Abstract
Background
The study explores the impact of microleakage on bracket (metal/ceramic) debonding and the occurrence of white spot lesions during orthodontic treatment. Various curing techniques are employed to assess shear bond strength (SBS) and microleakage in both metal and ceramic brackets.
Materials and methods
A total of 120 samples were divided into six groups, each consisting of 20 samples. The groups were categorized based on the bracket material (metal or ceramic) and further subdivided according to the light-emitting diode (LED) curing method (traditional, transillumination, or combination). Fifty percent (60 samples) of each group were allocated for SBS evaluation, while the remaining 50% (60 samples) were used for microleakage assessment. The buccal enamel surfaces of all teeth in the six groups were etched and coated with a uniform layer of sealant. Stainless steel and ceramic maxillary premolar brackets were affixed using Transbond XT adhesive and light-cured with an LED unit. SBS was measured using the Instron ElectroPuls E3000 universal testing machine, and microleakage was examined using a stereomicroscope.
Results
One-way analysis of variance (ANOVA) with Bonferroni post-hoc test revealed significant differences in SBS among the six groups. Group IV exhibited the minimum SBS mean (7.02 MPa), while group VI displayed the maximum SBS mean (21.73 MPa). Microleakage assessment demonstrated that group IV had a maximum depth of 0.26 mm using the transillumination method, whereas group VI showed a minimum depth of 0.14 mm with the combination technique.
Conclusion
Brackets cured with a combination of conventional (5 seconds) and transillumination (5 seconds per bracket) methods exhibited significantly higher SBS. Conversely, group IV, cured solely with the transillumination technique (10 seconds per bracket), demonstrated the lowest strength. In terms of microleakage, group VI, treated with the combination technique, displayed the shallowest depth, while group IV, cured exclusively with transillumination, showed the greatest depth of microleakage. These findings underscore the importance of the curing method in influencing both SBS and microleakage, offering valuable insights for optimizing orthodontic bracket placement techniques.
How to cite this article
Lenin A, Anbarasu P, S SK, et al. Comparison of Microleakage and Bond Strength in Metal and Ceramic Brackets Cured by Conventional and Transillumination Methods: An In-vitro Evaluation. Int J Clin Pediatr Dent 2024;17(9):999–1003.
Keywords: Ceramic brackets, Microleakage, Shear bond strength, Transillumination curing
Introduction
Fixed orthodontic treatment has been significantly improved by advancements in bonding techniques, reducing chair time, enhancing aesthetics, and improving oral hygiene. Successful bonding of orthodontic brackets relies on the effective curing of composite resin and adhesives, establishing a strong mechanical connection between the bracket, resin, and enamel interface through resin tags penetrating tooth surface irregularities.1
The mechanical properties, including modulus of elasticity, tensile, and compressive strength, of adhesives and composite resin play a pivotal role in the bonding process. The depth of polymerization is influenced by factors such as the degree, duration, and direction of curing.2
Traditional light-curing methods, directed from the sides of the bracket, often result in incomplete polymerization at the bracket center due to the convexity of the labial tooth surface.3 To address this, newer methods like the transillumination technique have been proposed to cure the composite under metallic brackets by Tavas and Watts in 1979.4 In this technique, light is emitted from the opposite side (palatal side) of the tooth and passes through buccolingual thickness toward the composite under the metallic bracket. Transillumination, particularly with a 50-second cure period, has been shown to enhance bracket bond strength by intensifying light exposure and extending curing time.5 Light energy attenuation through ceramic orthodontic brackets is manufacturer-dependent, with no overall difference between monocrystalline and polycrystalline brackets.6
Shear bond strength (SBS) is crucial, especially as bonding materials and techniques evolve. For metal/ceramic brackets, a robust SBS is necessary to withstand forces during orthodontic treatment.7 Reynolds suggested SBS values of 5.9–7.8 MPa can withstand these forces.8 Establishing a strong bracket–teeth interface is pivotal for biomechanical control as inadequate bonding can lead to prolonged treatment duration, microleakage at the enamel–adhesive interface, and white spot lesions, manifesting as enamel decalcification defects with a common pattern being diffuse opacity.
Microleakage's impact on bracket debonding and white spot lesion formation during orthodontic treatment has been extensively studied.9 This research employs various curing techniques to assess SBS and microleakage in both metal and ceramic brackets.
