Abstract
Background
The Surgical Safety Checklist (SSC) is a cornerstone of ensuring the safety and accuracy of communication among interdisciplinary teams in the operating room. Central to the successful implementation of such a checklist is the concept of psychological safety. Despite the extensive body of research on the checklists’ efficacy, the association between healthcare professionals’ (HCPs) perceptions of the checklist and their level of psychological safety remains uninvestigated. This study attempts to address this gap by examining how their perceptions of the checklist intersect with their sense of psychological safety.
Methods
A cross-sectional survey comprising 25 items was conducted from November 2022 to January 2023 on; Demographics (6 items), the SSC (12 items), and the Psychological Safety Scale (7 items). We invited 125 HCPs from five different professional groups in the operation ward to complete the survey.
Results
Of the 125 asked to participate, 107 responded, and 100 of whom completed the entire survey. The level of psychological safety increased by 1.25 (95 % CI 0.36 to 2.14, p=0.006) per one-point increase of the perception that colleagues listen when checklist items are being reviewed, and increased by 1.1 (95% CI 0.4 to 1.7, p=0.002) per one-point increase in the perception that the checklist enhances interdisciplinary teamwork, and increased by 0.86 (95% CI 0.15 to 1.57, p=0.02) per one-point increase in the perception that the checklist provides structure in the operating room. Conversely, the level of psychological safety decreased by 1.4 (95 % CI 0.5 to 2.3, p=0.004) per one-point increase in the perception that the checklist is time-consuming.
Conclusion
Our findings reveal a significant association between psychological safety levels and perceptions of the SSC. Increased psychological safety was linked to more positive views on the checklist’s role in enhancing interdisciplinary teamwork, creating structure and attentiveness among colleagues. While seeing the checklist as time-consuming was associated with a lower psychological safety rating. These results suggest that psychological safety influences how individuals view and engage with patient safety measures like the checklist, highlighting the importance of fostering a supportive environment to optimise safety practice.
Keywords: Patient safety, Surveys, Safety culture, Checklists, Surgery
WHAT IS ALREADY KNOWN ON THIS TOPIC
The Surgical Safety Checklist (SSC) is not always used correctly and compliantly.
A psychologically safe environment enhances learning, performance and error reporting.
WHAT THIS STUDY ADDS
This study attempts to address the gap in understanding the association between healthcare professionals’ (HCPs) perceptions of the SSC and their level of psychological safety to improve interventions designed to enhance the efficacy of the SSC.
HCPs who report a higher level of psychological safety tend to perceive the SSC as a more effective tool for enhancing interdisciplinary teamwork, creating structure and listening to colleagues when reviewing the checklist, offering valuable insights into the factors impacting its consistent and accurate use in clinical settings.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The link between psychological safety and the perception of the SSC’s effectiveness highlights the need for research into how psychological safety influences the implementation and use of safety protocols.
Introduction
The complexity of the operating room (OR) and its rapidly changing and demanding environment requires good collaboration and communication across interprofessional teams to improve learning and enhance patient safety. One important factor in cultivating effective interprofessional communication and collaboration in healthcare is psychological safety,1 2 which means members of a team feel safe enough to speak up about their observations, safety concerns and questions without the fear of negative repercussions.3 Researchers have identified certain organisational, team and individual factors that enable psychological safety in healthcare.4 Feeling psychologically safe is associated with, for example, improved team communication and knowledge sharing,5 team learning,3 5 error reporting,6 team performance7 and successful adoption of new interventions.8 Moreover, it is considered an important aspect of safety culture in healthcare.4 These factors emphasise the importance of consistently fostering psychological safety among healthcare professionals (HCPs) in the OR and enabling them to speak up.
An example of a situation requiring OR staff to be candid is non-adherence to standard procedures like the Surgical Safety Checklist (SSC), which the WHO introduced in 2008 as a vital tool to improve safety and mitigate the occurrence of adverse events in the OR by fostering teamwork and enhancing interprofessional communication.9
SSC systematically and consistently guides HCPs through a comprehensive three-phase checklist with essential steps before (sign in), during (time out) and after surgery (sign out). The checklist ensures that critical information, including patient identification, verification of surgical procedure and site, presentation of the team, anticipated complications and estimated blood loss, is effectively communicated among all HCPs in the OR, allowing the team to be prepared and manage expected and unexpected events.
