Abstract
Objectives
Whilst public health measures were effective in reducing COVID-19 transmission, unintended negative consequences may have occurred. This study aims to assess changes alcohol consumption and the heavy episodic drinking (HED) during the pandemic.
Methods
Data were from the Optimise Study, a longitudinal cohort of Australian adults September 2020–August 2022 that over-sampled priority populations at higher risk of contracting COVID-19, developing severe COVID-19 or experiencing adverse consequences of lockdowns. Frequency of alcohol consumption (mean number of days per week) and past-week HED were self-reported. Generalised linear models estimated the association between time and (1) the frequency of alcohol consumption and (2) heavy episodic drinking.
Results
Data from 688 participants (mean age: 44.7 years, SD:17.0; 72.7% female) and 10,957 surveys were included. Mean days of alcohol consumption per week decreased from 1.92 (SD: 1.92) in 2020 to 1.54 (SD:1.94) in 2022. The proportion of participants reporting HED decreased from 25.4% in 2020 to 13.1% in 2022. During two lockdown periods, known as “lockdown five”, (OR:0.65, 95%CI [0.47,0.90]) and “lockdown six” (OR:0.76, 95%CI [0.67,0.87]), participants were less likely to report HED.
Conclusions
Participants alcohol drinking frequency and HED decreased during the pandemic. This study provides a strong description of alcohol consumption during the pandemic and suggests that lockdowns did not have the unintended consequences of increased alcohol consumption.
Background
The COVID-19 pandemic has dramatically changed people’s lives since the first case was reported in November 2019. To reduce COVID-19 transmission, many countries implemented public health measures [1]. In the jurisdiction of Victoria, the second most populous state in Australia, the first high-level lockdown was imposed on 30 March 2020. Restrictions involved stay-at-home orders, closures of schools and non-essential businesses, and restrictions on travel [2]. Between 2020 and 2021, the state of Victoria went through six lockdowns, collectively spanning a total of 262 days [3]. Lockdown measures in Victoria were strict and heavily policed, with only five reasons permitted to leave your home (food and supplies, exercise, caregiving, work if necessary and to get vaccinated). During these periods on-premise licensed venues were closed, but takeaway alcohol sales continued [4]. Although these measures were effective in limiting COVID-19 cases, hospitalisations and deaths in Victoria [5], they also restricted access to in-person social interactions, mental health services and physical health facilities, which are strategies many people use during times of increased distress [6]. Therefore, the COVID-19 pandemic created an environment that had the potential to lead to detrimental strategies, such as harmful alcohol consumption [7]. Previous studies indicated that exposure to such community-wide disasters (including natural disasters, pandemics, and terrorism) were associated with increased alcohol use [8–10].
The key mechanisms by which the pandemic may have increased alcohol consumption is via increases in stress. Victorians were subject to a range of stressors including direct concerns about a contagious and deadly disease, increased pressures related to the social isolation linked to the public health restrictions that were implemented and the potential economic impacts of the pandemic in terms of income and employment. A range of studies have highlighted that general stress can increase drinking and alcohol use disorders (e.g., see [11] for a review) and that drinking to cope is a key risk factor for problematic outcomes [12]. Similarly, while population-level studies often show that overall drinking declines during economic downturns (e.g. [13]), individuals who experience unemployment are at increased risk of alcohol use (e.g., [14]).
To date research on the impact of COVID-19 on alcohol consumption has generated mixed evidence. An early systematic review of the global literature that included 45 studies from December 2019 to November 2020 reported a trend towards increased alcohol consumption in the general population [15], while a cross-national European study found an average decrease in alcohol consumption and a reduced frequency of heavy episodic drinking during the first months of the COVID-19 pandemic [16]. More recent reviews point to significant heterogeneity in COVID-19 impacts between countries, meaning local evidence is key [17]. Australian data has generally showed relatively small impacts of the pandemic. For example, in one of the rare representative surveys conducted in the early part of the pandemic, Biddle et al. [18] found that one in five people reported increased alcohol use in May 2020 since the commencement of the pandemic, while a similar proportion of people reported that they reduced their alcohol consumption. More recent Australian studies have generally shown small declines in consumption [19, 20]. While early studies relied on convenience samples and retrospective measures, more recent survey and wastewater analyses have largely reproduced these findings [21, 22].
Existing studies suggest that some population groups were more likely to report increased alcohol consumption during the COVID-19 pandemic than others. A US national study comparing alcohol consumption in mid-2019 and mid-2020 found increased alcohol use among women, younger and non-Hispanic White participants [23]. A meta-analysis study investigating the factors associated with a change in alcohol consumption during the COVID-19 pandemic found that working remotely and losing income were predictors of increased alcohol consumption [24]. Analysis among samples of Australians pointed to bigger declines in drinking for young people [20] and baseline risky drinkers [19] than for older people and moderate drinkers.
Most Australian research that assessed alcohol consumption during the COVID-19 pandemic is based on cross-sectional, retrospective data [20, 25, 26], and therefore cannot explore changes in alcohol consumption over time. Existing Australian longitudinal studies have only examined the alcohol consumption at the early stage of lockdown or in the first year of the COVID-19 pandemic [7, 27, 28]. Measuring alcohol consumption over time in the pandemic, in a highly characterised group, is important to understand if changes occurred, and in what groups, to inform future pandemic planning. We aim to address this gap in evidence and use data from the Optimise Study, a longitudinal cohort study conducted from September 2020 to August 2022. We examined: (i) changes in the frequency of alcohol consumption and the proportion of heavy episodic drinking over time during the COVID-19 pandemic; (ii) the association between the frequency of alcohol consumption and social demographic characteristics, Christmas and lockdown periods; and (iii) the association between the heavy episodic drinking and social demographic characteristics, Christmas and lockdown periods.
Methods
Study design
The Optimise Study was a longitudinal cohort study of adults residing in Victoria, Australia.
Setting
The study was established to examine how the community managed and responded to the COVID-19 pandemic, including measuring the impact of public health restrictions aimed at reducing COVID-19 transmission.
Participants
Participants were recruited from 27 September 2020 to 18 December 2021, and were regularly followed up until August 2022. Optimise was not designed to be a representative sample but an in-depth study of priority populations. Thus, participants were intentionally oversampled from key groups considered at risk of: (i) contracting COVID-19; (ii) developing severe COVID-19; or (iii) experiencing adverse consequences of the restrictions. Eligible participants were aged 18 years or older, resided in Victoria, Australia, and provided verbal informed consent with research staff, recorded in the study database, due to public health restrictions at the time of recruitment precluding face-to-face contact with participants. Participants were recruited through paid and unpaid social media advertisements and flyers promoted through community and industry groups, community-based organisations, and social and professional networks. More detailed description of Optimise participants and methods can be found elsewhere [29–31].
Data measurement
Optimise participants were asked to complete a baseline survey and then monthly follow-up surveys, either self-completed online or in an interview with research staff. Participants included in the present study completed a baseline survey and at least two follow-up surveys, and completed their surveys in English.
