SUMMARY
Background
Health care-associated infections (HAIs), albeit being the most frequent adverse event in health care, are mostly preventable through hand hygiene (HH). Given the extremely low HH compliance among healthcare workers (HCWs), educational initiatives aimed at this group are crucial. This study used an ultraviolet (UV)-based technology to assess the efficacy of an educational and training program on HH for HCWs in a second-level hospital in southern Italy.
Methods
A quasi-experimental study was conducted between November 2020 and February 2022. Participants were asked to rub their hands with an UV-labelled disinfectant solution before having digital images of both sides of their hands taken under UV-A light, using a device that recorded the solution’s distribution on each surface before and after the training session. The instrument recorded the percentage of surface covered (quantitative data) for each measurement along with the eventual passing of the 95% threshold (qualitative data).
Results
Following the training session, we observed a significant increase in the number of valid procedures as well as the mean coverage (expressed as the percentage of surface covered) for each surface examined. From 16.9% in the pre-interventional phase to 48.7% in the post-interventional phase, the percentage of HCWs who exceeded the 95% threshold on both sides of hands increased significantly (p<0,001).
Conclusions
The findings of our study show that the training intervention was effective in raising participants HH performance. Secondly, they suggest that giving HCWs immediate visual feedback on their progress throughout the learning process could help increase HH adequacy.
Keywords: HAI, hand hygiene, handrub, training, UV-A
INTRODUCTION
Health care-associated infections (HAIs), namely infections occurring in a patient during the process of care in a hospital or other healthcare facility which were not present or incubating at the time of admission, albeit being the most frequent adverse event in health care, can be significantly reduced by implementing effective infection prevention and control (IPC) policies and strategies, which include simple and low-cost practices such as good hand hygiene (HH) [1].
HH is an essential part of infection prevention and control (IPC) measures, a lack of which increases the risk of outbreaks of highly transmissible diseases within health facilities. In fact, HH monitoring is acknowledged as a crucial health care quality indicator [2].
Based on a review of hand hygiene studies run by the World Health Organization (WHO), baseline compliance with hand hygiene among healthcare workers (HCWs) is really low (only 38.7%, on average), despite the fact that it is widely regarded as the most crucial activity for HAI prevention [3].
Improving hand hygiene compliance among HCWs may be challenging since patterns of HH behaviour are formed and absorbed early in life. Given this, initiatives to enhance HH compliance in HCWs should consider obstacles to changing their pre-existing habits [4]. Despite the fact that educational programmes alone are often insufficient in order to achieve long-term changes and changes in habits, successful HH programmes must inevitably include an educational component [5].
According to The Guideline for Hand Hygiene in Health-Care Settings HCWs spend, on average, less than 15 seconds to perform HH and frequently fail to cover all areas of their hands and fingers [6]. In fact, even though the most common way to measure HCWs’ HH behaviour is the compliance rate (CR), defined as the number of HH episodes/ number of HH opportunities, it does not show the effectiveness of the used technique [7]. In fact, in addition to HH duration, several variables can affect HH efficacy, including the amount of liquid soap or alcohol-based handrub used, the HH agent chosen, and the wearing of rings or artificial fingernails. Inadequate HH can result in hands remaining contaminated and, eventually, in between-patient cross-transmission [8].
According to a large systematic review on the relative efficacy of interventions to promote HH among HCWs, most studies use direct observation to measure HH compliance, while others evaluate proxy measures such as HH event rate, HH product consumption, and an HH score checklist, and others report clinical outcomes [3]. Direct observation was revealed as the most common method to assess the impact of interventions to improve HCWs’ HH in a Cochrane review published in 2017 [9]. Nevertheless, new technologies can be adopted to electronically monitor HH, including ultraviolet (UV) fluorescent substances to detect the surface covered by HH products [10]. In this respect, Lehotsky et al. focused their work on HH technique, using an automated device to provide HCWs involved in the study with direct feedback on their performance. Participants rubbed their hands with an ultraviolet (UV)-labelled solution before having digital images of their hands taken under UV-A light, allowing them to identify areas that had been properly treated as those that shone brighter under UV light. They observed that repetitive practice with prompt objective feedback can increase HH adequacy, leading to a reduced rate of inadequate HH performance and fewer missed spots on the hands surfaces [11]. Afterwards the procedure was validated as a reliable training method [12]. In order to produce further evidence on this topic, this study used this UV automated device to assess the efficacy of an educational and training program on HH for HCWs in a second-level hospital in southern Italy.
