited participants with disorders that were compatible with our definition of adjustment disorders. Two studies used the DSM‐IV or ICD‐10 diagnostic criteria for adjustment disorder to select participants (Blonk psychologist 2006; van der Klink 2003). Two studies (Bakker 2007; van Oostrom 2010) used a validated distress screener to select participants, based on three questions of the Four‐Dimension Symptom Questionnaire developed by Terluin et al (Braam 2009; Terluin 2004; Terluin 2006). Two studies used the Composite International Diagnostic Interview (CIDI) (World Health Organization 1990) to exclude participants with other mental disorders than adjustment disorders and used a diagnosis of minor mental disorders according to the general practitioner (GP) (Brouwers 2006) or symptoms of neurasthenia diagnosed in a semi‐structured interview by clinical psychologist (de Vente individual 2008) as inclusion criterion. In one study, a Stress Clinic was responsible for psychological examinations to confirm the diagnosis of burnout. Furthermore, participants had to score above a cut‐off score on the Shirom–Melamed Burnout Questionnaire (SMBQ) (Melamed 1992). In the study of Rebergen 2009, the Depression, Anxiety and Stress Scales (DASS) (Lovibond 1995) were used, after diagnosis of a mental health problem by the OP, to define subgroups of participants with anxiety or depression and a subgroup of participants with stress symptoms related to adjustment disorders. Finally, one study used a semi‐structured assessment interview by a clinical psychologist to diagnose persistent symptoms of work‐related stress and to exclude severe psychiatric conditions or a history of repeated psychiatric conditions in participants (Willert 2011).
1. Study characteristics.
| Study | Number | Follow‐up | Diagnosis | Treatment type | CBT or PST | Treatment provider | Treatment frequency | Comparison type | Work outcome |
| Bakker 2007; the Netherlands | 227 versus 206 | 12 months | Stress‐related mental disorders measured by means of self reported levels of distress with a validated questionnaire | Individual sessions on: information on the importance of the patient's active role with regard to successful RTW; advice on the content of functional rehabilitation; monitoring of the patient's efforts to translate the (work) situation into a problem that could be solved; referral to specialised care in case of no progressions | PST: translate the (work) situation into a problem that could be solved Work: information on successful RTW; the work situation is translated into a problem that could be solved |
24 primary care physicians trained in the intervention (2 session of 3.5 hours and 2 follow‐up sessions of 2 hours) | 3 consultations within 3 months | Care as usual by primary care physician | Duration of sick leave in calendar days from the first day of sick leave until full RTW, lasting for a period of at least 4 weeks without partial or full relapse into sick leave (self report) |
| Blonk 2006; the Netherlands | 40 versus 21 | 12 months | Adjustment disorders diagnosed with the CIDI | Individual sessions on cognitive restructuring; registration of symptoms and situations; sessions on time‐management, work resumption, workplace interventions, conflict handling and fatigue; assignments related to the work situation | CBT: sessions on cognitive restructuring Work: sessions on work resumption and workplace interventions |
Psychologists who followed a highly structured protocol | 11 sessions of 45 minutes (2 sessions a week) | No treatment | The length of time until partial RTW and the length of time until full RTW (register‐based) |
| Blonk work 2006; the Netherlands | 40 versus 21 | 12 months | Adjustment disorders diagnosed with the CIDI | Individual sessions on: psycho education on work stress; registration of symptoms and situations; relaxation; self help books on rational emotive behaviour therapy; time‐management; writing assignments; advice on work processes (setting priorities, planning, conflict management, reducing work demands, delegating tasks, organisation of work); stimulating work resumption | CBT: self help books on rational emotive behaviour therapy Work: advice on work processes; stimulating work resumption |
6 labour experts trained in brief CBT‐based stress management | 5 to 6 1‐hour sessions (2 sessions a week) | No treatment | The length of time until partial RTW and the length of time until full RTW (register‐based) |
| Brouwers 2006; the Netherlands | 98 versus 96 | 18 months | Emotional distress or minor mental disorders according to GPs and self report | Individual sessions on: acknowledging the problem and accepting responsibility for its resolution; developing and implementing problem solving strategies, with a special focus on solving work‐related problems and promoting early work resumption; making a daily activity schedule | PST: developing and implementing problem solving strategies Work: focus on work‐related problems and promoting early work resumption |
11 social workers trained in the intervention (3‐day training course with 2 follow‐up sessions) | 5 individual 50‐minute sessions over 10 weeks | Care as usual by the GP | Sick leave duration (in days), defined as the period between the first day of absenteeism and the first day of partial and full work resumption (self report) |
| de Vente group 2008; the Netherlands | 28 versus 13 | 10 months | Symptoms of neurasthenia based on a screening interview | Group sessions and homework assignments on: psycho education; self assessment of stressors and complaints; life style; relaxation techniques; cognitive restructuring; time‐management; goal setting; assertiveness skills; evaluation and relapse prevention | CBT: cognitive restructuring | 12 clinical psychologists trained in the intervention (4 x 1‐hour sessions) | 12 x 1‐hour sessions | Care as usual by the occupational physician and GP | Number of days absent and number of weeks until complete work resumption (self report) |
| de Vente individual 2008; the Netherlands | 28 versus 13 | 10 months | Symptoms of neurasthenia based on a screening interview | Individual sessions and homework assignments on: psycho education; self assessment of stressors and complaints; life style; relaxation techniques; cognitive restructuring; time‐management; goal setting; assertiveness skills; evaluation and relapse prevention | CBT: cognitive restructuring | 12 clinical psychologists trained in the intervention (4 x 1‐hour sessions) | 12 x 2‐hour sessions | Care as usual by the occupational physician and GP | Number of days absent and number of weeks until complete work resumption (self report) |
| Rebergen 2009; the Netherlands | 125 versus 115 | 12 months | Symptoms of adjustment disorders based on the DASS (based on unpublished data from author) | Individuals sessions on: information about the origin and cause of loss of control; structuring daily activities developing and implementing problem solving skills and strategies for the causes of stress; gradual RTW | PST: developing and implementing problem solving skills Work: gradual RTW |
5 OPs trained in the intervention (3‐day training course) | Mean number of consultations with OP was 3.4 | Minimal involvement of the OP (same OPs as intervention group) and access to treatment by a psychologist |
Duration of sick leave due to mental health problems in calendar days from the moment of inclusion to first (partial or full) and full RTW, respectively, in own or equal earnings; duration of sick leave days until full RTW added with number of days of recurrences on sick leave in the 1‐year follow‐up |
| Stenlund 2009; Sweden | 67 versus 69 | 2 years | Burnout based on psychological examinations at the Stress Clinic | Group session on: education on stress reactions, medication and rest; awareness of reactions and self talk; development of cognitive/behavioural/emotional skills; spiritual issues and life values; preparation for RTW; physical relaxation and mindfulness meditation | CBT: awareness of reactions and self talk Work: preparation for RTW |
1 group leader trained in CBR; 1 physiotherapist | CBR: 30 x 3‐hour sessions over 1 year with short follow‐up meetings 3, 6 and 12 months after the treatment year; Qigong: a 1‐hour session every week during 1 year | Physical relaxation and mindfulness meditation | Sick leave rate: 100, 75, 50, 25 or 0% (register‐based) |
| van der Klink 2003; the Netherlands | 109 versus 83 | 12 months | Adjustment disorders diagnosed with a checklist based on the DSM‐IV criteria for adjustment disorder | Individual sessions on: information on the origin and cause of loss of control; structuring daily activities; development and implementation of problem solving strategies for the causes of stress; gradual RTW | PST: development and implementation of problem solving strategies Work: gradual RTW |
17 occupational physicians trained in the intervention (3‐day training course) | 4 to 5 sessions (with a total length over all sessions of at least 90 minutes) in the first 6 weeks of sickness leave and 1 session after work resumption | Care as usual by occupational physicians | Time (days) to partial and full RTW; duration (days) of sick leave; partial and full RTW rate at 3 and 12 months follow‐up; incidence of recurrent sick leave in the year following full RTW; time to first recurrent sick leave in the year following full RTW (register‐based) |
| van Oostrom 2010; the Netherlands | 73 versus 72 | 12 months | Distress based on a validated screening questionnaire | Consultations with the worker and supervisor to (1) identify obstacles and solutions for RTW, (2) formulate a plan for implementation of the solutions and (3) to evaluate the actual implementation of solutions | PST: identifying obstacles (problems) for RTW and finding/implementing solutions Work: problems related to RTW |
9 RTW co‐ordinators (company social worker or a labour expert) trained in the intervention | 3 sessions at 1 day and a follow‐up meeting after 1 month |
Care as usual by occupational physicians | Days until full and lasting RTW; total number of days of sick leave in the 12‐month follow‐up (register‐based) |
| Willert 2011; Denmark | 51 versus 51 | 48 weeks | Persistent symptoms of work‐related stress based on a semi‐structured assessment interview | Group sessions and homework on: introduction to CBT; psycho education on stress; identifying dysfunctional thinking; modifying dysfunctional thinking; communication and stress; communication skills training; implementing strategies at work (e.g. cope with stressful situations at work); review of techniques | CBT: identifying and modifying dysfunctional thinking Work: implementing strategies at work (e.g. cope with stressful situations at work) |
2 licensed clinical psychologists, with > 5 years of clinical experience and a 1‐year advanced training course in CBT | 8 x 3‐hour sessions over a period of 3 months | Waiting list control group; after 3 months on the waiting list, the participants also received the intervention | Sick leave days 3‐month in retrospect (self report); weeks registered with part‐ or full‐time sick leave (register‐based) |
CBR: Cognitively oriented Behavioural Rehabilitation CBT: cognitive behavioural therapy CIDI: Composite International Diagnostic Interview DASS: Depression, Anxiety and Stress Scales GP: general practitioner OP: occupational physician PST: problem solving therapy RTW: return to work
In all but one of the nine studies (Willert 2011), participants were on sick leave at the start of the study. In the study of Willert 2011, 57% of the participants were on sick leave. The maximum duration of sick leave at baseline differed between studies. In two studies, participants were only included if they were on sick leave for no longer than half a year (de Vente individual 2008; Willert 2011); two other studies chose a maximum period of sick leave of three months (Bakker 2007; Brouwers 2006). The study by Stenlund 2009 allowed for a longer sick leave period, namely between three and 12 months. Compared to this, the study by van Oostrom 2010 only included participants with two to eight weeks of sick leave. In the study by Rebergen 2009, workers were immediately contacted in their first week of sick leave. Two studies had no criterion defined on the minimum or maximum length of sick leave (Blonk psychologist 2006; van der Klink 2003).
Interventions
Eight studies reported on the effect of 10 psychological interventions and one study on the effect of a combined intervention consisting of a psychological intervention and relaxation techniques. For the other intervention types (e.g. pharmacological intervention, exercise programme) no studies were found.
Of the 10 psychological interventions, five were based on CBT (Blonk psychologist 2006; de Vente individual 2008; Willert 2011) and the other five were based on PST (Bakker 2007; Brouwers 2006; Rebergen 2009; van der Klink 2003; van Oostrom 2010). Two of the interventions were performed in groups of (seven to nine) participants (de Vente individual 2008; Willert 2011); the other eight interventions were all performed with the individual participant. Eight interventions (Bakker 2007; Blonk psychologist 2006; Brouwers 2006; Rebergen 2009; van der Klink 2003; van Oostrom 2010; Willert 2011) had a strong focus on the work environment by incorporating consultations/assignments aimed at identifying work‐related problems to facilitate early work resumption. The other two psychological interventions were performed according to strict CBT protocols (one in a group format and one in an individual format) which focused on giving psycho education, cognitive restructuring, relaxation, conflict management and time management (de Vente individual 2008). These protocols were tailored to general life problems and had a less specific focus on work‐related problems. The study by Willert 2011 also used a CBT protocol with the aim of enabling participants to cope with stressful situations at their workplace and strengthen their ability to be active at work. The main components of this intervention were psycho education, cognitive restructuring, communication skills training and implementing strategies at work. The study of Blonk psychologist 2006 had two intervention arms; in one arm, participants received CBT according to a highly structured and commonly used protocol (in the Netherlands) which consisted mainly of cognitive restructuring but also focused on work resumption, time management, workplace interventions, conflict handling and fatigue. The other intervention arm consisted of a shorter CBT programme combined with advice on work processes (e.g. setting priorities, planning and conflict management) by labour experts. Treatment schedules of the interventions can be found in the Characteristics of included studies table.
The interventions tested by Brouwers 2006 and Rebergen 2009 used the same intervention as developed and evaluated by van der Klink 2003. These studies used an intervention protocol based on PST. The main components were to (1) give information about the origin and cause of loss of control, (2) develop and implement problem solving strategies and (3) apply gradual RTW. However, in the study by Brouwers et al the treatment providers were different (social workers instead of OPs) and the intervention protocol was adjusted to fit this group of treatment providers. Likewise, Bakker et al used a problem solving intervention which was conducted by primary care physicians (i.e. GPs) (Bakker 2007). The intervention focused on giving information about the active role of the worker in his RTW process, advising about functional rehabilitation and monitoring the problem solving strategies of the worker. Finally, the study by van Oostrom 2010 also used a problem solving intervention. However, the intervention in this study differentiates from the other PST‐based interventions because of a participatory approach in which the worker and supervisor work together in the development of problem solving strategies. Specifically, the intervention consisted of a stepwise communication process between the worker and his supervisor, guided by a RTW co‐ordinator, to identify and solve obstacles for RTW. Three meetings were planned; one with the worker and the RTW co‐ordinator, one with the supervisor and the RTW co‐ordinator and one with all three parties. Obstacles for RTW were identified from the perspective of the worker and the supervisor. Following this, solutions were discussed during the third meeting and a plan (based on consensus) was made for implementing the solutions. If needed, the RTW co‐ordinator visited the workplace of the worker to give advice or instructions. One month after the meetings, the RTW co‐ordinator planned an evaluation meeting with the worker and supervisor.
The combined intervention evaluated by Stenlund 2009 consisted of Cognitive Behavioural Rehabilitation (CBR) in groups of six to nine participants and Qigong in groups of 12 to 16 participants. The CBR programme had five key components: education; awareness of reactions and self talk (a form of cognitive restructuring); development of behavioural, cognitive and emotional skills; spiritual issues and life values; and preparation for RTW. Qigong was a form of relaxation techniques consisting of warm‐up movements; basic movements to affect body awareness, balance and co‐ordination, breathing and muscular tension; and relaxation and mindfulness meditation. Although participants had to perform some bodily exercises, we did not regard this as an exercise programme because the focus was on relaxation. CBR included 30 three‐hour sessions over one year and Qigong included weekly one‐hour sessions for one year.
Treatment providers were comparable for some studies. In three studies, (clinical) psychologists trained in CBT provided the intervention (Blonk psychologist 2006; de Vente individual 2008; Willert 2011). OPs were the treatment providers in the studies of Rebergen 2009 and van der Klink 2003 and had received a three‐day training in the intervention. Labour experts and social workers conducted the intervention in the study of van Oostrom 2010. Labour experts were also the treatment providers in one trial arm of the study by Blonk psychologist 2006, and social workers delivered the intervention in the study by Brouwers 2006. In all cases, the labour experts and social workers received training in the intervention. In Bakker 2007, primary care physicians were the treatment providers, and they had received seven hours of training in the intervention. Finally, Stenlund 2009 did not specify the professional background of the treatment providers providing CBR but did mention that the group leaders had received training in CBR. The Qigong intervention in this study was delivered by a physiotherapist trained in Qigong.
Three psychological interventions were compared to a waiting list control group (Blonk psychologist 2006; Willert 2011). Five psychological interventions were compared to non‐guideline based care (defined as "care as usual" in the studies) by a GP (Bakker 2007; Brouwers 2006) or OP (de Vente individual 2008; van der Klink 2003). One psychological intervention was compared to minimal intervention by the OP and treatment by psychologists working according to cognitive behavioural principles (Rebergen 2009). The combined intervention was compared to Qigong (Stenlund 2009) and the participatory problem solving intervention was compared to treatment by the OP according to a problem solving guideline (van Oostrom 2010).
Study design and setting
Seven studies were randomised controlled trials with randomisation at the level of the participant (Blonk psychologist 2006; Brouwers 2006; de Vente individual 2008; Rebergen 2009; Stenlund 2009; van Oostrom 2010; Willert 2011) and two studies were cluster‐randomised controlled trials with randomisation at the level of the GP (Bakker 2007) or OP (van der Klink 2003). Two studies had three treatment arms (Blonk psychologist 2006; de Vente individual 2008). In the study by Blonk psychologist 2006, the first trial intervention (named 'Blonk labour expert 2006' in the analyses) consisted of CBT‐based stress management intervention with a focus on graded RTW. The second trial intervention (named 'Blonk psychologist 2006' in the analyses) consisted of highly structured CBT according to a commonly used protocol. Both trial interventions were compared to a waiting list control group. In the study by de Vente individual 2008, the first trial intervention (named 'de Vente individual 2008' in the analyses) was individual stress‐management training (SMT) according to a strict protocol based on cognitive behavioural techniques. The second trial intervention (named 'de Vente group 2008' in the analyses) was group SMT according to the same protocol as the individual SMT. Both trial interventions were compared to care as usual by the OP and GP.
Four studies were performed in an occupational healthcare setting; in three studies participants were treated by an Occupational Health Care Service of a company (Rebergen 2009; van der Klink 2003; van Oostrom 2010) and in one study participants were treated by labour experts (Blonk psychologist 2006). Two studies were performed in a primary care setting where participants were treated by their general physicians (Bakker 2007) or by social workers (Brouwers 2006). Finally, three studies were performed in a clinical setting with treatment by a clinical psychologist (de Vente individual 2008; Willert 2011) or treatment in a Stress Clinic (Stenlund 2009).
Outcomes
Time to partial or full RTW, measured as number of days or weeks between the start of sick leave until partial or full work resumption or the number of days on sick leave during follow‐up, was measured in eight of the nine included studies (Bakker 2007; Blonk psychologist 2006; Brouwers 2006; de Vente individual 2008; Rebergen 2009; van der Klink 2003; van Oostrom 2010; Willert 2011). The follow‐up time ranged from four to 18 months. One study only reported on the rate of sick leave at different time measurements (Stenlund 2009). Clinical status of adjustment disorder was measured with a validated psychometric instrument in seven studies: four studies used the Four‐Dimension Symptom Questionnaire (Bakker 2007; Brouwers 2006; van der Klink 2003; van Oostrom 2010); two studies used the Depression, Anxiety and Stress Scales (Blonk psychologist 2006; de Vente individual 2008); and one study used the Shirom–Melamed Burnout Questionnaire (Stenlund 2009). All studies had multiple follow‐up measurements between two months and two years after baseline. One study measured generic functional status with the SF‐36, but only reported scores on subscales and no total scores (Brouwers 2006). None of the studies measured quality of life or work functioning.
Excluded studies
Of the 59 full‐text retrieved studies, 50 studies were excluded from the review because the study was not a randomised controlled trial (N = 5), the study population was not on sick leave (N = 11), participants did not have an adjustment disorder according to the definition of this review (N = 22), more than 30% of the participants were diagnosed with physical disorders or other mental disorders than adjustment disorders (N = 7) or because sick leave was not measured (N = 5). For a more detailed description, see the Characteristics of excluded studies table.
Risk of bias in included studies
The details on the 'Risk of bias' assessment for each included study are shown in the Characteristics of included studies table. The results are summarised in the 'Risk of bias' graph which presents the authors' judgement about each 'Risk of bias' item presented as percentages across all included studies (Figure 2). The results for each 'Risk of bias' item for each individual study are presented in the 'Risk of bias' summary (Figure 3). Of the nine included studies, we assessed seven as having a low risk of bias (Bakker 2007; Blonk psychologist 2006; de Vente individual 2008; Rebergen 2009; van der Klink 2003; van Oostrom 2010; Willert 2011). We assessed the other two studies as having high risk of bias (Brouwers 2006; Stenlund 2009).
2.
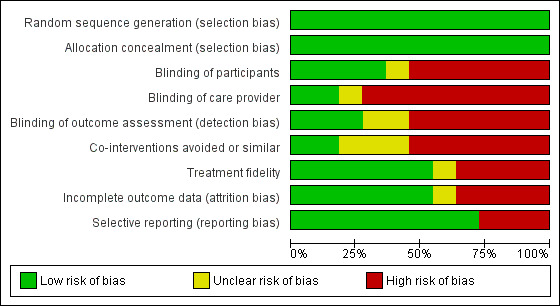
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
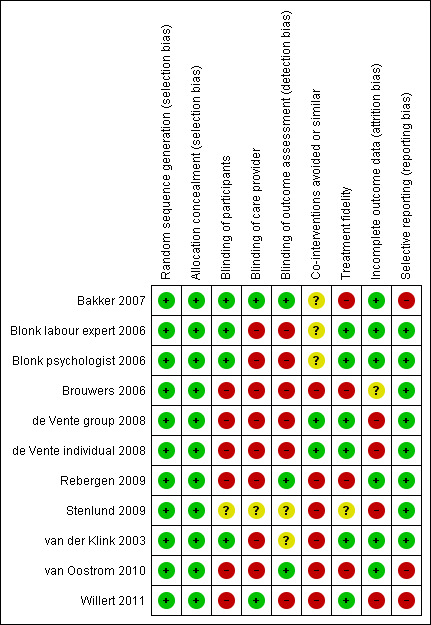
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
In all studies, an adequate system for random sequence generation was reported, as well as adequate allocation concealment. Overall, computer‐generated random numbers or dice were used for randomisation. To conceal allocation, the results of the randomisation were hidden in opaque envelopes or an independent research assistant performed the randomisation.
Blinding
Blinding of participants was realised in three studies (Bakker 2007; Blonk psychologist 2006; van der Klink 2003). We judged blinding of the care provider as having low risk of bias for two studies (Bakker 2007; Willert 2011). In the study of Bakker 2007, the care providers were randomised to the intervention or control group and treated all their patients according to their protocol, but they were unaware of which patients participated in the study. In the study of Willert 2011, two care providers treated participants from both the intervention and waiting list control group according to the intervention protocol and did not know if their participants belonged to the intervention or waiting list control group. In the study of van der Klink 2003, participants received a global overview of both treatment strategies which were presented as equally effective and of which the participants were not able to notice the difference. Blonk psychologist 2006 blinded the participants in their study by only giving general information about the goal of the study (based on personal communication with the author). Bakker 2007 used a cluster‐randomised controlled trial by which the allocation of participants was already pre‐defined by the allocation of their care provider (in this study, their treating GP). Therefore, the participants were not informed about the two different study groups and were only told that the study was about stress and sick leave. The care providers were blinded because they had to treat all their patients according to the intervention treatment or comparison treatment (depending on their randomisation) and were unaware of which patients were included. In the study of Willert 2011, the group leaders of the stress management intervention (i.e. the care providers) led the different groups of participants without knowledge of the participants' randomisation. The first two groups consisted of those randomised to the intervention arm of the trial. Groups three to 10 consisted of participants mixed from the intervention and waiting list control arms. Group 11 and 12 consisted of participants randomised to the waiting list control arm (based on unpublished information from the author).
Blinding of outcome assessors was reported in three studies (Bakker 2007; Rebergen 2009; van Oostrom 2010). In these studies, the researchers responsible for collecting outcome data as well as the researchers responsible for analysing the data were kept blind to treatment allocation.
Incomplete outcome data
All studies reported on drop‐outs, but in four studies the reasons for drop‐out were not comparable for all study groups (de Vente individual 2008; Stenlund 2009; van der Klink 2003; Willert 2011). Furthermore, for one study, no information was available about the reasons for drop‐out (Brouwers 2006) and this study was therefore judged as 'unclear risk of bias'. In all studies, except one (Blonk psychologist 2006) an intention‐to‐treat analysis was conducted.
Selective reporting
All but three studies (Bakker 2007; van Oostrom 2010; Willert 2011) were free from selective reporting. In the study of Bakker 2007 and van Oostrom 2010, analyses of secondary outcome measures that were planned in the study protocol were omitted from the papers in which the study results were reported. Willert 2011 presented supplementary analyses that were not described in the methods section.
Other potential sources of bias
Two authors were not able to provide information on the use of co‐interventions by the different groups in their study (Bakker 2007; Blonk psychologist 2006). In the other six studies, co‐interventions were not avoided and not similar for the different study groups.
In four studies, treatment fidelity was rated as acceptable (Blonk psychologist 2006; de Vente individual 2008; van der Klink 2003; Willert 2011). In these studies, fidelity was ensured by checking with questionnaires or feedback moments if care providers followed the study protocols.
Acceptable attendance rates were reported by de Vente individual 2008, and from Willert 2011 unpublished information was received on acceptable attendance rates.
We included studies with smaller (N = 82 in de Vente individual 2008) and larger (N = 431 in Bakker 2007) sample sizes, and studies with positive (e.g. Blonk psychologist 2006 and van der Klink 2003) as well as non‐significant results (e.g. Bakker 2007 and van Oostrom 2010) were included. However, we were not able to further analyse publication bias because of an insufficient number of studies.
Effects of interventions
See: Table 1
No studies were found that evaluated pharmacological interventions, relaxation techniques, exercise programmes or employee assistance programmes. The nine included studies reported on 10 psychological interventions and one combined intervention, consisting of a psychological intervention and relaxation techniques. A complete overview of the effects of the interventions is presented in the Data and analyses section of this review.