We include data on key socio-demographic and pandemic-related measures in our analyses: participants’ age, gender (woman/man/other), education (high school or lower/TAFE or trade certificate/undergraduate/postgraduate), employment status (full time or self-employed/part time or casual/not employed/retired), working environment (attend workplace/work from home/both workplace and working from home/not working), place of residence (metropolitan/region), chronic health condition (yes/no), and high-risk worker status (yes/no). In the present study, we grouped aged care, hotel quarantine or COVID-19 border control, and healthcare workers into a broad ‘high risk worker’ category.
The primary outcome was the frequency of alcohol consumption (count of days), measured using the self-reported number of days in the past week that a participant consumed alcohol. Frequency of alcohol consumption was measured in both the baseline survey and each month’s follow-up survey using the question ‘In the past week, please estimate how many days per week did you consume any alcohol?’, with options of 0–7 days.
The secondary outcome was heavy episodic drinking in the past week (yes/no). Heavy episodic drinking was measured by the question ‘In the past week, please estimate how many days per week did you consume six or more alcoholic drinks in a single day’ in baseline and follow-up surveys, asked of all participants who indicated consuming alcohol at least one day in the past week. Participants were presented options of 0–7 days. A binary variable (yes/no) was then created for the analysis purposes, with ‘0 days’ = no and those who answered ‘0 days’ to the consumption question described above also coded as no, and ‘1 day’ to ‘7 days’ = yes.
The study period of October 2020–August 2022 included five lockdown periods in Victoria. To estimate the association between alcohol consumption and lockdown periods, we derived a categorical variable (non-lockdown period/lockdown 2/lockdown 4/lockdown 5/lockdown 6) according to participants’ survey completion date. Lockdown 3 (13–17th Feb 2021) was classified as a non-lockdown period in the analysis due to the short period of time (5 days).
Due to prior evidence of increases in alcohol consumption during the Christmas and New Year period [32, 33], to account for confounding, we derived a categorical variable according to participants’ survey completion date, with three categories (non-Christmas period/Christmas 2020/Christmas 2021). We classified the last three weeks of December and the first week of January as the Christmas period (e.g., 14th December 2020 – 10th January 2021 as Christmas 2020).
Statistical methods
Descriptive analysis summarised the demographic characteristics of the sample. To summarise the frequency of alcohol consumption, we calculated the mean and standard deviation (SD) of the number of days of alcohol consumption per week separately for socio-demographic groups and calendar years. To summarise heavy episodic drinking, the proportion of participants’ heavy drinking was reported by different socio-demographic groups and calendar years.
To estimate the associations between frequency of alcohol consumption in the past week (number of days), time and all the covariates, we fitted a generalised linear model for count data. The covariates included time, socio-demographic characteristics, Christmas period and lockdown period. Time (in one-week blocks) was a continuous variable from 1 to 101, representing the first week of October 2020 to the last week of August 2022. Exploratory analysis confirmed that the data had excess zeroes (41.5% of surveys had zero-days of alcohol drinking) and therefore a Zero-inflated Poisson model was fitted. Participants with complete data on all covariates were included in the model. The model parameters are presented as rate ratios (RR) and 95% CIs. The inherent correlation in the data due to the inclusion of multiple surveys per person was accounted for by using bootstrapped confidence intervals (CIs). Previous literature suggests that for Zero-inflated Poisson models, bootstrapping provides reliable confidence intervals compared to other methods [34]. Therefore, 95% CIs for model coefficients were calculated using a non-parametric bootstrap with 200 samples.
A generalised linear model was used to estimate the association between the binary outcome of heavy episodic drinking and time, socio-demographic characteristics, and Christmas and lockdown periods, accounting for repeated measures with generalised estimating equations (GEEs). GEEs offer the benefit of minimal assumptions about missingness and tolerate misspecification of the correlation in the data. The model results were reported as odds ratios (ORs), and 95% CIs.
Participants with missing data on covariates were included in descriptive analysis. Only participants with complete data on the outcome and all covariates were included in the regression models (i.e., a complete case analysis).
Ethical statement
Ethics approval for Optimise was provided by the Alfred Human Research Ethics Committee, Approval Number 333/20. Participants provided verbal informed consent with research staff, recorded in the study database, due to public health restrictions at the time of recruitment precluding face-to-face contact with participants.
All analyses were conducted using R version 4.1.3.
Results
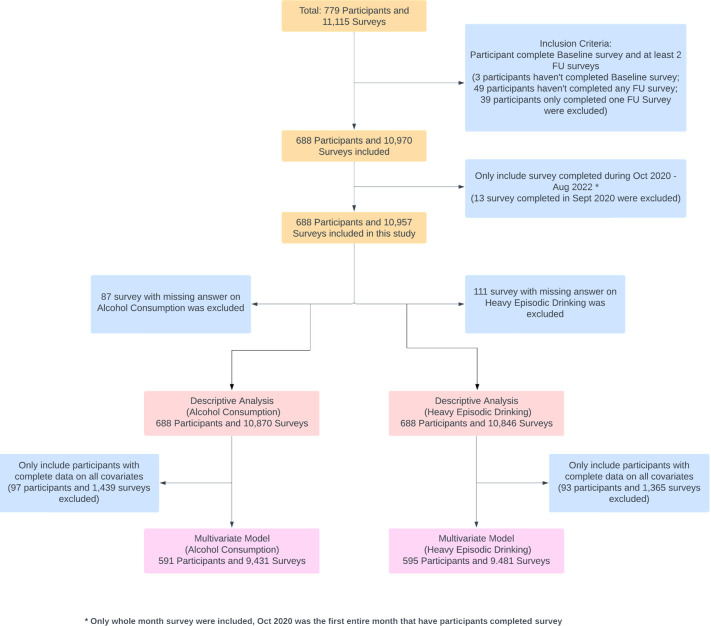
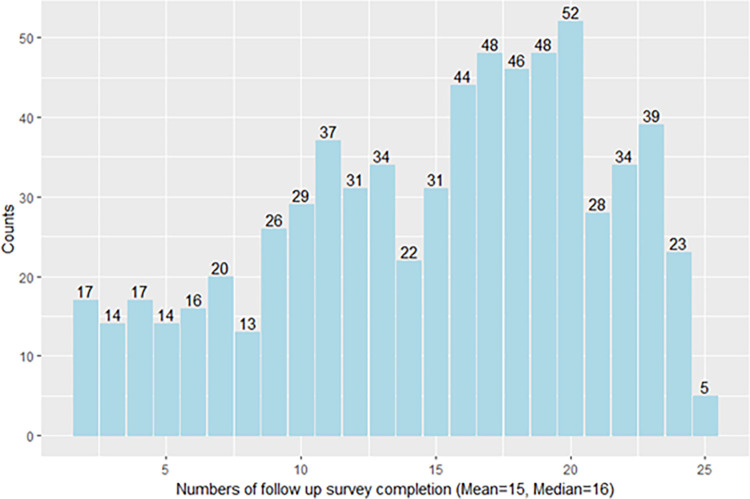
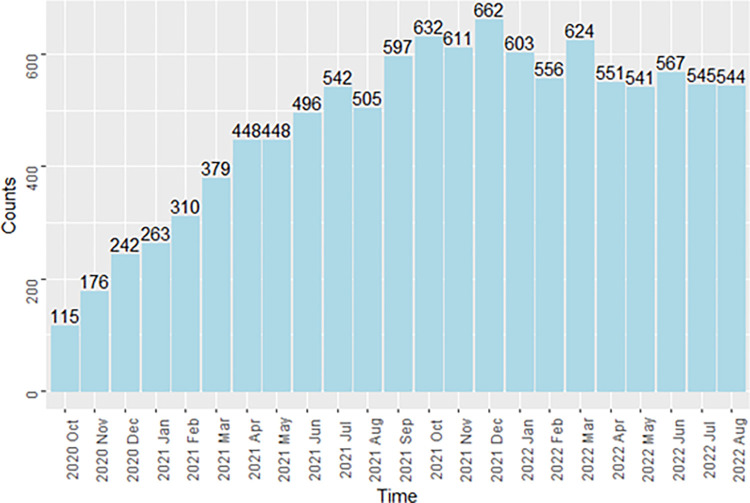
A participant flow chart is shown in Fig 1. In total, 779 participants were recruited into Optimise, of whom 688 (87.3%) completed the baseline survey and at least two follow-up surveys and were included in this study. Of the 688 participants, the mean number of completed follow-up surveys was 15, and the median number was 16 (Fig 2). Because Optimise had rolling recruitment, the number of follow-up surveys completed each month increased until reaching a peak in December 2021. Between July 2021 and August 2022, the total number of participants completing a follow-up survey was consistently above 500. Notably, the number of monthly completed surveys was still high (544) in the last month of the study period (Fig 3).