METHODS
Setting and participants
The study was performed between November 2020 and February 2022 at the San Pio Hospital, a 544 beds hospital that serves a population of around 300,000 people and is located in Benevento, in Campania region, in the south Italy. HCWs from all departments were invited to participate through an official letter sent to all facility managers. For HCWs to be eligible to take part in this study, they had to fulfil all of the following inclusion criteria:
– Age range: participants aged 18 years and above.
– Occupation: individuals employed in any profession within the healthcare sector.
– Gender: both male and female participants.
– Departmental affiliation: HCWs from any department within the hospital setting.
Study design
A quasi-experimental research design was used. Participants constituted a single group and took part in the pre- and post-interventional phases. The pre-interventional phase, the training session and the post-interventional evaluation were all conducted by trainers who were not members of the research team.
Pre-interventional phase
After signing a legal declaration form and receiving a personal radiofrequency identification (RFID) card, participants were asked by the training team to rub their hands with an UV-labelled disinfectant solution. They were then identified using the RFID card and digital images of both sides of their hands were captured under UV-A light, using the Semmelweis Scanner™ by Hand-in-Scan, to record the distribution of the UV marker on the investigated surface. (Figure 1) The two cameras within the scanner conducted the scanning process and transmitted the image to the software for data processing and storage. The software also detected anomalies in the scan, such as the presence of rings and jewellery. A processed image was also sent to the built-in screen, displaying the mapping of the hands alongside the corresponding percentage of surface area covered by the rubbing actions with the marked solution. Areas properly treated with the solution showed green, while missed areas showed red (Figures 2 and Figure 3), so participants had the opportunity to visualize the outcome of their performance on the screen. On the same day, participants were trained on HH tools and techniques. This intervention was carried out immediately after the first scan in order to evaluate the operators’ basic knowledge of proper HH.
Figure 1.
Device used to record the distribution of the UV marker on the investigated surface.
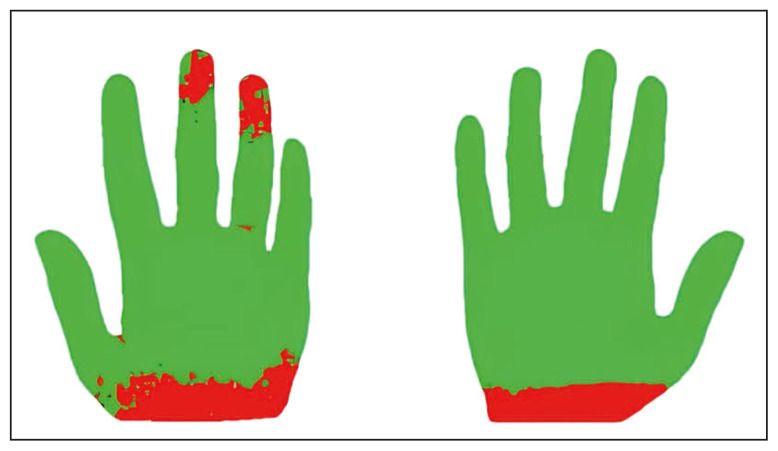
Figure 2.
An example of a processed image sent to the built-in screen that shows the solution distribution* on LP and RP.
* Areas properly treated with the solution are shown in green, missed areas are shown in red.
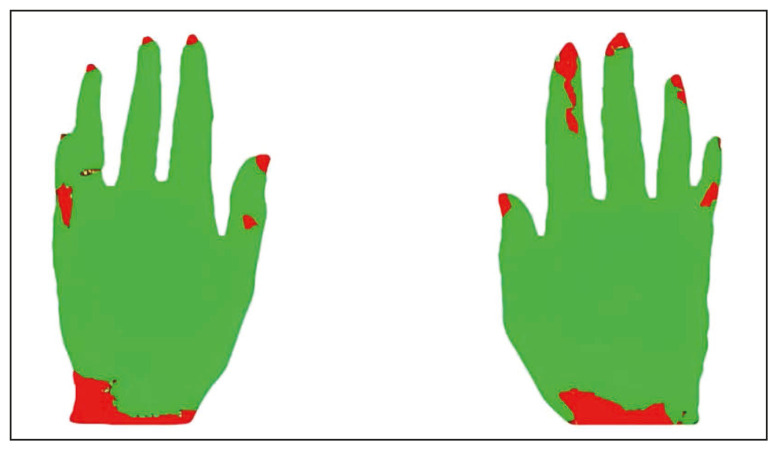
Figure 3.