Adopted worldwide, SSC has been mandatory in all ORs in Denmark since 2014. Numerous studies have shown a clear decrease in morbidity and mortality since its introduction,10,13 but these improvements are the subject of debate as others have not found the same effect.14 15 These divergent results may be due to ineffective implementation, for example, a lack of introduction and training, limited attention paid to local culture and context, minimal management support,16 variations in the assessment of checklist compliance17 18 or are a result of incorrect or non-compliant use of the SSC.18,24 Barriers to applying the SSC according to the WHO guidelines involve individual (eg, resistance, beliefs, lack of leadership), environmental (eg, workload, time pressure, competing tasks) and cultural (eg, surgical specialty, tick box exercise, professional independence) barriers.25 Another critical factor that remains unexplored is the association between HCP perceptions of the checklist and their levels of psychological safety, which is important to understand since effective use of SSC requires coordinated efforts from the entire surgical team, which a psychologically safe environment may support.
This study explores HCP perceptions of the SSC and examines how these perceptions are related to the level of psychological safety within various HCP groups.
Materials and methods
Setting and participants
We conducted the study at the Department of Gynaecology and the Department of Anaesthesiology at the Juliane Marie Centre, Copenhagen University Hospital—Rigshospitalet, Denmark, which is a tertiary teaching hospital, from November 2022 to January 2023. The hospital has a high turnover of HCPs and 2500 gynaecological surgeries a year. All HCPs working in a gynaecological OR at the Departments of Gynaecology and Anaesthesiology were eligible to participate. We invited all 125 HCPs working in the department to participate, which included anaesthesiologists (n=19), gynaecologists (n=25), nurse anaesthetists (n=24), OR nurses (n=38) and residents (in gynaecology and obstetrics and anaesthesiology) (n=19). The Strengthening the Reporting of Observational Studies in Epidemiology checklist for cross-sectional studies was used to report the study.26
Survey design and development
The final survey, developed based on a two-step process, was in Danish and comprised 25 items.
Step 1 involved identifying and clarifying items regarding SSC. We used a qualitative research design27 to determine which items to include in our SSC survey. Two researchers (OWM, JS) conducted eight semi-structured interviews with representatives from five HCP groups (anesthesiologist (n=1), gynaecologists (n=2), nurse anaesthetists (n=2), OR nurses (n=2) and resident (n=1)), selected based on a convenience sampling and their experience. Participants were asked general questions about SSC, and questions pertaining to the three specific phases, that is, sign in, time out and sign out.
During the interviews, field notes were taken and later consolidated into a spreadsheet. Three observers (OWM, JLS and JS) independently reviewed the anonymised spreadsheet to identify and eliminate duplicate entries. The final survey questions were then developed based on insights gained from semi-structured interviews. We used qualitative content analysis to analyse the data,28 which yielded two major themes: practical perceptions of SSC and personal perceptions of SSC.
Step 2 then involved translating Edmondson’s seven-item Psychological Safety Scale (PSS),3 which was selected and considered suitable for this study because semi-structured interviews indicated that the HCPs viewed psychological safety as an important and potential factor influencing the adherence to SSC.
As PSS was originally developed and validated in English, we translated it into Danish (See online supplemental figure S1 and table S1) using WHO translation guidelines29 to ensure the validity of the outcome data. The translation process involved forward translation by a professional, bilingual Danish-English translator and a blind backward translation into English by a professional, native English-speaking translator. Three researchers (OWM, JS and JLS) met to reach a consensus on the final version of the Danish translation.
Final survey
The final survey comprised three categories: demographics (6 items), perceptions of SSC (12 items) and PSS (7 items). The SSC and PSS items were based on a five-point Likert scale (1, strongly disagree; 2, disagree; 3, partly agree; 4, agree; and 5, strongly agree) and a free-text option was available at the end of each section.