Fig 1. Participant flow chart.
Fig 2. Counts of follow-up surveys completed by Optimise participants, Victoria, Australia, N = 688 participants.
Fig 3. Counts of unique participants who completed a survey each month during October 2020 to August 2022, Optimise, Victoria, Australia, N = 10,957 surveys.
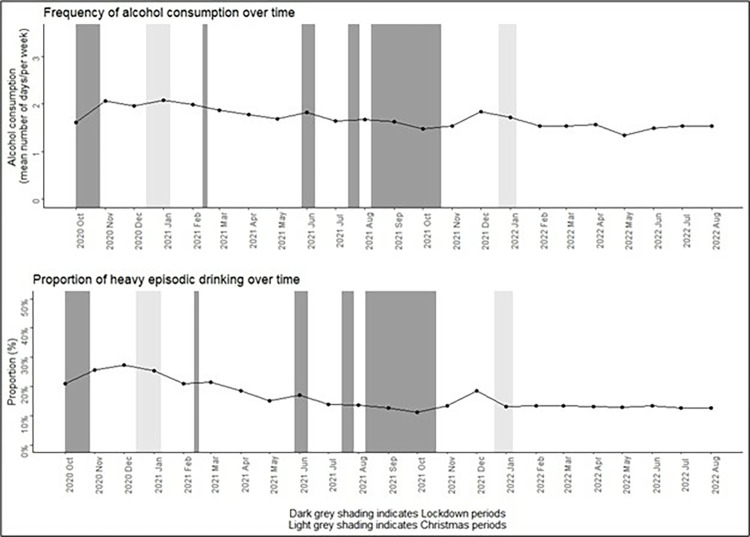
Among the 688 eligible participants, the mean age at baseline was 44.7 years (SD = 17.0), 72.7% were women, 81.0% lived in metropolitan Melbourne, 28.2% reported living with chronic health conditions, and 19.8% were identified as high-risk workers (Table 1). Across the entire study period of October 2020–August 2022, the mean days of alcohol consumption per week decreased from 1.92 (SD: 1.92) in 2020 to 1.54 (SD: 1.94) in 2022 (Table 2). Mean days of alcohol consumption per week increased slightly during the second lockdown period (October 2020) and 2020 Christmas period with some fluctuations throughout the study period (Fig 4).
Table 1. Description of the sociodemographic characteristics of Optimise participants, Victoria, Australia, N = 688.
| Demographic | Number | % total |
|---|---|---|
| Age (Years) | Mean = 44.7 | SD = 17.0 |
| Missing | 3 | |
| Age group, years | ||
| 18–24 | 113 | 16.4% |
| 25–34 | 141 | 20.5% |
| 35–44 | 104 | 15.1% |
| 45–54 | 112 | 16.3% |
| 55–64 | 114 | 16.6% |
| 65+ | 101 | 14.7% |
| Missing | 3 | 0.4% |
| Gender | ||
| Man | 181 | 26.3% |
| Woman | 500 | 72.7% |
| Other | 4 | 0.5% |
| Missing | 3 | 0.4% |
| Education | ||
| High school or lower | 118 | 17.2% |
| Tertiary education–TAFE/trade certificate | 111 | 16.1% |
| Tertiary education—undergraduate | 257 | 37.4% |
| Tertiary education—postgraduate | 198 | 28.8% |
| Missing | 4 | 0.6% |
| Employment status | ||
| Full-time/Self-employed | 243 | 35.3% |
| Part-time/Casual | 229 | 33.3% |
| Not employed | 86 | 12.5% |
| Retired | 105 | 15.3% |
| Missing | 25 | 3.7% |
| Working environment | ||
| Attend workplace | 224 | 32.6% |
| Work from home | 132 | 19.2% |
| Both workplace and working from home | 74 | 10.8% |
| Not working | 191 | 27.8% |
| Missing | 67 | 9.7% |
| Place of residence | ||
| Metro | 557 | 81.0% |
| Region | 124 | 18.0% |
| Missing | 7 | 1.0% |
| Chronic condition | ||
| Yes | 194 | 28.2% |
| No | 484 | 70.4% |
| Missing | 10 | 1.5% |
| High-risk workers * | ||
| Yes | 136 | 19.8% |
| No | 551 | 80.1% |
| Missing | 1 | 0.1% |
* High-risk workers: including aged care workers, hotel quarantine or COVID-19 border control workers, and healthcare workers
Table 2. Mean number of days of alcohol consumption past week and percentage of heavy episodic drinking of Optimise participants, Victoria, Australia, N = 688.