An example of a processed image sent to the built-in screen that shows the solution distribution* on LD and RD.
* Areas properly treated with the solution are shown in green, missed areas are shown in red.
Post-interventional phase
Following the training, participants were asked to repeat the previously mentioned hands rubbing procedure and, once again, received visual feedback of the solution distribution on their hands, as well as immediate feedback from the trainers, who explained any errors in their HH technique.
Training intervention
The training intervention involved the dissemination of information about the fundamentals of HAIs, with an emphasis on proper HH procedures and other hygiene practices like isolation, the use of personal protective equipment, disinfection, etc. Specifically, the training session began with an overview of important behaviours related to HAI prevention. Afterwards, a video illustrating proper HH practices, as described in the WHO campaign “Clean Care is Safer Care”, was shown and explained by the instructors, two medical specialists in hygiene and preventive medicine and members of the hospital’s Committee for Healthcare-Associated Infections.
The device took four images for every participant, one of the palm and one of the back of each hand, and recorded the product distribution for each of them in terms of percentage of hand surface that was covered by the disinfectant solution.
Statistical analysis
The percentage of the hand surface that was covered in the UV-labelled disinfectant solution after each hand rubbing was used to measure HH performance. We also gathered qualitative information for each measurement; if the hand surface coverage met the threshold (95%), the procedure was recorded as “successful”, otherwise, it was recorded as “failed”. In order to describe the overall performance for each hands rubbing, participants whose hand surface coverage met the threshold on all four surfaces were considered successful.
The change in hands rubbing performance before and after the training interventions was assessed using the paired sample t-test for quantitative data and the McNemar test for paired dichotomous data. The analysis was performed on the whole study population and stratified by sex, profession, type of ward (COVID-19 or not). The significance level was set at 0.05 and the statistical analysis was executed with SPSS for Windows.
RESULTS
213 HCWs from 19 different departments - out of the hospital’s 1,232 total HCWs - participated on a voluntary basis.
Among the participants, 109 (51.2%) were women and 104 (48.8%) were men. They worked in different departments or services: 5 (2.3%) in the outpatient department, 21 in surgical units (9.9%), 139 (65.3%) in medical units, 24 (11.3%) in the emergency department, 10 (4.7%) in diagnostic services and 14 (6.6%) in other services such as the board of medical directors or the pharmaceutical service. 140 (65.7%) of them were used to work with patients suffering from COVID-19, in the so-called COVID-19 wards, at the time of study conduction. 129 (60.6%) were nurses and other non-physician health care professionals, 34 (16%) were physicians and 50 (23.5%) were classified as “others professionals”.
At the first measurement, only 87 HCWs (40.8%) achieved 95% hand surface coverage on the left palm (LP), while 102 HCWs (47.9%) achieved it on the right palm (RP), 86 (40.4%) on the left hand dorsum (LD), and 75 (35.2%) on the right hand dorsum (RD). Only 36 (16.9%) reached the 95% threshold on all four surfaces.
Only 197 participants (92.5%) underwent post-interventional measurement and were therefore considered for the analysis of change between the pre-interventional and the post-interventional phases. Among the 16 HCWs who did not undergo post-interventional measurement, 6 HCWs (37.5%) achieved 95% hand surface coverage on the left palm (LP), 8 HCWs (50%) achieved it on the right palm (RP), 3 (18.7%) on the left hand dorsum (LD), and 3 (18.7%) on the right hand dorsum (RD). 3 HCWs (18.7%) reached the 95% threshold on all four surfaces.
