Abstract
Background
In the aftermath of the World Trade Center (WTC) attack on 11 September 2001, rescue and recovery workers faced hazardous conditions and toxic agents. Prior research linked these exposures to adverse health effects, but mainly examined individual factors, overlooking complex mixture effects.
Methods
This study applies an exposomic approach encompassing the totality of responders’ experience, defined as the WTC exposome. We analyzed data from 34,096 members of the WTC Health Program General Responder, including mental and physical health, occupational history, traumatic and environmental exposures using generalized weighted quantile sum regression.
Results
We find a statistically significant association between the exposure mixture index and all investigated health outcomes. Factors identified as risk factors include working in an enclosed heavily contaminated area, construction occupation, and exposure to blood and body fluids. Conversely, full-time employment emerged as a protective factor.
Conclusions
This exposomics study emphasizes the importance of considering combined exposures for the identification of harmful and protective factors within the WTC exposome, providing valuable insights for targeted interventions and preventive measures. In an era marked by more frequent and severe natural disasters due to the evolving climate crisis, the exposomic framework is a promising tool for disaster preparedness.
Subject terms: Diseases, Health care
Plain language summary
After the 9/11 World Trade Center attacks, rescue and recovery workers were exposed to many harmful substances and hazardous conditions. We assessed all aspects of these exposures and compared these with responders’ health and work history. We found that exposure to harmful substances and hazardous conditions was associated with all investigated health problems. Working in contaminated areas, in construction, or with blood and body fluids increased health risks. However, being employed full-time seemed to protect against some health issues. This research highlights the need to consider all things that rescue and recovery workers are exposed to during disasters to better understand and prevent health problems during and after future events.
Rechtman et al. analyse the exposome of rescue and recovery workers who attended the World Trade Center on and after September 11, 2001. Mental and physical health outcomes associate with all aspects of occupational history, as well as traumatic and environmental exposures.
Introduction
The World Trade Center (WTC) rescue and recovery responders were exposed to a complex mixture of smoke, dust, and debris generated by the collapse and long-lasting fires of the WTC buildings on 11 September, 2001. In addition to exposure to chemicals, responders were exposed to traumatic psychosocial stressors, including fear for personal safety, injury, or illness, and working long hours and performing arduous work in chaotic conditions1. These exposures have been linked to increased risk for adverse health outcomes, including respiratory2–5, metabolic6, neurologic7, and mental health disorders8–11 Despite clear associations between responders’ experience and health outcomes, no studies have comprehensively examined the overall effect of the mixture of exposures that may have increased the risk for disease or promoted resilience against developing disease. Here, we apply an exposomics approach, combining chemical and non-chemical exposures with baseline (post-9/11) health and sociodemographic status, to encompass the variety of responders’ experiences during the rescue and recovery efforts. We refer to this concept as the WTC exposome.
Although several studies have attempted to identify risk factors associated with the onset and development of WTC-related diseases, most focus on individual factors selected a priori and use traditional regression approaches to examine associations between those individual factors (e.g., when started on the effort, work duration, previous respiratory symptoms, previous mental health symptoms, sociodemographic characteristics) and health outcomes12–17. However, at the time of 9/11 and in the months following the attacks, WTC responders were simultaneously exposed to a varying mixture of factors, rather than to one factor at a time. A growing body of literature suggests that co-exposure may influence the toxicity of individual factors. Under joint exposure, different factors may interact to cause synergistic or antagonistic effects18. One approach proposed to better capture responders’ exposure was to group responders into exposure categories. For example, Wisnivesky et al.17 categorized exposure into very high, high, intermediate, and low16 groups, based on three self-reported experiences (total time at the site, being caught in the dust cloud, and work on the pile arising from the collapse of the towers). While this approach helped link WTC exposure with increased risk of disease outcomes, it could not (nor claimed to) identify specific factors. As such, it does not provide information on the mixture’s overall impact or individual factors within the mixture that may increase or decrease the risk for adverse health effects.
The exposome, defined by C. Wild in 2005, is the totality of individuals’ exposure experience from conception until death and has been proposed to be critical for disease etiology19. The exposome can include toxicants, nutrients, drugs, microbiome metabolites, physical and psychosocial stress, lifestyle choices, and socioeconomic status. The increased recognition of the significant role that nongenetic factors play in disease has led to increased efforts to comprehensively characterize the exposome at a scale similar to that of the human genome20. The exposome concept offers a data-driven approach to investigating the environmental causes of disease and can indicate a unique exposure profile, rendering individuals more or less susceptible to the effects of stressors in their environment21. Critical to this concept is that an individual’s “exposome” contains both risk and protective factors. In the context of the WTC responders, understanding the health effects of different combinations of exposures is important for identifying at-risk responders, as well as protective factors that may guide the development of appropriate interventions.