| Demographic | Alcohol consumption | Heavy episodic drinking | ||
|---|---|---|---|---|
| Mean (SD) | Number of surveys* | Yes (%) | Number of surveys* | |
| Total | 1.65 (1.95) Median = 1.00 |
10,870 | 1,659 (15.2%) | 10,846 |
| Year of survey completion | ||||
| 2020 | 1.92 (1.92) | 531 | 135 (25.4%) | 532 |
| 2021 | 1.72 (1.95) | 5,836 | 931 (16.0%) | 5,820 |
| 2022 | 1.54 (1.94) | 4,503 | 588 (13.1%) | 4,494 |
| Age group, years | ||||
| 18–24 | 1.21 (1.48) | 1,598 | 381 (23.8%) | 1,600 |
| 25–34 | 1.28 (1.54) | 2,130 | 397 (18.7%) | 2,128 |
| 35–44 | 1.58 (2.00) | 1,558 | 265 (17.0%) | 1,556 |
| 45–54 | 1.86 (2.05) | 1,717 | 304 (17.7%) | 1,714 |
| 55–64 | 1.81 (1.88) | 2,059 | 140 (6.8%) | 2,051 |
| 65+ | 2.19 (2.45) | 1,775 | 167 (9.5%) | 1,764 |
| Gender | ||||
| Man | 1.95 (2.01) | 2,711 | 605 (22.3%) | 2,709 |
| Woman | 1.55 (1.92) | 8,032 | 1,034 (12.9%) | 8,010 |
| Education | ||||
| High school or lower | 1.51 (1.91) | 1,768 | 322 (18.2%) | 1,765 |
| Tertiary education–TAFE/trade certificate | 1.44 (1.90) | 1,834 | 312 (17.0%) | 1,831 |
| Tertiary education—undergraduate | 1.67 (1.95) | 4,137 | 666 (16.1%) | 4,132 |
| Tertiary education—postgraduate | 1.81 (1.97) | 3,071 | 345 (11.3%) | 3,059 |
| Employment status | ||||
| Full-time/Self-employed | 1.83 (1.99) | 3,791 | 751 (19.9%) | 3,782 |
| Part-time/Casual | 1.51 (1.77) | 3,499 | 525 (15.0%) | 3,499 |
| Not employed | 1.21 (1.66) | 1,317 | 231 (17.6%) | 1,315 |
| Retired | 1.96 (2.29) | 1,880 | 113 (6.1%) | 1,867 |
| Working environment | ||||
| Attend workplace | 1.52 (1.80) | 3,315 | 531 (16.0%) | 3,310 |
| Work from home | 1.86 (1.96) | 2,168 | 401 (18.5%) | 2,163 |
| Both workplace and working from home | 2.06 (1.99) | 1,205 | 254 (21.1%) | 1,205 |
| Not working | 1.65 (2.08) | 3,197 | 344 (10.8%) | 3,182 |
| Place of residence | ||||
| Metro | 1.60 (1.92) | 8,653 | 1,333 (15.4%) | 8,634 |
| Region | 1.87 (2.06) | 2,138 | 307 (14.4%) | 2,133 |
| Chronic condition | ||||
| Yes | 1.73 (2.15) | 3,211 | 300 (9.4%) | 3,202 |
| No | 1.63 (1.86) | 7,519 | 1,343 (17.9%) | 7,506 |
| High-risk workers ** | ||||
| Yes | 1.49 (1.84) | 2,133 | 1,417 (16.3%) | 8,700 |
| No | 1.70 (1.97) | 8,718 | 235 (11.0%) | 2,127 |
*Number of surveys completed during the study period
**High-risk workers: including aged care workers, hotel quarantine or COVID-19 border control workers, and healthcare workers
All demographic variables (including Age, Gender, Education, Employment status, Working environment, Place of residence, Chronic condition and high-risk workers) were measured at baseline.
Fig 4. Frequency of alcohol consumption and proportion of heavy episodic drinking by month, October 2020 to August 2022, Optimise, Victoria, Australia, N = 688.
* Lockdown 2: 9th July 2020 – 27th October 2020, Lockdown 3: 13th Feb 2021 – 17th Feb 2021, Lockdown 4: 28th May 2021 – 10th June 2021, Lockdown 5: 16th July 2021 – 27th July 2021, Lockdown 6: 5th August 2021 – 21st October 2021.
Among the 688 participants, the prevalence of heavy episodic drinking decreased from 25.4% in 2020 to 13.1% in 2022. In contrast to the frequency of alcohol consumption, participants aged 18–25 years (23.8%) reported a higher prevalence of heavy episodic drinking compared with other age groups. Higher prevalence of heavy episodic drinking was also reported among participants who were male (22.3%) compared with female (12.9%); those who had a hybrid working environment (21.1%); or were high-risk workers (16.3%) (Table 2).
Of the 688 eligible participants, 591 participants had complete data on the outcome and all covariates and contributed 9,431 surveys to the regression modelling of frequency of alcohol consumption. Compared to participants aged 18–24 years, those aged 35–44 (adjusted rate ratio (aRR): 1.50; 95% CI: 1.17–1.99), 45–54 (aRR: 1.68; 95% CI: 1.36–2.11), 55–64 (aRR:1.56; 95% CI: 1.24–1.96), and over 65 years (aRR:2.19; 95% CI: 1.69–2.79) reported higher frequency of alcohol consumption during the study period. The frequency of alcohol consumption was associated with Christmas periods compared to the non-Christmas period, the mean number of days per week that participants consumed alcohol was 1.09 times higher (95% CI: 1.01–1.19) during the 2020 Christmas period, and 1.21 times higher (95% CI: 1.11–1.31) during the 2021 Christmas period (Table 3). We did not find evidence of an association between the frequency of alcohol consumption and lockdown periods.
Table 3. Association between alcohol consumption frequency and sociodemographic variables, lockdown period and Christmas period.
Results of zero-inflated Poisson regression, Optimise, Victoria, Australia, N = 9,431 surveys from 591 participants.