Following the training, both the mean coverage for each surface and the number of measurements that reached the 95% threshold increased significantly. Specifically, the mean coverage improved from 85.38 ± 19.88 to 94.83 ± 9.44 for the LP, from 83.55 ± 23.44 to 94.35 ± 11.12 for the RP, from 81.50 ± 25.66 to 92.84 ± 13.26 for the LD, and from 78.41 ± 26.63 to 92.25 ± 12.91 for the RD. Furthermore, the proportion of HCWs meeting the 95% threshold increased from 41.1% to 75.1% for the LP, from 47.7% to 73.1% for the RP, from 42.1% to 69.5% for the LD, and from 36.5% to 63.5% for the RD. The proportion of HCWs who met the 95% threshold across all four surfaces also increased significantly, from 16.8% to 48.7% (Table 1). Those measures increased significantly even in the subgroup analyses, with only two exceptions, namely LD successful procedures among other professionals and RD successful procedures among physicians. Table 2 reports the “successful on all surfaces” procedures in the different subgroups prior to and after the training intervention. As shown, in both females and males, there was a significant increase in in the proportion of HCWs who met the 95% threshold across all four surfaces. Likewise, a significant increase was observed in the two subgroups of HCWs who either worked or did not work in COVID-19 wards. Regarding the job role, all three subgroups (“Nurses and other non-physician HCWs”, “Physicians” and “Others”) showed a significant increase in terms of HCWs who reached the 95% threshold across all four surfaces.
Table 1.
Comparison of HH performance before and after the training intervention.
| Surface | Pre intervention | Post intervention | P a | P b | ||
|---|---|---|---|---|---|---|
| Mean coverage (%)±SD | Successful (N (%)) | Mean coverage (%)±SD | Successful (N (%)) | |||
| Left Palm (LP) | 85.38±19.88 | 81 (41.1%) | 94.83±9.44 | 148 (75.1%) | P<0.001 | P<0.001 |
| Right Palm (RP) | 83.55±23.44 | 94 (47.7%) | 94.35±11.12 | 144 (73.1%) | P<0.001 | P<0.001 |
| Left Dorsum (LD) | 81.50±25.66 | 83 (42.1%) | 92.84±13.26 | 137 (69.5%) | P<0.001 | P<0.001 |
| Right Dorsum (RD) | 78.41±26.63 | 72 (36.5%) | 92.25±12.91 | 125 (63.5%) | P<0.001 | P<0.001 |
| All surfaces (LP+RP+LD+RD) | – | 33 (16.8%) | – | 96 (48.7%) | – | P<0.001 |
Determined by paired samples t-test on mean coverage,
determined by McNemar test for paired dichotomous data (successful procedures).
Table 2.
Comparison of HH performance before and after the training intervention in different subgroups – All surfaces.
| Variable | Pre intervention | Post intervention | P b |
|---|---|---|---|
| Successful in All surfaces (N (%)) | Successful in All surfaces (N(%)) | ||
| Female (N=104) | 18 (17.3%) | 55 (52.9%) | P<0.001 |
| Male (N=93) | 15 (16.1%) | 41 (44.1%) | P<0.001 |
| Not working with Covid-19 patients (N=65) | 22 (33.8%) | 41 (63.1%) | P<0.001 |
| Working with Covid-19 patients (N=132) | 11 (8.3%) | 55 (41.7%) | P<0.001 |
| Nurses and other non-physician HCW (N=118) | 17 (14.4%) | 58 (49.2%) | P<0.001 |
| Physicians (N=34) | 4 (11.8%) | 13 (38.2%) | P=0.012 |
| Others (N=45) | 12 (26.7%) | 25 (55.6%) | P<0.001 |
Determined by McNemar test for paired dichotomous data (successful procedures).
DISCUSSION
Although prior studies assessed HH employing UV-labelled disinfectant solutions, most of them did not use them as part of intervention for increasing HCWs’ success in performing hands rubbing and did not rely on quantitative approaches. The findings of our study show that the training intervention was successful in improving HH. Secondly, they suggest that providing HCWs with immediate visual feedback on their performance could contribute to improve HH. This result was already reported by Lehotsky et al. and, more recently, by Dray et al., who observed that when an HH educational programme includes the use of supervised personal feedback with a fluorescent alcohol-based hand rub and UV light inspection system, HH completeness and compliance with WHO’s HH opportunities were significantly improved [11, 13].