Pilot test of survey and face validity
The research group began by assessing the survey using computers, smartphones and tablets in an iterative process involving proofreading and pilot testing to ensure understandability and that all technical aspects worked smoothly. Next, a group of participants (one anaesthesiologist, one gynaecologist, four nurse anaesthetists, three OR nurses and two residents) representing the target group did a review of the survey to assess its clarity, comprehensibility and appropriateness for the target group.30 Based on an analysis of their comments on the pilot test, two specific terms from the ‘Psychological Safety Scale’ section, ‘team’ and ‘risk’, needed further elaboration. A detailed definition of the two terms was added to the final survey, but no questions were rephrased. At this point, we concluded that the survey now had an acceptable level of face validity. The individuals who participated in the eight semi-structured interviews were included in the final panel but not in the pilot test group.
Administering the survey
The secure web application Research Electronic Data Capture31 32 was used to design, test and distribute the survey to participants via their employee e-mails and to subsequently collect and manage data. E-mail reminders were sent to non-responders at 10-day intervals for 2 months.
Data analysis and statistics
We used descriptive statistics to describe the demographic characteristics, presenting numbers and percentages for participants’ characteristics, while for quantitative variables, we report median and IQR.
Measures of perceptions of SSC and level of psychological safety
Scores were summarised at the item level using mean, median and IQR. PSS items I, III and V were reverse scored due to negative items, with a higher score on the items indicating higher disagreement with the item. The level of psychological safety was calculated as the total sum of the item scores (minimum score of 7 and maximum score of 35) and SD. Cronbach’s alpha was calculated independently for PSS and SSC to measure internal consistency, with a value >0.7 considered acceptable. The general linear model was used to compare the mean of the scores between the five HCP groups (anaesthesiologists, gynaecologists, nurse anaesthetists, OR nurses and residents) adjusted for age. The analyses were adjusted for age and not years of experience, as the latter is not explicitly delineated in our survey to distinguish between experience from the OR and general clinical experience. Tukey’s post-hoc tests were performed to correct for multiple pairwise comparisons.
The mean of the psychological safety score across groups of age, years of experience and OR days per month was compared using one-way analysis of variance. The means of psychological safety score items were compared using a linear mixed model with a random intercept to take into account the correlation among item responses for each individual. Tukey’s post hoc test was also performed for all analyses to correct for multiple pairwise comparisons of the outcomes.
For each SSC item, we explored its association with the level of psychological safety using the general linear model adjusted for age and profession. We examined whether the conclusion was robust with respect to the exclusion of potentially influential observations. The supplementary material (online supplemental tables S4 and S5) contains all of the multivariable analyses. All statistical analyses were performed using R version 4.2.0.33 P values <0.05 were considered significant. However, the large number of tests performed increases the risk of false-positive findings, and therefore, we interpret p values near 0.05 with caution.
Results
Of the 125 HCPs invited to participate, 107 responded, corresponding to a response rate of 86%. 100 participants completed the entire survey, six partially completed it and one declined to do so. The analysis only includes fully completed surveys. We grouped data according to five professions. Online supplemental table S2 and S3 present the distribution of scores (1–5) for each item of SSC and PSS.
The median age of the total study population was 46 (IQR 39, 55), and the median years’ experience was 17.5 (IQR 8.8, 28). Table 1 presents the demographic data.
Table 1. Demographic data on the study population and the five healthcare professional groups.
| Study population | Anaesthesiologists | Gynaecologists | Nurse anaesthetists | OR nurses | Residents | |
| Number | 100 | 14 | 22 | 19 | 26 | 19 |
| Gender n (%) | ||||||
| Female | 79 (79) | 5 (35.7) | 17 (77) | 15 (79) | 26 (100) | 16 (84) |
| Male | 20 (20) | 8 (57.1) | 5 (23) | 4 (21) | 0 (0) | 3 (16) |
| Other | 1 (1) | 1 (7.1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Age (median (IQR)) | 46 (39, 55) | 50 (45, 54) | 51.5 (46, 61) | 52 (47, 62.5) | 42.5 (32, 55) | 35 (34, 40) |
| Years’ experience (median (IQR)) | 17.5 (8.8, 28) | 18.5 (16, 24.8) | 23.50 (17, 32.5) | 28 (22, 34) | 16 (6, 23.8) | 7 (5, 12) |
| Days in OR per month (median (IQR)) | 15 (6, 18) | 19 (15, 20) | 8 (3, 9) | 16 (10, 18) | 16 (15, 20) | 4 (3, 8.5) |
OROperating Room
Internal validity
Internal validity measured by Cronbach’s alpha was α=0.69 (95% CI 0.6 to 0.8) for SSC and α=0.76 (95% CI 0.7 to 0.8) for PSS.