| Variable | Alcohol consumption | |
|---|---|---|
| Unadjusted Rate Ratio (95% CI†) | Adjusted Rate Ratio* (95% CI) | |
| Age group, years | ||
| 18–24 | Reference group | Reference group |
| 25–34 | 1.08 (0.87, 1.34) | 1.06 (0.81, 1.31) |
| 35–44 | 1.43 (1.07, 1.83) | 1.50 (1.17, 1.99) |
| 45–54 | 1.60 (1.30, 1.96) | 1.68 (1.36, 2.11) |
| 55–64 | 1.45 (1.17, 1.78) | 1.56 (1.24, 1.96) |
| 65+ | 1.97 (1.56, 2.44) | 2.19 (1.69, 2.79) |
| Gender | ||
| Woman | Reference group | Reference group |
| Man | 1.11 (0.95, 1.24) | 1.11 (0.96, 1.26) |
| Education | ||
| High school or lower | Reference group | Reference group |
| Tertiary education–TAFE/trade certificate | 1.09 (0.82, 1.37) | 0.94 (0.69, 1.20) |
| Tertiary education—undergraduate | 1.07 (0.86, 1.33) | 1.10 (0.91, 1.37) |
| Tertiary education—postgraduate | 1.14 (0.90, 1.45) | 1.01 (0.81, 1.23) |
| Working environment | ||
| Not working | Reference group | Reference group |
| Attend workplace | 0.83 (0.68, 1.00) | 1.01 (0.82, 1.25) |
| Work from home | 0.95 (0.81, 1.13) | 1.11 (0.91, 1.34) |
| Both workplace and working from home | 1.01 (0.82, 1.23) | 1.24(0.98, 1.54) |
| Place of residence | ||
| Region | Reference group | Reference group |
| Metro | 0.91 (0.77, 1.10) | 1.03 (0.84, 1.18) |
| Chronic condition | ||
| No | Reference group | Reference group |
| Yes | 1.21 (1.05, 1.36) | 1.04 (0.86, 1.17) |
| High-risk workers ** | ||
| No | Reference group | Reference group |
| Yes | 0.98 (0.82, 1.14) | 1.00 (0.82, 1.22) |
| Lockdown period *** | ||
| Non-lockdown period | Reference group | Reference group |
| Lockdown 2 | 0.95 (0.75, 1.15) | 0.93 (0.71, 1.13) |
| Lockdown 4 | 1.02 (0.96, 1.11) | 1.01 (0.94, 1.10) |
| Lockdown 5 | 1.01 (0.91, 1.11) | 1.00 (0.90, 1.08) |
| Lockdown 6 | 1.03 (0.97, 1.08) | 1.00 (0.95, 1.04) |
| Christmas period | ||
| Non-Christmas period | Reference group | Reference group |
| Christmas 2020 | 1.05 (0.96, 1.13) | 1.09 (1.01, 1.19) |
| Christmas 2021 | 1.23 (1.15, 1.31) | 1.21 (1.11, 1.31) |
†95% CIs were calculated for this model using a non-parametric bootstrap with 200 samples
*Adjusted for time
**High-risk workers: including aged care workers, hotel quarantine or COVID-19 border control workers, and healthcare workers
***Lockdown 2: 9th July 2020 – 27th October 2020
Lockdown 4: 28th May 2021 – 10th June 2021
Lockdown 5: 16th July 2021 – 27th July 2021
Lockdown 6: 5th August 2021 – 21st October 2021
Lockdown 3 (13th Feb 2021 – 17th Feb 2021) was classified as non-lockdown period in the analysis due to the short period of time
All demographic variables (including Age, Gender, Education, Working environment, Place of residence, Chronic condition and high-risk workers) were measured at baseline.
Of the 688 eligible participants, 595 participants had complete data on the outcome and all covariates and contributed 9,481 surveys to the analysis of heavy episodic drinking. Men had 1.58 times (95% CI: 1.10–2.31) higher odds of reporting heavy episodic drinking compared with women during the study period. Participants aged over 55 (adjusted odds ratio (aOR): 0.29, 95% CI: 0.14–0.60; aOR: 0.32, 95% CI: 0.13–0.81) had lower odds of reporting heavy episodic drinking compared to those aged 18–24 years. Participants with a postgraduate degree had a 0.53 (95% CI: 0.28–0.99) reduced odds of reporting heavy episodic drinking compared to those with a high school or lower degree. Lockdown five (OR: 0.65, 95% CI: 0.48–0.90) and six (OR: 0.76, 95% CI: 0.66–0.86) were strongly associated with a decreased odds of reporting heavy episodic drinking compared to non-lockdown periods. Both the 2020 and 2021 Christmas periods were strongly associated with reporting heavy episodic drinking (Table 4).
Table 4. Association between heavy episodic drinking and sociodemographic variables, lockdown period and Christmas period.
Results of generalised linear model with GEEs, Optimise, Victoria, Australia, N = 9,481 surveys from 595 participants.
| Variable | Heavy episodic drinking | |
|---|---|---|
| Unadjusted Odds Ratio (95% CI) | Adjusted Odds Ratio* (95% CI) | |
| Age group, years | ||
| 18–24 | Reference group | Reference group |
| 25–34 | 0.73 (0.46, 1.16) | 0.82 (0.46, 1.44) |
| 35–44 | 0.69 (0.40, 1.20) | 0.79 (0.41, 1.53) |
| 45–54 | 0.77 (0.44, 1.32) | 0.90 (0.45, 1.78) |
| 55–64 | 0.25 (0.13, 0.47) | 0.29 (0.14, 0.59) |
| 65+ | 0.32 (0.16, 0.65) | 0.32 (0.13, 0.80) |
| Gender | ||
| Female | Reference group | Reference group |
| Male | 1.90 (1.32, 2.75) | 1.58 (1.09, 2.31) |
| Education | ||
| High school or lower | Reference group | Reference group |
| Tertiary education–TAFE/trade certificate | 0.96 (0.53, 1.73) | 0.96 (0.50, 1.84) |
| Tertiary education—undergraduate | 0.83 (0.52, 1.33) | 0.83 (0.49, 1.40) |
| Tertiary education—postgraduate | 0.54 (0.32, 0.91) | 0.53 (0.28, 0.99) |
| Working environment | ||
| Not working | Reference group | Reference group |
| Attend workplace | 1.59 (0.96, 2.65) | 1.04 (0.53, 2.01) |
| Work from home | 1.84 (1.05, 3.22) | 1.28 (0.62, 2.61) |
| Both workplace and working from home | 2.14 (1.14, 4.02) | 1.62 (0.79, 3.33) |
| Place of residence | ||
| Region | Reference group | Reference group |
| Metro | 1.09 (0.67, 1.78) | 0.80 (0.47, 1.37) |
| Chronic condition | ||
| No | Reference group | Reference group |
| Yes | 0.46 (0.30, 0.71) | 0.64 (0.40, 1.04) |
| High-risk workers ** | ||
| No | Reference group | Reference group |
| Yes | 0.66 (0.41, 1.05) | 0.67 (0.39, 1.16) |
| Lockdown period *** | ||
| Non-lockdown period | Reference group | Reference group |
| Lockdown 2 | 0.79 (0.50, 1.25) | 0.85 (0.51, 1.41) |
| Lockdown 4 | 0.75 (0.61, 0.93) | 0.81 (0.64, 1.02) |
| Lockdown 5 | 0.67 (0.51, 0.89) | 0.65 (0.47, 0.90) |
| Lockdown 6 | 0.74 (0.66, 0.83) | 0.76 (0.67, 0.87) |
| Christmas period | ||
| Non-Christmas period | Reference group | Reference group |
| Christmas 2020 | 1.40 (1.07, 1.82) | 1.37 (1.01, 1.84) |
| Christmas 2021 | 1.37 (1.17, 1.60) | 1.27 (1.06, 1.52) |
* Adjusted for time
** High-risk workers: including aged care workers, hotel quarantine or COVID-19 border control workers, and healthcare workers
*** Lockdown 2: 9th July 2020 – 27th October 2020
Lockdown 4: 28th May 2021 – 10th June 2021
Lockdown 5: 16th July 2021 – 27th July 2021
Lockdown 6: 5th August 2021 – 21st October 2021
Lockdown 3 (13th Feb 2021 – 17th Feb 2021) was classified as non-lockdown period in the analysis due to the short period of time
All demographic variables (including Age, Gender, Education, Working environment, Place of residence, Chronic condition and high-risk workers) were measured at baseline.