Most studies investigating the efficacy of HH training programmes used different approaches to measure HCWs’ baseline compliance with HH (mainly qualitative or semiquantitative methods, such as direct observations) making comparisons with our findings difficult.
Though, Škodová et al. evaluated the quality of HH technique among HCWs in real conditions, without previous education or training, using an alcohol-based hand rub with a fluorescent marker to identify the product distribution: only 9.5% of participants actually achieved the highest rating [14]. Our results showed that 16.9% of the measurements recorded before the training session met the 95% threshold on all four surfaces; this slightly higher rating may be explained by the pandemic period in which our study was conducted.
According to Luangasanatip et al., both multifaceted HH intervention and single interventions (such as system change, training and education, or reminders alone) are associated with better compliance with HH among HCWs as compared to standard practice [3]. However, in respect to the objective evaluation of training programmes of HCWs on HH, as already reported in introduction, the evidence is poor and only a small number of studies’ protocols included UV-marked solutions. Widmer et al. designed an HH training programme in which HCWs put their hands under UV light after conducting HH with an alcohol-based hand rub that was UV-labelled but, in this case, the number of areas that had been cleaned adequately was determined in a semi-quantitative manner. In addition, they evaluated the degree of bacterial killing before and after the use of hand rub by finger imprint technique. Following the training, both the HCWs’ compliance to the recommended technique and the microbiological effectiveness of alcohol-based hand rub significantly increased [15]. Also Wiles et al. used a UV-labelled disinfectant solution during an experiential learning activity in a 41-bed emergency department, while changes in performance were evaluated by a 25-items pre-test/post-test survey concerning HH, HAI, standard precautions and transmission-based precautions, and the hospital’s audit tool routinely used by hospital staff to collect HH compliance data (auditors classify HH opportunities as soap and water or alcohol foam events and document whether the correct procedure was followed). After completing the learning activities, clinical staff knowledge of current CDC HH guidelines and overall HH compliance significantly improved when compared to baseline data. Additionally, increases in HH compliance were documented in tandem with the experiential learning activities [16].
The quantitative approach used in this study represents one of its strengths. In fact, the UV-dye based HH assessment method is a reliable indicator of correctly disinfected and pathogen-free areas on the hand surface, and UV-markers can accurately identify the hand surface areas that have been properly disinfected [12]. Furthermore, the bulk of studies on the subject employ less structured approaches to evaluate HH performance, such as direct observation, the evaluation of proxy measures, or the reporting of clinical outcomes [3]. Nevertheless, the study also presents some limitations. First of all, the enrolment of HCWs was voluntary and therefore a self-selection bias could not be ruled out. This means that findings could be optimistic in respect to other setting. Biased results could also be due to the time frame of the study that was performed during the COVID-19 pandemic when the attention toward hand hygiene was high. However, we should have likely expected a lower impact of the training intervention, because of a high proportion of HCWs meeting the 95% threshold before the intervention, but this was not the case. Eventually, HCWs’ awareness about the study objective could have led them to pay more attention to the HH procedure either pre and post-intervention. Unfortunately, this last limitation cannot be easily addressed when such a kind of interventions are tested. Another limit is the lack of long-term follow-up that prevent to conclude if the training programme could be effective in the long time horizon. A continuous monitoring could give further useful insights in understanding variations in time both in the success rate of HH procedures and the effectiveness of any intervention performed to implement them. Eventually, the study cannot disentangle the single contribution of the training intervention and of the use of UV-labelled disinfectant solution and automated device as they were used together. Nonetheless, in our opinion, all these aspects do not impair the findings on the relevant significant change in HH performance before and after the intervention.
CONCLUSIONS
Based on the results of this study, it can be concluded that the HH performance could be successfully increased among HCWs through the use of targeted device, such as UV based one, and the implementation of training initiatives. Therefore, the findings of the study could represent the evidence basis to use this combined approach in the educational training of HCWs albeit further studies, with longer follow up time, would be envisaged to understand how far results are generalizable to other contexts and how long efficacy could be maintained.