Psychological interventions
1 Cognitive behavioural therapy (CBT) versus no treatment
1.1 Partial return to work (RTW), follow‐up one year
Two studies (Blonk psychologist 2006; Willert 2011), one of which had two treatment arms (Blonk psychologist 2006), compared three CBT interventions to a no treatment control group. The results of these two studies showed that there is moderate‐quality evidence (Table 3) that days until partial RTW are similar for the CBT intervention groups and the no treatment control groups (mean difference (MD) ‐8.78, 95% confidence interval (CI) ‐23.26 to 5.71) (Analysis 1.1).
2. Quality of the evidence (GRADE).
| Comparison/outcome | Studies in comparison | Risk of bias in studies | Inconsistency | Indirectness | Imprecision | Publication bias | Overall quality of evidence |
| CBT versus no treatment/partial RTW follow‐up 1 year | Blonk psychologist 2006; Willert 2011 | No: the majority of studies have low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| CBT versus no treatment/full RTW follow‐up 1 year | Blonk psychologist 2006 | No: the study has low risk of bias | Inconsistent: I2 > 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| CBT versus no treatment/distress follow‐up 1 year | Blonk psychologist 2006 | No: the study has low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| CBT versus non‐guideline based care/full RTW follow‐up 1 year | de Vente individual 2008 | Yes: the study has high risk of attrition bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| CBT versus non‐guideline based care/distress follow‐up 3 months | de Vente individual 2008 | Yes: the study has high risk of attrition bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| CBT versus non‐guideline based care/distress follow‐up 1 year | de Vente individual 2008 | Yes: the study has high risk of attrition bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| PST versus non‐guideline based care/partial RTW follow‐up 1 year | van der Klink 2003 | No: the study has low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| PST versus non‐guideline based care/full RTW follow‐up 1 year | Bakker 2007; van der Klink 2003 | No: the studies have low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| PST versus non‐guideline based care/full RTW follow‐up 1 to 2 years | Brouwers 2006 | Serious limitation: the study has high risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| PST versus non‐guideline based care/distress follow‐up 3 months | Bakker 2007; Brouwers 2006; van der Klink 2003 | No: the majority of studies have low risk of bias | Consistent: I2 < 50% |
Direct | Precise: > 400 participants | Undetected | High quality |
| PST versus non‐guideline based care/distress follow‐up 3 to 12 months | Bakker 2007; Brouwers 2006; van der Klink 2003 | No: the majority of studies have low risk of bias | Consistent: I2 < 50% |
Direct | Precise: > 400 participants | Undetected | High quality |
| PST versus non‐guideline based care/distress follow‐up 1 to 2 years | Brouwers 2006 | Serious limitation: the study has high risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| PST work versus CBT work/partial RTW follow‐up 1 year | Rebergen 2009 | No: the study has low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| PST work versus CBT work/full RTW follow‐up 1 year | Rebergen 2009 | No: the study has low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| Participatory PST work versus PST work/full RTW follow‐up 1 year | van Oostrom 2010 | No: the study has low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| Participatory PST work versus PST work/distress follow‐up 3 months | van Oostrom 2010 | No: the study has low risk of bias | No: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| Participatory PST work versus PST work/distress follow‐up 3 to 12 months | van Oostrom 2010 | No: the study has low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| CBT and physical relaxation versus Physical relaxation/rate of partial RTW follow‐up 1 year | Stenlund 2009 | Serious limitation: the study has high risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| CBT and physical relaxation versus physical relaxation/rate of partial RTW follow‐up 1 to 2 years | Stenlund 2009 | Serious limitation: the study has high risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| CBT and physical relaxation versus physical relaxation/rate of full RTW follow‐up 1 year | Stenlund 2009 | Serious limitation: the study has high risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| CBT and physical relaxation versus physical relaxation/rate of full RTW follow‐up 1 to 2 years | Stenlund 2009 | Serious limitation: the study has high risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| CBT and physical relaxation versus physical relaxation/SMBQ score follow‐up 1 year | Stenlund 2009 | Serious limitation: the study has high risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| CBT and physical relaxation versus physical relaxation/SMBQ score follow‐up 1 to 2 years | Stenlund 2009 | Serious limitation: the study has high risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| Individual CBT versus group CBT/full RTW follow‐up 1 year | de Vente individual 2008 | Yes: the study has high risk of attrition bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| Individual CBT versus group CBT/distress follow‐up 3 months | de Vente individual 2008 | Yes: the study has high risk of attrition bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| Individual CBT versus group CBT/distress follow‐up 3 to 12 months | de Vente group 2008 | Yes: the study has high risk of attrition bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Low quality |
| CBT versus no treatment full AD/partial RTW follow‐up 1 year | Blonk psychologist 2006 | No: the study has low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| PST versus Non‐guideline based care full AD/full RTW follow‐up 1 year | van der Klink 2003 | No: the study has low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| PST versus non‐guideline based care full AD/distress follow‐up 3 months | van der Klink 2003 | No: the study has low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
| PST versus non‐guideline based care full AD/distress follow‐up 4 to 12 months | van der Klink 2003 | No: the study has low risk of bias | Consistent: I2 < 50% |
Direct | Imprecise: < 400 participants | Undetected | Moderate quality |
AD: adjustment disorder CBT: cognitive behavioural therapy PST: problem solving therapy RTW: return to work SMBQ: Shirom–Melamed Burnout Questionnaire
1.1. Analysis.
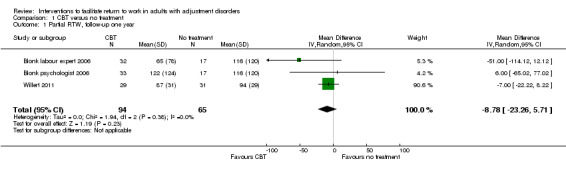
Comparison 1 CBT versus no treatment, Outcome 1 Partial RTW, follow‐up one year.
1.2 Full RTW, follow‐up one year
Blonk psychologist 2006 also evaluated the effect of the two CBT interventions on time until full RTW compared to no treatment. The results indicated that there is low‐quality evidence (Table 3) of no significant difference between the CBT interventions and no treatment for this outcome measure (MD ‐35.73, 95% CI ‐113.15 to 41.69) (Analysis 1.2)
1.2. Analysis.
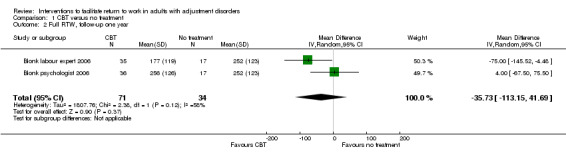
Comparison 1 CBT versus no treatment, Outcome 2 Full RTW, follow‐up one year.
1.3 Depression, Anxiety and Stress Scales (DASS) distress score, follow‐up one year
Concerning the secondary outcome of clinical status of adjustment disorder, Blonk psychologist 2006 evaluated the effect of CBT interventions on the stress scale of the DASS. The results showed that there is moderate‐quality evidence (Table 3) of a similar outcome for the CBT interventions and no treatment for mean score on the DASS stress scale at one‐year follow‐up (MD 0.06, 95% CI ‐3.91 to 4.02) (Analysis 1.3).
1.3. Analysis.
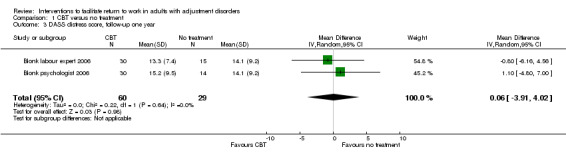
Comparison 1 CBT versus no treatment, Outcome 3 DASS distress score, follow‐up one year.
2 CBT versus non‐guideline based care
2.1 Full RTW, follow‐up one year
One study (de Vente individual 2008), consisting of two treatment arms, assessed the effects of a group‐based CBT intervention and an individual‐based CBT intervention on time to full RTW after one year of follow‐up. The interventions were compared to non‐guideline based care by the occupational physician (OP) and general practitioner (GP), which was defined as "care as usual" in the study paper. The pooled analysis showed that the CBT interventions were slightly less effective in reducing time to full RTW compared to non‐guideline based care, but this effect was not significant (MD 35.50, 95% CI ‐30.84 to 101.84), with low‐quality evidence (Table 3) (Analysis 2.1).
2.1. Analysis.
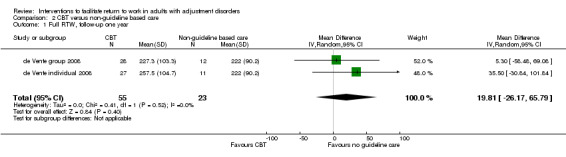
Comparison 2 CBT versus non‐guideline based care, Outcome 1 Full RTW, follow‐up one year.
2.2 DASS distress score, follow‐up three months
De Vente et al (de Vente individual 2008) also investigated the effect of the two CBT interventions on mean score on the DASS stress scale at three months follow‐up. The results indicated that there is low‐quality evidence (Table 3) of a similar outcome for the CBT interventions and non‐guideline based care for the mean score on the DASS stress scale at three months follow‐up (MD 0.66, 95% CI ‐2.78 to 4.11) (Analysis 2.2).
2.2. Analysis.
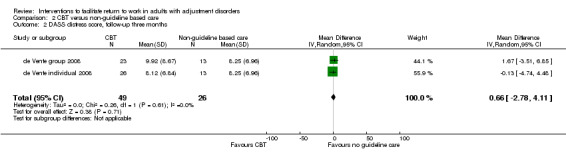
Comparison 2 CBT versus non‐guideline based care, Outcome 2 DASS distress score, follow‐up three months.
2.3 DASS distress score, follow‐up one year
Also, based on one study (de Vente individual 2008), no significant difference was found between CBT interventions and non‐guideline based care for the DASS stress scale at one‐year follow‐up (MD ‐0.67, 95% CI ‐6.06 to 4.73), with low‐quality evidence (Table 3) (Analysis 2.3).
2.3. Analysis.
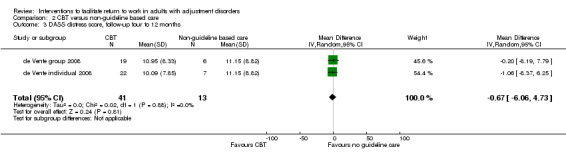
Comparison 2 CBT versus non‐guideline based care, Outcome 3 DASS distress score, follow‐up four to 12 months.
3 Problem solving therapy (PST) versus non‐guideline based care
3.1 Partial RTW, follow‐up one year
One study (van der Klink 2003) investigated the effect of PST‐based intervention on time to partial RTW after one year of follow‐up, compared to non‐guideline based care by the OP. The results showed that there is moderate‐quality evidence (Table 3) that the PST‐based intervention significantly reduced time to partial RTW with 17 days compared to non‐guideline based care (MD ‐17.00, 95% CI ‐26.48 to ‐7.52) (Analysis 3.1).
3.1. Analysis.
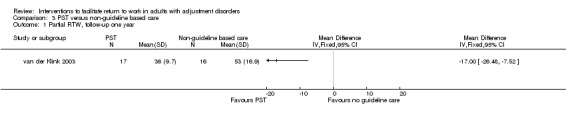
Comparison 3 PST versus non‐guideline based care, Outcome 1 Partial RTW, follow‐up one year.
3.2 Full RTW, follow‐up one year
Based on two studies (Bakker 2007; van der Klink 2003), meta‐analysis showed that there is moderate‐quality evidence (Table 3) that PST‐based interventions did not result in a significant reduction of time until full RTW compared to non‐guideline based care by the OP or GP (MD ‐17.73, 95% CI ‐37.35 to 1.90). The confidence interval still included a potential relevant effect (Analysis 3.2).
3.2. Analysis.
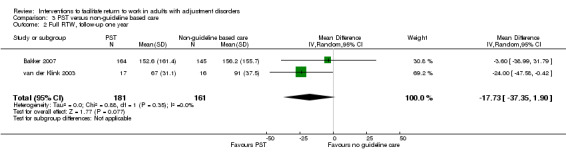
Comparison 3 PST versus non‐guideline based care, Outcome 2 Full RTW, follow‐up one year.
3.3 Full RTW, follow‐up one to two years
In line with the findings for full RTW with a follow‐up of one year and based on low‐quality evidence (Table 3), a PST‐based intervention had a similar reduction of days until full RTW compared to non‐guideline based care by the GP with a follow‐up of one to two years (MD ‐4.00, 95% CI ‐41.61 to 33.61) (Analysis 3.3).
3.3. Analysis.
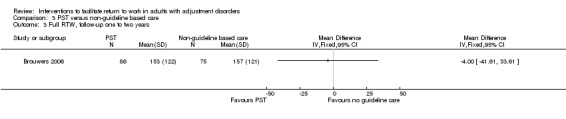
Comparison 3 PST versus non‐guideline based care, Outcome 3 Full RTW, follow‐up one to two years.
3.4 Four‐Dimension Symptom Questionnaire (4DSQ) distress score, follow‐up three months
Three studies (Bakker 2007; Brouwers 2006; van der Klink 2003) investigated the effect of PST‐based interventions on the score on the distress scale of the 4DSQ, compared to non‐guideline based care by the OP or GP. The results indicated moderate‐quality evidence (Table 3) of a significant reduction in the distress score in favour of the PST‐based interventions (MD ‐1.69, 95% CI ‐3.11 to ‐0.27) (Analysis 3.4).
3.4. Analysis.
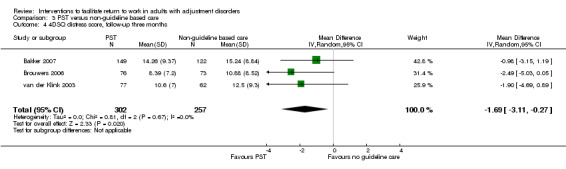
Comparison 3 PST versus non‐guideline based care, Outcome 4 4DSQ distress score, follow‐up three months.
3.5 4DSQ distress score, follow‐up four to 12 months
The significant reduction in the distress score by the PST‐based interventions was not found for the follow‐up period of three to 12 months (MD ‐0.36, 95% CI ‐1.76 to 1.04), based on moderate‐quality evidence (Table 3) (Analysis 3.5).
3.5. Analysis.
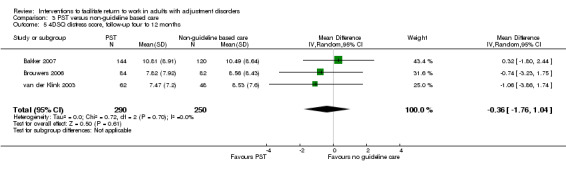
Comparison 3 PST versus non‐guideline based care, Outcome 5 4DSQ distress score, follow‐up four to 12 months.
3.6 4DSQ distress score, follow‐up one to two years
Also, at one to two years follow‐up, the results showed that there is low‐quality evidence (Table 3) of no significant difference between a PST‐based intervention and non‐guideline based care (MD ‐2.03, 95% CI ‐4.25 to 0.19) (Analysis 3.6).
3.6. Analysis.
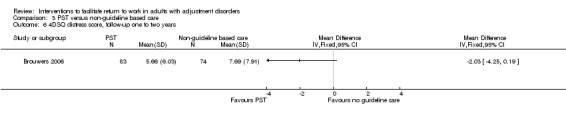
Comparison 3 PST versus non‐guideline based care, Outcome 6 4DSQ distress score, follow‐up one to two years.
4 Problem solving therapy (PST) versus CBT
4.1 Partial RTW, follow‐up one year
Rebergen 2009 investigated the effect of a PST‐based intervention compared to a CBT intervention on partial RTW after one year of follow‐up. Based on moderate‐quality evidence (Table 3), no difference was found between these treatments in the effect on time to partial RTW (MD ‐6.28, 95% CI ‐29.36 to 16.80) (Analysis 4.1).
4.1. Analysis.
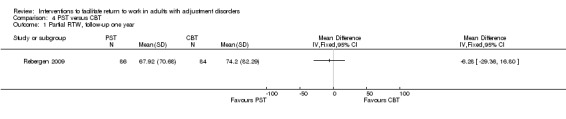
Comparison 4 PST versus CBT, Outcome 1 Partial RTW, follow‐up one year.
4.2 Full RTW, follow‐up one year
For days until full RTW after one year of follow‐up, a non‐significant reduction of sick leave was found between the PST‐based intervention compared to the CBT intervention (MD ‐6.74, 95% CI ‐37.43 to 23.95), with moderate‐quality evidence (Table 3) (Analysis 4.2).
4.2. Analysis.
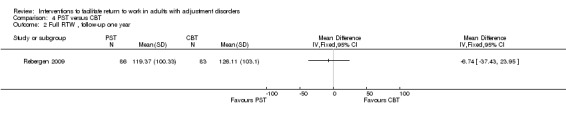
Comparison 4 PST versus CBT, Outcome 2 Full RTW , follow‐up one year.
5 Participatory PST versus PST
5.1 Full RTW, follow‐up one year
One study (van Oostrom 2010) investigated the effect of a participatory PST‐based intervention compared to a PST‐based intervention on full RTW after one year of follow‐up. The results showed that there is moderate‐quality evidence (Table 3) that there is no difference in effectiveness between the two treatments (MD ‐1.00, 95% CI ‐36.32 to 34.32) (Analysis 5.1).
5.1. Analysis.
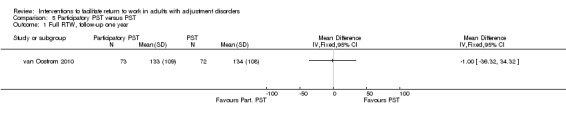
Comparison 5 Participatory PST versus PST, Outcome 1 Full RTW, follow‐up one year.
5.2 4DSQ distress score, follow‐up three months
van Oostrom 2010 also investigated the effect of the participatory PST‐based intervention on distress score, based on the distress scale of the 4DSQ, measured at three months follow‐up. The data analysis showed moderate‐quality evidence (Table 3) of no difference in distress score compared to a PST‐based intervention (MD ‐0.40, 95% CI ‐3.27 to 2.47) (Analysis 5.2).
5.2. Analysis.
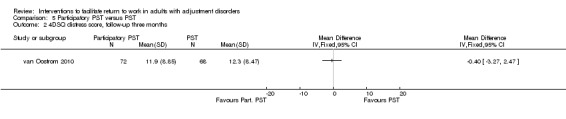
Comparison 5 Participatory PST versus PST, Outcome 2 4DSQ distress score, follow‐up three months.
5.3 4DSQ distress score, follow‐up four to 12 months
There was also no effect of the participatory PST‐based intervention compared to the PST‐based intervention on distress score at three to 12 months follow‐up (MD 0.63, 95% CI ‐2.05 to 3.31), based on moderate‐quality evidence (Table 3) (Analysis 5.3).
5.3. Analysis.
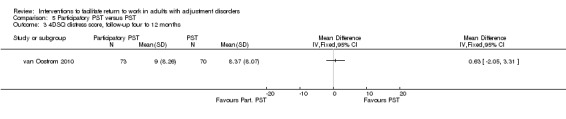
Comparison 5 Participatory PST versus PST, Outcome 3 4DSQ distress score, follow‐up four to 12 months.
Combination of interventions
1 CBT and physical relaxation versus physical relaxation
1.1 Rate of partial RTW, follow‐up one year
One study (Stenlund 2009) reported on the effectiveness of a CBT intervention and physical relaxation compared to physical relaxation alone on rate of partial RTW at one‐year follow‐up. The results indicate that there is low‐quality evidence (Table 3) of a similar outcome for the two study groups on this outcome measure (risk ratio (RR) 1.04, 95% CI 0.58 to 1.89) (Analysis 6.1).
6.1. Analysis.
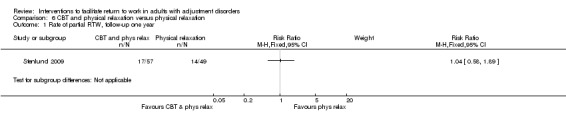
Comparison 6 CBT and physical relaxation versus physical relaxation, Outcome 1 Rate of partial RTW, follow‐up one year.
1.2 Rate of partial RTW, follow‐up one to two years
For rate of partial RTW with a follow‐up of one to two years, no significant difference was also found between the CBT intervention and physical relaxation versus physical relaxation alone (RR 0.82, 95% CI 0.50 to 1.34). This result was based on low‐quality evidence (Table 3) (Analysis 6.2).
6.2. Analysis.
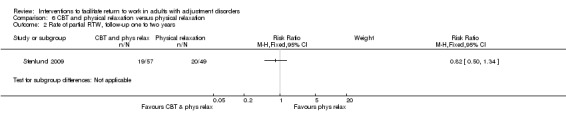
Comparison 6 CBT and physical relaxation versus physical relaxation, Outcome 2 Rate of partial RTW, follow‐up one to two years.
1.3 Rate of full RTW, follow‐up one year
In the same study by Stenlund 2009, the combined intervention was also compared to physical relaxation for the effect on rate of full RTW after one year of follow‐up. The analysis showed low‐quality evidence (Table 3) of a similar outcome for the two study groups (RR 0.72, 95% CI 0.23 to 2.20) (Analysis 6.3).
6.3. Analysis.
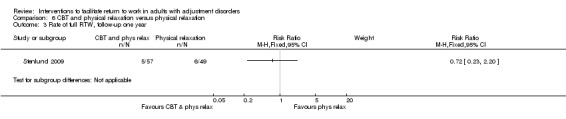
Comparison 6 CBT and physical relaxation versus physical relaxation, Outcome 3 Rate of full RTW, follow‐up one year.
1.4. Rate of full RTW, follow‐up one to two years
For rate of full RTW after one to two years follow‐up, the results showed no significant difference between the combined intervention and physical relaxation (RR 1.25, 95% CI 0.64 to 2.43), based on low‐quality evidence (Table 3) (Analysis 6.4).
6.4. Analysis.
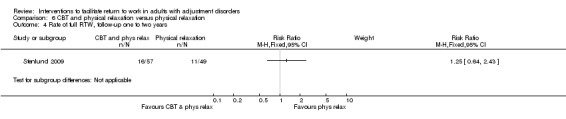
Comparison 6 CBT and physical relaxation versus physical relaxation, Outcome 4 Rate of full RTW, follow‐up one to two years.
1.5 Shirom–Melamed Burnout Questionnaire (SMBQ) score, follow‐up one year
Stenlund 2009 also investigated if the CBT intervention and physical relaxation had an effect on the SMBQ score at one‐year follow‐up compared to physical relaxation alone. The results indicated that there is low‐quality evidence (Table 3) that there is a significant reduction of the SMBQ score in favour of the combined intervention (RR ‐0.50, 95% CI ‐0.97 to ‐0.03) (Analysis 6.5).
6.5. Analysis.
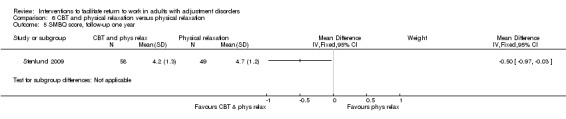
Comparison 6 CBT and physical relaxation versus physical relaxation, Outcome 5 SMBQ score, follow‐up one year.
1.6 SMBQ score, follow‐up one to two years
There was no significant difference in mean SMBQ score at one to two years follow‐up between the combined intervention and physical relaxation alone (RR ‐0.40, 95% CI ‐0.92 to 0.12), based on low‐quality evidence (Table 3) (Analysis 6.6).
6.6. Analysis.
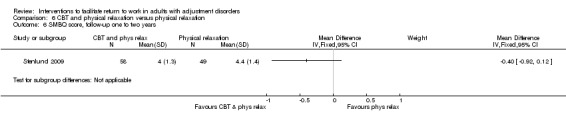
Comparison 6 CBT and physical relaxation versus physical relaxation, Outcome 6 SMBQ score, follow‐up one to two years.
Subgroup analyses
1. Individual CBT versus group CBT
1.1 Full RTW, follow‐up one year
Analysis 7.1 presents a direct comparison between individual‐based CBT and group‐based CBT on time until full RTW, based on the data from the study by de Vente individual 2008. The analysis indicates that there is low‐quality evidence (Table 3) that there is no significant difference between individual‐based and group‐based CBT on time to full RTW (MD 2.94, 95% CI ‐12.07 to 17.95) (Analysis 7.1).
7.1. Analysis.
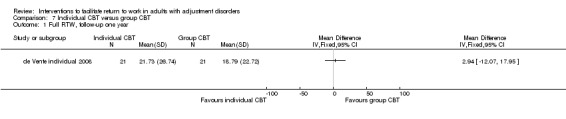
Comparison 7 Individual CBT versus group CBT, Outcome 1 Full RTW, follow‐up one year.
1.2 DASS distress score, follow‐up three months
The study by de Vente individual 2008 also evaluated the effect of individual‐based CBT versus group‐based CBT on distress score at three months follow‐up based on the DASS. The results showed that there is low‐quality evidence (Table 3) of no significant difference between the two study groups (MD ‐1.80, 95% CI ‐6.21 to 2.61) (Analysis 7.2).
7.2. Analysis.
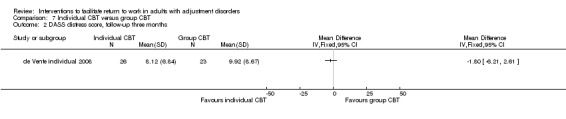
Comparison 7 Individual CBT versus group CBT, Outcome 2 DASS distress score, follow‐up three months.