Perceptions of SSC and level of psychological safety
Table 2 presents an overview of HCP perceptions of SSC and any significant findings between the HCP groups. The mean score for the study population was >3 for all items, except item 10, which had a mean score of 1.7.
Table 2. Overview of healthcare professional (HCP) perception of the SSC across the study population and five groups of HCPs and significant findings* for the study population.
| SSC items | Study populationMeanMedian (IQR)n=100 | AnaesthesiologistsMeanMedian (IQR)n=14 | GynaecologistsMeanMedian (IQR)n=22 | Nurse anaesthetistsMeanMedian (IQR)n=19 | OR nursesMeanMedian (IQR)n=26 | ResidentsMeanMedian (IQR)n=19 | Significant findings among the five healthcare professional groups* |
| 1. I have received training in the clinical use of SSC | 3.64 (3, 4) | 3.43.5 (3, 4) | 3.13 (2.25, 4) | 3.84 (3, 4) | 4.55 (4, 5) | 3.23 (3, 4) | OR nurses reported a higher score compared with anaesthesiologists (1.1, 95% CI 0.2 to 1.9, p=0.008), gynaecologists (1.5, 95% CI 0.7 to 2.2, p<0.001) and residents (1.3, 95% CI 0.5 to 2.1, p<0.001). |
| 2. I am familiar with other staff groups' important items on the SSC | 3.54 (3, 4) | 3.64 (3, 4) | 3.33 (3, 4) | 3.84 (3.5, 4) | 3.84 (3, 4.75) | 33 (3, 3.5) | |
| 3. My colleagues listen when I review SSC items | 3.54 (3, 4) | 3.84 (3.25, 4) | 3.74 (3, 4) | 33 (2.5, 3.5) | 3.23 (3, 3.75) | 4.14 (4, 5) | OR nurses (0.9, 95% CI 0.3 to 1.6, p=0.001) and nurse anaesthetists (1.1, 95% CI 0.3 to 1.9, p=0.002) reported a lower score than residents, and nurse anaesthetists (0.8, 95% CI 0.04 to 1.6, p=0.04) reported a lower score than anesthesiologists |
| 4. SSC works best when only one person reviews all items on the checklist throughout all three phases (sign in, time out and sign out) | 3.84 (3, 4) | 3.84 (3, 4) | 3.74 (3, 4.75) | 3.94 (4, 4) | 3.84 (3, 5) | 3.64 (3, 4) | |
| 5. A visualisation of SSC (eg, poster) would help me review SSC items | 3.54 (3, 4) | 3.54 (2.25, 4) | 3.74 (3, 5) | 3.33 (3, 4) | 33 (2, 4) | 4.35 (4, 5) | OR nurses (1.3, 95% CI 0.4 to 2.2, p<0.001) reported a lower score than residents |
| 6. SSC increases patient safety in the OR | 4.45 (4, 5) | 3.94 (3.25, 4) | 4.34 (4, 5) | 4.55 (4, 5) | 4.65 (5, 5) | 4.85 (5, 5) | |
| 7. SSC provides the opportunity to reflect on the operation | 4.14 (4, 5) | 3.64 (3, 4) | 44 (3.25, 5) | 44 (4, 4.5) | 4.35 (4, 5) | 4.75 (4.5, 5) | Anaesthesiologists (1.2, 95% CI 0.2 to 2.1, p=0.008) reported a lower score than residents. |
| 8. SSC provides structure in the OR | 44 (3, 5) | 3.74 (3, 4) | 44 (4, 5) | 3.94 (3.5, 4) | 3.94 (3, 5) | 4.55 (4, 5) | |
| 9. SSC enhances interdisciplinary teamwork in the OR | 3.94 (3, 5) | 3.43 (3, 4) | 44 (4, 5) | 3.94 (3, 5) | 3.94 (3, 5) | 4.34 (4, 5) | |
| 10. SSC is unnecessarily time-consuming | 1.72 (1, 2) | 2.12 (2, 2.75) | 1.62 (1, 2) | 1.51 (1, 2) | 1.61 (1, 2) | 1.72 (1, 2) | |
| 11. It would be a good idea to add a couple of minutes to reflect on the operation that just took place in continuation of the 'time out phase' | 3.13 (2, 4) | 3.23 (2.25, 4) | 2.62.5 (2, 3) | 3.13 (2.25, 4) | 3.33 (2.25, 4) | 3.23 (3, 4) | |
| 12. I think that there is a need to implement a project on training to use SSC correctly | 3.23 (2, 4) | 2.62 (2, 3) | 2.92 (2, 3.75) | 33 (2, 4) | 3.54 (3, 4) | 3.64 (3, 4) |
All analysis adjusted for age, profession, and multiple testing. Item 10 was the only negative phrased item.