Discussion
Using longitudinal data from 688 participants, this study assessed the frequency of alcohol consumption and heavy episodic drinking over time during the COVID-19 pandemic (October 2020 to August 2022). Our study findings show that the alcohol consumption and heavy episodic drinking among a sample facing increased levels of risk from the pandemic decreased between 2020 and 2022. Consistent with the existing evidence [35, 36], our study found that older adults reported the highest frequency of alcohol consumption, but lower rates of heavy episodic drinking. Men and participants with lower educational attainment were more likely to engage in heavy episodic drinking. Again, this is consistent with both Australian and international research [37–39]. Notably, our study, among people vulnerable to unintended consequences of public health measures used to control COVID-19, suggests that alcohol use did not increase during periods of lockdowns and intense restrictions.
This study found that lockdowns five and six were strongly associated with decreased odds of reporting heavy episodic drinking compared with non-lockdown periods. Notably, lockdown six was the second longest lockdown, at 77 days and the final lockdown imposed. This finding is contrast to some previous studies that found increased alcohol consumption during lockdown periods [40–42], although these studies were from the US and did not focus on specifically vulnerable populations. Previous Australian research focused on the 2020 lockdowns found shifts in drinking locations, but no major changes in levels of consumption [19], while other Australian work suggested that people experiencing specific distresses from the pandemic were more likely to increase drinking [43], but again found limited overall changes in population drinking. No Australian research has examined the specific sub-populations included here or examined the major lockdowns that occurred in 2021 in Victoria, Australia. One potential reason for a decline in heavy episodic drinking, might be the restrictions on public gatherings, along with the shutdown of bars and restaurants, resulting in a decline in heavy drinking occasions [44]. Previous work has also shown that young people’s drinking likely declined in Australia during the pandemic [20], and the reductions in heavy episodic drinking found here likely reflect this shift. Previous international studies suggested that increases in drinking may reflect its use as a negative coping mechanism during the pandemic to manage psychological distress [45, 46], and there is some evidence that severe alcohol-related harms increased in Australia during the pandemic [47], so the reductions identified here may reflect the particular characteristics of our study sample although we expected the sub-populations we recruited to experience higher levels of distress given their increased exposure to risk. On the whole, the negative association between lockdowns and alcohol consumption observed in this sample does alleviate some concern about unintended consequences of public health measures used to control future pandemics, at least where those measures are successful. In contrast to the general finding that Australian alcohol consumption declined, a number of other jurisdictions saw clear increases in population drinking and alcohol harms (e.g. [48–50]). These differences may reflect the additional stress of high levels of exposure to COVID-19 and associated increases in morbidity and mortality compared to the Australian experience, although more detailed cross-national work is needed to better understand the heterogeneity in alcohol trends across the pandemic internationally.
The longitudinal design we used is a strength of this study. By actively following the participants for two years during the COVID-19 pandemic, our study provides new insights on changes in alcohol consumption during the pandemic. Beyond the short-term effects of lockdown onset on drinking behaviours that have been examined in previous studies [19, 20], this study has included five lockdown periods in the analysis, thus offering a more comprehensive view on how extended or recurring lockdowns can impact individuals’ alcohol consumption patterns. Additionally, our study has excellent sample retention, which reduces the potential for selection bias and further increases the internal validity of the results.
Several limitations of this study should be acknowledged. First, our study relied on self-reported frequency of alcohol consumption and heavy episodic drinking, which are subject to recall and other biases. Recall bias and social desirability bias may have led to under- or over-reporting of alcohol consumption therefore the effect of these biases on our study findings is unknown. Secondly, we were only able to assess the frequency of alcohol consumption and heavy episodic drinking by single survey items in this study, as the focus of Optimise was much broader than just substance use. More reliable measurement of alcohol use such as a validated scale may have improved the robustness of our results. In this study, we defined heavy episodic drinking as consuming six or more alcoholic drinks in a single day, which is not consistent with the Australian low risk drinking guidelines of more than four drinks [51], but this item is still broadly reflective of the international literature [52] and trends are unlikely to be affected. It is important to note that survey responses were assigned as being in a category of the lockdown variable based on the date the participant completed the survey. Therefore, a participant may be recalling the past seven days in which not all seven days were “lockdown” or not all seven days were “non-lockdown”. It is important to note though that each participant was on an individual schedule of when they were invited to complete a survey, depending on their day of recruitment. Therefore, it was a small proportion of the sample that would have their alcohol consumption misclassified; misclassification may bias the estimates effects towards the null. Whilst we adjusted the model for important, measured confounders, we did not include an indicator for whether a participant was infected with COVID-19 around the time of survey completion which may have influenced their consumption of alcohol. Lastly, and most importantly, due to the design of the Optimise Study which oversampled high-risk groups, the findings of this study are not broadly generalisable.
This study provides one of the most comprehensive pictures of drinking changes in Victoria during the COVID-19 pandemic by using longitudinal data collected across two years. Although we did not find evidence of an association between frequency of alcohol consumption and lockdown periods in this study, we did find lockdowns five and six were strongly associated with decreased odds of reporting heavy episodic drinking, potentially easing early concerns about the impacts of public health restrictions on alcohol problems in the population.
Acknowledgments
Optimise is a partnership between the Burnet Institute and Peter Doherty Institute in collaboration with The University of Melbourne, Swinburne University, La Trobe University, Monash University, Victorian Department of Health and Human Services, Centre for Culture Ethnicity and Health, Health Issues Centre, and Royal Children’s Hospital, Independent Multicultural Consultant. The authors gratefully acknowledge the generosity of the community members who participated in the study. The authors appreciatively acknowledge the work of all Optimise project team members and collaborators who have contributed to the ongoing delivery of the study.
Data Availability
Data cannot be shared publicly because it contains sensitive information such as but not limited to detailed demographics of people, their use of alcohol, views on COVID-19 vaccines, and views on government policies. Data are required to be stored on a secure Burnet Institute server in line with the Alfred Health ethics-approved study protocol. Data are available from the Burnet Institute (contact via the Optimise Study team at optimisecovid.com.au) for researchers who meet the criteria for access to confidential data. Approved researchers would be able to access these data in the same manner as the authors.
Funding Statement
Optimise received funding support from the Victorian Government Department of Jobs, Precincts and Regions, the Victorian Department of Health, the Macquarie Group Foundation, and Burnet Institute donors. Funders did not have a role in the study design, data collection, analysis, decision to publish, nor preparation of the manuscript. The authors gratefully acknowledge the contribution to this work of the Victorian Operational Infrastructure Support Program received by the Burnet Institute. M.H. and K.B.G receive funding support from National Health and Medical Research Council Investigator grants. M.L. is funded by an ARC Future Fellowship. M.H., M.S. and A.P. have received investigator-initiated research funding from Gilead Sciences and AbbVie. M.S. and A.P. have received consultant fees from Gilead Sciences for activities unrelated to this work.