1.3 DASS distress score, follow‐up four to 12 months
For the distress score at three to 12 months follow‐up, the results also showed no significant difference between individual‐based CBT and group‐based CBT (MD ‐0.86, 95% CI ‐5.84 to 4.12), based on moderate‐quality evidence (Table 3) (Analysis 7.3).
7.3. Analysis.
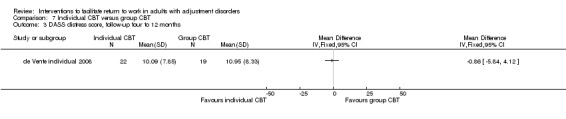
Comparison 7 Individual CBT versus group CBT, Outcome 3 DASS distress score, follow‐up four to 12 months.
Sensitivity analyses
1. CBT versus no treatment, full adjustment disorder diagnosis
1.1 Partial RTW, follow‐up one year
Analysis 8.1 presents the comparison of CBT versus no treatment excluding the study of Willert 2011, because adjustment disorder was not diagnosed according to the DSM‐IV or ICD‐10 in this study. The analysis shows that there is moderate‐quality evidence (Table 3) that there is no significant difference between CBT and no treatment on time to partial RTW (MD ‐24.92, 95% CI ‐80.58 to 30.74) (Analysis 8.1).
8.1. Analysis.
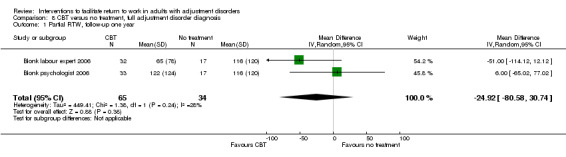
Comparison 8 CBT versus no treatment, full adjustment disorder diagnosis, Outcome 1 Partial RTW, follow‐up one year.
2. PST versus non‐guideline based care full adjustment disorder diagnosis
2.1 Full RTW, follow‐up one year
When excluding the study by Bakker 2007, based on no diagnosis of adjustment disorder according to the DSM‐IV or ICD‐10, the results showed that there is moderate‐quality evidence (Table 3) of a significant difference between PST and non‐guideline based care for full RTW after one year of follow‐up (MD ‐24.00, 95% CI ‐47.58 to ‐0.42) (Analysis 9.1).
9.1. Analysis.
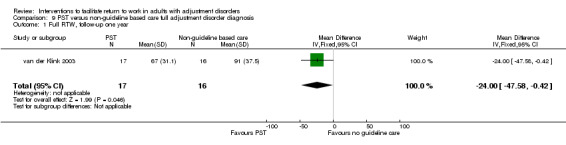
Comparison 9 PST versus non‐guideline based care full adjustment disorder diagnosis, Outcome 1 Full RTW, follow‐up one year.
2.2 4DSQ distress score, follow‐up three months
Results for the distress score at three months follow‐up based on studies including a diagnosis of adjustment disorder according to the DSM‐IV or ICD‐10 criteria showed that there is moderate‐quality evidence (Table 3) of no significant difference between PST and non‐guideline based care (MD ‐1.90, 95% CI ‐4.69 to 0.89) (Analysis 9.2).
9.2. Analysis.
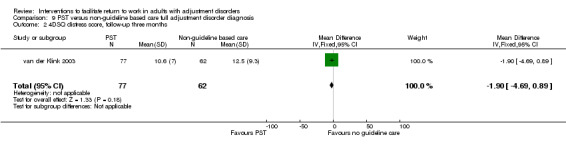
Comparison 9 PST versus non‐guideline based care full adjustment disorder diagnosis, Outcome 2 4DSQ distress score, follow‐up three months.
2.3 4DSQ distress score, follow‐up four to 12 months
Similarly, there was no significant difference between PST and non‐guideline based care for the distress score at four to 12 months follow‐up (MD ‐1.06, 95% CI ‐3.86 to 1.74), based on moderate‐quality evidence (Table 3) (Analysis 9.3).
9.3. Analysis.
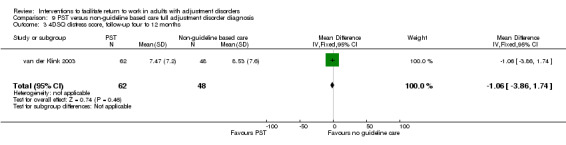
Comparison 9 PST versus non‐guideline based care full adjustment disorder diagnosis, Outcome 3 4DSQ distress score, follow‐up four to 12 months.
Discussion
Summary of main results
We found nine randomised controlled trials (RCTs) of psychological interventions and of one intervention that combined a psychological intervention with physical relaxation. We did not find RCTs of pharmacological interventions, exercise programmes or employee assistance programmes. Of the psychological interventions, five consisted of cognitive behavioural therapy (CBT) and five of problem solving therapy (PST).
Our results showed moderate‐quality evidence that time until partial return to work (RTW) was similar for workers receiving CBT or no treatment (mean difference (MD) ‐8.78, 95% confidence interval (CI) ‐23.6 to 5.71) at one‐year follow‐up. A sensitivity analysis, including studies in which adjustment disorder was diagnosed according to the DSM‐IV and ICD‐10, confirmed this result (MD ‐24.92, 95% CI ‐80.58 to 30.74). For full RTW, we found low‐quality evidence that CBT did not significantly reduce days until full RTW at one‐year follow‐up compared to no treatment. There was also moderate‐quality evidence that CBT did not significantly reduce distress complaints at one‐year follow‐up compared to no treatment (Table 1).
PST significantly reduced time until partial RTW by 17 days (MD ‐17.00, 95% CI ‐26.48 to ‐7.52) after one year of follow‐up compared to non‐guideline based care, but no significant differences were found for full RTW and distress complaints at one‐year follow‐up. However, a sensitivity analysis, only including studies with a diagnosis of adjustment disorder according to the DSM‐IV or ICD‐10, showed a significant difference between PST and non‐guideline based care for full RTW after one year of follow‐up (MD ‐24.00, 95% CI ‐47.58 to ‐0.42).
Moderate‐quality evidence showed that PST led to similar effects on partial and full RTW as CBT. Participatory PST led to similar results as PST. The rate of partial and full RTW was similar after a combined intervention consisting of CBT and physical relaxation compared to physical relaxation alone at one and two years follow‐up. Finally, we found moderate‐quality evidence that individual CBT and group CBT led to a similar time to full RTW.
Overall completeness and applicability of evidence
We have performed an extensive literature search for this study to find all relevant RCTs. By searching the WHO trials portal and ClinicalTrials.gov, we also found studies that are still being conducted and which can be followed until they are finished and ready to be assessed for inclusion in this review. Furthermore, the review authors are all experts in the field of occupational health care and work disability prevention and are knowledgeable about the studies that have been performed in this field. This ensures that most available studies have been found for this review. Considering the variability in the interventions that are included in this review and because we have not searched the grey literature, there remains a possibility that some studies have not been found.
Regarding the overall completeness of the review, it should be noted that we only found studies on psychological interventions and a combined intervention which consisted of a psychological intervention and physical relaxation. Thus, studies on the effect of other types of interventions, such as pharmacological interventions or exercise programmes, on RTW are lacking. Furthermore, not enough studies were included to perform subgroup analyses for organisational setting, treatment setting and type of job, which impedes generalisation of the results. Also, we could not assess publication bias because of the small number of studies included in the review. We have to acknowledge that the review might have been affected by publication bias.
On the other hand, there were a wide range of participants included in the studies. The mean age of participants ranged between 39 and 49 years, and the percentage of females ranged from 19% to 71%. The percentage of participants with a high educational level ranged from 4% to 52%. This indicates that the current review consists of a rather heterogeneous group of participants. Some studies did not provide information on job type, but the studies that did so indicated that participants worked, for example, for a postal company, the police department, a university, a hospital and a steel company. Although this shows a relative mixture of job types, it may be interesting to conduct more research on workers in job types that are known to be related to high sick leave rates because of adjustment disorders, such as in health care and education (Innstrand 2011; Roelen 2009). Furthermore, the results that we found in this review for partial RTW were based on studies which mainly consisted of men (Blonk psychologist 2006; van der Klink 2003). It could be that this is a gender‐specific effect and it should be studied more among women.
Applicability of the findings of this review may be restricted to the Dutch context, since seven of the nine included studies were performed in the Netherlands. In particular, the term adjustment disorder, which is commonly used in the Netherlands to refer to the group of patients suffering from distress‐related complaints, is not frequently used in other countries. Terminology such as burnout, distress, minor mental disorders or (occupational or work) stress is more common (Flaxman 2010; Hakanen 2011; Lander 2009). Furthermore, the term 'common mental disorders' is becoming more popular in research articles, where distress‐related complaints are defined as being a subgroup of common mental disorders (Feltz‐Cornelis 2010; Nielsen 2011; Rai 2010; Rebergen 2009). This made it challenging to operationalise the diagnosis of adjustment disorder for this review. Our aim was to only include participants with burnout‐related or distress‐related complaints and, therefore, we excluded participants suffering from more debilitating disorders, such as anxiety and depressive disorders. For future research, it would be helpful to come to a shared definition for the group of patients that suffer from adjustment disorders and validated assessment tools, to enhance comparability between studies.
Although the majority of the included studies were performed in the Netherlands, the problem of sick leave related to adjustment disorders is encountered in many other countries (Henderson 2005; Kessler 1997). It could be that the interventions evaluated in this review are more effective in other countries than the Netherlands, because the comparison interventions may have included effective interventions. Occupational physicians (OPs) in the Netherlands have had a guideline for managing sick leave because of mental health problems since 2000 (van der Klink 2000; van der Klink 2007). Furthermore, with the Gatekeeper Improvement Act, that has been effective in the Netherlands since 2002, more investments have been made in RTW by employers, employees and occupational healthcare services. Six of the Dutch studies included in this review were performed after these dates. Thus, participants in the comparison interventions of these studies were obliged to see the OP to be supported in RTW and will have received support from their employers to enhance RTW. This may have led to small contrasts between study groups in some of the Dutch studies, such as the studies of van Oostrom 2010 and Rebergen 2009. However, when comparing the mean days until partial or full RTW for the comparison interventions of the Dutch studies performed before 2002 and after 2002, no clear difference in time to RTW can be seen. When looking at the two studies included in this review that were performed in other countries (Denmark and Sweden), one study showed a significant difference in sick leave days between the experimental (CBT) and comparison (no treatment) group (Willert 2011). The other study, comparing CBT and physical relaxation versus physical relaxation alone, did not detect a significant difference in rate of sick leave (Stenlund 2009). Thus, our hypothesis that the interventions included in this review might be more effective in other countries than the Netherlands needs to be evaluated by future research to be confirmed.
Finally, the follow‐up time in most studies was one year. Only two studies had a follow‐up time of 18 months (Brouwers 2006) and two years (Stenlund 2009). However, we believe that a follow‐up time of one year is sufficient when evaluating the effect of an intervention on RTW, because most workers on sick leave because of adjustment disorders return to work within one year.
Quality of the evidence
We were able to include nine RCTs. We considered this a fair number, since it is not easy to perform randomised studies in a healthcare setting. Furthermore, we used a clear definition of adjustment disorders, also including studies that did not use a strict DSM‐IV or ICD‐10 diagnosis but did focus on a study population with comparable complaints. Since only two studies used a strict DSM‐IV and ICD‐10 diagnosis, our broadened definition of adjustment disorders allowed us to give a good overview of the research done on study populations with more mild mental health complaints. The drawback of the broadened definition is that the different studies did not consist of homogeneous populations. We dealt with this by performing sensitivity analyses on the studies that did use the diagnostic criteria of the DSM‐IV or ICD‐10 to assess whether participants had an adjustment disorder. In future research, a strict diagnosis of adjustment disorder, based on the DSM‐IV or ICD‐10, should be used to enhance comparability between studies.
The studies mainly included small numbers of participants with a mean number of 156 participants. The outcome measure of mean days until partial or full RTW had a large standard deviation (SD) with approximately the same magnitude as the mean. Given these large SDs, the power to detect relevant differences in these studies may have been insufficient. Moreover, most comparisons were based on one study and only a few comparisons consisted of two or three studies. In light of this, results have to be carefully interpreted. The extent to which the findings are applicable to other study settings and future trials may be limited. Future researchers investigating interventions to facilitate RTW of workers with adjustment disorders should try to recruit double the amount of participants and will need to find ways to overcome recruitment problems.
A potential threat to the quality of the evidence could be the way we incorporated multiple trial arms in the meta‐analyses. We chose to include each trial arm in the comparison and divide the control group in two. This method can influence the estimate of between‐study variance, especially because of the small number of studies in the meta‐analyses. Thus, these estimates are imprecise and should be interpreted cautiously.
Some studies used the median when reporting days until partial or full RTW, because sick leave data are known to be skewed. Although the mean number of days until partial and full RTW was used in this review, our results are comparable to the results of the individual studies. For example, van Oostrom 2010 reported on the median days until full RTW and found a non‐significant hazard ratio (HR) of 0.99, which is comparable to the MD of one day found in this review. In general, it is known that the t‐test is fairly robust for data being skewed to one side (Lumley 2002).
All studies had acceptable randomisation and treatment allocation procedures. However, only one study succeeded in keeping co‐interventions comparable between the treatment and control group (de Vente individual 2008). The fact that the other studies did not succeed in preventing co‐interventions or keeping them similar for all study groups, makes it difficult to draw strong conclusions on the effectiveness or ineffectiveness of the interventions in this review. If control groups had easy access to psychiatrists, psychologists and psychotropic medication, the contrast with the intervention groups, and thus the chance of finding an effect of the intervention, will have been diminished. Furthermore, compliance to the treatment was not acceptable in four of the nine studies (Bakker 2007; Brouwers 2006; Rebergen 2009; van Oostrom 2010). This could explain our finding that most of the interventions had no significant effect. Thus, researchers need to become more aware of avoiding or keeping co‐interventions similar for all study groups and ensuring compliance to the study protocol by care providers.
Another problem encountered in the studies in this review was the lack of blinding of participants and care providers. Only three studies succeeded in blinding participants (Bakker 2007; Blonk psychologist 2006; van der Klink 2003) and two in blinding care providers (Bakker 2007; Willert 2011). This problem often arises in studies that are designed as pragmatic trials, such as the studies in this review. Pragmatic trials investigate the effectiveness of an intervention in everyday practice. Often, it is difficult to blind participants and care givers for the treatment intervention, because it is clearly different from normal practice (Fransen 2007). A possible solution to this problem is to design a cluster‐randomised controlled trial or to pre‐randomise participants (Huibers 2004). In a pre‐randomised design, randomisation takes place before detailed information is given about the study, and participants allocated to one study group are kept blind to the randomisation procedure and to the existence of the other study group.
We also planned to analyse, as a secondary outcome measure, outcomes related to work functioning or work productivity, but the studies in this review only used time until RTW as a work‐related outcome measure. It would be interesting to know more about workers after they have returned to work. It could be that workers are less productive or not functioning well after their RTW. Therefore, it would be helpful to include other work‐related outcomes in addition to sick leave measures to gain insight into the process after RTW in future studies.
Potential biases in the review process
In this review, we did not restrict the languages in which studies were published. This prevented bias in the selection of studies only published in the English language. However, it should be mentioned that two of the review authors were the study authors of one of the included studies (Rebergen 2009). To prevent biased assessment, these authors were not involved in the selection, 'Risk of bias' assessment and data extraction for this study. Moreover, all these steps of the review process were always independently performed by two review authors.
To prevent reporting bias, we reported on individual studies, not on individual articles. For every RCT, we traced all articles that were related to the same study and used for data extraction for that single study.
Potential bias might have occurred in defining the different interventions included in the review. Instead of using the names that the authors gave to their intervention, we first predefined which components should be part of an intervention to frame it as CBT or PST. Following this, we checked the components of every intervention and, based on this, we classified it as being CBT or PST. We feel that this approach is more systematic than using the names that were given to the interventions by the authors, and we believe that it has not biased our results.
We combined studies that evaluated the same intervention, but in which the intervention was provided by different healthcare professionals. In some studies, these professionals were specialised psychologists and in other studies they were OPs or GPs with little experience in providing CBT or PST. This could increase heterogeneity in two ways. First of all, because of a higher‐intensity treatment and effect with more professional treatment. Secondly, the relationship of the healthcare professional with the employer and the focus on work differs between professionals and could have an effect on how a treatment is delivered. However, we were not able to evaluate these hypotheses because of a lack of a sufficient number of studies.
Finally, bias might have been introduced by using the intra‐cluster correlation (ICC) of the distress score, which was given in the study of Bakker 2007, to calculate the ICC for RTW in Bakker 2007 and the ICC for distress in the study of van der Klink 2003. This could have inflated the variance for both outcomes and misrepresented the true degree of variation of the study population for the outcomes concerned.
Agreements and disagreements with other studies or reviews
There are other reviews that have also focused on interventions to facilitate RTW but for different study populations. For example, Schaafsma 2010 investigated the effect of physical conditioning programmes for improving work outcomes in workers with back pain. In this systematic review, the authors could not find an effect of light or intensive physical conditioning programmes on the reduction of sick leave, compared to usual care or other exercise programmes. These results are in line with the results of this review, which mainly showed no significant effects of the interventions on time to full RTW at one‐year follow‐up, although CBT and PST did show a significant effect for time to partial RTW.
Nieuwenhuijsen 2008 investigated the effect of interventions aimed at improving occupational health in depressed people and did not find clear evidence of an effect of medication, enhanced primary care, psychological interventions or a combination of these interventions with medication on sick leave in depressed workers. A systematic review evaluating the effect of workplace intervention on sick leave for all types of disorders only found a significant effect of a workplace intervention on the reduction of sick leave among workers with musculoskeletal disorders, compared to usual care. No effect was found of workplace intervention for back pain, upper‐extremity disorders or mental health problems (van Oostrom 2009).
Finally, de Boer 2011 recently published a systematic review on interventions to enhance RTW for cancer patients. This review showed that physical training was not effective in reducing time to RTW compared to usual care. Furthermore, medical interventions with a functioning conservative approach were not more effective in increasing RTW rates than more radical treatments. There was only a positive effect of multidisciplinary interventions (consisting of physical, psychological and vocational components) on RTW rates compared to care as usual.
When combining the results of this review and the reviews mentioned above, we can conclude that there are already quite a number of studies performed on the effects of different types of intervention on reducing sick leave or time to RTW for different study populations. Overall, none of the reviews showed high‐quality evidence that any type of intervention was effective in reducing sick leave or time to RTW.
Authors' conclusions
Implications for practice.
We found moderate‐quality evidence that time until partial return to work (RTW) at one‐year follow‐up was similar for workers receiving cognitive behavioural therapy (CBT) or no treatment. Results from low‐quality evidence indicate that CBT was not significantly effective in reducing time to full RTW at one‐year follow‐up compared to no treatment. Moderate‐quality evidence showed that problem solving therapy (PST) significantly enhanced partial RTW at one‐year follow‐up compared to non‐guideline based care but did not significantly enhance time to full RTW at one‐year follow‐up. A PST intervention could readily be implemented in a work context by occupational healthcare professionals to enable participants to take the first steps towards RTW. This might also reduce the costs related to sick leave. However, there was insufficient evidence that PST or CBT are effective in restoring individuals back to their full duties.
Implications for research.
International consensus should be reached on the terminology used to address the group of workers with adjustment disorders and assessment tools need to be developed and validated for diagnosing adjustment disorder. Almost every study in this review used different terms for describing complaints related to adjustment disorders, such as distress, stress, burnout and minor mental disorders, which impedes the making of comparisons.
Future studies should include more women and should focus research on participants with certain job types that are prone to adjustment disorders (e.g. distress complaints and burnout), such as nurses and teachers. Because of the large standard deviations related to mean days until RTW, which led to a loss of power, studies need to recruit at least 300 or more participants.
Researchers may consider exploring other possible interventions, in addition to CBT and PST interventions, to try to affect full RTW. Moreover, in future studies more attention should be paid to proper blinding of participants, care providers and data analysts, and to controlling of co‐interventions and compliance with the treatment protocol by care providers. Comparison conditions such as 'usual care' should be better defined and described. Otherwise, it is hard to compare the effects of different studies.
Finally, different types of work‐related outcome measures, such as work functioning and work productivity, should be used besides sick leave days and time until RTW to better understand how workers are performing following RTW.
Acknowledgements
We would like to thank the Cochrane Occupational Safety and Health Group for their valuable comments and the Finnish Institute of Occupational Health for receiving the first author as a guest at the institute to complete the necessary analyses and to finalise the review text.