Materials and Methods
This experimental study, approved by the institutional ethical committee (approval no: 138/IHEC/Jan 2021), involved 120 first premolar samples extracted for orthodontic treatment. G*Power version 3.1.9.4 estimated the sample size at 90% power with a 1% α error. The teeth were collected following the Occupational Safety and Health Administration (OSHA) and Centers for Disease Control and Prevention (CDC) guidelines for extraction, sterilization, storage, and handling.
Six groups of twenty samples each were created based on bracket material (metal vs ceramic) and light-emitting diode (LED) curing method (traditional, transillumination, or combination) (Table 1). Half of the samples from each group (60 in total) were used for SBS evaluation, while the other half were used for microleakage assessment. The buccal enamel surface of all the six groups of teeth was etched with 37% orthophosphoric acid for 15 seconds, rinsed with water, and then given a gentle air spray. After etching, the surfaces were coated with a thin, even layer of sealant (Transbond XT Primer, 3M Unitek). Stainless steel and ceramic maxillary premolar brackets (MBT 3M Gemini 0.022 slot) were placed on the surface of the tooth (Transbond XT Adhesive, 3M Unitek), adjusted to their final position, pressed firmly, and light cured using an LED light curing unit (Woodpecker ILED Plus curing light).
Table 1.
Shear bond strength (MPa) for the six groups
| N | Mean | Standard deviation | Standard error | 95% Confidence interval for mean | Minimum | Maximum | ||
|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||||
| Group I | 10 | 15.8470 | 5.16215 | 1.63242 | 12.1542 | 19.5398 | 7.51 | 21.81 |
| Group II | 10 | 17.1760 | 5.10875 | 1.61553 | 13.5214 | 20.8306 | 9.15 | 23.96 |
| Group III | 10 | 9.3740 | 3.57100 | 1.12925 | 6.8195 | 11.9285 | 5.38 | 14.84 |
| Group IV | 10 | 7.0240 | 2.82539 | 0.89347 | 5.0028 | 9.0452 | 3.17 | 11.25 |
| Group V | 10 | 15.7890 | 4.67166 | 1.47731 | 12.4471 | 19.1309 | 10.23 | 21.28 |
| Group VI | 10 | 21.7350 | 6.60888 | 2.08991 | 17.0073 | 26.4627 | 10.72 | 32.64 |
| Total | 60 | 14.4908 | 6.76774 | 0.87371 | 12.7425 | 16.2391 | 3.17 | 32.64 |
Shear bond strength was measured using an Instron ElectroPuls E3000 universal testing machine. A beveled flattened metal rod applied force at the bracket–tooth interface with a crosshead speed of 0.5 mm/min. UTM software transformed force values into shear stress, which was reported in megapascals.
Before microleakage assessment, samples were kept in distilled water at 37°C for 24 hours, sealed at the apex, and dyed with 2% methylene blue. After dye penetration, teeth were washed, air-dried, covered in nail polish (except for 1 mm around brackets), and soaked in distilled water. After 24 hours, teeth were rinsed, and longitudinal sections were made with a precision microtome. Sections were viewed under a stereomicroscope (Leica M205) for analysis.
Results
The statistical software (SPSS, version 17) for Microsoft Windows was used for all statistical analyses. The results were reported as mean and standard deviation (SD) as descriptive statistics, which were displayed as numbers and percentages. One-way analysis of variance (ANOVA) was used to study the statistical correlations within the groups, and the post-hoc test was used to assess the interactions between the groups. At the 0.05 level, the mean difference was significant.
The study involved six groups (group I to group VI) with different techniques applied to cure brackets. SBS was measured for each group, and the mean and SD values are presented in Table 1. A one-way ANOVA with the Bonferroni post-hoc test was conducted to compare the SBS parameters among the six groups. The results of the post-hoc test revealed significant differences in SBS between all groups. Group IV had the minimum SBS mean (7.02 MPa), while group VI had the maximum SBS mean (21.73 MPa) (Table 2).
Table 2.