OR, operating room; SSC, Surgical Safety Checklist
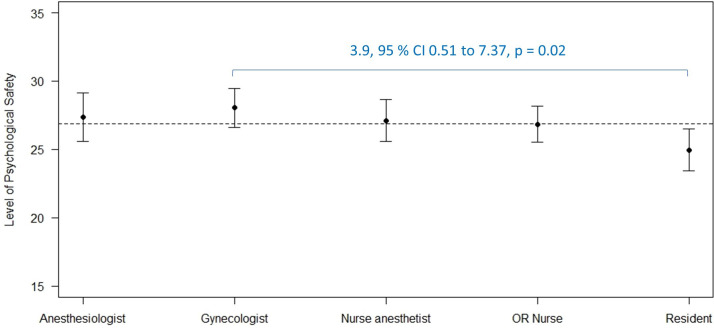
Table 3 presents an overview of the mean scores and significant findings for each PSS item and the level of psychological safety in the study population and five HCP groups. The mean level of psychological safety for the study population was 26.9 (SD 3.5) out of a potential 35. Figure 1 illustrates the total mean score for each HCP group. When adjusting for age and multiple testing, the mean psychological safety score for residents was 3.9 (95% CI 0.5 to 7.4, p=0.02) lower than the mean psychological safety score for gynaecologists. We did not find a difference between the level of psychological safety and groups divided by years of experience (<5 years, 5–9 years, 10–14 years and >15 years), age (< 40 years, 40–49 years, 50–59 years and>60 years) and OR days per month (<5 days, 5–9 days, 10–14 days, 15–19 days and >20 days) (results not shown). In general, the respondents’ mean scores were >3 for all PSS items. No differences were found between the HCP groups for each item. Residents reported the lowest mean score for each item, with the exception of item VI. Items II and IV had the lowest mean scores for the study population and were related to participants’ feelings of being unable to raise concerns or discuss difficult issues and to their lack of confidence in taking risks.
Table 3. Results for each Psychological Safety Scale item and the level of psychological safety among the study population and the five healthcare professional groups and significant findings for study population.