Appendices
Appendix 1. CENTRAL search terms
| Search terms |
| Cochrane Central Register of Controlled Trials (CENTRAL) #1 MeSH descriptor ADJUSTMENT DISORDERS, this term only #2 MeSH descriptor BURNOUT, PROFESSIONAL, this term only #3 MeSH descriptor NEURASTHENIA, this term only #4 (mental NEXT disorder*):ti,ab #5 (adjustment NEXT disorder*):ti,ab,kw #6 (burnout):ti,ab,kw #7 (reactive NEXT disorder*):ti,ab,kw #8 (reactive NEXT depression):ti,ab,kw #9 (psychologic* or mental health or depress* or anxi* or somat* or distress or stress[TSC2] ):ti,ab,kw #10 ((sick* NEAR/3 leave) or (sick NEAR/3 list*) or (sick NEAR/3 absen*)):ti,ab,kw #11 (workplace or (work NEAR/3 related) or occupation* or job):ti,ab,kw #12 (#9 and (#10 or #11)) #13 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #12) #14 MeSH descriptor SICK LEAVE, this term only #15 MeSH descriptor ABSENTEEISM, this term only #16 MeSH descriptor REHABILITATION, VOCATIONAL, this term only #17 ((sick* NEAR/3 leave) or (sick NEAR/3 list*) or (sick NEAR/3 absen*)):ti,ab,kw #18 (return* NEAR/3 work*):ti,ab,kw #19 ((sick* or absen*) AND (workplace or (work NEAR/2 related) or occupation* or job)):ti,ab,kw #20 (#14 or #15 or #16 or #17 or #18 or #19) #21 (#13 and #20) |
Appendix 2. OVID MEDLINE search terms
| Search terms |
| OVID MEDLINE 1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomi#ed.ti,ab. 4. randomly.ab. 5. placebo.ab. 6. drug therapy.fs. 7. trial.ab. 8. groups.ab. 9. (control$ adj3 (trial or study)).ab,ti. 10. ((singl$ or doubl$ or tripl$ or trebl$) adj3 (blind$ or mask$ or dummy)).mp. 11. or/1‐10 12. ADJUSTMENT DISORDERS/ 13. BURNOUT, PROFESSIONAL/ 14. *MENTAL DISORDERS/ 15. NEURASTHENIA/ 16. adjustment disorder*.tw. 17. burnout.tw. 18. reactive disorder*.tw. 19. reactive depression.tw. 20. (psychologic* or mental health or mental disorder* or depress* or anxi* or somat* or distress or stress).tw. 21. ((sick* adj3 (leave or list* or absen*)) or (workplace or (work adj2 related)) or occupation* or job).tw. 22. 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or (20 and 21) 23. SICK LEAVE/ 24. ABSENTEEISM/ 25. REHABILITATION, VOCATIONAL/ 26. (sick adj3 (leave or list* or absen*)).tw. 27. (return* adj3 work*).tw. 28. ((sick* or absen*) adj5 (workplace or (work adj2 related) or occupation* or job)).tw. 29. or/23‐28 30. 11 and 22 and 29 |
Appendix 3. OVID EMBASE search terms
| Search terms |
| OVID EMBASE 1. randomized controlled trial.de. 2. randomization.de. 3. placebo.de. 4. placebo$.ti,ab. 5. randomi#ed.ti,ab. 6. randomly.ab. 7. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 8. factorial$.ti,ab. 9. allocat$.ti,ab. 10. assign$.ti,ab. 11. volunteer$.ti,ab. 12. crossover procedure.de. 13. (crossover$ or cross over$).ti,ab. 14. (quasi adj (experimental or random$)).mp. 15. (control$ adj3 (trial$ or study or studies or group$)).ti,ab. 16. ((animal or nonhuman) not (human and (animal or nonhuman))).de. 17. or/1‐15 18. 17 not 16 19. adjustment disorder/ 20. neurasthenia/ 21. burnout/ 22. job stress/ 23. *mental disease/ 24. reactive depression/ 25. adjustment disorder*.tw. 26. burnout.tw. 27. reactive disorder*.tw. 28. reactive depression.tw. 29. (psychologic* or mental health or mental disorder* or depress* or anxi* or somat* or distress or stress).tw. 30. ((sick* adj3 (leave or list* or absen*)) or (workplace or (work adj2 related)) or occupation* or job).tw. 31. 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or (29 and 30) 32. medical leave/ 33. absenteeism/ 34. vocational rehabilitation/ 35. (sick adj3 (leave or list* or absen*)).tw. 36. (return* adj3 work*).tw. 37. ((sick* or absen*) adj5 (workplace or (work adj2 related) or occupation* or job)).tw. 38. or/32‐37 39. 18 and 31 and 38 |
Appendix 4. OVID PsycINFO search terms
| Search terms |
| OVID PsycINFO 1. treatment effectiveness evaluation.sh. 2. clinical trials.sh. 3. mental health program evaluation.sh. 4. placebo.sh. 5. placebo$.ti,ab. 6. randomly.ab. 7. randomi#ed.ti,ab. 8. trial.ti,ab. 9. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 10. (control$ adj3 (trial$ or study or studies or group$)).ti,ab. 11. factorial$.ti,ab. 12. allocat$.ti,ab. 13. assign$.ti,ab. 14. volunteer$.ti,ab. 15. (crossover$ or cross over$).ti,ab. 16. (quasi adj (experimental or random$)).mp. 17. "2000".md. 18. or/1‐17 19. Adjustment Disorders/ 20. asthenia/ or myasthenia/ or neurasthenia/ 21. occupational stress/ or work related illnesses/ 22. *mental disorders/ 23. Reactive Depression/ 24. adjustment disorder*.tw. 25. burnout.tw. 26. reactive disorder*.tw. 27. reactive depression.tw. 28. (psychologic* or mental health or mental disorder* or depress* or anxi* or somat* or distress or stress).tw. 29. ((sick* adj3 (leave or list* or absen*)) or (workplace or (work adj2 related)) or occupation* or job).tw. 30. 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or (28 and 29) 31. employee leave benefits/ 32. employee absenteeism/ 33. reemployment/ 34. exp vocational rehabilitation/ 35. (sick adj3 (leave or list* or absen*)).tw. 36. (return* adj3 work*).tw. 37. ((sick* or absen*) adj5 (workplace or (work adj2 related) or occupation* or job)).tw. 38. or/31‐37 39. 18 and 30 and 38 |
Appendix 5. Web of Science search terms
| Search terms |
| Web of Science 1. Topic=(randomized controlled trial) 2. Topic=(randomi*ed) 3. Topic=(placebo) 4. Title=(trial) 5. Topic=(groups) 6. Topic=((singl* OR doubl* OR tripl* or trebl*) SAME (blind* OR mask* OR dummy)) 7. Topic=(control* SAME (trial* or study or studies or group*)) 8. Topic=(factorial* OR allocat* OR assign* OR volunteer* OR crossover* OR cross‐over*) 9. Topic=(quasi SAME (experimental or random*)) 10. 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 11. Topic=("adjustment disorder*") 12. Topic=(burnout) 13. Topic=(reactive SAME disorder*) 14. Topic=(reactive SAME depression) 15. Topic=(psychologic* OR mental health OR depress* OR anxi* OR somat* OR distress OR stress*) 16. Topic=((sick SAME (leave OR list* OR absen*)) OR (workplace OR (work SAME related) OR occupation* OR job)) 17. 15 AND 16 18. 11 OR 12 OR 13 OR 14 OR 17 19. Topic=(absentee*) 20. Topic=(rehabilitat* SAME (vocation* or workplace)) 21. Topic=((sick* SAME leave) OR (sick* SAME list*) OR (sick* SAME absen*)) 22. Topic=(return* SAME work*) 23. Topic=((sick* OR absen*) AND (workplace OR (work SAME related) OR occupation* OR job)) 24. 19 OR 20 OR 21 OR 22 OR 23 25. 10 AND 18 AND 24 |
Appendix 6. International Trial Registers (ICTRP, ClinicalTrials.gov) search terms
| Search terms |
| The WHO Trials Portal (ICTRP) and ClinicalTrials.gov was searched by entering individual keywords and phrases related to return to work: "return to work" "sick leave" "absenteeism" "vocational rehabilitation" "sickness absence" "workplace" |
Appendix 7. Study eligibility form
| Study ID |
| ID code: First author: Publication year: |
| Type of study |
|
Instruction: RCT: study is described as randomised □ RCT □ other study design → exclusion □ unsure |
| Type of participants |
| 1. Adults? □ yes □ no → exclusion □ unsure 2. Worker population? □ yes □ no → exclusion □ unsure 3. At least 50% of study population on sick leave? □ yes □ no → exclusion □ unsure 4. Participants with adjustment disorders? Instruction: adjustment disorder must be defined as either: ‐ diagnosis of adjustment disorder according to DSM‐IV ‐ level of stress‐related symptoms according to validated self rated or clinician‐rated instrument, published in peer‐reviewed journal □ yes □ no → exclusion □ unsure 5. Co‐morbidity? □ none or common mental disorder □ bipolar or psychotic features → exclusion □ unsure |
| Intervention |
| Is the study an intervention study? Instruction: interventions can be aimed at the workplace (e.g. job re‐design) or the individual (e.g. pharmacological or psychotherapeutic interventions) □ yes □ no → exclusion □ unsure |
| Outcome measure |
| Was sickness absence measured as outcome? □ yes □ no → exclusion □ unsure |
Data and analyses
Comparison 1. CBT versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Partial RTW, follow‐up one year | 3 | 159 | Mean Difference (IV, Random, 95% CI) | ‐8.78 [‐23.26, 5.71] |
| 2 Full RTW, follow‐up one year | 2 | 105 | Mean Difference (IV, Random, 95% CI) | ‐35.73 [‐113.15, 41.69] |
| 3 DASS distress score, follow‐up one year | 2 | 89 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐3.91, 4.02] |
Comparison 2. CBT versus non‐guideline based care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Full RTW, follow‐up one year | 2 | 78 | Mean Difference (IV, Random, 95% CI) | 19.81 [‐26.17, 65.79] |
| 2 DASS distress score, follow‐up three months | 2 | 75 | Mean Difference (IV, Random, 95% CI) | 0.66 [‐2.78, 4.11] |
| 3 DASS distress score, follow‐up four to 12 months | 2 | 54 | Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐6.06, 4.73] |
Comparison 3. PST versus non‐guideline based care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Partial RTW, follow‐up one year | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Full RTW, follow‐up one year | 2 | 342 | Mean Difference (IV, Random, 95% CI) | ‐17.73 [‐37.35, 1.90] |
| 3 Full RTW, follow‐up one to two years | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 4DSQ distress score, follow‐up three months | 3 | 559 | Mean Difference (IV, Random, 95% CI) | ‐1.69 [‐3.11, ‐0.27] |
| 5 4DSQ distress score, follow‐up four to 12 months | 3 | 540 | Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐1.76, 1.04] |
| 6 4DSQ distress score, follow‐up one to two years | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 4. PST versus CBT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Partial RTW, follow‐up one year | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Full RTW , follow‐up one year | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 5. Participatory PST versus PST.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Full RTW, follow‐up one year | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 4DSQ distress score, follow‐up three months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 4DSQ distress score, follow‐up four to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 6. CBT and physical relaxation versus physical relaxation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Rate of partial RTW, follow‐up one year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2 Rate of partial RTW, follow‐up one to two years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Rate of full RTW, follow‐up one year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4 Rate of full RTW, follow‐up one to two years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5 SMBQ score, follow‐up one year | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6 SMBQ score, follow‐up one to two years | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
Comparison 7. Individual CBT versus group CBT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Full RTW, follow‐up one year | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 DASS distress score, follow‐up three months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 DASS distress score, follow‐up four to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 8. CBT versus no treatment, full adjustment disorder diagnosis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Partial RTW, follow‐up one year | 2 | 99 | Mean Difference (IV, Random, 95% CI) | ‐24.92 [‐80.58, 30.74] |
Comparison 9. PST versus non‐guideline based care full adjustment disorder diagnosis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Full RTW, follow‐up one year | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | ‐24.0 [‐47.58, ‐0.42] |
| 2 4DSQ distress score, follow‐up three months | 1 | 139 | Mean Difference (IV, Fixed, 95% CI) | ‐1.90 [‐4.69, 0.89] |
| 3 4DSQ distress score, follow‐up four to 12 months | 1 | 110 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐3.86, 1.74] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bakker 2007.
| Methods | Trial design: cluster‐randomised controlled trial
Country: the Netherlands Healthcare setting: primary care in the Netherlands Work setting: employees in the Netherlands Randomisation procedure: cluster‐randomisation at the level of the treatment provider Recruitment: employees who visited consulting hours of the participating general practitioners were approached by mail by the research team Inclusion period: September 2003 to October 2004 Follow‐up: 12 months |
|
| Participants | Number: trial intervention: n = 227; comparison intervention: n = 206 Lost to follow‐up: 91 (44 trial intervention, 47 comparison intervention) Age, mean (SD): trial intervention: 42.0 (8.8) years; comparison intervention: 39.5 (9.6) years Sex: trial intervention: 67% female; comparison intervention: 65% female Duration of sick leave at baseline: not reported Inclusion: symptoms of stress‐related mental disorders (measured with 3 self reported questions of the Four‐Dimensional Symptom Questionnaire (4DSQ) distress scale), having paid work and being (partially) on sick leave for no longer than 3 months Exclusion: severe psychiatric disorders (mania or psychosis), terminal illness or inadequate command of the Dutch language |
|
| Interventions | Trial intervention:
Treatment type: minimal intervention for stress‐related mental disorders with sick leave (MISS) for general practice. Primary care physicians were instructed to use specific methods of communication to help the patient, within 3 consultations on a time‐contingent course, to achieve functional recovery.
Treatment providers: 24 primary care physicians Training of treatment providers: training of 2 x 3.5‐hour sessions and 2 x 2‐hour follow‐up sessions by a primary care physician and an occupational physician over a 6 to 10‐week period Treatment frequency/duration: no more than 3 consultations of 10 to 20 minutes Comparison intervention: Treatment type: usual care based on routine care by primary care physicians. Guidelines for the physicians are available on the treatment of depression and anxiety, but not specifically for stress‐related mental disorders. Treatment providers: 22 primary care physicians Training of treatment providers: the primary care physicians had received no information or advice about the content of the intervention Treatment frequency/duration: the mean number of visits to the primary care physician, counted from the day of sick leave up to 3 months, was 2.50 (standard deviation 2.23) |
|
| Outcomes | Work outcomes:
Self reported duration of sick leave in calendar days from the first day of sick leave until full (not partial) return to work, lasting for a period of at least 4 weeks without partial or full relapse into sick leave Other outcomes: Self reported symptoms of distress, depression, anxiety and somatization: 4DSQ. Measured at baseline and at 2, 6 and 12 months follow‐up. Care provided by primary care physicians: at 2 months follow‐up, the primary care physicians in both groups were asked to fill in a structured self reported questionnaire on the care provided and any diagnoses or working hypotheses in the past 3 months according to their electronic medical record |
|
| Notes | Source of funding: The Netherlands Organisation for Health Research and Development (ZonMw), (grant 4200.0003)
Ethics: approved by the medical ethics committee of the VU University Medical Center Missing data asked from author: (1) the mean and standard deviation (SD) for days until full RTW for each study group (2) the baseline difference between study groups on days of sick leave (3) blinding of care providers (4) differences in co‐interventions between study groups (5) treatment compliance in all study groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The PCPs [Primary Care Physicians] were randomly allocated at four different recruitment moments, with block sizes of n=10, n=7, n=14, and n=15. A standard procedure was followed to conceal allocation: the names of the PCPs were put on a list in random order. Independently, a randomly ordered list of codes was generated. These lists were brought together and the first PCP on the list was allocated to the group indicated by the first code, and so on." (p. 5, Bakker 2007) |
| Allocation concealment (selection bias) | Low risk | "A standard procedure was followed to conceal allocation: the names of the PCPs were put on a list in random order. Independently, a randomly ordered list of codes was generated. These lists were brought together and the first PCP on the list was allocated to the group indicated by the first code, and so on." (p. 5, Bakker 2007) |
| Blinding of participants | Low risk | "Patients and external interviewers were blinded. They were kept unaware that two different groups were formed, and were told that the study was about stress and sickness absence." (p. 5, Bakker 2007) |
| Blinding of care provider | Low risk | The PCPs in the intervention group treated all their patients according to the intervention and did not know which of their patients participated in the study. Only at the end of the study, the PCPs were asked for the diagnoses of the patients that had participated (based on unpublished information from the author). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Patients and external interviewers were blinded. They were kept unaware that two different groups were formed, and were told that the study was about stress and sickness absence." (p. 5, Bakker 2007) |
| Co‐interventions avoided or similar | Unclear risk | In Bakker 2010, on page 209, there is a table with information on the treatment delivered to the patients. From this table it can be seen that there is no significant difference between the 2 groups concerning referral to mental health care. Also, the mean number of GP visits is comparable for both groups. However, no information on use of psychotropic medication is given. |
| Treatment fidelity | High risk | "Overall, adherence to the specific approach to SMDs [stress related mental disorders] for both the GP [general practitioner] and the patient is questionable. Given the low rate of application of the MISS [minimal intervention for stress related mental disorders with sick leave] elements …" (p. 209, Bakker 2010) The intervention was not conducted similarly by the PCPs (based on unpublished data from the author). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | In Bakker 2007, on page 4, figure 1 shows comparable reasons for drop‐out in the 2 treatment groups. For the outcome full return to work, N = 30 (13%) and N = 32 (18%) were lost to follow‐up for the intervention and control group, respectively (total loss to follow‐up 14%). |
| Selective reporting (reporting bias) | High risk | In Bakker 2006, 2 secondary outcome measures, being problem evaluation and coping styles, were planned to be evaluated that are not analysed in Bakker 2007 (nor in Bakker 2010). These 2 outcome measures were planned to evaluate the effective components of the intervention. In Bakker 2007 and Bakker 2010 no information is given on why these outcome measures are not analysed. |
Blonk labour expert 2006.
| Methods | Trial design: randomised controlled trial
Country: the Netherlands Healthcare setting: occupational health care Work setting: self employed individuals insured for work disability at a private insurance company Randomisation procedure: randomisation on patient level Recruitment: self employed individuals who were unable to work owing to psychological complaints and had called upon their insurance company for disability benefits were approached by the research team Inclusion period: January 2001 to September 2002 (based on unpublished information from the author) Follow‐up: 360 days |
|
| Participants | Number: trial intervention 1: n = 40; trial intervention 2: n = 40; comparison intervention: n = 42 Lost to follow‐up: 33 (10 trial intervention 1, 10 trial intervention 2, 13 comparison intervention) Age, mean (SD): 42 (7.9) years Sex: 19% female Duration of sick leave at baseline: not reported Inclusion: sick leave caused by adjustment disorders (e.g. burnout and job stress) based on a structured diagnostic telephone interview using a shortened version of the Composite International Diagnostic Interview (CIDI) conducted by experienced psychologists Exclusion: serious psychiatric disorders (e.g. major depression, addictive disorders, post‐traumatic disorders, and other anxiety disorders) based on the structured diagnostic telephone interview, or individuals who did not want to postpone their current treatment during the research period |
|
| Interventions | Trial intervention 1:
Treatment type: individual intervention based on cognitive behavioural therapy (CBT) combined with a workplace intervention focusing on stressor reduction at work using a graded activity approach
Treatment providers: 6 labour experts Training of treatment providers: training in brief CBT‐based stress management with follow‐up meetings every 3 months during the course of the study Treatment frequency and duration: 5 to 6 sessions of approximately an hour, twice a week, which were held at home or at the workplace of the self employed Trial intervention 2: Treatment type: individual cognitive behavioural therapy (CBT) based on a highly structured protocol for the treatment of burnout or other adjustment disorders Treatment providers: psychologists Training of treatment providers: psychologists followed a highly structured protocol Treatment frequency and duration: 11 x 2‐weekly sessions of approximately 45 minutes per session Comparison intervention: Treatment type: no treatment intervention consisting of 2 brief medical checks of the legitimacy of the work‐disability benefit Treatment providers: general practitioners assigned by the private insurance company Training of treatment providers: not reported Treatment frequency and duration: a first visit shortly after the initial sick leave and a second visit approximately 4 months later |
|
| Outcomes | Work outcomes:
Length of time until partial RTW and the length of time until full RTW, extracted from the database system of the insurance company Other outcomes: Psychological complaints: Depression Anxiety Stress Scales (DASS). Measured at baseline and at 4 and 10 months follow‐up. Psychological complaints: Maslach Burnout Inventory (MBI‐NL). Measured at baseline and at 4 and 10 months follow‐up |
|
| Notes | Source of funding: not reported
Ethics: approved by ethical committee of the Netherlands Organisation for Applied Scientific Research (TNO) Missing data asked from author: (1) the randomisation procedure (2) the allocation concealment procedure (3) baseline differences between study groups on age, sex and days of sick leave (4) blinding of participants and care providers (5) differences in co‐interventions between study groups (6) treatment compliance in all study groups (7) reasons for drop‐out in all study groups (8) the use of an intention‐to‐treat analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | In Blonk 2006, page 133, it is stated that "122 self‐employed people finally enrolled in the study and were randomly assigned to one of three treatment conditions." Participants were randomised based on fate by using dice (based on unpublished information from the author) |
| Allocation concealment (selection bias) | Low risk | In Blonk 2006, page 133, it is stated that "122 self‐employed people finally enrolled in the study and were randomly assigned to one of three treatment conditions." Randomisation was conducted blindly by an independent researcher (based on unpublished information from the author) |
| Blinding of participants | Low risk | Participants were blinded for the treatment allocation. They did not receive information about the different possible treatments, but were only informed that they would receive treatment (based on unpublished information from the author). |
| Blinding of care provider | High risk | The care provider was not blinded (based on unpublished data from the author) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The outcome assessors were not blinded (based on unpublished data from the author) |
| Co‐interventions avoided or similar | Unclear risk | In Blonk 2006, page 133, it is described that "Individuals receiving psychotherapeutic treatment were asked to postpone this treatment for at least 4 months. … Individuals who did not want to postpone their current treatment during the research period were excluded." However, no information is available on use of psychotropic medication in the different study groups. |
| Treatment fidelity | Low risk | For the combined intervention, multiple feedback moments were planned to enhance treatment integrity. For the cognitive behavioural treatment intervention a strict protocol was used by which treatment providers needed to indicate what they did during every consultation and needed to check all the aspects of the protocol to ensure treatment compliance. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | In Blonk 2006, on page 136, the authors report drop‐out analyses. However, they only look at the comparability between the drop‐out group and the group that participated in the whole study. Based on unpublished information from the author, no significant differences were found in reasons for drop‐out between the 3 treatment groups. For the outcome partial return to work, N = 8 (20%), N = 7 (18%) and N = 8 (19%) were lost to follow‐up for the 2 treatment groups and the control group, respectively (total loss to follow‐up 19%) For full return to work, N = 5 (13%), N = 4 (10%) and N = 8 (19%) were lost to follow‐up (total loss to follow‐up 14%) |
| Selective reporting (reporting bias) | Low risk | In the methods section no outcome measures are mentioned that are not analysed in the results section. Furthermore, in the results section no findings are mentioned on measures not mentioned in the methods section. Survival analyses on return to work were performed as planned and the results of the questionnaires were analysed longitudinally as planned. |
Blonk psychologist 2006.
| Methods | Trial design: randomised controlled trial
Country: the Netherlands Healthcare setting: occupational health care Work setting: self employed individuals insured for work disability at a private insurance company Randomisation procedure: randomisation on patient level Recruitment: self employed individuals who were unable to work owing to psychological complaints and had called upon their insurance company for disability benefits were approached by the research team Inclusion period: January 2001 to September 2002 (based on unpublished information from the author) Follow‐up: 360 days |
|
| Participants | Number: trial intervention 1: n = 40; trial intervention 2: n = 40; comparison intervention: n = 42 Lost to follow‐up: 33 (10 trial intervention 1, 10 trial intervention 2, 13 comparison intervention) Age, mean (SD): 42 (7.9) years Sex: 19% female Duration of sick leave at baseline: not reported Inclusion: sick leave caused by adjustment disorders (e.g. burnout and job stress) based on a structured diagnostic telephone interview using a shortened version of the Composite International Diagnostic Interview (CIDI) conducted by experienced psychologists Exclusion: serious psychiatric disorders (e.g. major depression, addictive disorders, post‐traumatic disorders, and other anxiety disorders) based on the structured diagnostic telephone interview, or individuals who did not want to postpone their current treatment during the research period |
|
| Interventions | Trial intervention 1:
Treatment type: individual intervention based on cognitive behavioural therapy (CBT) combined with a workplace intervention focusing on stressor reduction at work using a graded activity approach
Treatment providers: 6 labour experts Training of treatment providers: training in brief CBT‐based stress management with follow‐up meetings every 3 months during the course of the study Treatment frequency and duration: 5 to 6 sessions of approximately an hour, twice a week, which were held at home or at the workplace of the self employed Trial intervention 2: Treatment type: individual cognitive behavioural therapy (CBT) based on a highly structured protocol for the treatment of burnout or other adjustment disorders Treatment providers: psychologists Training of treatment providers: psychologists followed a highly structured protocol Treatment frequency and duration: 11 x 2‐weekly sessions of approximately 45 minutes per session Comparison intervention: Treatment type: no treatment intervention consisting of 2 brief medical checks of the legitimacy of the work‐disability benefit Treatment providers: general practitioners assigned by the private insurance company Training of treatment providers: not reported Treatment frequency and duration: a first visit shortly after the initial sick leave and a second visit approximately 4 months later |
|
| Outcomes | Work outcomes:
Length of time until partial return to work (RTW) and the length of time until full RTW, extracted from the database system of the insurance company Other outcomes: Psychological complaints: Depression Anxiety Stress Scales (DASS). Measured at baseline and at 4 and 10 months follow‐up. Psychological complaints: Maslach Burnout Inventory (MBI‐NL). Measured at baseline and at 4 and 10 months follow‐up |
|
| Notes | Source of funding: not reported
Ethics: approved by ethical committee of the Netherlands Organisation for Applied Scientific Research (TNO) Missing data asked from author: (1) the randomisation procedure (2) the allocation concealment procedure (3) baseline differences between study groups on age, sex and days of sick leave (4) blinding of participants and care providers (5) differences in co‐interventions between study groups (6) treatment compliance in all study groups (7) reasons for drop‐out in all study groups (8) the use of an intention‐to‐treat analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | In Blonk 2006, page 133, it is stated that "122 self‐employed people finally enrolled in the study and were randomly assigned to one of three treatment conditions." Participants were randomised based on fate by using dice (based on unpublished information from the author) |
| Allocation concealment (selection bias) | Low risk | In Blonk 2006, page 133, it is stated that "122 self‐employed people finally enrolled in the study and were randomly assigned to one of three treatment conditions." Randomisation was conducted blindly by an independent researcher (based on unpublished information from the author) |
| Blinding of participants | Low risk | Participants were blinded for the treatment allocation. They did not receive information about the different possible treatments, but were only informed that they would receive treatment (based on unpublished information from the author). |
| Blinding of care provider | High risk | The care provider was not blinded (based on unpublished data from the author) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The outcome assessors were not blinded (based on unpublished data from the author) |
| Co‐interventions avoided or similar | Unclear risk | In Blonk 2006, page 133, it is described that "Individuals receiving psychotherapeutic treatment were asked to postpone this treatment for at least 4 months. … Individuals who did not want to postpone their current treatment during the research period were excluded." However, no information is available on use of psychotropic medication in the different study groups. |
| Treatment fidelity | Low risk | For the combined intervention, multiple feedback moments were planned to enhance treatment integrity. For the cognitive behavioural treatment intervention a strict protocol was used by which treatment providers needed to indicate what they did during every consultation and needed to check all the aspects of the protocol to ensure treatment compliance. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | In Blonk 2006, on page 136, the authors report drop‐out analyses. However, they only look at the comparability between the drop‐out group and the group that participated in the whole study. Based on unpublished information from the author, no significant differences were found in reasons for drop‐out between the 3 treatment groups. For the outcome partial return to work, N = 8 (20%), N = 7 (18%) and N = 8 (19%) were lost to follow‐up for the 2 treatment groups and the control group, respectively (total loss to follow‐up 19%) For full return to work, N = 5 (13%), N = 4 (10%) and N = 8 (19%) were lost to follow‐up (total loss to follow‐up 14%) |
| Selective reporting (reporting bias) | Low risk | In the methods section no outcome measures are mentioned that are not analysed in the results section. Furthermore, in the results section no findings are mentioned on measures not mentioned in the methods section. Survival analyses on return to work were performed as planned and the results of the questionnaires were analysed longitudinally as planned. |
Brouwers 2006.