In this study, we adopt an exposomic-based, data-driven approach to systematically examine associations between WTC responders’ experience on 9/11 and during the rescue and recovery effort, and the risk of adverse health outcomes in 34,096 responders enrolled in the CDC/NIOSH World Trade Center Health Program General Responder Cohort (GRC). We define the “WTC exposome” to be the mixture of WTC-related experience, mental and physical health status, current/prior occupation, traumatic and environmental exposures, socioeconomic status, and social support during the work on the rescue and recovery effort. We find a statistically significant association between the WTC exposome and all investigated health outcomes (i.e., post-traumatic stress disorder; PTSD, gastroesophageal reflux disease; GERD, respiratory conditions, diabetes, and headaches) and identify risk and protective factors. This exposomics study emphasizes the importance of considering combined exposures for the identification of harmful and protective factors within the WTC exposome, providing valuable insights for targeted interventions and preventive measures.
Methods
Study design and participants
This study includes 34,096 enrollees of the World Trade Center Health Program (WTCHP) GRC who (1) consented to have their data aggregated for research purposes, (2) had an Exposure assessment questionnaire (EAQ) record, and (3) had mental health diagnostic interview. The GRC has been described in detail by Dasaro et al.22. Briefly, participants were monitored at any of the seven CDC/NIOSH-funded Clinical Centers of Excellence (CCE) and completed an initial ‘baseline’ visit. All members worked or volunteered on WTC rescue and recovery efforts following the 9/11 attack on the WTC towers, meeting at least one of the following criteria: (i) involved for ≥4 h from September 11 to September 14, 2001, or ≥24 h in September 2001, or ≥80 h from September 11 to July 2002; (ii) member of the Office of the Chief Medical Examiner for New York City, handling and processing human remains for ≥4 h; (iii) worked for the Port Authority Trans Hudson Corporation (PATH), cleaning PATH tunnels for ≥24 h between February 2002 and July 2002. At the baseline visit, responders completed self- and interviewer-administered questionnaires. These instruments collected information on sociodemographic characteristics, exposure history, medical conditions, and mental health symptoms22. Physical examinations, clinical chemistry laboratory tests, and pulmonary function tests (PFTs) were also performed. Questionnaires used for this study are summarized in supplementary Table 1. For responders who were minors during the rescue and recovery efforts, consent was obtained at enrollment, with a minimum age of 20 at the first visit, as shown in Table 1. This study was approved by the Institutional Review Board of the Icahn School of Medicine at Mount Sinai (STUDY-19-01072).
Table 1.
Sociodemographic characteristics of participants included in the study
| WTCHP-GRC participants (N = 34,096) | |
|---|---|
| Age at 09/11/2001 (years) [range] | 38 [13.0, 78.0] |
| Age at first visit (years) [range] | 45 [20.0, 89.0] |
| Gender | |
| Female | 4566 (13.4%) |
| Male | 29487 (86.6%) |
| Race | |
| American Indian and Alaskan Native | 86 (0.3%) |
| Asian | 390 (1.1%) |
| Black or African American | 3126 (9.2%) |
| Multi-Racial | 3845 (11.3%) |
| Pacific Islander | 38 (0.1%) |
| White or Caucasian | 19186 (56.3%) |
| Unknown | 7382 (21.7%) |
| Ethnicity | |
| Hispanic | 6179 (23.4%) |
| Non-Hispanic | 20262 (76.6%) |
| Education | |
| Less than a high school diploma | 2253 (6.9%) |
| High school or equivalent | 6764 (20.8%) |
| College degree (or some college) | 20747(63.8%) |
| Graduate degree | 2780 (8.5%) |
WTCHP-GRC World Trade Center Health Program–General Responder Cohort.