References
- 1.Mathieu E, Ritchie H, Rodés-Guirao H, Appel C, Giattino C, Hasell J, et al. Policy Responses to the Coronavirus Pandemic: Our World in Data; 2020. [Available from: https://ourworldindata.org/coronavirus. [Google Scholar]
- 2.Nally A. How Victoria’s coronavirus lockdown across 10 Melbourne postcodes will work: ABC News; 2020. [Available from: https://www.abc.net.au/news/2020-06-30/victorias-coronavirus-outbreak-prompts-stay-at-home-order/12407518. [Google Scholar]
- 3.Boaz J. Melbourne passes Buenos Aires’ world record for time spent in COVID-19 lockdown: ABC News; 2021. [Available from: https://www.abc.net.au/news/2021-10-03/melbourne-longest-lockdown/100510710. [Google Scholar]
- 4.Miller M, Mojica-Perez Y, Callinan S, Livingston M. A timeline of alcohol-related restrictions during the COVID-19 pandemic: Centre for Alcohol Policy Research, La Trobe University, Melbourne, Australia; 2020. [Available from: https://www.latrobe.edu.au/__data/assets/pdf_file/0006/1324149/A-timeline-of-alcohol-relevant-restrictions-during-the-COVID-19-pandemic-1.pdf. [Google Scholar]
- 5.Scott N, Abeysuriya RG, Delport D, Sacks-Davis R, Nolan J, West D, et al. COVID-19 epidemic modelling for policy decision support in Victoria, Australia 2020–2021. BMC Public Health. 2023;23(1):988. doi: 10.1186/s12889-023-15936-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lechner WV, Sidhu NK, Jin JT, Kittaneh AA, Laurene KR, Kenne DR. Increases in Risky Drinking During the COVID-19 Pandemic Assessed via Longitudinal Cohort Design: Associations With Racial Tensions, Financial Distress, Psychological Distress and Virus-Related Fears. Alcohol Alcohol. 2021;56(6):702–7. doi: 10.1093/alcalc/agab019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bollen Z, Pabst A, Creupelandt C, Fontesse S, Laniepce A, Maurage P. Longitudinal Assessment of Alcohol Consumption throughout the First COVID-19 Lockdown: Contribution of Age and Pre-Pandemic Drinking Patterns. Eur Addict Res. 2022;28(1):48–55. doi: 10.1159/000518218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boscarino JA, Kirchner HL, Hoffman SN, Sartorius J, Adams RE. PTSD and alcohol use after the World Trade Center attacks: a longitudinal study. J Trauma Stress. 2011;24(5):515–25. doi: 10.1002/jts.20673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.North CS, Ringwalt CL, Downs D, Derzon J, Galvin D. Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Arch Gen Psychiatry. 2011;68(2):173–80. doi: 10.1001/archgenpsychiatry.2010.131 [DOI] [PubMed] [Google Scholar]
- 10.Wu P, Liu X, Fang Y, Fan B, Fuller CJ, Guan Z, et al. Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol Alcohol. 2008;43(6):706–12. doi: 10.1093/alcalc/agn073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keyes KM, Hatzenbuehler ML, Grant BF, Hasin DS. Stress and alcohol: epidemiologic evidence. Alcohol Res. 2012;34(4):391–400. [PMC free article] [PubMed] [Google Scholar]
- 12.Corbin WR, Farmer NM, Nolen-Hoekesma S. Relations among stress, coping strategies, coping motives, alcohol consumption and related problems: A mediated moderation model. Addictive Behaviors. 2013;38(4):1912–9. doi: 10.1016/j.addbeh.2012.12.005 [DOI] [PubMed] [Google Scholar]
- 13.Pacula RL. Substance use and recessions: What can be learned from economic analyses of alcohol? International Journal of Drug Policy. 2011;22(5):326–34. doi: 10.1016/j.drugpo.2011.07.008 [DOI] [PubMed] [Google Scholar]
- 14.Popovici I, French MT. Does Unemployment Lead to Greater Alcohol Consumption? Industrial Relations: A Journal of Economy and Society. 2013;52(2):444–66. doi: 10.1111/irel.12019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roberts A, Rogers J, Mason R, Siriwardena AN, Hogue T, Whitley GA, et al. Alcohol and other substance use during the COVID-19 pandemic: A systematic review. Drug Alcohol Depend. 2021;229(Pt A):109150. doi: 10.1016/j.drugalcdep.2021.109150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kilian C, Rehm J, Allebeck P, Braddick F, Gual A, Barták M, et al. Alcohol consumption during the COVID-19 pandemic in Europe: a large-scale cross-sectional study in 21 countries. Addiction. 2021;116(12):3369–80. doi: 10.1111/add.15530 [DOI] [PubMed] [Google Scholar]
- 17.Sohi I, Chrystoja BR, Rehm J, Wells S, Monteiro M, Ali S, et al. Changes in alcohol use during the COVID-19 pandemic and previous pandemics: A systematic review. Alcoholism: Clinical and Experimental Research. 2022;46(4):498–513. doi: 10.1111/acer.14792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Biddle N, Edwards B, Gray M, Sollis K. Alcohol consumption during the COVID-19 period: May 2020. 2020. [Google Scholar]
- 19.Mojica-Perez Y, Livingston M, Pennay A, Callinan S. How did COVID-19 restrictions impact alcohol consumption in Australia? A longitudinal study. Drug Alcohol Rev. 2024;43(2):465–74. doi: 10.1111/dar.13810 [DOI] [PubMed] [Google Scholar]
- 20.Callinan S, Smit K, Mojica-Perez Y, D’Aquino S, Moore D, Kuntsche E. Shifts in alcohol consumption during the COVID-19 pandemic: early indications from Australia. Addiction. 2021;116(6):1381–8. doi: 10.1111/add.15275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bade R, Simpson BS, Ghetia M, Nguyen L, White JM, Gerber C. Changes in alcohol consumption associated with social distancing and self-isolation policies triggered by COVID-19 in South Australia: a wastewater analysis study. Addiction. 2021;116(6):1600–5. doi: 10.1111/add.15256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mojica-Perez Y, Livingston M, Pennay A, Callinan S. Examining how the first year of the COVID-19 pandemic affected alcohol use in different socio-demographic groups in an Australian representative longitudinal sample. Addiction. 2024;n/a(n/a). [DOI] [PubMed] [Google Scholar]
- 23.Pollard MS, Tucker JS, Green HD, Jr. Changes in Adult Alcohol Use and Consequences During the COVID-19 Pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. doi: 10.1001/jamanetworkopen.2020.22942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Acuff SF, Strickland JC, Tucker JA, Murphy JG. Changes in alcohol use during COVID-19 and associations with contextual and individual difference variables: A systematic review and meta-analysis. Psychol Addict Behav. 2022;36(1):1–19. doi: 10.1037/adb0000796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neill E, Meyer D, Toh WL, van Rheenen TE, Phillipou A, Tan EJ, et al. Alcohol use in Australia during the early days of the COVID-19 pandemic: Initial results from the COLLATE project. Psychiatry Clin Neurosci. 2020;74(10):542–9. doi: 10.1111/pcn.13099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int J Environ Res Public Health. 2020;17(11). doi: 10.3390/ijerph17114065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clare PJ, Aiken A, Yuen WS, Upton E, Kypri K, Degenhardt L, et al. Alcohol use among young Australian adults in May-June 2020 during the COVID-19 pandemic: a prospective cohort study. Addiction. 