| Methods | Trial design: randomised controlled trial
Country: the Netherlands
Healthcare setting: primary care in the city of Almere
Work setting: employees living in the city of Almere Randomisation procedure: block randomisation on patient level (block size 4) Recruitment: patients were recruited by 70 general practitioners (GPs) in the city of Almere Inclusion period: August 2001 to July 2003 Follow‐up: 18 months |
|
| Participants | Number: trial intervention: n = 98; comparison intervention: n = 96 Lost to follow‐up: 31 (trial 12 intervention, 19 comparison interventions) Age, mean (SD): trial intervention: 39.4 (9.1) years; comparison intervention: 40.1 (9.3) years Sex: trial intervention: 58% female; comparison intervention: 60% female Duration of sick leave at baseline: not reported Inclusion: suffering from emotional distress or minor mental disorders according to GP and self report; paid employment; on sick leave or planning to be on sick leave directly after visit to a GP for emotional or mental problems for no longer than 3 months; aged 18 to 60 years; Dutch‐speaking Exclusion: patients with moderately severe or severe mood disorders (major depressive disorder and bipolar disorder), agoraphobia, panic disorder and social phobia based on a Composite International Diagnostic Interview (CIDI); patients already receiving psychotherapy |
|
| Interventions | Trial intervention:
Treatment type: activating and supporting the patient to restore coping and to adopt a problem solving approach toward his/her problems, using a graded activity approach and based on a 3 stage model
Treatment providers: 11 social workers Training of treatment providers: a 3‐day training conducted by the researchers, including 2 follow‐up sessions at different times during the study period wherein adherence to the protocol was checked and knowledge was refreshed Treatment frequency and duration: 5 individual 50 minute sessions over 10 weeks Comparison intervention: Treatment type: usual care based on routine care by GPs, which comprised (any combination of) guidance and counselling by the GP, medication and referral to mental health care Treatment providers: 70 GPs Training of treatment providers: not reported Treatment frequency/duration: not reported |
|
| Outcomes | Work outcomes:
Sick leave duration (days between the first day of absenteeism and the first day of full or partial work resumption) Other outcomes: Anxiety and depression: Hospital Anxiety and Depression Scale (HADS). Measured at baseline and at 3, 6 and 18 months follow‐up. Anxiety and depression: Four‐Dimensional Symptom Questionnaire (4DSQ). Measured at baseline and at 3, 6 and 18 months follow‐up. Functional status: Short Form Health Survey (SF‐36). 8 individual sub scales, as well as the mental component summary scale score and the physical component summary scale score were computed and used in analyses. Measured at baseline and at 3, 6 and 18 months follow‐up. Patient satisfaction with treatment based on a questionnaire with 8 statements developed for this study. Measured at 3 months follow‐up. |
|
| Notes | Source of funding: The Netherlands Organisation for Health Research and Development (ZonMw), (grant 2200.0100)
Ethics: approved by the ethical committee of The Netherlands Institute of Mental Health and Addiction Missing data asked from author: (1) the number of participants in each study group on which the measurement of mean days until full RTW was based (2) the mean score and SD on the distress scale of the 4DSQ for each study group including the number of participants used for calculating these means (3) the randomisation procedure (4) the baseline difference between study groups on days of sick leave (5) blinding of care providers and outcome assessors (6) reasons for drop‐out in all study groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | In Brouwers 2006, on page 224, it is described that "Block randomization (block size 4) was carried out ..." and page 225 describes "98 participants were randomized to the experimental condition and 96 were randomized to the control group." Randomisation was conducted blindly by an administrative assistant who was not in contact with the patients, with the aid of a dice (evens being intervention group; based on unpublished information of the author) |
| Allocation concealment (selection bias) | Low risk | Brouwers 2006, page 224: "Block randomization (block size 4) was carried out by an administrative assistant who was not in contact with the patients and who sealed the results in consecutive envelopes" |
| Blinding of participants | High risk | Brouwers 2006, page 228: ".. it is also possible that patients randomized to the control group were disappointed to miss out on therapy.." and page 224: "The interviewers did not receive any information regarding group assignments, but they may have received information from patients." |
| Blinding of care provider | High risk | The social workers were not blinded to treatment allocation of participants (based on unpublished information of the author) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Brouwers 2006, page 224: "The interviewers did not receive any information regarding group assignments, but they may have received information from patients." The analyses were partly done by the principal investigator who was not blinded (based on unpublished data from the author) |
| Co‐interventions avoided or similar | High risk | Brouwers 2006, page 226; “In the first 3 months after baseline, 34 (35%) patients from the control group were referred to specialized mental health care by their GPs [general practitioners]. Seven patients (7%) from the intervention group were referred to specialized mental health care during or following the intervention. During the study period of 18 months, psychotropic medication was prescribed in 18.4% of patients of the intervention group and in 21.9% of the control group. Nonpsychotropic medication was prescribed in 60.2% of patients in the intervention group and in 50% of the control group.” And on page 228: "Thirty‐five percent of the control patients were referred to specialized mental health care, whereas normally about 10% of all patients with mental problems are referred by their GPs." |
| Treatment fidelity | High risk | Brouwers 2006, page 228 "... the intervention may not have been intensive enough or may not have been delivered with adequate fidelity. Although the registration forms suggested that the social workers had adhered well to the protocol, direct observation or recording of the sessions would have been preferable to self‐report. ... Thus, it is possible that the social workers were not as directive regarding work resumption as was originally intended." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Brouwers 2006, page 226: "The difference in drop‐out between the two groups was not significant." The reasons for drop‐out are not known (based on unpublished data from the author). For the outcome sick leave duration, N = 0 and N = 6 (6%) were lost to follow‐up for the intervention and control group, respectively, at 3 months follow‐up (total loss to follow‐up 3%). At 6 and 18 months follow‐up, N = 6 (6%) and N = 9 (9%) and N = 12 (12%) and N = 19 (19%) were lost to follow‐up (total loss to follow‐up 8% and 11%). |
| Selective reporting (reporting bias) | Low risk | In the methods section no outcome measures are mentioned that are not analysed in the results section. Furthermore, in the results section no findings are mentioned on measures not mentioned in the methods section. The techniques described in the methods section to analyse the data are also used in the results section. |
de Vente group 2008.
| Methods | Trial design: randomised controlled trial
Country: the Netherlands
Healthcare setting: clinical care in the Netherlands
Work setting: employees in the Netherlands Randomisation procedure: randomisation on patient level Recruitment: employees who were between 2 weeks and 6 months on sick leave were recruited through 2 occupational health services (n = 62), general practitioners (GPs) (n = 7), and by self referral in reaction to advertisements (n = 13) Inclusion period: not reported Follow‐up: 10 months |
|
| Participants | Number: trial intervention 1: n = 28; trial intervention 2: n = 28; comparison intervention: n = 26
Age, mean (SD): trial intervention 1: 41.6 (9.4) years; trial intervention 2: 41.5 (10.3) years; comparison intervention: 40.9 (9.6) years
Sex: trial intervention 1: 39% female; trial intervention 2: 43% female; comparison intervention: 35% female
Duration of sick leave at baseline, mean weeks (SD): trial intervention 1: 9.59 (7.21), trial intervention 2: 8.61 (7.23), comparison intervention: 8.73 (8.43) Inclusion: the presence of symptoms of neurasthenia; a primary role of work‐related stressors in the development of complaints; and the presence of impaired daily functioning as indicated by (partial) sick leave Exclusion: a primary diagnosis of major depression, social phobia, panic disorder, somatoform disorder other than undifferentiated, post‐traumatic stress disorder, obsessive‐compulsive disorder, hypomania or psychotic disorders as assessed with the short version of the Composite International Diagnostic Interview; severe depressive complaints; a medical condition that might explain fatigue (e.g. diabetes); excessive alcohol or drug use |
|
| Interventions | Trial intervention 1:
Treatment type: individual CBT‐based stress management training (SMT) including (a) psycho education, self assessment of stressors and complaints, lifestyle and relaxation techniques; (b) cognitive restructuring; (c) time management and goal setting; (d) assertiveness skills; and (e) evaluation and relapse prevention
Treatment providers: 12 experienced therapists with a master’s degree in clinical psychology Training of treatment providers: therapists were trained in delivering the treatment according to the protocol in 4 training sessions of 1 hour and received at least 4 supervision sessions per treatment by 1 of 2 experienced senior cognitive‐behavioural therapists Treatment frequency and duration: 12 sessions of approximately 1 hour Trial intervention 2: Treatment type: group CBT‐based stress management training (SMT) including (a) psycho education, self assessment of stressors and complaints, lifestyle and relaxation techniques; (b) cognitive restructuring; (c) time management and goal setting; (d) assertiveness skills; and (e) evaluation and relapse prevention Treatment providers: 12 experienced therapists with a master’s degree in clinical psychology Training of treatment providers: therapists were trained in delivering the treatment according to the protocol in 4 training sessions of 1 hour and received at least 4 supervision sessions per treatment by 1 of 2 experienced senior cognitive‐behavioural therapists Treatment frequency and duration: 12 sessions of approximately 2 hours with 8 participants Comparison intervention: Treatment type: usual care based on routine care by an occupational physician or GP, or a maximum of 5 treatment sessions by a psychologist or social worker Treatment providers: occupational physicians, GPs, psychologists, social workers Training of treatment providers: not reported Treatment frequency/duration: the mean number of consultations during the treatment phase of the OP was 2.56 and of the GP, 1.44. The mean number of sessions from a psychologist or social worker received by a subgroup of 11 patients was 4.64. |
|
| Outcomes | Work outcomes:
Number of days absent measured at 4, 7 and 10 months follow‐up Time until complete work resumption Other outcomes: Burnout: Maslach Burnout Inventory (MBI‐NL). Measured at baseline and at 4, 7 and 10 months of follow‐up. Fatigue: Checklist Individual Strength (CIS). Measured at baseline and at 4, 7 and 10 months of follow‐up. Depression, anxiety and stress complaints: Depression Anxiety Stress Scales (DASS). Measured at baseline and at 4, 7 and 10 months of follow‐up. Treatment satisfaction and perceived effectiveness with the care received. Measured with 4 questions at 4 months follow‐up. |
|
| Notes | Source of funding: The Netherlands Organisation for Health Research and Development (ZonMw), The Netherlands Organization for Scientific Research (NWO; Concerted research action: “Fatigue at work”)
Ethics: approved by ethical committee of the Department of Psychology of the University of Amsterdam Missing data asked from author: (1) the number of participants in each study group on which the measurement of mean weeks until full RTW and mean days of sick leave during follow‐up was based (2) the SD belonging to the mean weeks until full RTW for all study groups (3) blinding of participants, care providers and outcome assessors (4) differences in co‐interventions between study groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | de Vente 2008, page 218: “Randomization was performed by a person independent of the study with use of a computer generated list of random numbers in blocks of 24.” |
| Allocation concealment (selection bias) | Low risk | de Vente 2008, page 218: “Randomization was performed by a person independent of the study...” |
| Blinding of participants | High risk | Participants were informed about the treatment condition they were randomised to after baseline measurement (based on unpublished information from the author). |
| Blinding of care provider | High risk | Care providers knew about the different treatments and were not blinded (based on unpublished information from the author) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The researcher who performed the analyses was not blinded (based on unpublished information from the author) |
| Co‐interventions avoided or similar | Low risk | de Vente 2008, page 219: “It should be noted that the SMTs [stress management trainings] were given in addition to regular visits to an OP [occupational physician]. The mean number of OP consultations in the SMT conditions during the treatment phase was 3.00. CAU [care as usual] was defined as regular visits to an OP, GP [general practitioner], or a maximum of five treatment sessions by a psychologist or social worker. The mean number of consultations during the treatment phase of the OP was 2.56 and of the GP, 1.44. The mean number of sessions from a psychologist or social worker received by a subgroup of 11 patients was 4.64.” Use of psychotropic medication was low; only 5 participants used psychotropic medication (antidepressive or anxiolyticum) |
| Treatment fidelity | Low risk | de Vente 2008, page 219: “Treatment integrity was high. Delivery of the SMT protocol was registered for 81% of the core treatment elements included in the protocol. Of these registered elements, 96% was delivered according to protocol.” |
| Incomplete outcome data (attrition bias) All outcomes | High risk | In de Vente 2008, figure 1 shows differences in reasons for drop‐out between the study groups. For the outcome absenteeism at 4 months follow‐up, N = 2 (7%), N = 3 (11%) and N = 9 (35%) were lost to follow‐up in the 2 treatment groups and the control group, respectively (total loss to follow‐up (17%). At 7 and 10 months follow‐up these numbers were: N = 3 (11%), N = 4 (14%) and N = 10 (38%) and N = 3 (11%), N = 5 (18%) and N = 12 (46%) (total loss to follow‐up 21% and 24%). |
| Selective reporting (reporting bias) | Low risk | All outcome variables described in the methods section are analysed in the results section. Subgroup analyses as presented in the introduction and methods section were performed. Longitudinal results are presented as described. All results with means and standard deviations. |
de Vente individual 2008.
| Methods | Trial design: randomised controlled trial
Country: the Netherlands
Healthcare setting: clinical care in the Netherlands
Work setting: employees in the Netherlands Randomisation procedure: randomisation on patient level Recruitment: employees who were between 2 weeks and 6 months on sick leave were recruited through 2 occupational health services (n = 62), general practitioners (GPs) (n = 7), and by self referral in reaction to advertisements (n = 13) Inclusion period: not reported Follow‐up: 10 months |
|
| Participants | Number: trial intervention 1: n = 28; trial intervention 2: n = 28; comparison intervention: n = 26
Age, mean (SD): trial intervention 1: 41.6 (9.4) years; trial intervention 2: 41.5 (10.3) years; comparison intervention: 40.9 (9.6) years
Sex: trial intervention 1: 39% female; trial intervention 2: 43% female; comparison intervention: 35% female
Duration of sick leave at baseline, mean weeks (SD): trial intervention 1: 9.59 (7.21), trial intervention 2: 8.61 (7.23), comparison intervention: 8.73 (8.43) Inclusion: the presence of symptoms of neurasthenia; a primary role of work‐related stressors in the development of complaints; and the presence of impaired daily functioning as indicated by (partial) sick leave Exclusion: a primary diagnosis of major depression, social phobia, panic disorder, somatoform disorder other than undifferentiated, post‐traumatic stress disorder, obsessive‐compulsive disorder, hypomania or psychotic disorders as assessed with the short version of the Composite International Diagnostic Interview; severe depressive complaints; a medical condition that might explain fatigue (e.g. diabetes); excessive alcohol or drug use |
|
| Interventions | Trial intervention 1:
Treatment type: individual CBT‐based stress management training (SMT) including (a) psycho education, self assessment of stressors and complaints, lifestyle and relaxation techniques; (b) cognitive restructuring; (c) time management and goal setting; (d) assertiveness skills; and (e) evaluation and relapse prevention
Treatment providers: 12 experienced therapists with a master’s degree in clinical psychology Training of treatment providers: therapists were trained in delivering the treatment according to the protocol in 4 training sessions of 1 hour and received at least 4 supervision sessions per treatment by 1 of 2 experienced senior cognitive‐behavioural therapists Treatment frequency and duration: 12 sessions of approximately 1 hour Trial intervention 2: Treatment type: group CBT‐based stress management training (SMT) including (a) psycho education, self assessment of stressors and complaints, lifestyle, and relaxation techniques; (b) cognitive restructuring; (c) time management and goal setting; (d) assertiveness skills; and (e) evaluation and relapse prevention Treatment providers: 12 experienced therapists with a master’s degree in clinical psychology Training of treatment providers: therapists were trained in delivering the treatment according to the protocol in 4 training sessions of 1 hour and received at least 4 supervision sessions per treatment by 1 of 2 experienced senior cognitive‐behavioural therapists Treatment frequency and duration: 12 sessions of approximately 2 hours with 8 participants Comparison intervention: Treatment type: usual care based on routine care by an occupational physician or GP, or a maximum of 5 treatment sessions by a psychologist or social worker Treatment providers: occupational physicians, GPs, psychologists, social workers Training of treatment providers: not reported Treatment frequency/duration: the mean number of consultations during the treatment phase of the OP was 2.56 and of the GP, 1.44. The mean number of sessions from a psychologist or social worker received by a subgroup of 11 patients was 4.64. |
|
| Outcomes | Work outcomes:
Number of days absent measured at 4, 7 and 10 months follow‐up Time until complete work resumption Other outcomes: Burnout: Maslach Burnout Inventory (MBI‐NL). Measured at baseline and at 4, 7 and 10 months of follow‐up. Fatigue: Checklist Individual Strength (CIS). Measured at baseline and at 4, 7 and 10 months of follow‐up. Depression, anxiety and stress complaints: Depression Anxiety Stress Scales (DASS). Measured at baseline and at 4, 7 and 10 months of follow‐up. Treatment satisfaction and perceived effectiveness with the care received. Measured with 4 questions at 4 months follow‐up. |
|
| Notes | Source of funding: The Netherlands Organisation for Health Research and Development (ZonMw), The Netherlands Organization for Scientific Research (NWO; Concerted research action: “Fatigue at work”)
Ethics: approved by ethical committee of the Department of Psychology of the University of Amsterdam Missing data asked from author: (1) the number of participants in each study group on which the measurement of mean weeks until full RTW and mean days of sick leave during follow‐up was based (2) the SD belonging to the mean weeks until full RTW for all study groups (3) blinding of participants, care providers and outcome assessors (4) differences in co‐interventions between study groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | de Vente 2008, page 218: “Randomization was performed by a person independent of the study with use of a computer generated list of random numbers in blocks of 24.” |
| Allocation concealment (selection bias) | Low risk | de Vente 2008, page 218: “Randomization was performed by a person independent of the study...” |
| Blinding of participants | High risk | Participants were informed about the treatment condition they were randomised to after baseline measurement (based on unpublished information from the author). |
| Blinding of care provider | High risk | Care providers knew about the different treatments and were not blinded (based on unpublished information from the author) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The researcher who performed the analyses was not blinded (based on unpublished information from the author) |
| Co‐interventions avoided or similar | Low risk | de Vente 2008, page 219: “It should be noted that the SMTs [stress management trainings] were given in addition to regular visits to an OP [occupational physician]. The mean number of OP consultations in the SMT conditions during the treatment phase was 3.00. CAU [care as usual] was defined as regular visits to an OP, GP [general practitioner], or a maximum of five treatment sessions by a psychologist or social worker. The mean number of consultations during the treatment phase of the OP was 2.56 and of the GP, 1.44. The mean number of sessions from a psychologist or social worker received by a subgroup of 11 patients was 4.64.” Use of psychotropic medication was low; only 5 participants used psychotropic medication (antidepressive or anxiolyticum) |
| Treatment fidelity | Low risk | de Vente 2008, page 219: “Treatment integrity was high. Delivery of the SMT protocol was registered for 81% of the core treatment elements included in the protocol. Of these registered elements, 96% was delivered according to protocol.” |
| Incomplete outcome data (attrition bias) All outcomes | High risk | In de Vente 2008, figure 1 shows differences in reasons for drop‐out between the study groups. For the outcome absenteeism at 4 months follow‐up, N = 2 (7%), N = 3 (11%) and N = 9 (35%) were lost to follow‐up in the 2 treatment groups and the control group, respectively (total loss to follow‐up (17%). At 7 and 10 months follow‐up these numbers were: N = 3 (11%), N = 4 (14%) and N = 10 (38%)and N = 3 (11%). |
| Selective reporting (reporting bias) | Low risk | All outcome variables described in the methods section are analysed in the results section. Subgroup analyses as presented in the introduction and methods section were performed. Longitudinal results are presented as described. All results with means and standard deviations. |
Rebergen 2009.
| Methods | Trial design: randomised controlled trial
Country: the Netherlands
Healthcare setting: Occupational Health Care
Work setting: employees of the Dutch police force Randomisation procedure: block randomisation on patient level (block size 50) Recruitment: each employee on sick leave due to mental health problems was invited to meet with a case manager of the Occupational Health Service (OHS) within 1 week. This case manager informed the employee about the study and planned a consultation with an occupational physician (OP) in the first 2 weeks of sick leave. To enhance recruitment 1 of the researchers (DB), who was allowed to check the registration system of the OHS, informed the OP when a potential participant would come for consultation. Each employee who consulted an OP, and was still on sick leave due to mental health problems, was then asked by the OP to participate in the study Inclusion period: January 2002 to January 2005 Follow‐up: 12 months |
|
| Participants | Number: trial intervention: n = 125; comparison intervention: n = 115 Lost to follow‐up: 16 Age, mean (SD): trial intervention: 38.8 (8.4) years; comparison intervention: 40.0 (9.5) years Sex: trial intervention: 51.2% male; comparison intervention: 60.5% male Duration of sick leave at baseline; mean (SD) days of sick leave in previous year: trial intervention: 56.9 (61.4); comparison intervention: 56.1 (86.0) Inclusion: mental health problems according to the diagnosis of the OP; sick leave at the moment of inclusion; sick leave period did not start before 2002 Exclusion: mental health symptoms that were caused by somatic illness; disagreement between OP and employee about the diagnosis; lack of confidence in the relation between OP and employee |
|
| Interventions | Trial intervention:
Treatment type: treatment by occupational physicians according to the guideline of employees on sick leave due to mental health problems; the guideline is based on an activating approach, time contingent process evaluation and cognitive behavioural principles
Treatment providers: 5 occupational physicians Training of treatment providers: a 3‐day course with 10 to 15 OPs, knowledge about and practice in working with the guideline were educated and exchanged Treatment frequency and duration: mean number of consultations with OP = 3.4 Comparison intervention: Treatment type: minimal involvement of the OP and access to treatment by a psychologist Treatment providers: 5 occupational physicians (same OPs as intervention group) and psychologists (number unknown) Training of treatment providers: a 3‐day course with 10 to 15 OPs, knowledge about and practice in working with the guideline were educated and exchanged; the psychologists were working according to cognitive behavioural principles, the standard therapy offered was based on protocols of the Dutch Institute for Work and Stress Treatment frequency/duration: mean number of consultations with OP = 3.3, 82% of the participants was immediately referred to a psychologist |
|
| Outcomes | Work outcomes:
Productivity loss: first and full RTW operationalised as duration of sick leave due to mental health problems in calendar days from the moment of inclusion to first (partial or full) and full RTW, respectively, in own or equal earnings; total productivity loss: duration of sick leave days until full RTW added with number of days of recurrences of sick leave in the 1‐year follow‐up Other outcomes: Treatment satisfaction of employee and employer: short version of the Patient Satisfaction with Occupational Health professionals Questionnaire. Measured at baseline, during treatment and after full RTW or 1‐year follow‐up (when full RTW did not happen). Treatment satisfaction of OP: self made questionnaire. Measured at 1‐year follow‐up. |
|
| Notes | Source of funding: the Dutch Ministry of Internal Affairs and Kingdom Relations, the Health Insurance for the Dutch Police (DGVP), occupational health service Commit and the VU University Medical Center in the Netherlands
Ethics: the study design, protocol and procedures were approved by the Medical Ethics Review Committee of the VU University Medical Center Missing data asked from the author: (1) the number of participants in each study group with an adjustment disorder according to the cut‐off score on the stress scale of the DASS (2) baseline differences between the subgroups with adjustment disorders on age, sex and days of sick leave (3) number of drop‐outs among the subgroups with adjustment disorders at each follow‐up measurement (4) mean and SD of days until partial and full RTW for the subgroups with adjustment disorders |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Rebergen 2007, page 3: "Block randomisation (size 50) was done on the patient level before the start of the study using SPSS." |
| Allocation concealment (selection bias) | Low risk | Rebergen 2007, page 3: "The randomization results were sealed in 250 consecutive envelopes. The OPs [occupational physicians] were informed about the study procedure and received sealed numbered envelopes, in which the treatment was stated which they had to provide. They were allowed to open an envelope only after an employee voluntarily signed an informed consent. Then the OP told the participant to which treatment he or she was assigned. To minimize the risk of irregularities by letting OPs open their treatment concealment themselves, randomization was checked by an independent researcher (AvdB) one year after the start of the study. At the end of the study this procedure was repeated by checking the treatment allocation of all the in‐ and excluded persons." |
| Blinding of participants | High risk | Rebergen 2009, page 2: "Participants, employers, and OPs were not blinded for the intervention." |
| Blinding of care provider | High risk | Rebergen 2009, page 2: "Participants, employers, and OPs were not blinded for the intervention." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Rebergen 2009, page 2: "The researchers were blinded for the treatment allocation and for protocol compliance as well." |
| Co‐interventions avoided or similar | High risk | In Rebergen 2010, page 493, table 2 shows that in the intervention group participants were significantly more referred to a company social worker compared to CAU |
| Treatment fidelity | High risk | In Rebergen 2010, page 494, table 3 shows that there are very little differences between the guideline use (which was the intervention being studied) in the intervention and usual care group (the usual care group could also use the guideline). It was expected that the different aspects of the guideline would have been used more often in the intervention group; so the compliance is not acceptable for this group. Furthermore on page 495 the authors mention: “Psychological treatments were indeed significantly higher in usual care, but referral patterns to a company social worker were significantly higher in the guideline group. This caused an unexpected lack of contrast between the groups, as the intended and expected involvement of the OP in the guideline group did not seem to materialize, as no differences in guideline adherence were found between the groups.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Rebergen 2009, page 308: "In total 16 participants were lost to follow‐up: 15 because they left the police force during their RTW [return to work] process and one committed suicide." For the subgroup of participants with adjustment disorders (N = 86 in both study groups) there were no drop‐outs in the intervention group and only 3 drop‐outs in the control group (based on unpublished information of the author). It is unlikely that this will have biased the results. For the outcome partial return to work, N = 0 and N = 2 (2%) were lost to follow‐up for the intervention and control group, respectively. For full return to work, N = 0 and N = 3 (3%) were lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | All outcomes described in the protocol (Rebergen 2007) are also reported in Rebergen 2009, 2009b and 2010. Furthermore, potential effect‐modifiers were pre‐defined in the protocol (2007) and tested as planned in the effectiveness article (2009). The data analysis techniques were used as planned. |
Stenlund 2009.