WTC-related health outcomes
For our outcomes, we selected WTC-certified health conditions and non-certifiable conditions. The WTCHP uses a certification mechanism to provide medically necessary treatment to responders. WTC health conditions are determined by the designated CCE or National Provider Network (NPN) physician during the baseline health evaluation, a monitoring visit, or a treatment visit23. To diagnose a WTCHP member with a health condition, evidence collected from the member’s visits is used to justify certification of a condition. A combination of medical history, physical examination, present symptoms, exposure assessment and other questionnaires (summarized in supplementary Table 1), and diagnostic testing (e.g., PFTs, imaging, chemical laboratory tests) are used to arrive at diagnoses. The Diagnostic Interview Schedule (DIS) is administered to every responder at the second visit and assesses psychological trauma, PTSD, depression and alcohol consumption. The temporal relationship between the onset of symptoms of a condition and WTC exposures is also considered24. For the program to certify a condition, the following criteria need to be met: (i) the health condition is included on the List of WTC-Related Health Conditions; (ii) exposures present during WTC rescue and recovery efforts play a significant role in aggravating, causing or contributing to the physical and mental condition exhibited by the responder during their clinical evaluation. Certified conditions are categorized into the care suites: acute traumatic injuries, airway and digestive disorders, cancers, mental health conditions, and musculoskeletal disorders. Respiratory outcomes are specified as an indicator of certification for conditions in the obstructive airway disease (OAD) and upper respiratory disease (URD) care suites. The most common certifications under this outcome include Asthma, Chronic obstructive pulmonary disease, chronic rhinitis, Chronic pharyngitis, and Chronic sinusitis. Responders certified for any condition within a care suite do not need further certification to receive treatment for other conditions within the same care suite4. Non-certified conditions are WTC-related health problems that do not meet the criteria described above. Some of these outcomes can be described as potential WTC-related diseases as research about their associations with WTC exposures is ongoing. Examples of these potential conditions include late-onset diabetes and headaches6,22.
Statistics and reproducibility
Data preparation
From 239 variables gathered from the baseline surveillance dataset, we generated univariate summary statistics and examined distributions. To standardize all exposure data, we recoded each of the variables as a binary indicator (0/1) where zero indicated not present and one indicated present. Only items occurring in 10% to 90% of responders were included in further analyses, resulting in the selection of 84 factors. Covariates that are known predictors of health or strong potential confounders included a priori in the models, based on biological plausibility, were gender, age at the time of 9/11, and race (self-reported by participants at enrollment). The term ‘race’ is socially constructed and was used as a proxy for racism to measure inequity along the lines of ‘race’, which has been shown to have biological and physiological consequences.
Generalized weighted quantile sum regression
To comprehensively investigate how the WTC baseline exposome is associated with each health outcome (PTSD, GERD, respiratory problems, diabetes, and headaches), we used logistic generalized weighted quantile sum (gWQS) regression. The gWQS has been described in detail in Carrico et al.25. In brief, the gWQS is a mixtures-based ensemble modeling strategy that tests for associations between the combined effect of multiple exposures and an outcome of interest. It estimates a weighted index of all factors and performs inference on the regression coefficient that characterizes the association between the outcome and this weighted index. gWQS randomly splits the initial dataset into training and validation sets (i.e., 40% vs. 60%). In the training set, gWQS constructs a weighted additive index (Σj = 1[wjqij]) of all factors previously ranked in quantiles (qij). To facilitate the implementation and interpretation of the gWQS approach, all factors are harmonized to have a standard scale before ranking them. Each weight (wj) is mapped to an individual factor (j) of the mixture, and the mixture is constrained to be positive or negative. Additionally, all weights are constrained to sum to one, enabling sorting by relative importance. Factors that impact the association between the mixture index and the outcome have larger weights; factors with little or no impact have near-zero weights. To reduce the high correlation between factors and have more accurate and variable weight estimates, gWQS employs a bootstrap approach, randomly selecting samples from the training set. Here, a total of 10,000 bootstrap samples were generated from the training data to estimate the WQS index weights, and the effect of the index was assessed for statistical significance (p < 0.05) in the validation set. Thus, the test for the significance of β1 was based on independent data. WQS models were implemented in R (v4.0.2) with the gWQS package.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Demographics
Sociodemographic characteristics are reported in Table 1. Participants’ mean age was 38 years on 9/11/2001 and 45 years at the time of their first WTCHP visit. Participants included in this study are primarily male (86.6%), White (56.3%), and non-Hispanic (76.6%). College Degree education was most common (63.8%), followed by High school or equivalent (20.8%).