One-way ANOVA—intragroup comparison of SBS
| (I) Specimen label | (J) Specimen label | Mean difference (I – J) | Standard error | Significance | 95% Confidence interval | |
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| Group I | Group II | −1.32900 | 2.15239 | 0.989 | −7.6882 | 5.0302 |
| Group III | 6.47300* | 2.15239 | 0.044 | 0.1138 | 12.8322 | |
| Group IV | 8.82300* | 2.15239 | 0.002 | 2.4638 | 15.1822 | |
| Group V | 0.05800 | 2.15239 | 1.000 | −6.3012 | 6.4172 | |
| Group VI | −5.88800 | 2.15239 | 0.085 | −12.2472 | 0.4712 | |
| Group II | Group I | 1.32900 | 2.15239 | 0.989 | −5.0302 | 7.6882 |
| Group III | 7.80200* | 2.15239 | 0.008 | 1.4428 | 14.1612 | |
| Group IV | 10.15200* | 2.15239 | 0.000 | 3.7928 | 16.5112 | |
| Group V | 1.38700 | 2.15239 | 0.987 | −4.9722 | 7.7462 | |
| Group VI | −4.55900 | 2.15239 | 0.294 | −10.9182 | 1.8002 | |
| Group III | Group I | −6.47300* | 2.15239 | 0.044 | −12.8322 | −0.1138 |
| Group II | −7.80200* | 2.15239 | 0.008 | −14.1612 | −1.4428 | |
| Group IV | 2.35000 | 2.15239 | 0.883 | −4.0092 | 8.7092 | |
| Group V | −6.41500* | 2.15239 | 0.047 | −12.7742 | −0.0558 | |
| Group VI | −12.36100* | 2.15239 | 0.000 | −18.7202 | −6.0018 | |
| Group IV | Group I | −8.82300* | 2.15239 | 0.002 | −15.1822 | −2.4638 |
| Group II | −10.15200* | 2.15239 | 0.000 | −16.5112 | −3.7928 | |
| Group III | −2.35000 | 2.15239 | 0.883 | −8.7092 | 4.0092 | |
| Group V | −8.76500* | 2.15239 | 0.002 | −15.1242 | −2.4058 | |
| Group VI | −14.71100* | 2.15239 | 0.000 | −21.0702 | −8.3518 | |
| Group V | Group I | −0.05800 | 2.15239 | 1.000 | −6.4172 | 6.3012 |
| Group II | −1.38700 | 2.15239 | 0.987 | −7.7462 | 4.9722 | |
| Group III | 6.41500* | 2.15239 | 0.047 | 0.0558 | 12.7742 | |
| Group IV | 8.76500* | 2.15239 | 0.002 | 2.4058 | 15.1242 | |
| Group VI | −5.94600 | 2.15239 | 0.080 | −12.3052 | 0.4132 | |
| Group VI | Group I | 5.88800 | 2.15239 | 0.085 | −0.4712 | 12.2472 |
| Group II | 4.55900 | 2.15239 | 0.294 | −1.8002 | 10.9182 | |
| Group III | 12.36100* | 2.15239 | 0.000 | 6.0018 | 18.7202 | |
| Group IV | 14.71100* | 2.15239 | 0.000 | 8.3518 | 21.0702 | |
| Group V | 5.94600 | 2.15239 | 0.080 | −0.4132 | 12.3052 | |
*, denotes significant mean difference with p < 0.05
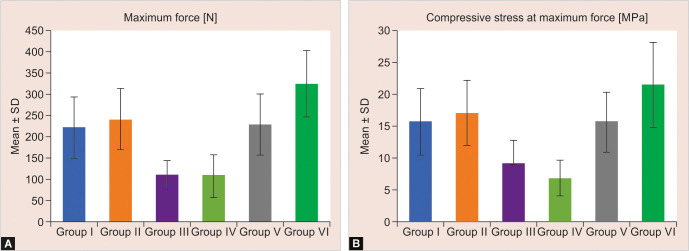
The SBS was graphically represented in Figures 1A and B, with group VI having the highest and group IV having the lowest SBS compared to the other groups. Group VI exhibited the highest maximum force (325.48 N), while group IV showed the lowest maximum force (108.88 N).
Figs 1A and B.