| PSS items | Study populationMeanMedian (IQR)n=100 | AnaesthesiologistsMeanMedian (IQR)n=14 | GynaecologistsMeanMedian (IQR)n=22 | Nurse anaesthetistsMeanMedian (IQR)n=19 | OR nursesMeanMedian (IQR)n=26 | ResidentsMeanMedian (IQR)n=19 | Significant findings for study population* |
| I. If you make a mistake on this team, it is often held against you (R) | 4.14 (4, 4) | 4.14 (4, 4) | 4.34 (4, 5) | 4.14 (4, 4) | 4.04 (4, 4.75) | 3.84 (4, 4) | The overall mean for item I was 0.5 (95% CI 0.3 to 0.8, p<0.001) higher than item II and 0.7 (95% CI 0.4 to 0.9, p<0.001) higher than item IV. |
| II. Members of this team are able to bring up problems and tough issues | 3.54 (3, 4) | 3.64 (3, 4) | 3.64 (3, 4) | 3.74 (3, 4) | 3.53 (3, 4) | 3.23 (3, 4) | |
| III. People on this team sometimes reject others for being different (R) | 4.04 (4, 4) | 44 (4, 4) | 4.14 (4, 5) | 4.14 (4, 4) | 4.14 (4, 5) | 3.64 (3, 4) | The overall mean for item III was 0.5 (95% CI 3.0 to 0.8, p<0.001) higher than item II and 0.7 (9% CI 0.4 to 0.9, p<0.001) higher than item IV. |
| IV. It is safe to take a risk on this team | 3.43 (3, 4) | 3.64 (3, 4) | 3.54 (3, 4) | 3.53 (3, 4) | 3.53.5 (3, 4) | 2.93 (2, 3.5) | |
| V. It is difficult to ask other members of this team for help (R) | 4.14 (4, 5) | 44 (4, 4.75) | 4.55 (4, 5) | 4.14 (4, 4.5) | 4.14 (4, 4.75) | 3.84 (4, 4) | The overall mean for item V was 0.6 (95% CI 0.3 to 0.8, p<0.001) higher than item II and 0.7 (95% CI 0.4 to 1, p<0.001) higher than item IV. |
| VI. No one on this team would deliberately act in a way that undermines my efforts | 44 (4, 5) | 3.94 (3, 5) | 44 (4, 5) | 44 (4, 4.5) | 3.94 (4, 4) | 44 (4, 4) | The overall mean for item VI was 0.4 (95% CI 0.2 to 0.7, p<0.001) higher than item II and 0.6 (95% CI 0.3 to 0.8, p<0.001) higher than item IV. |
| VII. Working with members of this team, my unique skills and talents are valued and used | 3.94 (3, 4) | 4.14 (4, 4) | 4.14 (4, 4.75) | 3.84 (3.5, 4) | 3.64 (3, 4) | 3.63 (3, 4) | The overall mean for item VII was 0.3 (95% CI 0.1 to 0.6, p=0.008) higher than item II and 0.5 (95% CI 0.2 to 0.7, p<0.001) higher than item IV. |
| Total PS item score (SD) | 26.9 (3.5) | 27.4 (2) | 28.0 (3.2) | 27.1 (3.1) | 26.8 (3.9) | 24.9 (3.9) |
Adjusted for age and for multiple testing.
PSS, Psychological Safety Scale; R, reverse scored (higher numbers indicating greater disagreement with the statement)
Figure 1. Total sum score of psychological safety and CI for each healthcare professional group. The dotted line represents the overall mean of the total sum score for psychological safety for the entire study population. The difference between gynaecologists and residents is illustrated.
Associations between level of psychological safety and perceptions of SSC
We found that, when adjusted for profession and age, the level of psychological safety increased by 1.25 (95 % CI 0.36 to 2.14, p=0.006) per each one-point increase of the perception of that colleagues listen when SSC items are being reviewed (Item 3). Additionally, we found that the level of psychological safety increased by 0.86 (95% CI 0.15 to 1.57, p=0.02) per each one-point increase of the perception that the SSC provides structure in the OR (Item 8). Furthermore, we found that the level of psychological safety increased by 1.1 (95% CI 0.4 to 1.7, p=0.002) per each one-point increase of the perception that the SSC enhances interdisciplinary teamwork in the OR (Item 9). Conversely, we found a decrease of 1.4 (95 % CI 0.5 to 2.3, p=0.004) in the level of psychological safety per one-point increase in the perception of the SSC as being time-consuming (Item 10). No significant association with the level of psychological safety was found for the remaining seven SSC items.