WTC-related health conditions
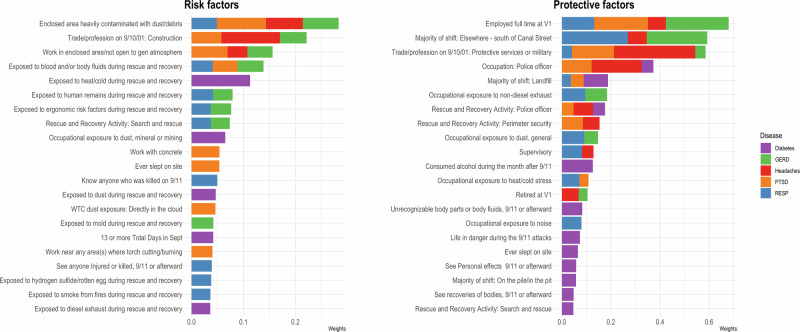
Frequencies of WTC-related physical or mental health conditions investigated in this study are reported in Table 2. Among the 34,096 responders included in this study, the most common health conditions were headaches (60%), respiratory disease (RESP) (46%), and gastroesophageal reflux disease (GERD) (34%). Diabetes was diagnosed in 17% of participants, and PTSD was diagnosed in 10%. The co-occurrence of WTC-related health conditions is reported in Fig. 1. The most common health condition is headaches alone (n = 6581). The most common subset of health conditions is the combination of GERD, RESP, and headaches (n = 4778). The next most common combination is RESP and headaches (n = 2487), followed by RESP alone (n = 1610).
Table 2.
Frequencies of World Trade Center (WTC)-related physical or mental health conditions investigated in this study (N = 34,096)
| Overall (N = 34,096) | |
|---|---|
| PTSD | |
| No | 30724 (90.1%) |
| Yes | 3372 (9.9%) |
| Diabetes | |
| No | 28208 (82.7%) |
| Yes | 5888 (17.3%) |
| GERD | |
| No | 22458 (65.9%) |
| Yes | 11638 (34.1%) |
| Respiratory | |
| No | 18360 (53.8%) |
| Yes | 15736 (46.2%) |
| Headaches | |
| No | 13684 (40.1%) |
| Yes | 20412 (59.9%) |
PTSD post-traumatic stress disorder, GERD gastroesophageal reflux disease, respiratory includes obstructive airway disease (OAD) and upper respiratory disease (URD).
Fig. 1.
An UpSet plot showing the co-occurrence> of World Trade Center (WTC)-related health conditions as a set of intersections in a matrix layout among participants included in this study (n = 34,096). Each row corresponds to a disease, and each column corresponds to a possible intersection of diseases. The filled-in cells show which set is part of an intersection and the bar charts on top show the size of the set. PTSD post-traumatic stress disorder, GERD gastroesophageal reflux disease, RESP Respiratory disease.
World Trade Center exposome and related health outcomes
Results from the gWQS regression analysis show a significant association between the WTC exposome and all investigated health outcomes in both the positive direction (i.e., factors associated with an increased likelihood of health outcomes; risk factors) and the negative direction (i.e., factors associated with a decreased likelihood of health outcomes; protective factors). Estimates reported as odds ratio, 95% confidence intervals, and p values for each model are reported in Table 3.
Table 3.
Results from generalized weighted quantile sum (gWQS) regression analyses among 34,096 World Trade Center (WTC) responders included in this study
| Outcome | Direction | Estimate | CI (95%) | P value |
|---|---|---|---|---|
| PTSD | Risk factors | 6.4 | 4.8−8.4 | <2e-16*** |
| Protective factors | 0.13 | 0.11−0.17 | <2e-16*** | |
| Diabetes | Risk factors | 1.57 | 1.25–1.97 | 0.00011*** |
| Protective factors | 0.71 | 0.59–0.85 | 0.00014*** | |
| OAD | Risk factors | 4.49 | 3.73–5.40 | <2e-16*** |
| Protective factors | 0.37 | 0.31–0.44 | <2e-16*** | |
| GERD | Risk factors | 4.36 | 3.66–5.19 | <2e-16*** |
| Protective factors | 0.46 | 0.39–0.54 | <2e-16*** | |
| URD | Risk factors | 3.87 | 3.31–4.52 | <2e-16*** |
| Protective factors | 0.66 | 0.56–0.78 | 6.17e-07*** | |
| RESP | Risk factors | 3.86 | 3.32–4.49 | <2e-16*** |
| Protective factors | 0.59 | 0.51–0.70 | 1.21e-10*** | |
| Headaches | Risk factors | 5.57 | 4.68–6.64 | <2e-16*** |
| Protective factors | 0.32 | 0.29–0.36 | <2e-16*** |
For each health condition, associations between the WTC exposome and outcomes were modeled in the positive (risk factors) and the negative (protective factors) directions.