(A) Comparison of maximum force (MF) between six groups (in N); (B) Comparison of SBS between six groups at MF (in MPa)
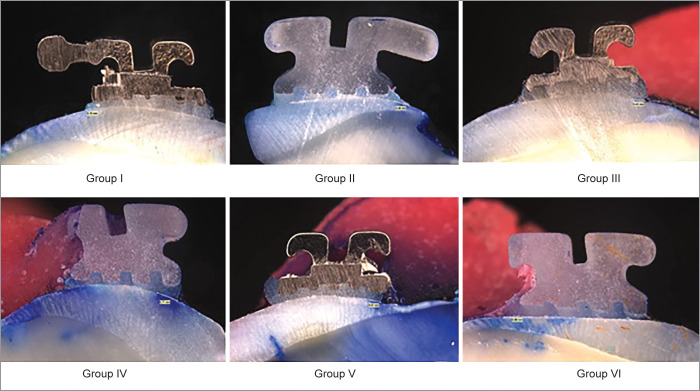
Evaluation of microleakage showed that group IV had a maximum microleakage of 0.26 mm with the transillumination method whereas group VI had a minimum microleakage of 0.14 mm with the combination technique. Quantitative data for the evaluation of microleakage were represented as mean and SD as shown in Table 3. One-way ANOVA indicated insignificant differences in microleakage with each other. The stereomicroscopic view of the depth of demineralization of different groups (groups I–VI) cured using conventional, transillumination, and combination techniques of ceramic and metal brackets is shown in Figure 2.
Table 3.
Quantitative data for evaluation of microleakage represented as mean and SD
| N | Mean | Standard deviation | Standard error | 95% Confidence interval for mean | Minimum | Maximum | ||
|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||||
| Group I | 10 | 0.1917 | 0.24318 | 0.09928 | −0.0635 | 0.4469 | 0.00 | 0.51 |
| Group II | 10 | 0.1950 | 0.28995 | 0.11837 | −0.1093 | 0.4993 | 0.00 | 0.74 |
| Group III | 10 | 0.2117 | 0.24498 | 0.10001 | −0.0454 | 0.4688 | 0.00 | 0.51 |
| Group IV | 10 | 0.2600 | 0.30796 | 0.12572 | −0.0632 | 0.5832 | 0.00 | 0.71 |
| Group V | 10 | 0.1650 | 0.25579 | 0.10443 | −0.1034 | 0.4334 | 0.00 | 0.51 |
| Group VI | 10 | 0.1433 | 0.35109 | 0.14333 | −0.2251 | 0.5118 | 0.00 | 0.86 |
| Total | 60 | 0.1944 | 0.26631 | 0.04439 | 0.1043 | 0.2846 | 0.00 | 0.86 |
Fig. 2.
Stereomicroscopic images showing the depth of demineralization
Discussion
In fixed orthodontics, selecting the optimal bonding technique is challenging. Tavas and Watts4 introduced light-cure adhesives, addressing bonding issues that may lead to bracket debonding and bacterial accumulation causing white spot lesions during treatment. Clinicians strive to identify the best adhesives, curing units, and methods, with bond strength and microleakage being critical in practice. This study compares conventional and transillumination curing methods, with a focus on posterior teeth due to higher bond failure risks.
Several studies, including those by Lee et al.10 and Olsen et al.,11 emphasize the importance of factors like storage conditions for extracted teeth and the impact of etching times on bond strength. Transbond XT is highlighted for its superior SBS.12 All samples were cured using a Woodpecker ILED Plus curing light based on solid-state LED technology proposed by Mills et al.13 Türkkahraman and Küçükeşmen previously compared the SBS of metal orthodontic brackets using two high power LED modes and halogen light. In this investigation, the fast mode LED curing results of 20 seconds are comparable to the 40 seconds of halogen-based lighting in terms of SBS.14
In the present study, group IV, ceramic brackets cured under the transillumination technique (10 seconds/bracket), showed a minimum mean of 7.02 MPa in 108.88 MF (maximum force), and group III, metal brackets cured under the transillumination technique, also resulted in a similar mean difference of 9.37 MPa in 111.13 MF. The results were similar to Heravi et al.,15 where the SBS value was dramatically reduced in the transillumination technique. They concluded that to obtain an acceptable SBS, one would need to double the curing time and increase the intensity.
Group VI, ceramic brackets cured under both techniques (conventional curing of 5 seconds followed by transillumination curing of 5 seconds) resulted in a maximum mean difference of 21.73 MPa in 325.48 MF. Kumar et al.16 carried out a similar study with metal brackets in maxillary first premolars and concluded that SBS achieved with 10 seconds of transillumination curing followed by conventional curing increased the bond strength and clinical significance.