| Methods | Trial design: randomised controlled trial
Randomisation procedure: randomisation on patient level
Country: Sweden
Healthcare setting: clinical care at the Stress Clinic of the University Hospital of Umeå
Work setting: employees in Umeå
Recruitment: patients were consecutively screened for participation; most patients were referred to the Stress Clinic by general practitioners (GPs) who were informed about the study and the eligibility criteria Inclusion period: December 2002 to December 2004 Follow‐up: 2 years |
|
| Participants | Number: trial intervention: n = 67; comparison intervention: n = 69 Lost to follow‐up: 29 (9 from the trial intervention, 20 from the comparison intervention) Age, mean (SD): trial intervention: 40.9 (7.1) years; comparison intervention: 42.3 (7.8) years Sex: trial intervention: 73% female; comparison intervention: 71% female Duration of sick leave at baseline, mean days (SD): trial intervention: 326 (176); comparison intervention: 344 (165) Inclusion: diagnosis of burnout; 25 to 55 years of age; sick leave for burnout ≥ 25% of the working hours during the previous 3 to 24 months; an average score ≥ 4.6 on the Shirom–Melamed Burnout Questionnaire (SMBQ) Exclusion: other diseases that could result in future sick leave due to fatigue and/or stress related symptoms (for example, chronic infections, chronic fatigue syndrome, endocrine disorders); other diseases or treatments that could interfere with active participation; post‐traumatic stress disorders (PTSD); unemployment for more than 2 years; known abuse of alcohol or drugs; speech and language difficulties; need for individual therapy; participation in other intervention studies |
|
| Interventions | Trial intervention:
Treatment type: Cognitively oriented Behavioural Rehabilitation (CBR), in parallel with CBR, patients performed Qigong consisting of (1) warm‐up movements; (2) basic movements to affect body awareness, balance and co‐ordination, breathing and muscular tension; and (3) relaxation and mindfulness meditation
Treatment providers: 1 group leader gave CBR, 1 physiotherapist supervised the Qigong Training of treatment providers: the group leader was specially trained in CBR and the physiotherapist was trained in Qigong Treatment frequency and duration: the CBR programme consisted of 30 sessions of 3 hours spread over 1 year with 20 meetings in the first 6 months and 10 meetings in the last 6 months, there were also 3 group meetings to which spouses and/or relatives were invited during the first year; the programme had short follow‐up meetings 3, 6 and 12 months after the 1‐year rehabilitation; the Qigong programme consisted of 1‐hour sessions once a week during 1 year Comparison intervention: Treatment type: Qigong consisting of (1) warm‐up movements; (2) basic movements to affect body awareness, balance and co‐ordination, breathing and muscular tension; and (3) relaxation and mindfulness meditation Treatment providers: 1 physiotherapist supervised the Qigong Training of treatment providers: the physiotherapist was trained in Qigong (not the same therapist that the intervention group had) Treatment frequency and duration: 1‐hour sessions once a week during 1 year |
|
| Outcomes | Work outcomes:
Sick leave rate (100%, 75%, 50%, 25%, 0%) based on information received from the Social Insurance Agency (sick leave includes sickness benefit, activity and sickness compensation and rehabilitation compensation). Measured at baseline, 1‐year and 2‐year follow‐up. Other outcomes: Burnout: Shirom–Melamed Burnout Questionnaire (SMBQ). Measured at baseline, 6 months, 1‐year, 1.5‐year and 2‐year follow‐up. Self rated stress behaviour and reactions in everyday living: Everyday Life Stress Scale (ELSS). Measured at baseline, 6 months, 1‐year, 1.5‐year and 2‐year follow‐up. Fatigue: Checklist Individual Strength questionnaire (CIS). Measured at baseline, 6 months, 1‐year, 1.5‐year and 2‐year follow‐up. Self rated affective syndromes: Self‐Rating Scale for Affective Syndromes (CPRS‐S‐A). Measured at baseline, 6 months, 1‐year, 1.5‐year and 2‐year follow‐up. |
|
| Notes | Source of funding: the Swedish Council for Working Life and Social Research, the Västerbotten County Council and the Swedish Social Insurance Agency
Ethics: the Research Ethics Committee of Umeå University approved the study Missing data asked from the author: (1) blinding of participants, care providers and outcome assessors (2) differences in co‐interventions between study groups (3) treatment compliance in all study groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stenlund 2009, page 296: “An independent person arranged opaque sealed consecutively numbered envelopes in accordance with a computer‐generated randomization list.” |
| Allocation concealment (selection bias) | Low risk | Stenlund 2009, page 296: “An independent person arranged opaque sealed consecutively numbered envelopes in accordance with a computer‐generated randomization list. After baseline assessments, the research nurse allocated the patients to either program A or to program B, by opening the envelopes.” |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of care provider | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Co‐interventions avoided or similar | High risk | Stenlund 2009, page 299: “ A fourth of the patients in program A and almost half of the patients in program B reported having a complementary treatment outside the Stress Clinic during the intervention period (Table 2; p = 0.058). The complementary treatments included acupuncture, massage, and different treatments of body awareness. Significantly more patients in program B (44%) than in program A (16%) had additional individual or group conversational therapy outside the Stress Clinic during the intervention period.” |
| Treatment fidelity | Unclear risk | Stenlund 2009, page 299: “The patients who completed program A attended an average of 25±3.1 of the 30 CBR group sessions and 21.7±7.5 of the 35 Qigong sessions. The mean attendance of Qigong sessions by patients in program B was 21.6±7.9.” No information is given on how many sessions a participant must follow to speak of acceptable compliance. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | In Stenlund 2009, figure 1 shows differences in reasons for drop‐out between the study groups. For the outcome rate of return to work, N = 7 (10%) and N = 19 (27%) were lost at 6 months follow‐up in the intervention and control group, respectively. For 12 months follow‐up these numbers were N = 9 (13%) and N = 20 (29%), for 18 months follow‐up N = 14 (21%) and N = 33 (48%) and for 2 years follow‐up N = 13 (19%) and N = 30 (43%). |
| Selective reporting (reporting bias) | Low risk | No outcome measures were omitted or added in the results. Longitudinal analyses were performed, as planned (no selective time point was chosen). Outcomes on different time points are given (in table) together with P values (in text). |
van der Klink 2003.
| Methods | Trial design: cluster‐randomised controlled trial
Randomisation procedure: cluster randomisation on treatment provider level
Country: the Netherlands
Healthcare setting: in‐company occupational health service
Work setting: employees of the Dutch postal service (Royal KPN)
Recruitment: employees who were 2 weeks on sick leave were referred to their occupational physician and were asked by their occupational physician to participate in the study Inclusion period: May 1995 to July 1996 Follow‐up: 12 months |
|
| Participants | Number: trial intervention: n = 109; comparison intervention: n = 83 Lost to follow‐up: none for the primary outcome measure; 75 for the secondary outcome measures Age, mean (SD): trial intervention: 39 (8.0) years; comparison intervention: 42 (8.8) years Sex: trial intervention: 34% female; comparison intervention: 41% female Duration of sick leave at baseline, mean number of spells in previous year (SD): trial intervention: 2.2 (1.9); comparison intervention: 2.3 (1.6) Inclusion: first sick leave caused by an adjustment disorder based on DSM‐IV criteria Exclusion: other disorder based on DSM‐IV criteria; treatment for an adjustment disorder in the previous year; physical comorbidity with an effect on absenteeism; communication in Dutch impossible; pregnancy or childbirth in the previous 6 months; termination of employment at KPN within 6 months |
|
| Interventions | Trial intervention:
Treatment type: the intervention comprised a graded activity approach and was based on a 3‐stage model, resembling stress inoculation training, a form of cognitive behavioural treatment Treatment providers: 17 occupational physicians Training of treatment physicians: occupational physicians were trained during a 3‐day training course by experienced trainers with backgrounds in psychology, occupational medicine and general practice. They were trained in multiple cognitive‐behavioural, prescriptive interventions to stimulate the patients’ acquisition of problem solving skills, and to structure the patients’ daily activities. Treatment frequency and duration: 4 or 5 consultations in the first 6 weeks of sickness leave with a total length over these sessions of at least 90 minutes; at least 3 contacts with company management were prescribed in the first 3 months; at least 1 session was prescribed after work resumption, focusses on relapse prevention Comparison intervention: Treatment type: usual care based on empathic counselling, instruction about stress, lifestyle advice and discussion of work problems with the patient and company management Treatment providers: 16 occupational physicians Training of treatment providers: no training in guidance, but a 3‐hour session on the use of the inclusion and exclusion criteria and on the recording of guidance activities Treatment frequency and duration: there was neither a professional nor a company guideline available for the care of patients with adjustment disorders |
|
| Outcomes | Work outcomes:
Time to partial and full RTW
Duration of sickness leave
Partial and full RTW rate at 3 and 12 months follow‐up
Incidence of recurrent sick leave in the year following full RTW
Time to first recurrent sick leave in the year following full RTW Absenteeism data were obtained from the company’s computerised record system Other outcomes: Psychopathology: Four‐Dimensional Symptom Questionnaire (4DSQ). Measured at baseline and at 3 and 12 months follow‐up. Psychopathology: Symptom Checklist‐90 (SCL‐90). Measured at baseline and at 3 and 12 months follow‐up. Mastery: Mastery Scale. Measured at baseline and at 3 and 12 months follow‐up. |
|
| Notes | Source of funding: the Occupational Health Service of Royal KPN; the Netherlands Organisation of Scientific Research (NWO); TNO Work and Employment; the Foundation for Quality in Occupational Health (SKB)
Ethics: not reported Missing data asked from author: (1) the randomisation procedure (2) blinding of care providers and outcome assessors (3) differences in co‐interventions between study groups (4) treatment compliance in all study groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | van der Klink 2003, page 430: "The randomisation was conducted blindly by an independent research assistant who assigned two groups of occupational physicians to the two study groups." An independent research assistant performed the randomisation based on a computer‐generated list (based on unpublished information from the author) |
| Allocation concealment (selection bias) | Low risk | van der Klink 2003, page 430: "The randomisation was conducted blindly by an independent research assistant who assigned two groups of occupational physicians to the two study groups." |
| Blinding of participants | Low risk | van der Klink 2003, page 430: "Patients were not aware of which treatment they received." |
| Blinding of care provider | High risk | The occupational physicians (OPs) were not blinded for the intervention (based on unpublished information from the author) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | van der Klink 2003, page 431: "Research assistants who administered the questionnaires had no knowledge of which study group responders belonged to." However, no information is available on whether absenteeism data obtained from the company's record system were collected by a person blinded to intervention/control group, and whether researchers analysing the data were blinded |
| Co‐interventions avoided or similar | High risk | Use of co‐interventions (such as contacts with a psychologist or use of psychotropic medication) was somewhat higher in the intervention group (based on unpublished information from the author) |
| Treatment fidelity | Low risk | In van der Klink 2003, on page 430 it is described that “OPs had to plan four or five consultations in the first six weeks of sickness leave with a total length over these sessions of at least 90 minutes. … At least three contacts with company management were prescribed in the first three months. For the intervention group at least one session was prescribed after work resumption, focusses on relapse prevention.” On page 434 the following is reported: “Total contact duration was about 25 minutes longer in the intervention group compared with the control group over approximately five consultations for both groups, a significant difference. Ninety three per cent of the OPs in the intervention group applied at least one specific tool versus 20% of the OPs in the control group.” Contacts with the company management and the relapse prevention session were, overall, good adhered to by the OPs. Furthermore, during the study period feedback moments were organised to enhance adherence to the intervention protocol (based on unpublished information from the author). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | van der Klink 2003, page 434: “We finally conducted an analysis between completers on 12 months (n = 117) and drop‐outs since the 3 months assessment (n = 36). There was only one significant difference: completers had a lower incidence of absenteeism periods in the year before the onset of this period (mean number of spells (2.0 v 2.7, p < 0.05). This difference was greater for the intervention group (1.8 v 3.0 periods of absenteeism) than for the control group (2.1 v 2.3 absenteeism periods).” However, for the primary outcome absenteeism all included patients could be analysed and, thus, there were no incomplete data (no loss to follow‐up) |
| Selective reporting (reporting bias) | Low risk | In the methods section no outcome measures are mentioned that are not analysed in the results section. Furthermore, in the results section no findings are mentioned on measures not mentioned in the methods section. Analyses were done at cluster and individual level, as planned in the methods section. |
van Oostrom 2010.
| Methods | Trial design: randomised controlled trial
Country: the Netherlands
Healthcare setting: occupational healthcare setting
Work setting: employees of 3 Dutch companies; the VU University and the VU University Medical Center in Amsterdam and Corus (a steel company) in Velsen‐Noord
Randomisation procedure: block randomisation (blocks of 4) on patient level Recruitment: all employees sick‐listed for more than 1 week received a letter from their occupational physician together with a screening questionnaire. Employees who returned the screening questionnaire and who met the distress and sick leave criteria were contacted by the researchers to check the inclusion and exclusion criteria. Inclusion period: April 2006 to May 2008 Follow‐up: 12 months |
|
| Participants | Number: trial intervention: n = 73; comparison intervention: n = 72 Lost to follow‐up: none for the primary outcome measure; 2 for the secondary outcome measure Age, mean (SD): trial intervention: 48.6 (7.7) years; comparison intervention: 49.2 (8.6) years Sex: trial intervention: 76.7% male; comparison intervention: 80.6% male Duration of sick leave at baseline, sick leave days in past year: trial intervention: 42.5% less than 10 days, 31.5% 11 to 30 days, 26% more than 31 days; comparison intervention: 51.4% less than 10 days, 29.2% 11 to 30 days, 19.4% more than 31 days Inclusion: employees on sick leave from regular work for 2 to 8 weeks and meeting the distress criterion of the screening questionnaire were included Exclusion: a conflict between the employee and the employer with legal involvement; working less than 12 hours a week; pregnancy; any other episode of sick leave within 1 month before the current episode; inability to complete questionnaires written in the Dutch language; severe psychiatric disorders (mania, psychosis or severe risk of suicide); employees with a terminal illness |
|
| Interventions | Trial intervention:
Treatment type: usual care from the occupational physicians (according to the evidence‐based guideline of the Dutch Association of Occupational Physicians published in 2000 and updated in 2007) and a participatory workplace intervention consisting of a stepwise communication process between the sick‐listed employee and the supervisor to identify and solve obstacles for RTW Treatment providers: 9 return to work (RTW) co‐ordinators (for the participatory workplace intervention) and 14 occupational physicians (for care as usual) Training of treatment providers: RTW co‐ordinators had been trained in the guidance of employees and supervisors according to the workplace intervention Treatment frequency and duration: for the workplace intervention 2 meetings on 1 day and a follow‐up meeting after 1 month, additional meetings were possible, the duration of the meetings is unknown; for care as usual 100% consulted their occupational physician in the first 3 months after randomisation, 21 employees (29%) consulted a company social worker (apart from the consultations with a company social worker in the workplace intervention), 36 (49%) were treated by a specialised mental health professional (psychologist, psychiatrist, psychotherapist), 63 (86%) consulted their general practitioner, 23 (32%) consulted a physiotherapist, and 24 (33%) consulted a medical specialist Comparison intervention: Treatment type: usual care from their occupational physicians (according to the evidence‐based guideline of the Dutch Association of Occupational Physicians published in 2000 and updated in 2007) Treatment providers: 14 occupational physicians Training of treatment providers: not reported Treatment frequency and duration: 70 employees (97%) consulted their occupational physician in the first 3 months after randomisation, 24 (33%) consulted a company social worker, 25 (35%) were treated by a specialised mental health professional, 67 (93%) consulted their GP, 28 (39%) consulted a physiotherapist and 30 (42%) consulted a medical specialist |
|
| Outcomes | Work outcomes:
Lasting RTW, defined as the duration of sick leave with distress in calendar days from the day of randomisation until full RTW to the employee’s previous or another position with equal earnings, for at least 4 weeks without (partial or full) recurrence Total number of days of sick leave in 12 months, sick leave data were gathered from the continuous registration systems of the occupational health services Other outcomes: Stress‐related symptoms: Four‐Dimensional Symptom Questionnaire (4DSQ). Measured at baseline and at 3, 6 and 12 months follow‐up. |
|
| Notes | Source of funding: the Dutch Ministry of Social Affairs and Employment and the participating occupational health services
Ethics: the Medical Ethics Committee of VU University Medical Center approved the study design Missing data asked from author: (1) the mean and standard deviation (SD) for days until full RTW for each study group (2) baseline differences between study groups on age, sex and days of sick leave (3) differences in co‐interventions between study groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | van Oostrom 2010, page 597: “An independent statistician prepared the randomisation scheme by using computer‐generated randomisation. To prevent unequal randomisation, employees were pre‐stratified by organisation (VU, VU Medical Center or Corus) and whether they were on full or part time sick leave, resulting in six strata. Block randomisation (with blocks of four) was applied to ensure equal group sizes within each stratum.” |
| Allocation concealment (selection bias) | Low risk | van Oostrom 2010, page 597: “Based on the randomisation scheme, sealed envelopes were prepared before the start of the study containing a referral either to the workplace intervention group or to the usual care group. After completing the baseline questionnaire each employee opened a sealed envelope provided by the research assistant.” |
| Blinding of participants | High risk | van Oostrom 2010: page 597: “The participants and occupational health professionals were not blinded for group assignment.” |
| Blinding of care provider | High risk | van Oostrom 2010: page 597: “The participants and occupational health professionals were not blinded for group assignment.” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | van Oostrom 2008, page 5: "The registration of sick leave in the Netherlands is done by companies and managed by the occupational health services. Since these measurements are extracted from computerized databases, bias caused by a lack of blinding is prevented for this outcome. ... After randomisation all participants receive a research code consisting of a consecutive number. A research assistant will put all data in the computer by the research code. Therefore, the analysis of the data by the researcher will be blind." |
| Co‐interventions avoided or similar | High risk | van Oostrom 2010, page 599: “All employees in the workplace intervention group consulted their occupational physician in the first 3 months after randomisation, 21 employees (29%) consulted a company social worker (apart from the consultations with a company social worker in the workplace intervention), 36 (49%) were treated by a specialised mental health professional (psychologist, psychiatrist, psychotherapist), 63 (86%) consulted their GP [general practitioner], 23 (32%) consulted a physiotherapist, and 24 (33%) consulted a medical specialist.” “In the usual care group, 70 employees (97%) consulted their occupational physician in the first 3 months after randomisation, 24 (33%) consulted a company social worker, 25 (35%) were treated by a specialised mental health professional, 67 (93%) consulted their GP, 28 (39%) consulted a physiotherapist, and 30 (42%) consulted a medical specialist.” There was a difference between the study groups in the use of specialised mental health professionals, like psychologists, psychiatrists and psychotherapists (based on unpublished information from the author) |
| Treatment fidelity | High risk | van Oostrom, page 599: “In total, 20 employees allocated to the workplace intervention did not receive the allocated intervention.” 20 of 56 participants is 36% that did not receive the intervention as planned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up for the primary outcome data. Only 2 participants were lost to follow‐up for questionnaire data. It is unlikely that this will have biased the results. |
| Selective reporting (reporting bias) | High risk | In van Oostrom 2008 (the study protocol), secondary outcome measures have been described that have not been included in van Oostrom 2010 (the study results). These outcomes are: coping, job content and attitude, social influence and self efficacy (ASE). Furthermore, information on recurrences is given, which was not planned according to the methods section. |
Willert 2011.
| Methods | Trial design: randomised waiting list control design Country: Denmark Healthcare setting: clinical care in Aarhus, Denmark Work setting: employees in Aarhus, Denmark Randomisation procedure: block randomisation (blocks of 6) on patient level Recruitment: referral to the study was available through local GPs, union social workers and direct inquiry Inclusion period: December 2006 to September 2007 Follow‐up: 48 weeks |
|
| Participants | Number: trial intervention: 51; comparison intervention: 51 Lost to follow‐up: none for the administrative data, 15 for the self reported data (6 trial intervention, 9 comparison intervention) Age, mean (range): trial intervention 44 (28 to 61) years; comparison intervention: 46 (24 to 58) years Sex: trial intervention: 80.4% female; comparison intervention: 84.3% female Duration of sick leave at baseline, % on sick leave at baseline: trial intervention: 47.1% not on sick leave, 56.9% on part‐/full‐time sick leave, 2% other status; comparison intervention: 37.3% not on sick leave, 62.7% on part‐/full‐time sick leave, 0% other status Inclusion: persistent symptoms of work‐related stress, defined by physiological and psychological symptoms of sustained animation, lasting > 4 weeks and elevated reactivity of symptoms to demands at work; motivation to remain employed and, if on sick leave, a planned RTW ≤ 4 weeks. Participants were either on sick leave following an assessment by their general practitioner (GP) or working. For the latter, a score of ≥ 20 points on the Perceived Stress Scale (PSS) was required. Exclusion: > 26 consecutive weeks of sick leave (to select individuals recently active at their workplace and deselect those at risk of falling under social service regulations); substantial psychosocial strains outside of work; bullying as the main problem; severe psychiatric condition or a history of repeated psychiatric conditions; and current abuse of alcohol or psychoactive stimulants |
|
| Interventions | Trial intervention: Treatment type: a group cognitive behavioural stress management intervention; goal of the intervention was to enable the participants to cope with stressful situations at their workplace and strengthen their ability to be active at work, despite their current difficulties Treatment providers: 2 licensed clinical psychologists with > 5 years of clinical experience Training of treatment providers: a 1‐year advanced training course in cognitive behavioural therapy Treatment frequency/duration: 8 x 3‐hour sessions over a period of 3 months Comparison intervention: Treatment type: waiting list control (WLC) group; after 3 months on the waiting list, the WLC group also received the intervention; participants were not hindered in seeking supplementary help while on the waiting list Treatment providers: not reported Training of treatment providers: not reported Treatment frequency/duration: not reported |
|
| Outcomes | Work outcomes: Self reported sick leave days in the past 3 months. Measured at 16, 32 and 48 weeks. Weeks registered with part‐ or full‐time sick leave in DREAM database (registration of public transfer payment; start of registration after 2 consecutive weeks of part‐ or full‐time sick leave; termination of registration occurs following the first full week of not receiving any type of transfer payment). Measured at 16, 32 and 48 weeks. Other outcomes: none |
|
| Notes | Source of funding: not reported Ethics: not reported Missing data asked from author: (1) why some of the 95% CI reported in the results tables were not symmetrical (2) blinding of participants, care providers and outcome assessors (3) treatment compliance in all study groups (4) reasons for drop‐out in all study groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Willert 2011, page 188: “The study used block randomization in blocks of six, generated using the RANNOR computer algorithm.” |
| Allocation concealment (selection bias) | Low risk | Willert 2011, page 188: “After the baseline measurement, an independent individual open the envelopes containing the participants’ allocation.” |
| Blinding of participants | High risk | Participants were not blinded. They received information about their treatment allocation after the baseline measurement (based on unpublished information from the author). |
| Blinding of care provider | Low risk | The care providers led the groups without knowledge of the participants' randomisation. The first 2 groups consisted of those randomised to the intervention arm of the trial. Groups 3 to 10 consisted of participants mixed from the intervention and waiting list control (WLC) arms. Group 11 and 12 consisted of participants randomised to the waiting list control arm (based on unpublished information from the author). |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The data were collected by an administration officer at the Danish Labour Market authority. Data for both the primary and secondary psychological outcome measures were analysed blindly, by letting an external consultant recode the grouping variable. However, when analysing the data on absenteeism, the principal investigator was so well acquainted with the data that this blinding procedure was no longer effective (based on unpublished data of the author). |
| Co‐interventions avoided or similar | High risk | Willert 2011, page 190: “A total of 14 participants in the WLC group consulted a psychologist outside of the study, with a mean number of 5.4 visits. However, surprisingly, 13 participants from the intervention group also consulted a psychologist outside of the study but while still in group, with a mean of 3.1 visits.” |
| Treatment fidelity | Low risk | Delivery of the intervention was assisted by a Powerpoint slide show. Additional analyses showed that participation in different groups and with different group leaders did not effect the study's outcome (based on unpublished information from the author). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Willert 2011, page 190: “Dropout analyses were performed and revealed no systematic differences between those dropping out of the study and those remaining in terms of gender, age, sick leave status or PSS [Perceived Stress Scale] score at inclusion. Also, no systematic differences were found between those dropping out of the intervention and WLC groups, respectively.” However, the flow diagram in Willert 2010 shows that there were more participants in the waiting list control group that dropped out because of lack of motivation to participate For the outcome absenteeism at 4 months follow‐up, N = 6 (12%) and N = 9 (18%) were lost to follow‐up in the intervention and control group, respectively (total loss to follow‐up 15%) |
| Selective reporting (reporting bias) | High risk | In Willert 2011, on page 190 and 191, supplementary analyses are presented that were not described in the methods section |
CAU: care as usual CBR: Cognitively oriented Behavioural Rehabilitation CBT: cognitive behavioural therapy CI: confidence interval GP: general practitioner OP: occupational physician PCP: Primary Care Physician RTW: return to work SD: standard deviation SMT: stress management training WLC: waiting list control
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Allgulander 2007 | Participants did not have an adjustment disorder according to our definition |
| Bee 2010 | Participants did not have an adjustment disorder according to our definition |
| Boyer 1998 | Participants did not have an adjustment disorder according to our definition |
| Braathen 2007 | The study design was non‐randomised |
| Brattberg 2006 | More than 30% of the participants were diagnosed with physical disorders |
| Brattberg 2007 | More than 30% of the participants were diagnosed with physical disorders |
| Cabrera 2009 | Participants did not have an adjustment disorder according to our definition |
| Dahl 2004 | The study population was not on sick leave |
| De Zeeuw 2010 | The study population was not on sick leave |
| DellaPosta 2006 | The study population was not on sick leave |
| Dewa 2009 | The study design was non‐randomised |
| Duijts 2008 | The study population was not on sick leave |
| Fantino 2007 | Participants did not have an adjustment disorder according to our definition |
| Feltz‐Cornelis 2010 | Participants did not have an adjustment disorder according to our definition |
| Fernandez 2005 | Participants did not have an adjustment disorder according to our definition |
| Fleten 2006 | More than 30% of the participants were diagnosed with physical disorders |
| Grime 2004 | Sick leave was not measured |
| Hees 2010 | The study population was not on sick leave |
| Heiden 2007 | Participants did not have an adjustment disorder according to our definition |
| Herz 1971 | Participants did not have an adjustment disorder according to our definition |
| Huibers 2004 | Participants did not have an adjustment disorder according to our definition |
| Knekt 2008 | Participants did not have an adjustment disorder according to our definition |
| Kobayashi 2008 | The study design was non‐randomised |
| Lander 2009 | The study design was non‐randomised |
| Lo Sasso 2006 | Participants did not have an adjustment disorder according to our definition |
| Malkinson 1997 | The study population was not on sick leave |
| Martin 2009 | The study population was not on sick leave |
| Meesters 2010 | Sick leave was not measured |
| Mynors‐Wallis 1997 | The study population was not on sick leave |
| Nord 2006 | Participants did not have an adjustment disorder according to our definition |
| Nystuen 2003 | More than 30% of the participants were diagnosed with physical disorders |
| Nystuen 2006 | More than 30% of the participants were diagnosed with physical disorders |
| Peterson 2008 | Sick leave was not measured |
| Rahe 2002 | Participants did not have an adjustment disorder according to our definition |
| Roessler 1977 | Sick leave was not measured |
| Rollman 2005 | Participants did not have an adjustment disorder according to our definition |
| Rost 2010 | Participants did not have an adjustment disorder according to our definition |
| Saksvik 2001 | The study design was non‐randomised |
| Schene 2007 | Participants did not have an adjustment disorder according to our definition |
| Schilte 2001 | The study population was not on sick leave |
| Schuring 2009 | Participants did not have an adjustment disorder according to our definition |
| Sogaard 2009 | More than 30% of the participants is diagnosed with other psychiatric disorders than adjustment disorders |
| Sogaard 2010 | Sick leave was not measured |
| Thorslund 2007 | More than 30% of the participants were diagnosed with other psychiatric disorders than adjustment disorders or with physical disorders |
| van Rhenen 2007 | The study population was not on sick leave |
| Vlasveld 2008 | Participants did not have an adjustment disorder according to our definition |
| Wade 2008 | Participants did not have an adjustment disorder according to our definition |
| Wallace 2004 | Participants did not have an adjustment disorder according to our definition |
| Wang 2007 | The study population was not on sick leave |
| Yates 2004 | Participants did not have an adjustment disorder according to our definition |
Characteristics of ongoing studies [ordered by study ID]
Arends 2010.