Footnotes
Authors contribution: C.d.W. and F.D. designed the study and coordinated the research activities. F.D. collected the data, and E.B. analysed them. E.B. wrote the manuscript, while G.D.S., D.D.S. and M.L. provided critical revisions and ensured the manuscript met all academic standards. All authors have approved the final version of the manuscript and are accountable for all aspects of the work.
Conflicts of interest: None to declare
Funding: This study did not receive any financial support or funding from external sources. The research was conducted independently.
REFERENCES
- 1.World Health Organization. Report on the burden of endemic health care-associated infection worldwide. 2011. [Accessed 07 March 2023]. Available at: https://apps.who.int/iris/handle/10665/80135.
- 2.World Health Organization. Evidence of hand hygiene as the building block for infection prevention and control. 2017. [Accessed 07 March 2023]. Available at: https://www.who.int/publications/i/item/WHO-HIS-SDS-2017.7.
- 3.Luangasanatip N, Hongsuwan M, Limmathurotsakul D, et al. Comparative efficacy of interventions to promote hand hygiene in hospital: systematic review and network meta-analysis. BMJ. 2015;351:h3728. doi: 10.1136/bmj.h3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitby M, Pessoa-Silva C, McLaws ML, et al. Behavioural considerations for hand hygiene practices: the basic building blocks. J Hosp Infect. 2007;65(1):1–8. doi: 10.1016/j.jhin.2006.09.026. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization; WHO Patient Safety, editor. WHO guidelines on hand hygiene in health care. 2009. [Accessed 07 March 2023]. Available at: https://iris.who.int/bitstream/handle/10665/44102/9789241597906_eng.pdf?sequence=1.
- 6.Boyce JD, Pittet D. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. [Accessed 07 March 2023];MMWR Morb Mortal Wkly Rep. 2002 51:1–45. Available at: https://archive-ouverte.unige.ch/unige:7119. [Google Scholar]
- 7.Haas J, Larson E. Measurement of compliance with hand hygiene. J Hosp Infect. 2007;66(1):6–14. doi: 10.1016/j.jhin.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 8.Pittet D, Allegranzi B, Sax H, et al. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis. 2006;6(10):641–652. doi: 10.1016/s1473-3099(06)70600-4. [DOI] [PubMed] [Google Scholar]
- 9.Gould DJ, Moralejo D, Drey N, et al. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev. 2017;9(9):CD005186. doi: 10.1002/14651858.CD005186.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang C, Jiang W, Yang K, et al. Electronic monitoring systems for hand hygiene: Systematic review of technology. J Med Internet Res. 2021;23(11):e27880. doi: 10.2196/27880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lehotsky Szilágyi L, Ferenci T, Kovács L, et al. Quantitative impact of direct, personal feedback on hand hygiene technique. J Hosp Infect. 2015;91(1):81–84. doi: 10.1016/j.jhin.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 12.Lehotsky Szilágyi L, Bánsághi S, Szerémy P, et al. Towards objective hand hygiene technique assessment: validation of the ultraviolet-dye-based hand-rubbing quality assessment procedure. J Hosp Infect. 2017;97(1):26–29. doi: 10.1016/j.jhin.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 13.Dray S, Lehingue S, Valera S, et al. Using an ultraviolet cabinet improves compliance with the World Health Organization’s hand hygiene recommendations by undergraduate medical students: a randomized controlled trial. Antimicrob Resist Infect Control. 2020;9(1):147. doi: 10.1186/s13756-020-00808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Škodová M, García Urra F, Gimeno Benítez A, et al. Hand hygiene assessment in the workplace using a UV lamp. Am J Infect Control. 2015;43(12):1360–1362. doi: 10.1016/j.ajic.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 15.Widmer AF, Conzelmann M, Tomic M, et al. Introducing Alcohol-Based Hand Rub for Hand Hygiene: The Critical Need for Training. Infect Control Hosp Epidemiol. 2007;28(1):50–54. doi: 10.1086/510788. [DOI] [PubMed] [Google Scholar]
- 16.Wiles LL, Roberts C, Schmidt K. Keep It Clean: A Visual Approach to Reinforce Hand Hygiene Compliance in the Emergency Department. J Emerg Nurs. 2015;41(2):119–124. doi: 10.1016/j.jen.2014.11.012. [DOI] [PubMed] [Google Scholar]