In group II, ceramic brackets cured by the conventional method for 10 seconds resulted in a mean of 17.17 MPa in 241.26 MF. Reddy et al.17 evaluated the SBSs of ceramic and metal brackets and found that the metal brackets’ mean bond strength was 12.15 ± 1.32 MPa, whereas the bond strength of ceramic brackets was 20.68 ± 3.89 MPa. The SBS of the ceramic brackets, when conventionally cured, is shown to be superior to that of the metal brackets. The present study results are similar in comparing metal to ceramic brackets.
Group II (metal brackets cured in combination—conventional technique for 5 seconds and transillumination technique for 5 seconds) and group V (metal brackets cured by the conventional method for 10 seconds) resulted in an average SBS of 15.78 MPa in 229.06 MF and 15.84 MPa in 221.86 MF, respectively.
In evaluating SBS using conventional and transillumination methods, ceramic brackets consistently demonstrated higher SBS than metal brackets, especially when coupled with both curing techniques (transillumination followed by conventional).
Microleakage was assessed in this study using the dye penetration method with 2% methylene blue, a commonly used technique, and then examined under a stereomicroscope at 20× magnification.
The study results reveal that group VI, where ceramic brackets were cured with a combination of conventional (5 seconds/bracket) and transillumination (5 seconds/bracket), exhibited the lowest mean microleakage of 0.1433 mm. Group V, with metal brackets cured similarly, showed a mean microleakage of 0.1650 mm, consistent with Raza et al.'s findings regarding transillumination and conventional methods reducing demineralization.18
On the contrary, group III (metal brackets cured by transillumination for 10 seconds/bracket) and group IV (ceramic brackets cured by transillumination for 10 seconds/bracket) exhibited the highest microleakage, with mean values of 0.2117 mm and 0.2600 mm, respectively. Pakshir and Ajami's study also found increased microleakage with direct illumination and transillumination.19 Comparing all study groups, group II (ceramic brackets cured conventionally for 10 seconds/bracket) and group I (metal brackets cured conventionally for 10 seconds/bracket) showed mean microleakage values of 0.1950 mm and 0.1917 mm, respectively.
The study suggests that ceramic brackets cured with both conventional and transillumination techniques exhibit the least microleakage, followed by metal brackets treated similarly. The highest microleakage occurs in groups cured solely with the transillumination technique (10 seconds/bracket), while brackets cured only with the conventional technique (10 seconds/bracket) show less microleakage.
Limitation of the Study
The sample size may be considered relatively small for drawing generalizable conclusions. Additionally, the teeth were extracted for orthodontic treatment, which may not fully represent the diversity of teeth encountered in clinical practice. Factors such as patient variability, saliva contamination, and oral hygiene practices were not accounted for in this experimental design. A longer-term follow-up would be necessary to assess the durability of the bond and the potential for enamel demineralization throughout orthodontic treatment. The study did not explore other types of brackets or materials (e.g., polycarbonate, composite). Different bracket materials may exhibit varying bonding characteristics and susceptibility to microleakage.
Conclusion
Ceramic brackets resulted in increased SBS when compared to metal brackets, and maximum force at debonding was recorded. There was a significant difference in SBS between conventional, transillumination, and combination curing of bracket surfaces.
When brackets were cured in combination (conventional technique for 5 seconds and transillumination technique for 5 seconds/bracket), they showed significantly higher SBS. The SBS of group IV (curing only with transillumination technique for 10 seconds/bracket) resulted in minimum strength.
Group VI (cured with conventional technique for 5 seconds and transillumination technique for 5 seconds/bracket) showed the minimum depth of microleakage. Group IV (curing only with transillumination technique for 10 seconds/bracket) showed maximum depth of microleakage.