Estimates are reported as odds ratio. CI confidence interval, PTSD post-traumatic stress disorder, GERD gastroesophageal reflux disease, RESP respiratory disease. *** Indicates p < 0.001.
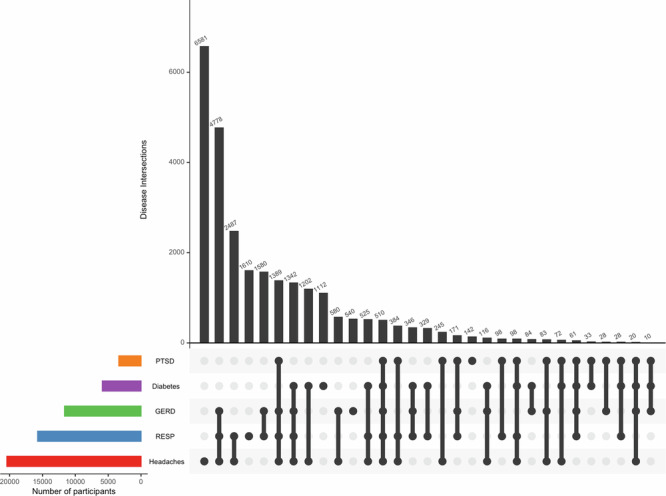
Risk and protective factors
Weights from gWQS models are shown in Fig. 2. The main risk factors for WTC-related health conditions include working in an enclosed area heavily contaminated with dust/debris, construction occupation before 9/11/01, working in an area/not open to the general atmosphere, exposure to blood and body fluids, heat/cold, human remains, and ergonomic risk factors during rescue and recovery efforts, performing search and rescue activities, and occupational exposure to dust, mineral or mining. The main protective factors for WTC-related health conditions include being employed full-time at the first WTCHP visit, performing the majority of shift south of Canal Street26 but neither on the pile nor in the pit; protective services or military occupation before 9/11/01, and police officer occupation on 9/11. Detailed exposure profiles as they relate to increased and decreased associations for each specific WTC-related health outcome are shown in Supplementary Fig. 1.
Fig. 2.
Weights from generalized weighted quantile sum (gWQS) regression analyses among 34,096 responders included in this study. Bar plots represent estimated weights for each mixture component in the WQS regressions. Weights are color-coded to indicate health outcomes PTSD post-traumatic stress disorder, GERD gastroesophageal reflux disease, RESP respiratory disease.
Post-traumatic stress disorder
Working in an enclosed area heavily contaminated with dust/debris, working in an area not open to the general atmosphere, construction occupation before 9/11/01, working with concrete, and sleeping on site contributed most to the harmful effect of the WTC exposure to PTSD. In contrast, being employed full-time at the first WTCHP visit, protective services or military occupation before 9/11/01, and police officer occupation at 9/11 contributed most to the protective effect of the WTC exposome on PTSD.
Gastroesophageal reflux disease
Working in an enclosed area heavily contaminated with dust/debris, construction occupation before 9/11/01, and being exposed to blood and body fluids during rescue and recovery efforts contributed most to the harmful effect of the WTC exposome on GERD. In contrast, WTC responders who reported full-time employment at the first WTCHP visit and performing the majority of the shift elsewhere (south of Canal Street) experienced less GERD.
Respiratory diseases
Knowing anyone who was killed on 9/11, working in an enclosed area heavily contaminated with dust/debris, and being exposed to human remains during rescue and recovery contributed most to the harmful effect of the WTC exposome on respiratory diseases. Performing the majority of shift elsewhere (south of Canal Street), and being employed full-time at the first WTCHP visit contributed most to the protective effect of the WTC exposome on respiratory outcomes.
Diabetes
Being exposed to heat/cold during rescue and recovery efforts, occupational exposure to dust, minerals, or mining, and being exposed to dust during rescue and recovery working contributed most to the harmful effect of the WTC exposome on diabetes, while reporting consumed alcohol during the month after 9/11, and performing the majority of shift at landfill contributed most to the protective effect of the WTC exposome.
Headaches
Construction occupation before 9/11/01, working in an enclosed area heavily contaminated with dust/debris, and working in an area not open to the general atmosphere contributed most to the harmful effect of the WTC exposome, while protective services or military occupation before 9/11/01, and police officer occupation at 9/11 contributed most to the protective effect of the WTC exposome.