| Trial name or title | Prevention of recurrent sickness absence among employees with common mental disorders; design of a cluster‐randomised controlled trial with cost‐benefit and effectiveness evaluation |
| Methods | Cluster RCT |
| Participants | Workers with common mental disorders |
| Interventions | Active guidance of employees by occupational physicians during the first weeks of work after sick leave |
| Outcomes | Cumulative recurrent sick leave days, mental health, work functioning and coping |
| Starting date | December 2009 |
| Contact information | I. Arends, University Medical Center Groningen, Groningen, the Netherlands |
| Notes |
Brouwers 2011.
| Trial name or title | Effectiveness of the guideline management of workers with common mental health problems by occupational physicians: a randomised controlled trial |
| Methods | RCT |
| Participants | Workers on sick leave with common mental disorders |
| Interventions | The Dutch guideline 'management of workers with common mental health problems by occupational physicians' |
| Outcomes | Time to full RTW, partial RTW, total days of sick leave, patient satisfaction, symptoms |
| Starting date | October 2010 |
| Contact information | E. Brouwers, Tilburg University Department Tranzo, Tilburg, the Netherlands |
| Notes |
Netterstrøm 2011.
| Trial name or title | A randomised controlled trial of a immediate versus delayed stress management program versus traditional psychological therapy in adults suffering from work‐related stress symptoms |
| Methods | RCT |
| Participants | Adults with a moderate to high stress symptom score |
| Interventions | A stress‐management programme |
| Outcomes | RTW rate, Symptom Checklist 92, World Health Organization Major Depression Inventory, absenteeism, Copenhagen Psychosocial Questionnaire (COPSOQ), salivary cortisol, high density lipoprotein cholesterol, total cholesterol, blood pressure, C‐reactive protein and interleukin‐6 (immunological status), HbA1C and dehydroepiandrosterone sulfate (metabolic condition), heart rate variability |
| Starting date | May 2010 |
| Contact information | B. Netterstrøm, Department of Occupational and Environmental Medicine Bispebjerg University Hospital, Copenhagen, Denmark |
| Notes |
Noordik 2009.
| Trial name or title | Effectiveness and cost‐effectiveness of an exposure‐based return‐to‐work programme for patients on sickness absence due to common mental disorders: design of a cluster‐randomized controlled trial |
| Methods | Cluster RCT |
| Participants | Patients absent from work due to common mental disorders |
| Interventions | A work‐directed intervention programme based on the principles of exposure in vivo |
| Outcomes | Time until full RTW, duration of sick leave, time until partial RTW, rate of partial and full RTW, distress, anxiety, depression, somatisation, fatigue, work capacity, working conditions, self efficacy for RTW, coping behaviour, avoidance behaviour related to work, patient satisfaction, work adaptations |
| Starting date | May 2006 |
| Contact information | E. Noordik, Coronel Institute of Occupational Health, Academic Medical Center, Amsterdam, the Netherlands |
| Notes |
RCT: randomised controlled trial RTW: return to work
Differences between protocol and review
Authors: Iris Arends, Ute Bültmann and Jos Verbeek were added as review authors.
Title: The title has been changed from 'Return to work interventions for adjustment disorders' to 'Interventions to facilitate return to work in adults with adjustment disorders' as this better represents the topic of the review.
Types of studies: A more clear definition is given of the focus of the types of studies included in the review.
Types of participants: The word 'adults' is replaced by 'workers', because the review is not focused on all adults but only on working adults. Also, we have further operationalised the definition of 'adjustment disorder' because the definition of the protocol was insufficient to decide if studies were on workers with adjustment disorders and could be included on this point. The sentence in the protocol on including "patients in all organisational settings..." has been deleted because we felt this information was superfluous. Furthermore, we have added that studies could be included when not all participants were on sick leave at baseline (i.e. some were still at work), as long as the outcome data on sick leave/RTW were separately reported for the group that was on sick leave at baseline.
Types of interventions: The interventions (and the comparisons) are more thoroughly explained. Furthermore we added a mixed group of interventions, consisting of combined interventions, because otherwise we were not able to categorise an intervention that used a mixture of two or more interventions. We deleted the sentence on separately managing interventions aimed at the workplace, because we chose to categorise interventions based on their core elements instead of looking at the setting where they were implemented.
Types of outcomes: For the primary outcomes, we have chosen to minimise the number of outcomes presented in the protocol as per the advice in the Cochrane Handbook. We focused on time lost from work as the primary outcome and defined this more clearly as partial and full RTW, which is a frequently used outcome measure in the research literature for workers on sick leave. The other primary outcomes mentioned in the protocol have been grouped in the review as secondary outcome measures defined as work functioning. Two secondary outcome measures have been deleted. These were 'patient compliance to the intervention' and 'trial drop‐out', because these variables were already taken into account in the 'Risk of bias' analyses.
Search methods: Based on discussions with the Trial Search Co‐ordinator of the CCDAN Group, it was decided to search the CCDAN registers, CENTRAL, EMBASE, MEDLINE, PsycINFO, Web of Science, the WHO trials portal and ClinicalTrials.gov. The Trial Search Co‐ordinator helped with finding the right terms for adjustment disorders and randomised clinical trials. We decided not to use search terms for the interventions because we wanted to find all types of interventions and the naming of interventions varies widely. Instead, we used terms to identify studies on RTW or on workers on sick leave. We refrained from writing to all authors of articles because we felt that there was enough expertise in the review team, and this would unnecessarily burden the authors. We also refrained from searching congress abstracts as there was not just one forum of discussion, but proceedings of many different conferences should have been searched. This went beyond our resources.
Selection of studies: To enhance a structured first selection of studies based on title and abstract screening, we developed a standardised form with the following criteria: (1) study design is a RCT, (2) study population consists of a working population and (3) study population has common mental disorders (adjustment disorders, depressive disorders, anxiety disorders).
Assessment of risk of bias: In the protocol, a quality assessment with the Downs and Black list was planned. However, we decided to analyse the risk of bias in accordance with the recommendations made in the Cochrane Handbook.
Data extraction: No differences.
Data analysis: We changed the reporting of dichotomous outcome measures from odds ratios to risk ratios because the event of returning to work is quite common which inflates the odds ratio. Moreover, risk ratios are easier to interpret.
Contributions of authors
DB wrote the protocol and IA wrote the systematic review. IA, DB, UB and KN included eligible studies, and JV helped when authors could not agree. IA and UB did the 'Risk of bias' assessment and DB helped when these authors could not agree. DB, IA and AN conducted the data extraction from the original studies. IA contacted study authors for additional information. IA and JV conducted the data synthesis. DR, AN, IM and KN reviewed the protocol. AN, DB, DR, IM, KN, UB and JV reviewed the systematic review. All authors were involved in designing the search strategy and choosing the comparison groups for the data analyses.
Sources of support
Internal sources
EMGO Institute, Department of Public and Occupational Health, VU University Medical Center, Netherlands.
Community & Occupational Medicine, Department of Health Sciences, University Medical Center Groningen, University of Groningen, Groningen, Netherlands.
-
Ministry of Social Affairs and Employment, Netherlands.
David Bruinvels received a grant as part of the Occupational Health Knowledge Infrastructure Programme of the Ministry
External sources
Dutch Cochrane Centre, Netherlands.
Declarations of interest
DR and DB are authors of one of the included studies, but they were not involved in the selection, 'Risk of bias' analysis or data extraction for this study.
IA and UB are the authors of a potentially eligible study for this review. They will not be involved in the selection, 'Risk of bias' analysis or data extraction for this study.
KN is the author of a potentially eligible study for this review. She will not be involved in the selection, 'Risk of bias' analysis or data extraction for this study.
IA, DB, DR, KN, IM, AN, UB and JV declare no financial conflicts of interest.
New
References
References to studies included in this review
Bakker 2007 {published data only}
- Bakker IM, Terluin B, Marwijk HW, Gundy CM, Smit JH, Mechelen W, et al. Effectiveness of a Minimal Intervention for Stress‐related mental disorders with Sick leave (MISS); study protocol of a cluster randomised controlled trial in general practice [ISRCTN43779641]. BMC Public Health 2006;6(124):e‐publication. [DOI: 10.1186/1471-2458-6-124; PUBMED: 16674806] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker IM, Terluin B, Marwijk HW, Windt DA, Rijmen F, Mechelen W, et al. A cluster‐randomised trial evaluating an intervention for patients with stress‐related mental disorders and sick leave in primary care. PLoS Clinical Trials 2007;2(6):e26. [DOI: 10.1371/journal.pctr.0020026; PUBMED: 17549228] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker IM, Marwijk HW, Terluin B, Anema JR, Mechelen W, Stalman WA. Training GP's to use a minimal intervention for stress‐related mental disorders with sick leave (MISS): Effects on performance: Results of the MISS project; a cluster‐randomised controlled trial [ISRCTN43779641]. Patient Education and Counseling 2010;78(2):206‐11. [DOI] [PubMed] [Google Scholar]
- Uegaki K, Bakker I, Bruijne M, Beek A, Terluin B, Marwijk H, et al. Cost‐effectiveness of a minimal intervention for stress‐related sick leave in general practice: results of an economic evaluation alongside a pragmatic randomised control trial. Journal of Affective Disorders 2010;120(1‐3):177‐87. [DOI] [PubMed] [Google Scholar]
Blonk labour expert 2006 {published data only}
- Blonk RWB, Brenninkmeijer V, Lagerveld SE, Houtman ILD. Return to work: a comparison of two cognitive behavioural interventions in cases of work‐related psychological complaints among the self‐employed. Work & Stress 2006;20(2):129‐44. [DOI: 10.1080/02678370600856615] [DOI] [Google Scholar]
Blonk psychologist 2006 {published data only}
- Blonk RWB, Brenninkmeijer V, Lagerveld SE, Houtman ILD. Return to work: a comparison of two cognitive behavioural interventions in cases of work‐related psychological complaints among the self‐employed. Work & Stress 2006;20(2):129‐44. [DOI: 10.1080/02678370600856615] [DOI] [Google Scholar]
Brouwers 2006 {published data only}
- Brouwers EP, Tiemens BG, Terluin B, Verhaak PF. Effectiveness of an intervention to reduce sickness absence in patients with emotional distress or minor mental disorders: a randomized controlled effectiveness trial. General Hospital Psychiatry 2006;28(3):223‐9. [DOI: 10.1093/eurpub/ckl099; PUBMED: 16675365] [DOI] [PubMed] [Google Scholar]
- Brouwers EP, Bruijne MC, Terluin B, Tiemens BG, Verhaak PF. Cost‐effectiveness of an activating intervention by social workers for patients with minor mental disorders on sick leave: a randomized controlled trial. European Journal of Public Health 2006;17(2):214‐20. [DOI: ; PUBMED: 16837516] [DOI] [PubMed] [Google Scholar]
- Brouwers EPM, Tiemens BG, Terluin B, Verhaak PFM. Effectiveness of an intervention to reduce sickness absenteeism from work in patients with emotional distress or minor mental disorders: a randomised controlled effectiveness trial [De effectiviteit van een interventie door het maatschappelijk werk bij huisartspatiënten die overspannen zijn. Een gerandomiseerd vergelijkend onderzoek]. Huisarts & Wetenschap 2007;50(6):238‐44. [Google Scholar]
de Vente group 2008 {published data only}
- Vente W, Kamphuis JH, Emmelkamp PM, Blonk RW. Individual and group cognitive‐behavioral treatment for work‐related stress complaints and sickness absence: a randomized controlled trial. Journal of Occupational Health Psychology 200;13(3):214‐31. [DOI] [PubMed] [Google Scholar]
de Vente individual 2008 {published data only}
- Vente W, Kamphuis JH, Emmelkamp PM, Blonk RW. Individual and group cognitive‐behavioral treatment for work‐related stress complaints and sickness absence: a randomized controlled trial. Journal of Occupational Health Psychology 2008;13(3):214‐31. [DOI: 10.1037/1076-8998.13.3.214; PUBMED: 18572993] [DOI] [PubMed] [Google Scholar]
Rebergen 2009 {published data only}
- Rebergen DS, Bruinvels DJ, Bezemer PD, Beek AJ, Mechelen W. Guideline‐Based Care of Common Mental Disorders by Occupational Physicians (CO‐OP study): a randomized controlled trial. Journal of Occupational and Environmental Medicine 2009;51(3):305‐12. [DOI] [PubMed] [Google Scholar]
- Rebergen DS, Bruinvels DJ, Bos CM, Beek AJ, Mechelen W. Return to work and occupational physicians’ management of common mental health problems – process evaluation of a randomized controlled trial. Scandinavian Journal of Work, Environment and Health 2010;36(6):488‐98. [DOI] [PubMed] [Google Scholar]
- Rebergen DS, Bruinvels DJ, Tulder MW, Beek AJ, Mechelen W. Cost‐ effectiveness of guideline‐based care for workers with mental health problems. Journal of Occupational and Environmental Medicine 2009;51(3):313‐22. [DOI] [PubMed] [Google Scholar]
- Rebergen DS, Bruinvels DJ, Beek AJ, Mechelen W. Design of a randomized controlled trial on the effects of Counseling of mental health problems by Occupational Physicians on return to work: the CO‐OP‐study. BMC Public Health 2007;7:183. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stenlund 2009 {published data only}
- Stenlund T, Ahlgren C, Lindahl B, Burell G, Steinholtz K, Edlund C, et al. Cognitively oriented behavioral rehabilitation in combination with Qigong for patients on long‐term sick leave because of burnout: REST‐‐a randomized clinical trial. International Journal of Behavioral Medicine 2009;16(3):294‐303. [DOI] [PubMed] [Google Scholar]
van der Klink 2003 {published data only}
- Klink JJL, Blonk RWB, Schene AH, Dijk FJH. Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Occupational and Environmental Medicine 2003;60(6):429‐37. [DOI: 10.1136/oem.60.6.429; PUBMED: 12771395] [DOI] [PMC free article] [PubMed] [Google Scholar]
van Oostrom 2010 {published data only}
- Oostrom S H, Heymans M W, Vet H C W, Tulder M W, Mechelen W, Anema J R. Economic evaluation of a workplace intervention for sick‐listed employees with distress. Occupational and environmental medicine 2010;67(9):603‐10. [DOI] [PubMed] [Google Scholar]
- Oostrom S H, Mechelen W, Terluin B, Vet H C W, Knol D L, Anema J R. A workplace intervention for sick‐listed employees with distress: Results of a randomised controlled trial. Occupational and environmental medicine 2010;67(9):596‐602. [DOI] [PubMed] [Google Scholar]
- Oostrom SH, Anema JR, Terluin B, Vet HCW, Knol DL, Mechelen W. Cost‐effectiveness of a workplace intervention for sick‐listed employees with common mental disorders: design of a randomized controlled trial. BMC Public Health 2008;8:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oostrom SH, Mechelen W, Terluin B, Vet HC, Anema JR. A participatory workplace intervention for employees with distress and lost time: a feasibility evaluation within a randomized controlled trial. Journal of Occupational Rehabilitation 2009;19(2):212‐22. [DOI] [PubMed] [Google Scholar]
Willert 2011 {published data only}
- Willert MV, Thulstrup AM, Bonde JP. Effects of a stress management intervention on absenteeism and return to work‐‐results from a randomized wait‐list controlled trial. Scandinavian Journal of Work, Environment & Health 2011;37(3):186‐95. [DOI] [PubMed] [Google Scholar]
- Willert MV, Thulstrup AM, Hertz J, Bonde JP. Sleep and cognitive failures improved by a three‐month stress management intervention. International Journal of Stress Management 2010;17(3):193‐213. [Google Scholar]
References to studies excluded from this review
Allgulander 2007 {published data only}
- Allgulander C, Jorgensen T, Wade A, Francois C, Despiegel N, Auquier P, et al. Health‐related quality of life (HRQOL) among patients with generalised anxiety disorder: evaluation conducted alongside an escitalopram relapse prevention trial. Current Medical Research and Opinion 2007;23(10):2543‐9. [DOI] [PubMed] [Google Scholar]
Bee 2010 {published data only}
- Bee PE, Bower P, Gilbody S, Lovell K. Improving health and productivity of depressed workers: a pilot randomized controlled trial of telephone cognitive behavioral therapy delivery in workplace settings. General Hospital Psychiatry 2010;32(3):337‐40. [DOI] [PubMed] [Google Scholar]
Boyer 1998 {published data only}
- Boyer P, Danion JM, Bisserbe JC, Hotton JM, Troy S. Clinical and economic comparison of sertraline and fluoxetine in the treatment of depression. A 6‐month double‐blind study in a primary‐care setting in France. PharmacoEconomics 1998;13(1):157‐69. [DOI] [PubMed] [Google Scholar]
Braathen 2007 {published data only}
- Braathen TNl, Veiersted KB, Heggenes J. Improved work ability and return to work following vocational multidisciplinary rehabilitation of subjects on long‐term sick leave. Journal of Rehabilitation Medicine 2007;39(6):493‐9. [DOI] [PubMed] [Google Scholar]
Brattberg 2006 {published data only}
- Brattberg G. Internet‐based rehabilitation for individuals with chronic pain and burnout: a randomized trial. International Journal of Rehabilitation Research 2006;29(3):221‐7. [DOI] [PubMed] [Google Scholar]
Brattberg 2007 {published data only}
- Brattberg G. Internet‐based rehabilitation for individuals with chronic pain and burnout II: a long‐term follow‐up. International Journal of Rehabilitation Research 2007;30:231‐4. [DOI] [PubMed] [Google Scholar]
Cabrera 2009 {published data only}
- Cabrera Pivaral CE, Ruiz Cruz LK, Gonzalez Perez GJ, Vega Lopez MG, Valadez Figueroa I. Effect of a psycho‐educative intervention to decrease burnout syndrome on confidence employees working for the CFE (Federal Electric Commission). Salud Mental 2009;32(3):215‐21. [Google Scholar]
Dahl 2004 {published data only}
- Dahl J, Wilson KG, Nilsson A. Acceptance and commitment therapy and the treatment of persons at risk for long‐term disability resulting from stress and pain symptoms: a preliminary randomized trial. Behavior Therapy 2004;35(4):785‐801. [Google Scholar]
DellaPosta 2006 {published data only}
- DellaPosta C, Drummond PD. Cognitive behavioural therapy increases re‐employment of job seeking worker's compensation clients. Journal of Occupational Rehabilitation 2006;16(2):223‐30. [DOI] [PubMed] [Google Scholar]
Dewa 2009 {published data only}
- Dewa CS, Hoch JS, Carmen G, Guscott R, Anderson C. Cost, effectiveness, and cost‐effectiveness of a collaborative mental health care program for people receiving short‐term disability benefits for psychiatric disorders. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie 2009;54(6):379‐88. [DOI] [PubMed] [Google Scholar]
De Zeeuw 2010 {published data only}
- Zeeuw ELEJ, Tak ECPM, Dusseldorp E, Hendriksen IJM. Workplace exercise intervention to prevent depression: a pilot randomized controlled trial. Mental Health and Physical Activity 2010;3(2):72‐7. [Google Scholar]
Duijts 2008 {published data only}
- Duijts SF, Kant I, Brandt PA, Swaen GM. Effectiveness of a preventive coaching intervention for employees at risk for sickness absence due to psychosocial health complaints: results of a randomized controlled trial. Journal of Occupational and Environmental Medicine 2008;50(7):765‐76. [DOI] [PubMed] [Google Scholar]
Fantino 2007 {published data only}
- Fantino B, Moore N, Verdoux H, Auray J‐P. Cost‐effectiveness of escitalopram vs. citalopram in major depressive disorder. International Clinical Psychopharmacology 2007;22(2):107‐15. [DOI] [PubMed] [Google Scholar]
Feltz‐Cornelis 2010 {published data only}
- Feltz‐Cornelis CM, Hoedeman R, Jong FJ, Meeuwissen JAC, Drewes HW, Laan NC, et al. Faster return to work after psychiatric consultation for sicklisted employees with common mental disorders compared to care as usual. A randomized clinical trial. Neuropsychiatric Disease and Treatment 2010;6:375‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fernandez 2005 {published data only}
- Fernandez JL, Montgomery S, Francois C. Evaluation of the cost effectiveness of escitalopram versus venlafaxine XR in major depressive disorder. PharmacoEconomics 2005;23(2):155‐67. [DOI] [PubMed] [Google Scholar]
Fleten 2006 {published data only}
- Fleten N, Johnsen R. Reducing sick leave by minimal postal intervention: a randomised, controlled intervention study. Occupational and Environmental Medicine 2006;63(10):676‐82. [DOI: 10.1136/oem.2005.020438; PUBMED: 16644897] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grime 2004 {published data only}
- Grime PR. Computerized cognitive behavioural therapy at work: a randomized controlled trial in employees with recent stress‐related absenteeism. Occupational Medicine 2004;54(5):353‐9. [DOI] [PubMed] [Google Scholar]
Hees 2010 {published data only}
- Hees HL, Koeter Maarten WJ, Vries G, Ooteman W, Schene AH. Effectiveness of adjuvant occupational therapy in employees with depression: design of a randomized controlled trial. BMC Public Health 2010;10:558. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heiden 2007 {published data only}
- Heiden M, Lyskov E, Nakata M, Sahlin K, Sahlin T, Barnekow‐Bergkvist M. Evaluation of cognitive behavioural training and physical activity for patients with stress‐related illnesses: a randomized controlled study. Journal of Rehabilitation Medicine 2007;39(5):366‐73. [DOI] [PubMed] [Google Scholar]
Herz 1971 {published data only}
- Herz M I, Endicott J, Spitzer R L, Mesnikoff A. Day versus inpatient hospitalization: a controlled study. American Journal of Psychiatry 1971;127(10):1371‐82. [DOI] [PubMed] [Google Scholar]
Huibers 2004 {published data only}
- Huibers MJ, Beurskens AJ, Schayck CP, Bazelmans E, Metsemakers JF, Knottnerus JA, et al. Efficacy of cognitive‐behavioural therapy by general practitioners for unexplained fatigue among employees: randomised controlled trial. British Journal of Psychiatry 2004;184:240‐60. [DOI] [PubMed] [Google Scholar]
- Huibers MJ, Bleijenberg G, Amelsvoort LG, Beurskens AJ, Schayck CP, Bazelmans E, et al. Predictors of outcome in fatigued employees on sick leave: results from a randomised trial. Journal of Psychosomatic Research 2004;57(5):443‐9. [DOI] [PubMed] [Google Scholar]
Knekt 2008 {published data only}
- Knekt P, Lindfors O, Laaksonen MA, Raitasalo R, Haaramo P, Jarvikoski A. Effectiveness of short‐term and long‐term psychotherapy on work ability and functional capacity ‐ a randomized clinical trial on depressive and anxiety disorders. Journal of Affective Disorders 2008;107(1‐3):95‐106. [DOI] [PubMed] [Google Scholar]
Kobayashi 2008 {published data only}
- Kobayashi Y, Kaneyoshi A, Yokota A, Kawakami N. Effects of a worker participatory program for improving work environments on job stressors and mental health among workers: a controlled trial. Journal of Occupational Health 2008;50(6):455‐70. [DOI] [PubMed] [Google Scholar]