Orcid
Prema Anbarasu https://orcid.org/0000-0001-9355-0543
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Condò R, Mampieri G, Cioffi A, et al. Physical and chemical mechanisms involved in adhesion of orthodontic bonding composites: in vitro evaluations. BMC Oral Health. 2021;21(1) doi: 10.1186/s12903-021-01715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.AlShaafi MM. Factors affecting polymerization of resin-based composites: a literature review. Saudi Dental J. 2017;29(2):48–58. doi: 10.1016/j.sdentj.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mäkinen E, Lassila L, Varrela J, et al. Light-curing of orthodontic bracket adhesive by transillumination through dentine and enamel. Biomater Investig Dent. 2019;6(1):6–12. doi: 10.1080/26415275.2019.1632709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tavas MA, Watts DC. Bonding of orthodontic brackets by transillumination of a light activated composite: an in vitro study. British J Orthod. 1979;6(4):207–208. doi: 10.1179/bjo.6.4.207. [DOI] [PubMed] [Google Scholar]
- 5.Oesterle LJ, Shellhart WC. Bracket bond strength with transillumination of a light-activated orthodontic adhesive. Angle Orthod. 2001;71(4):307–311. doi: 10.1043/0003-3219(2001)071<0307:BBSWTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Aldossary MS, Hajia SS, Santini A. Light energy transmission through six different makes of ceramic orthodontic brackets. Int Orthod. 2018;16(4):638–651. doi: 10.1016/j.ortho.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Subramanian SK, Anbarasu P, Joushua RS, et al. Effect of Er, Cr:YSGG laser enamel etching with varying power output and irradiation time on the shear bond strength. J Orthod Sci. 2022:11. doi: 10.4103/jos.jos_129_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reynolds IR. A review of direct orthodontic bonding. Br J Orthod. 1975;2:171–178. [Google Scholar]
- 9.Masarykova N, Tkadlec E, Chlup Z, et al. Comparison of microleakage under orthodontic brackets bonded with five different adhesive systems: in vitro study. BMC Oral Health. 2023;23(1):637. doi: 10.1186/s12903-023-03368-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JJ, Nettey-Marbell A, Cook A, Jr,, et al. Using extracted teeth for research: the effect of storage medium and sterilization on dentin bond strengths. J Am Dental Assoc. 2007;138(12):1599–1603. doi: 10.14219/jada.archive.2007.0110. [DOI] [PubMed] [Google Scholar]
- 11.Olsen ME, Bishara SE, Boyer DB, et al. Effect of varying etching times on the bond strength of ceramic brackets. Am J Orthod Dentofacial Orthop. 1996;109(4):403–409. doi: 10.1016/s0889-5406(96)70122-1. [DOI] [PubMed] [Google Scholar]
- 12.Hellak A, Ebeling J, Schauseil M, et al. Shear bond strength of three orthodontic bonding systems on enamel and restorative materials. BioMed Res Int. 2016 doi: 10.1155/2016/6307107. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mills RW, Jandt KD, Ashworth SH. Dental composite depth of cure with halogen and blue light emitting diode technology. Br Dental J. 1999;186(8):388–391. doi: 10.1038/sj.bdj.4800120. [DOI] [PubMed] [Google Scholar]
- 14.Türkkahraman H, Küçükeşmen HC. Orthodontic bracket shear bond strengths produced by two high-power light-emitting diode modes and halogen light. Angle Orthod. 2005;75(5):854–857. doi: 10.1043/0003-3219(2005)75[854:OBSBSP]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Heravi F, Moazzami SM, Ghaffari N, et al. Evaluation of shear bond strength of orthodontic brackets using trans-illumination technique with different curing profiles of LED light-curing unit in posterior teeth. Prog Orthod. 2013;14(1) doi: 10.1186/2196-1042-14-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar P, Nayak RS, Tan K, et al. Bracket bond strength with transillumination of a light activated orthodontic adhesive and the effect of curing time and tooth thickness on it: an in vitro study. J Ind Orthod Soc. 2013;47(3):148–153. [Google Scholar]
- 17.Reddy YG, Sharma R, Singh A, et al. The shear bond strengths of metal and ceramic brackets: an in-vitro comparative study. J Clin Diagn Res. 2013;7(7):1495. doi: 10.7860/JCDR/2013/5435.3172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raza M, Kumar P, Gulati N, et al. Comparison of demineralization around orthodontic brackets cured by conventional method and transillumination technique—an in vitro evaluation. J Orthod Sci. 2020;9:16. doi: 10.4103/jos.JOS_3_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pakshir H, Ajami S. Effect of enamel preparation and light curing methods on microleakage under orthodontic brackets. J Dentistry (Tehran, Iran) 2015;12(6):436. [PMC free article] [PubMed] [Google Scholar]