Discussion
In this study, we applied an exposomic approach to systematically examine associations between World Trade Center (WTC) Responders’ experience and selected health outcomes. As reported previously, 9/11 WTC responders continue to have a substantial burden of physical and mental health problems17. Compared to the general population, participants in this study exhibit a higher prevalence of the investigated health outcomes: headaches (60% vs. 15%27), respiratory symptoms (46% vs. 6–7%28,29), GERD (34% vs. 18–28%30), diabetes (17% vs. 11.6%31), and PTSD (10% vs. 6.8%32). By considering all recorded exposures, both chemical and non-chemical, along with baseline (post-9/11) health and sociodemographic status, we captured the complexity of the WTC exposome and its effect on the long-term health of responders. Our findings demonstrate a significant overall mixture effect of the WTC exposome on investigated health outcomes (PTSD, GERD, respiratory conditions, diabetes, and headaches), as well as the identification of risk and protective factors associated with the likelihood of adverse health outcomes.
Our exposomic approach revealed specific factors that contributed most to the harmful effects of the WTC exposome on health. The most prominent risk factor identified was working in enclosed areas heavily contaminated with dust and debris. This finding is consistent with prior research indicating that inhalation of the dust from the collapses during the rescue and recovery operations is the main cause of respiratory injuries17,33 and GERD3 in responders and was also found to be associated with chronic PTSD symptoms34. Interestingly, factors associated with the total duration or frequency of work (i.e., Number of days per month), being caught in the dust cloud, month work started on the effort, and the majority of the shift spent on the pile- all exhibited a comparatively modest impact on the overall outcome. Prior occupational exposure to dust, noise, diesel exhaust, heat/cold, gasoline, and welding fumes was not determined to significantly contribute to the overall effect, highlighting the notion that mere occupational involvement in hazardous conditions may not be the most significant factor in driving adverse health outcomes. Instead, they emphasize the critical importance of equipping responders with appropriate respiratory protection and prompting its utilization during disaster response efforts.
Other salient risk factors that have emerged relate to psychological trauma experienced during the rescue and recovery, including exposure to blood, bodily fluids, and human remains. These findings highlight the importance of preserving and strengthening the mental health support and resources offered to responders through the WTCHP. This involves early intervention initiatives, comprehensive support programs, routine mental health screenings, as well as the implementation of employer policies designed to promote overall resilience.
Importantly, our approach also identified factors within the WTC exposome that exhibited a protective effect against adverse health outcomes. Among these factors, being employed full-time at the first visit to the WTCHP and not working on the pile nor in the pit, were associated with a reduced likelihood of developing health conditions. These findings may be related to a “Healthy worker” effect, a phenomenon observed in occupational health studies where employed individuals tend to exhibit better health outcomes35. This effect occurs because people who are healthier and more physically able are more likely to remain in the workforce, while those with health issues may exit the workforce. Other identified factors associated with a decreased likelihood of disease, specifically those related to neurological health (PTSD and headaches), include being a police officer or military. These findings may be related to prior training and exposure to similar stressors. Another explanation is that the protective effect we detect may result from report bias due to underreported mental health concerns among police and military personnel. Rates of mental health reports remain disproportionately low within these populations due to fear of professional consequences and stigmas surrounding mental health17.
The use of an exposomics approach in this study has several strengths. By considering a wide range of exposures and their interactions, the study provides a more complete understanding of the complex mixture of factors that responders were exposed to during the WTC rescue and recovery efforts. The WQS regression analysis identified harmful and protective factors within the WTC exposome, providing valuable insights for targeted interventions and preventive measures. For example, our identification of the link between exposure to extreme temperatures and the development of diabetes can inform the creation of surveillance programs and dietary recommendations aimed at protecting the most vulnerable responders. Importantly, our approach ensures that these interventions target risk factors as part of a mixture, recognizing that WTC responders were exposed to a varying combination of factors simultaneously and that co-exposure can influence the toxicity of individual elements.
When interpreting the results of this study, some limitations should be considered. The study relied on self-reported information and retrospective data, which may be subject to recall bias. Additionally, while the gWQS regression analysis accounted for potential confounders and estimated the association between the weighted index and health outcomes, causality cannot be established due to the study’s observational nature. Further research is needed to confirm these findings, including leveraging longitudinal data collected under the WTCHP.
In conclusion, this study contributes to our understanding of the health effects of the WTC exposome on responders and may guide policy and regulatory decision-making regarding responders’ health preparedness in the event of future disasters. By adopting an exposomics approach, the study provides valuable insights into the specific exposome factors associated with an increased or decreased risk of adverse health outcomes. These findings may inform the development of targeted interventions and support the well-being of WTC responders.