2021;116(12):3398–407. doi: 10.1111/add.15599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mojica-Perez Y, Livingston M, Pennay A, Callinan S. Examining the relationship between alcohol consumption, psychological distress and COVID-19 related circumstances: An Australian longitudinal study in the first year of the pandemic. Addict Behav. 2022;135:107439. doi: 10.1016/j.addbeh.2022.107439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gibbs L, Thomas AJ, Coelho A, Al-Qassas A, Block K, Meagher N, et al. Inclusion of Cultural and Linguistic Diversity in COVID-19 Public Health Research: Research Design Adaptations to Seek Different Perspectives in Victoria, Australia. Int J Environ Res Public Health. 2023;20(3). doi: 10.3390/ijerph20032320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nguyen T, Thomas AJ, Kerr P, Stewart AC, Wilkinson AL, Nguyen L, et al. Recruiting and retaining community-based participants in a COVID-19 longitudinal cohort and social networks study: lessons from Victoria, Australia. BMC Medical Research Methodology. 2023;23(1):54. doi: 10.1186/s12874-023-01874-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pedrana A, Bowring A, Heath K, Thomas AJ, Wilkinson A, Fletcher-Lartey S, et al. Priority populations’ experiences of isolation, quarantine and distancing for COVID-19: protocol for a longitudinal cohort study (Optimise Study). BMJ Open. 2024;14(1):e076907. doi: 10.1136/bmjopen-2023-076907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lemmens PH, Knibbe RA. Seasonal variation in survey and sales estimates of alcohol consumption. J Stud Alcohol. 1993;54(2):157–63. doi: 10.15288/jsa.1993.54.157 [DOI] [PubMed] [Google Scholar]
- 33.Lloyd B, Matthews S, Livingston M, Jayasekara H, Smith K. Alcohol intoxication in the context of major public holidays, sporting and social events: a time-series analysis in Melbourne, Australia, 2000–2009. Addiction. 2013;108(4):701–9. doi: 10.1111/add.12041 [DOI] [PubMed] [Google Scholar]
- 34.Kong M, Xu S, Levy SM, Datta S. GEE type inference for clustered zero-inflated negative binomial regression with application to dental caries. Comput Stat Data Anal. 2015;85:54–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Australian Institute of Health and Welfare. National Drug Strategy Household Survey 2019. 2020.
- 36.Institute of Alcohol Studies. Older people and alcohol. 2013.
- 37.Australian Bureau of Statistics. Alcohol consumption 2022 [Available from: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/alcohol-consumption/latest-release.
- 38.Gutema BT, Chuka A, Ayele G, Tariku EZ, Aschalew Z, Baharu A, et al. Prevalence of heavy episodic drinking and associated factors among adults residing in Arba Minch health and demographic surveillance site: a cross sectional study. BMC Public Health. 2020;20(1):1895. doi: 10.1186/s12889-020-09998-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murakami K, Hashimoto H. Associations of education and income with heavy drinking and problem drinking among men: evidence from a population-based study in Japan. BMC Public Health. 2019;19(1):420. doi: 10.1186/s12889-019-6790-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lechner WV, Laurene KR, Patel S, Anderson M, Grega C, Kenne DR. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addict Behav. 2020;110:106527. doi: 10.1016/j.addbeh.2020.106527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Merlo A, Severeijns NR, Benson S, Scholey A, Garssen J, Bruce G, et al. Mood and Changes in Alcohol Consumption in Young Adults during COVID-19 Lockdown: A Model Explaining Associations with Perceived Immune Fitness and Experiencing COVID-19 Symptoms. Int J Environ Res Public Health. 2021;18(19). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weerakoon SM, Jetelina KK, Knell G. Longer time spent at home during COVID-19 pandemic is associated with binge drinking among US adults. Am J Drug Alcohol Abuse. 2021;47(1):98–106. doi: 10.1080/00952990.2020.1832508 [DOI] [PubMed] [Google Scholar]
- 43.Tran TD, Hammarberg K, Kirkman M, Nguyen HTM, Fisher J. Alcohol use and mental health status during the first months of COVID-19 pandemic in Australia. Journal of Affective Disorders. 2020;277:810–3. doi: 10.1016/j.jad.2020.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.White HR, Stevens AK, Hayes K, Jackson KM. Changes in Alcohol Consumption Among College Students Due to COVID-19: Effects of Campus Closure and Residential Change. J Stud Alcohol Drugs. 2020;81(6):725–30. doi: 10.15288/jsad.2020.81.725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clay JM, Parker MO. Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? Lancet Public Health. 2020;5(5):e259. doi: 10.1016/S2468-2667(20)30088-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rodriguez LM, Litt DM, Stewart SH. Drinking to cope with the pandemic: The unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addict Behav. 2020;110:106532. doi: 10.1016/j.addbeh.2020.106532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Australian Bureau of Statistics. Causes of Death, Australia 2022 [Available from: https://www.abs.gov.au/statistics/health/causes-death/causes-death-australia/latest-release.
- 48.Angus C, Henney M, Pryce R. Modelling the longer-term health and health inequality impacts of changes in alcohol consumption during the COVID-19 pandemic in England. Journal of Public Health. 2024;46(2):286–93. doi: 10.1093/pubmed/fdae010 [DOI] [PubMed] [Google Scholar]
- 49.Angus C, Buckley C, Tilstra AM, Dowd JB. Increases in ‘deaths of despair’ during the COVID-19 pandemic in the United States and the United Kingdom. Public Health. 2023;218:92–6. doi: 10.1016/j.puhe.2023.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Castaldelli-Maia JM, Segura LE, Martins SS. The concerning increasing trend of alcohol beverage sales in the U.S. during the COVID-19 pandemic. Alcohol. 2021;96:37–42. doi: 10.1016/j.alcohol.2021.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.National Health and Medical Research Council. Australian guidelines to reduce health risks from drinking alcohol 2020 [Available from: https://www.nhmrc.gov.au/health-advice/alcohol.
- 52.Gmel G, Rehm J. Measuring alcohol consumption. Contemporary Drug Problems: An Interdisciplinary Quarterly. 2004;31(3):467–540. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data cannot be shared publicly because it contains sensitive information such as but not limited to detailed demographics of people, their use of alcohol, views on COVID-19 vaccines, and views on government policies. Data are required to be stored on a secure Burnet Institute server in line with the Alfred Health ethics-approved study protocol. Data are available from the Burnet Institute (contact via the Optimise Study team at optimisecovid.com.au) for researchers who meet the criteria for access to confidential data. Approved researchers would be able to access these data in the same manner as the authors.