Lander 2009 {published data only}
- Lander F, Friche C, Tornemand H, Andersen J H, Kirkeskov L. Can we enhance the ability to return to work among workers with stress‐related disorders?. BMC Public Health 2009;9:372. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lo Sasso 2006 {published data only}
- Lo Sasso A T, Rost K, Beck A. Modeling the impact of enhanced depression treatment on workplace functioning and costs: a cost‐benefit approach. Medical Care 2006;44(4):352‐8. [DOI] [PubMed] [Google Scholar]
Malkinson 1997 {published data only}
- Malkinson R, Kushnir T, Weisberg E. Stress management and burnout prevention in female blue‐collar workers: theoretical and practical implications. International Journal of Stress Management 1997;4(3):183‐95. [Google Scholar]
Martin 2009 {published data only}
- Martin A, Sanderson K, Scott J, Brough P. Promoting mental health in small‐medium enterprises: an evaluation of the "business in mind" program. BMC Public Health 2009;9:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
Meesters 2010 {published data only}
- Meesters Y, Waslander M. Burnout and light treatment. Stress and Health 2010;26(1):13‐20. [Google Scholar]
Mynors‐Wallis 1997 {published data only}
- Mynors‐Wallis L, Davies I, Gray A, Barbour F, Gath D. A randomised controlled trial and cost analysis of problem‐solving treatment for emotional disorders given by community nurses in primary care. British Journal of Psychiatry 1997;170:113‐9. [PUBMED: 9093498] [DOI] [PubMed] [Google Scholar]
Nord 2006 {published data only}
- Nord E, Dalgard OS. Economic evaluation of a course in coping with depression. Tidsskrift for den Norske laegeforening 2006;126(5):586‐8. [PubMed] [Google Scholar]
Nystuen 2003 {published data only}
- Nystuen P, Hagen KB. Feasibility and effectiveness of offering a solution‐focused follow‐up to employees with psychological problems or muscle skeletal pain: a randomised controlled trial. BMC Public Health 2003;3:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nystuen 2006 {published data only}
- Nystuen P, Hagen KB. Solution‐focused intervention for sick listed employees with psychological problems or muscle skeletal pain: a randomised controlled trial [ISRCTN39140363]. BMC Public Health 2006;6:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peterson 2008 {published data only}
- Peterson U, Bergstrom G, Samuelsson M, Asberg M, Nygren A. Reflecting peer‐support groups in the prevention of stress and burnout: randomized controlled trial. Journal of Advanced Nursing 2008;63(5):506‐16. [DOI] [PubMed] [Google Scholar]
Rahe 2002 {published data only}
- Rahe RH, Taylor CB, Tolles RL, Newhall LM, Veach TL, Bryson S. A novel stress and coping workplace program reduces illness and healthcare utilization. Psychosomatic Medicine 2002;64(2):278‐86. [DOI] [PubMed] [Google Scholar]
Roessler 1977 {published data only}
- Roessler R, Cook D, Lillard D. Effects of systematic group counseling on work adjustment clients. Journal of Counseling Psychology 1977;24(4):313‐7. [Google Scholar]
Rollman 2005 {published data only}
- Rollman BL, Belnap BH, Mazumdar S, Houck PR, Zhu F, Gardner W, et al. A randomized trial to improve the quality of treatment for panic and generalized anxiety disorders in primary care. Archives of General Psychiatry 2005;62(12):1332‐41. [DOI] [PubMed] [Google Scholar]
Rost 2010 {published data only}
- Rost KM, Marshall D. Marketing depression care management to employers: design of a randomized controlled trial. Implementation Science 2010;5:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saksvik 2001 {published data only}
- Saksvik PO, Nytro K. Improving subjective health and reducing absenteeism in a natural work life‐intervention. Scandinavian Journal of Psychology 2001;42(1):17‐24. [DOI] [PubMed] [Google Scholar]
Schene 2007 {published data only}
- Schene AH, Koeter MWJ, Kikkert MJ, Swinkels JA, McCrone P. Adjuvant occupational therapy for work‐related major depression works: randomized trial including economic evaluation. Psychological Medicine 2007;37(3):351‐62. [DOI] [PubMed] [Google Scholar]
Schilte 2001 {published data only}
- Schilte AF, Portegijs PJ, Blankenstein AH, Horst HE, Latour MB, Eijk JT, et al. Randomised controlled trial of disclosure of emotionally important events in somatisation in primary care. BMJ 2001;323(7304):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schuring 2009 {published data only}
- Schuring M, Burdorf A, Voorham AJ, Weduwe K, Mackenbach JP. Effectiveness of a health promotion programme for long‐term unemployed subjects with health problems: a randomised controlled trial. Journal of Epidemiology and Community Health 2009;63(11):893‐9. [DOI] [PubMed] [Google Scholar]
Sogaard 2009 {published data only}
- Sogaard HJ, Bech P. The effect on length of sickness absence by recognition of undetected psychiatric disorder in long‐term sickness absence. A randomized controlled trial. Scandinavian Journal of Public Health 2009;37(8):864‐71. [DOI] [PubMed] [Google Scholar]
Sogaard 2010 {published data only}
- Sogaard HJ, Bech P. The effect of detecting undetected common mental disorders on psychological distress and quality of life in long‐term sickness absence: a randomised controlled trial. Scandinavian Journal of Public Health 2010;38(8):845‐56. [DOI] [PubMed] [Google Scholar]
Thorslund 2007 {published data only}
- Thorslund KW. Solution‐ focused group therapy for patients on long‐term sick leave: a comparative outcome study. Journal of Family Psychotherapy 2007;18(3):11‐24. [Google Scholar]
van Rhenen 2007 {published data only}
- Rhenen W, Blonk RWB, Schaufeli WB, Dijk FJH. Can sickness absence be reduced by stress reduction programs: on the effectiveness of two approaches. International Archives of Occupational and Environmental Health 2007;80(6):505‐15. [DOI] [PubMed] [Google Scholar]
Vlasveld 2008 {published data only}
- Vlasveld MC, Anema JR, Beekman ATF, Mechelen W, Hoedeman R, Marwijk HW, et al. Multidisciplinary collaborative care for depressive disorder in the occupational health setting: design of a randomised controlled trial and cost‐effectiveness study. BMC Health Services Research 2008;8:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wade 2008 {published data only}
- Wade AG, Fernandez J‐L, Francois C, Hansen K, Danchenko N, Despiegel N. Escitalopram and duloxetine in major depressive disorder: a pharmacoeconomic comparison using UK cost data. PharmacoEconomics 2008;26(11):969‐81. [DOI] [PubMed] [Google Scholar]
Wallace 2004 {published data only}
- Wallace CJ, Tauber R, Kopelowicz A, Liberman RP. Supplementing supported employment with workplace skills training. Psychiatric Services 2004;55(5):513‐5. [DOI] [PubMed] [Google Scholar]
Wang 2007 {published data only}
- Wang PS, Simon GE, Avorn J, Azocar F, Ludman EJ, McCulloch J, et al. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA 2007;298(12):1401‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yates 2004 {published data only}
- Yates WR, Mitchell J, Rush AJ, Trivedi MH, Wisniewski SR, Warden D, et al. Clinical features of depressed outpatients with and without co‐occurring general medical conditions in STAR*D. General Hospital Psychiatry 2004;26(6):421‐9. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Arends 2010 {published data only}
- Arends I, Klink JJL, Bultman U. Prevention of recurrent sickness absence among employees with common mental disorders; design of a cluster‐randomised controlled trial with cost‐benefit and effectiveness evaluation. BMC Public Health 2010;10:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brouwers 2011 {published data only}
- Effectiveness of the guideline management of workers with common mental health problems by occupational physicians: a randomised controlled trial. http://apps.who.int/trialsearch/ Ongoing study October 2010.
Netterstrøm 2011 {published data only}
- A randomised controlled trial of a immediate versus delayed stress management program versus traditional psychological therapy in adults suffering from work‐related stress symptoms. http://apps.who.int/trialsearch/ Ongoing study May 2010.
Noordik 2009 {published data only}
- Noordik E, Dijk FJ, Nieuwenhuijsen K, Klink JJL. Effectiveness and cost‐effectiveness of an exposure‐based return‐to‐work programme for patients on sick leave due to common mental disorders: design of a cluster‐randomized controlled trial. BMC Public Health 2009;9:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
APA 1994
- APA. Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV). Washington DC: American Psychiatric Association, 1994. [Google Scholar]
Bakker 2010
- Bakker IM, Marwijk HW, Terluin B, Anema JR, Mechelen W, Stalman WA. Training GP's to use a minimal intervention for stress‐related mental disorders with sick leave (MISS): Effects on performance: Results of the MISS project; a cluster‐randomised controlled trial [ISRCTN43779641]. Patient Education and Counseling 2010;78(2):206‐11. [DOI] [PubMed] [Google Scholar]
Beck 1979
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York: Guilford Press, 1979. [Google Scholar]
Blank 2008
- Blank L, Peters J, Pickvance S, Wilford J, Macdonald E. A systematic review of the factors which predict return to work for people suffering episodes of poor mental health. Journal of Occupational Rehabilitation 2008;18(1):27‐34. [DOI] [PubMed] [Google Scholar]
Braam 2009
- Braam C, Oostrom SH, Terluin B, Vasse R, Vet HCW, Anema JR. Validation study of a distress screener. Journal of Occupational Rehabilitation 2009;19(3):231‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brouwers 2009
- Brouwers EP, Terluin B, Tiemens BG, Verhaak PF. Predicting return to work in employees sick‐listed due to minor mental disorders. Journal of Occupational Rehabilitation 2009;19(4):323‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bültmann 2005
- Bültmann U, Huibers MJ, Amelsvoort LP, Kant I, Kasl SV, Swaen GM. Psychological distress, fatigue and long‐term sickness absence: prospective results from the Maastricht Cohort Study. Journal of Occupational and Environmental Medicine 2005;47(9):941‐7. [DOI] [PubMed] [Google Scholar]
Carder 2009
- Carder M, Turner S, McNamee R, Agius R. Work‐related mental ill‐health and 'stress' in the UK (2002‐05). Occupational Medicine 2009;59(8):539‐44. [DOI] [PubMed] [Google Scholar]
Cuijpers 2007
- Cuijpers P, Straten A, Warmerdam L. Problem solving therapies for depression: a meta‐analysis. European Psychiatry 2007;22:9‐15. [DOI] [PubMed] [Google Scholar]
de Boer 2011
- Boer AGEM, Taskila T, Tamminga SJ, Frings‐Dresen MHW, Feuerstein M, Verbeek JH. Interventions to enhance return‐to‐work for cancer patients. Cochrane Database of Systematic Reviews 2011, Issue 3. [DOI: 10.1002/14651858.CD007569.pub2] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eriksson 2008
- Eriksson UB, Starrin B, Janson S. Long‐term sickness absence due to burnout: absentees' experiences. Qualitative Health Research 2008;18(5):620‐32. [DOI] [PubMed] [Google Scholar]
Eriksson 2010
- Eriksson T, Karlström E, Jonsson H, Tham K. An exploratory study of the rehabilitation process of people with stress‐related disorders. Scandinavian Journal of Occupational Therapy 2010;17(1):29‐39. [DOI] [PubMed] [Google Scholar]
EuroQol Group 1990
Flaxman 2010
- Flaxman PE, Bond FW. A randomised worksite comparison of acceptance and commitment therapy and stress inoculation training. Behaviour Research and Therapy 2010;48(8):816‐20. [DOI] [PubMed] [Google Scholar]
Fransen 2007
- Fransen GAJ, Marrewijk CJ, Mujakovic S, Muris JWM, Laheij RJF, Numans ME, et al. Pragmatic trials in primary care. Methodological challenges and solutions demonstrated by the DIAMOND‐study. BMC Medical Research Methodology 2007;7:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gehanno 2009
- Gehanno JF, Rollin L, Jean T, Louvel A, Darmoni S, Shaw W. Precision and recall of search strategies for identifying studies on return‐to‐work in MEDLINE. Journal of Occupational Rehabilitation 2009;19(3):223‐30. [DOI] [PubMed] [Google Scholar]
Glozier 2002
- Glozier N. Mental ill health and fitness for work. Occupational and Environmental Medicine 2002;59(10):714‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goetzel 2004
- Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. Journal of Occupational and Environmental Medicine 2004;46(4):398‐412. [DOI] [PubMed] [Google Scholar]
Hakanen 2011
- Hakanen JJ, Bakker AB, Jokisaari M. A 35‐year follow‐up study on burnout among Finnish employees. Journal of Occupational Health Psychology 2011;16(3):345–60. [DOI] [PubMed] [Google Scholar]
Hartman 2004
- Hartman H, Boerman A. Work disability pension 1987‐2003 [Arbeidsongeschiktheidsuitkeringen 1987‐2003]. Sociaal‐economische trends: statistischkwartaalblad over arbeidsmarkt, sociale zekerheid en inkomen 4e kwartaal. Voorburg: CBS, 2004. [Google Scholar]
Henderson 2005
- Henderson M, Glozier N, Elliott KH. Long term sickness absence. BMJ 2005;330(7495):802‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hensing 2004
- Hensing G, Wahlstrom R. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 7. Sickness absence and psychiatric disorders. Scandinavian Journal of Public Health. Supplement 2004;63:152‐80. [DOI] [PubMed] [Google Scholar]
Hensing 2006
- Hensing G, Andersson L, Brage S. Increase in sickness absence with psychiatric diagnosis in Norway: a general population‐based epidemiologic study of age, gender and regional distribution. BMC Medicine 2006;4:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Innstrand 2011
- Innstrand ST, Langballe EM, Falkum E, Aasland OG. Exploring within‐ and between‐gender differences in burnout: 8 different occupational groups. International Archives of Occupational and Environmental Health 2011;84(7):813‐24. [DOI] [PubMed] [Google Scholar]
Israel 1996
- Israel BA, Baker EA, Goldenhar LM, Heaney CA, Schurman SJ. Occupational stress, safety, and health: conceptual framework and principles for effective prevention interventions. Journal of Occupational Health Psychology 1996;1(3):261‐86. [DOI] [PubMed] [Google Scholar]
Jansson 2007
- Jansson I, Bjorklund A. The experience of returning to work. Work: Journal of Prevention, Assessment & Rehabilitation 2007;28(2):121‐34. [PubMed] [Google Scholar]
Jónsson 2011
- Jónsson H, Hougaard E, Bennedsen BE. Randomized comparative study of group versus individual cognitive behavioural therapy for obsessive compulsive disorder. Acta Psychiatrica Scandinavica 2011;123:387–97. [DOI] [PubMed] [Google Scholar]
Kessler 1997
- Kessler RC, Frank RG. The impact of psychiatric disorders on work loss days. Psychological Medicine 1997;27:861‐73. [DOI] [PubMed] [Google Scholar]
Kessler 2004
- Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research 2004;13(2):93‐121. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koopman 2002
- Koopman C, Pelletier KR, Murray JF, Sharda CE, Berger ML, Turpin RS, et al. Stanford presenteeism scale: health status and employee productivity. Journal of Occupational and Environmental Medicine 2002;44(1):14‐20. [DOI] [PubMed] [Google Scholar]
Koopmans 2011
- Koopmans PC, Bultmann U, Roelen CA, Hoedeman R, Klink JJ, Groothoff JW. Recurrence of sickness absence due to common mental disorders. International Archives of Occupational and Environmental Health 2011;84(2):193‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lagerveld 2010
- Lagerveld SE, Bultmann U, Franche RL, Dijk FJ, Vlasveld MC, Feltz‐Cornelis CM, et al. Factors associated with work participation and work functioning in depressed workers: a systematic review. Journal of Occupational Rehabilitation 2010;20(3):275‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lerner 2001
- Lerner D, Amick BC 3rd, Rogers WH, Malspeis S, Bungay K, Cynn D. The Work Limitations Questionnaire. Medical Care 2001;39(1):72‐85. [DOI] [PubMed] [Google Scholar]
Lerner 2008
- Lerner D, Henke RM. What does research tell us about depression, job performance, and work productivity?. Journal of Occupational and Environmental Medicine 2008;50(4):401‐10. [DOI] [PubMed] [Google Scholar]
Lim 2000
- Lim D, Sanderson K, Andrews G. Lost productivity among full‐time workers with mental disorders. Journal of Mental Health Policy and Economics 2000;3(3):139‐46. [DOI] [PubMed] [Google Scholar]
Lisv 2000
- Lisv. Trendrapportage arbeidsongeschiktheid 2000. Amsterdam: Landelijk Instituut Sociale Verzekeringen (Lisv), 2000. [Google Scholar]
Longmore 2007
- Longmore RJ, Worrell M. Do we need to challenge thoughts in cognitive behavior therapy?. Clinical Psychology Review 2007;27:173‐87. [DOI] [PubMed] [Google Scholar]
Lovibond 1995
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd Edition. Sydney: Psychology Foundation, 1995. [Google Scholar]
Lumley 2002
- Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annual Review of Public Health 2002;23:151‐69. [DOI] [PubMed] [Google Scholar]
Marine 2006
- Marine A, Ruotsalainen JH, Serra C, Verbeek JH. Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD002892.pub2] [DOI] [PubMed] [Google Scholar]
Maslach 1996
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd Edition. Palo Alto, CA: Consulting Psychologists Press, 1996. [Google Scholar]
Melamed 1992
- Melamed S, Kushnir T, Shirom A. Burnout and risk factors for cardiovascular diseases. Behavioral Medicine 1992;18:53‐60. [DOI] [PubMed] [Google Scholar]
Merrick 2007
- Merrick ES, Volpe‐Vartanian J, Horgan CM, McCann B. Alcohol & drug abuse: revisiting employee assistance programs and substance use problems in the workplace: key issues and a research agenda. Psychiatric Services 2007;58(10):1262‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Michie 2003
- Michie S, Williams S. Reducing work related psychological ill health and sickness absence: a systematic literature review. Occupational and Environmental Medicine 2003;60(1):3‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCOD 2009
- NCOD. Occupational Diseases in Numbers 2009 [Beroepsziekten in cijfers 2009]. Amsterdam: Netherlands Center for Occupational Diseases [Nederlands Centrum voor Beroepsziekten], 2009. [Google Scholar]
Nielsen 2010
- Nielsen MB, Bultmann U, Amby M, Christensen U, Diderichsen F, Rugulies R. Return to work among employees with common mental disorders: study design and baseline findings from a mixed‐method follow‐up study. Scandinavian Journal of Public Health 2010;38(8):864‐72. [DOI] [PubMed] [Google Scholar]
Nielsen 2011
Nielsen 2011b
- Nielsen MB, Madsen IE, Bültmann U, Christensen U, Diderichsen F, Rugulies R. Predictors of return to work in employees sick‐listed with mental health problems: findings from a longitudinal study. European Journal of Public Health 2011;21(6):806‐11. [DOI] [PubMed] [Google Scholar]
Nieuwenhuijsen 2006
- Nieuwenhuijsen K, Verbeek JH, Boer AG, Blonk RW, Dijk FJ. Predicting the duration of sickness absence for patients with common mental disorders in occupational health care. Scandinavian Journal of Work, Environment & Health 2006;32(1):67‐74. [DOI] [PubMed] [Google Scholar]
Nieuwenhuijsen 2008
- Nieuwenhuijsen K, Bültmann U, Neumeyer‐Gromen A, Verhoeven AC, Verbeek JHAM, Feltz‐Cornelis CM. Interventions to improve occupational health in depressed people. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD006237.pub2] [DOI] [PubMed] [Google Scholar]
Rai 2010
- Rai D, Skapinakis P, Wiles N, Lewis G, Araya R. Common mental disorders, subthreshold symptoms and disability: longitudinal study. British Journal of Psychiatry 2010;197:411‐2. [DOI] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Roelen 2009
- Roelen CA, Koopmans PC, Hoedeman R, Bültmann U, Groothoff JW, Klink JJ. Trends in the incidence of sickness absence due to common mental disorders between 2001 and 2007 in the Netherlands. European Journal of Public Health 2009;19(6):625‐30. [DOI] [PubMed] [Google Scholar]
Sanderson 2006
- Sanderson K, Andrews G. Common mental disorders in the workforce: recent findings from descriptive and social epidemiology. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie 2006;51(2):63‐75. [DOI] [PubMed] [Google Scholar]
Schaafsma 2010
- Schaafsma F, Schonstein E, Whelan KM, Ulvestad E, Kenny DT, Verbeek JH. Physical conditioning programs for improving work outcomes in workers with back pain. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD001822.pub2] [DOI] [PubMed] [Google Scholar]
Schröer 1993
- Schröer CAP. Ziekteverzuim wegens overspanning: een onderzoek naar de aard van overspanning, de hulpverlening en het verzuimbeloop [Absenteeism due to 'overstrain']. PhD Thesis. Maastricht: Universitaire Pers Maastricht, 1993. [ISBN 90‐5278‐058‐7] [Google Scholar]
Simon 2001
- Simon GE, Barber C, Birnbaum HG, Frank RG, Greenberg PE, Rose RM, et al. Depression and work productivity: the comparative costs of treatment versus nontreatment. Journal of Occupational and Environmental Medicine 2001;43(1):2‐9. [DOI] [PubMed] [Google Scholar]
Smith 1998
- Smith AP, Johal S, Wadsworth E, Smith GD, Harvey I, Peters T. The scale and costs of occupational stress. Occupational Health Review 1998;May/June:19‐22. [Google Scholar]
Smith 2000
- Smith A. The scale of perceived occupational stress. Occupational Medicine 2000;50(5):294‐8. [DOI] [PubMed] [Google Scholar]
Sobell 2009
- Sobell LC, Sobell MB, Agrawal S. Randomized controlled trial of a cognitive–behavioral motivational intervention in a group versus individual format for substance use disorders. Psychology of Addictive Behaviors 2009;23(4):672–83. [DOI] [PubMed] [Google Scholar]
Statistics Netherlands 2008
- Statistics Netherlands [CBS]. Work andSocial Security [Arbeid en Sociale Zekerheid]. Statistisch Jaarboek 2008. Voorburg: CBS, 2008. [Google Scholar]
Terluin 2004
- Terluin B, Rhenen W, Schaufeli WB, et al. The four‐dimensional symptom questionnaire (4DSQ): measuring distress and other mental health problems in a working population. Work Stress 2004;18(3):187‐207. [Google Scholar]
Terluin 2006
- Terluin B, Marwijk HW, Adèr HJ, Vet HC, Penninx BW, Hermens ML, et al. The Four‐Dimensional Symptom Questionnaire (4DSQ): a validation study of a multidimensional self‐report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry 2006;6(34):e‐publication. [DOI: 10.1186/1471-244X-6-34; PUBMED: 16925825] [DOI] [PMC free article] [PubMed] [Google Scholar]
van der Klink 2000
- Klink JJL, ed. Guideline for the Management of Mental Health Problems by Occupational Physicians [Dutch]. Eindhoven: NVAB [Netherlands Society of Occupational Medicine], 2000. [Google Scholar]
van der Klink 2001
- Klink JJL, Blonk RWB, Schene AH, Dijk FJH. The benefits of interventions for work‐related stress. American Journal of Public Health 2001;91(2):270‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
van der Klink 2007
- Klink JJL, ed. Guideline: Management of Mental Health Problems of Workers by Occupational Physicians [Dutch]. Utrecht: NVAB [Netherlands Society ofOccupational Medicine], 2007. [Google Scholar]
van Oostrom 2009
- Oostrom SH, Driessen MT, Vet HC, Franche RL, Schonstein E, Loisel P, et al. Workplace interventions for preventing work disability. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD006955.pub2] [DOI] [PubMed] [Google Scholar]
van Rhenen 2008
- Rhenen W, Schaufeli WB, Dijk FJ, Blonk RW. Coping and sickness absence. International Archives of Occupational and Environmental Health 2008;81(4):461‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Verbeek 2011
Wagstaff 2001
- Wagstaff AJ, Ormrod D, Spencer CM. Tianeptine: a review of its use in depressive disorders. CNS Drugs 2001;15(3):231‐59. [DOI] [PubMed] [Google Scholar]
Ware 1992
- Ware JE, Sherbourne CD. The MOS 36‐item short‐form health survey (SF‐36). I. Conceptual framework and item selection. Medical Care 1992;30(6):473‐83. [PubMed] [Google Scholar]
World Health Organization 1990
- World Health Organization. Composite International Diagnostic Interview. Geneva: World Health Organization, 1990. [Google Scholar]
World Health Organization 1992
- World Health Organization. The ICD‐10 Classification of Mental and Behavioural Disorders. Geneva: WHO, 1992. [Google Scholar]