Supplementary information
Description of Additional Supplementary Files
Acknowledgements
Funding was provided by the National Institute for Occupational Safety & Health (NIOSH) grant number U01 OH012075, and the National Institute of Environmental Health Sciences (NIEHS) grant number K99ES035120 and P30ES023515. Data were provided by the WTC Health Program General Responder Data Center at Mount Sinai (CDC/NIOSH contracts 200-2017-93325 and 75D30122C15187).
Author contributions
E.R. and M.K.H. conceptualized the study and E.R. drafted the manuscript. E.R. conducted all analyses with statistical support from E.C. and C.J.H., and M.K.H., M.R., A.I., C.R.D., S.L.T., and A.C.T. provided feedback on design and analysis. E.N. and C.J.H. ingested WTCHP-GRC data, recorded exposures, and conducted sensitivity analyses. All authors reviewed and approved the manuscript.
Peer review
Peer review information
Communications Medicine thanks Jennifer Cavallari, Mary Fox and the other, anonymous, reviewer for their contribution to the peer review of this work.
Data availability
Anonymised data and supporting documents are available upon request from the General Responder Data Center of the WTCHP via christopher.dasaro@mssm.edu. A Data Transfer and Use Agreement and IRB approval is required before the data release. The numerical data (source data) plotted in Fig. 1 is available in Supplementary Data 1. The numerical data (source data) plotted in Fig. 2 is available in Supplementary Data 2 and 3.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s43856-024-00683-9.
References
- 1.Landrigan, P. J. et al. Health and environmental consequences of the World Trade Center disaster. Environ. Health Perspect.112, 731–739 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aldrich, T. K. et al. Lung function in rescue workers at the world trade center after 7 years. N. Engl. J. Med.362, 1263–1272 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cleven, K. L. et al. Twenty-year reflection on the impact of world trade center exposure on pulmonary outcomes in fire department of the city of new york (FDNY) rescue and recovery workers. Lung199, 569–578 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herbert, R. et al. The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ. Health Perspect.114, 1853–1858 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tao, X. G. et al. The world trade center clean up and recovery worker cohort study: respiratory health amongst cleanup workers approximately 20 months after initial exposure at the disaster site. J. Occup. Environ. Med.49, 1063–1072 (2007). [DOI] [PubMed] [Google Scholar]
- 6.Miller-Archie, S. A. et al. Posttraumatic stress disorder and new-onset diabetes among adult survivors of the World Trade Center disaster. Prev. Med.66, 34–38 (2014). [DOI] [PubMed] [Google Scholar]
- 7.Brackbill, R. M. et al. Surveillance for World Trade Center disaster health effects among survivors of collapsed and damaged buildings. MMWR Surveill. Summ.55, 1–18 (2006). [PubMed] [Google Scholar]
- 8.Perrin, M. A. et al. Differences in PTSD prevalence and associated risk factors among World Trade Center disaster rescue and recovery workers. Am. J. Psychiatry164, 1385–1394 (2007). [DOI] [PubMed] [Google Scholar]
- 9.Yip, J. et al. World Trade Center-related physical and mental health burden among New York City Fire Department emergency medical service workers. Occup. Environ. Med.73, 13–20 (2016). [DOI] [PubMed] [Google Scholar]
- 10.Jordan, H. T. et al. Persistent mental and physical health impact of exposure to the September 11, 2001 World Trade Center terrorist attacks. Environ. Health18, 12 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu, B., Tarigan, L. H., Bromet, E. J. & Kim, H. World trade center disaster exposure-related probable posttraumatic stress disorder among responders and civilians: a meta-analysis. PLoS One9, e101491 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brackbill, R. M. et al. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the world trade center terrorist attack. JAMA302, 502–516 (2009). [DOI] [PubMed] [Google Scholar]
- 13.Alper, H. E., Yu, S., Stellman, S. D. & Brackbill, R. M. Injury, intense dust exposure, and chronic disease among survivors of the World Trade Center terrorist attacks of September 11, 2001. Inj. Epidemiol.4, 17 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kotov, R. et al. Posttraumatic stress disorder and the risk of respiratory problems in World Trade Center responders: longitudinal test of a pathway. Psychosom. Med.77, 438–448 (2015). [DOI] [PubMed] [Google Scholar]