Discussion
This study focuses on perceptions of SSC and the level of psychological safety among 100 HCPs who completed our survey and were from five HCP groups: anesthesiologists, gynaecologists, nurse anaesthetists, OR nurses and residents. Perceptions of SSC varied between the HCP groups, highlighting the importance of collecting data on the perceptions of all HCPs involved in patient care in the OR. The majority of our study population, with a mean score of 4.4, agreed that SSC increases patient safety in the OR, which aligns with findings from previous studies.34 Residents reported the highest scores in terms of SSC creating structure, allowing reflection on the surgical procedure, and the simultaneous strengthening of interprofessional teamwork in the OR. Due to its structured format and standardised approach across all departments and surgical specialties, SSC is beneficial for residents, enriching their structured education, training and team communication, which is particularly crucial in a high-pressure environment because it prompts the use of safety protocols.35
One of the key findings in this study was that OR nurses reported having received more training in the clinical use of SSC compared with the anaesthesiologists, gynaecologists and residents (in gynaecology and obstetrics and anesthesiology). Additionally, nurse anaesthetists and OR nurses reported a higher score on being familiar with other HCP groups important SSC items. This may reflect that becoming an OR nurse and nurse anaesthetist in Denmark requires earning specific qualifications that include learning objectives such as how to receive the surgical patient in the OR and using SSC.36 This requirement means that all new OR nurse and nurse anaesthetist team members consistently undergo systematic training and that the OR nurses and nurse anaesthetists conducting the training have more experienced and maintain their skills. Nurse anaesthetists, however, rotate to different departments during their education programme, which means their training depends on the local department. OR nurses, in contrast, receive their training at the same department. The anaesthesiologists, gynaecologists and residents do not undergo any formal SSC training and instead acquire their knowledge based on a ‘see one, do one, teach one’ approach. In the OR, the circulating OR nurse must tick off various SSC items in the patient’s electronic medical records, providing several additional repetitions of each SSC item. Consequently, anaesthesiologists, gynaecologists and residents must memorise checklist items if the OR nurse does not provide any help, which might explain why OR nurses reported the lowest scores on perceived usefulness of having a visible checklist in the OR. Nevertheless, studies have shown that a visible checklist in the OR supports the OR team37 38 by facilitating a more structured and consistent review of SSC. This visibility provides objective confirmation of data, which can help team members feel more confident in speaking up about concerns. This highlights the fact that adopting a tool like SSC involves more than simply mandating its use; it requires effective implementation strategies16 39 that enhance psychological safety. Such strategies must consider the local context,40 include thorough training and education,16 ensure transparency and clarity regarding checklist aims, actively involve stakeholders and engage leadership25 to foster an environment where team members feel secure in voicing their concerns.
Psychological safety is an emerging key concept in the understanding the ability of HCPs to speak up about their concerns.3 SSC is a tool designed to ensure that important elements are communicated during surgical procedures, where its usefulness depends on the input of everyone in the OR. Consequently, examining the level of psychological safety in relation to the perception of SSC is essential. We chose to focus on this issue because understanding the perception HCPs have of SSC and the level of psychological safety is vital to being able to target interventions aimed at improving use of the checklist. Notably, we found the lowest psychological safety score for PSS items II and IV, which relate to participants’ feelings of being unable to raise concerns or discuss difficult issues and to their lack of confidence in taking risks. These results highlight significant areas for improvement, suggesting that addressing these issues may be crucial for enhancing psychological safety and overall team effectiveness. Moreover, this indicates that certain aspects of the application of the SSC may need to be revised and refined to better support open communication and risk-taking. Addressing these issues could potentially enhance the effectiveness of the checklist and overall team performance. This may suggest the need for more formal interprofessional team training to ensure a consistent review of SSC among all HCP groups. Additional training and education on the practical use of the SSC can help create a psychologically safe environment and/or potentially reinforce the perceived value of the tool even when psychological safety is lacking.