- 15.Pietrzak, R. H. et al. Trajectories of PTSD risk and resilience in World Trade Center responders: an 8-year prospective cohort study. Psychol. Med.44, 205–219 (2014). [DOI] [PubMed] [Google Scholar]
- 16.Webber, M. P. et al. Prevalence and incidence of high risk for obstructive sleep apnea in World Trade Center-exposed rescue/recovery workers. Sleep. Breath.15, 283–294 (2011). [DOI] [PubMed] [Google Scholar]
- 17.Wisnivesky, J. P. et al. Persistence of multiple illnesses in World Trade Center rescue and recovery workers: a cohort study. Lancet378, 888–897 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanders, A. P., Claus Henn, B. & Wright, R. O. Perinatal and childhood exposure to cadmium, manganese, and metal mixtures and effects on cognition and behavior: a review of recent literature. Curr. Environ. Health Rep.2, 284–294 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wild, C. P. Complementing the genome with an ‘exposome’: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol. Biomark. Prev.14, 1847–1850 (2005). [DOI] [PubMed] [Google Scholar]
- 20.Vermeulen, R., Schymanski, E. L., Barabási, A.-L. & Miller, G. W. The exposome and health: where chemistry meets biology. Science367, 392–396 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vineis, P. et al. What is new in the exposome? Environ. Int.143, 105887 (2020). [DOI] [PubMed] [Google Scholar]
- 22.Dasaro, C. R. et al. Cohort profile: world trade center health program general responder cohort. Int. J. Epidemiol.46, e9 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Administrative Manual—WTC Health Program. https://www.cdc.gov/wtc/ppm.html#certification_physician (2014).
- 24.Centers for Disease Control and Prevention (CDC), Department of Health and Human Services (HHS). World Trade Center Health Program; amendments to list of WTC-related health conditions; cancer; revision. Interim final rule. Fed. Regist.79, 9100–9117 (2014). [PubMed] [Google Scholar]
- 25.Carrico, C., Gennings, C., Wheeler, D. C. & Factor-Litvak, P. Characterization of weighted quantile sum regression for highly correlated data in a risk analysis setting. J. Agric Biol. Environ. Stat.20, 100–120 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NYC disaster area and WTC responder eligibility maps. https://www.cdc.gov/wtc/define.html (2021).
- 27.Burch, R., Rizzoli, P. & Loder, E. The prevalence and impact of migraine and severe headache in the United States: figures and trends from government health studies. Headache58, 496–505 (2018). [DOI] [PubMed] [Google Scholar]
- 28.Liu, Y., Carlson, S. A., Watson, K. B., Xu, F. & Greenlund, K. J. Trends in the prevalence of chronic obstructive pulmonary disease among adults aged ≥18 years — United States, 2011–2021. MMWR Morb. Mortal. Wkly Rep.72, 1250–1256 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silins, I. & Högberg, J. Combined toxic exposures and human health: biomarkers of exposure and effect. Int. J. Environ. Res. Public Health8, 629–647 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Antunes, C., Aleem, A. & Curtis, S. A. Gastroesophageal reflux disease. In: StatPearls (StatPearls Publishing, Treasure Island (FL), 2024). [PubMed]
- 31.Diabetes Statistics - NIDDK. National institute of diabetes and digestive and kidney diseases, https://www.niddk.nih.gov/health-information/health-statistics/diabetes-statistics.
- 32.Post-Traumatic Stress Disorder (PTSD) - National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/statistics/post-traumatic-stress-disorder-ptsd.
- 33.Lippmann, M., Cohen, M. D. & Chen, L.-C. Health effects of World Trade Center (WTC) dust: an unprecedented disaster with inadequate risk management. Crit. Rev. Toxicol.45, 492–530 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang, Y., Rosen, R., Reibman, J. & Shao, Y. Posttraumatic stress disorder mediates the association between traumatic world trade center dust cloud exposure and ongoing systemic inflammation in community members. Int. J. Environ. Res. Public Health19, 8622 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chowdhury, R., Shah, D. & Payal, A. R. Healthy worker effect phenomenon: revisited with emphasis on statistical methods–a review. Indian J. Occup. Environ. Med.21, 2–8 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
Anonymised data and supporting documents are available upon request from the General Responder Data Center of the WTCHP via christopher.dasaro@mssm.edu. A Data Transfer and Use Agreement and IRB approval is required before the data release. The numerical data (source data) plotted in Fig. 1 is available in Supplementary Data 1. The numerical data (source data) plotted in Fig. 2 is available in Supplementary Data 2 and 3.