The mean level of psychological safety for our study population was 26.9 (SD 3.5), while gynaecologists had the highest mean score 28 (SD 3.2), and residents had the lowest mean score 24.9 (SD 3.9). There is a growing body of evidence that people with a higher status in a hierarchy report a higher level of psychological safety.41 Appelbaum et al6 found that a perceived power distance among residents was negatively associated with psychological safety and the intention to reporting medical errors, whereas leader inclusiveness was found to be positively associated with psychological safety among residents. We found that residents have the lowest level of psychological safety, and other studies indicate that they also suffer from the highest degree of imposter syndrome,42 which has also been associated with increased rates of burnout among HCPs.43 These findings underline the importance of senior staff being more aware of creating a safe environment for new colleagues regardless of their specialty; however, a humble approach must be taken. Our study sheds light on the complexity of psychological safety, which may be the first step in understanding how we can improve and change the level of psychological safety, in a high-pressure healthcare setting like the OR. Various factors and stimuli enable psychological safety at the organisational, team and individual level.4 44 For example, in healthcare, familiarity with colleagues and team leaders and across teams increases the likelihood of speaking up4; however, building familiarity in healthcare teams can be challenging in settings with high staff turnover, eg, residents rotation and dynamic and shifting teams. In Denmark, residency rotations last 3 to 18 months, depending on the specialty. This variability can hinder becoming familiar with all staff during rotation periods, which is why enhancing other well-known facilitating factors, for example, leader inclusiveness, peer support and organisational support, is indispensable to creating a psychologically safe environment for residents.4 Moreover, continuously fostering a positive learning environment among residents supports both the level of commitment and job satisfaction.45 It is crucial to remember that each of these factors represents only one aspect of psychological safety and cannot necessarily stand alone.4 46 The most widely used method to assess psychological safety is PSS, which is easy to use in a clinical setting5 44 but only provides a snapshot of the degree of psychological safety among HCPs. Still, a more refined understanding of the factors influencing and impacting psychological safety at our department is required before drawing any final conclusions. Tracking changes over time across various teams, departments and specialties within the same organisation and across a variety of different organisations would provide valuable information towards achieving adequate understanding. To shed more light on the subtleties of psychological safety, an assortment of approaches such as interviews, observations and surveys can be used, as O’Donovan et al suggested.46 Combining these methods strengthens the understanding of how and why psychological safety influences work and how it is linked to outcomes and antecedents.5
Using SSC involves verbally confirming that all items on the checklist have been reviewed. When used as intended, it can facilitate effective teamwork and communication among all HCPs on a surgical team regardless of professional role.24 For it to work optimally, all OR HCPs must feel that it is safe to be candid in their work environment. Research shows that psychological safety is a prerequisite for creating an environment that promotes speaking up1 47 and that good psychological safety outcomes are linked to better communication, knowledge sharing and voice behaviour.5 This suggests that better psychological safety may lead to better compliance towards using SSC.
Our study data represent a starting point for understanding the variations in HCP perceptions of SSC and how these perceptions relate to the level of psychological safety among providers. Our finding that HCPs who feel less psychologically safe are more likely to perceive the checklist as time-consuming underscores the importance of psychological safety in fostering trust and confidence within interdisciplinary teams. When individuals do not feel secure in expressing concerns or questions without fear of repercussions, they may perceive any additional task, such as completing the checklist, as burdensome or unwarranted. Conversely, higher levels of psychological safety may foster greater confidence in SSC, leading to increased compliance. Specifically, a high level of psychological safety was associated with the perception that the SSC strengthens teamwork inside the OR and that colleagues listen when SSC items are being reviewed. This indicates that psychological safety may influence the perception of SSC as a tool for enhancing interdisciplinary teamwork and how we listen to our colleagues. Our survey did not exhaustively investigate factors that may contribute to better interdisciplinary teamwork, which is why it is important to consider other safety factors and dimensions across multiple levels (individual, team and organisational) that impact teamwork48 49 and psychological safety5 in the OR.
When team members feel supported and respected within their work environment, they are more likely to view safety protocols positively and recognise their value in promoting patient well-being. These insights underscore the critical role of psychological safety in shaping perceptions and behaviours related to patient safety initiatives such as SSC. Strategies aimed at enhancing psychological safety within healthcare teams may improve overall team dynamics and bolster confidence in the efficacy of safety protocols, ultimately leading to better compliance and patient outcomes. Further research into interventions that reinforce psychological safety and their impact on checklist adherence could provide valuable insights for enhancing patient safety in surgical settings.
Strengths
One of the strengths of this study is that five different HCP groups participated and that there was a high overall response rate (86%), which is considered good compared with other surveys involving HCPs.50 Another strength is that the survey was developed using a combination of semi-structured interviews with representatives from the target group. Moreover, to ensure a transparent translation process for the Danish translation of Edmondson’s widely used and validated PSS3, we used a forward-backward method. Finally, participants who completed the survey did so anonymously, which may encourage great honesty and candour in responses, especially for sensitive topics concerning the perception of SSC and psychological safety.
Limitations
Our study has several limitations. First, our initial semi-structured interviews on the use of SSC contained open-ended questions, posing the risk of interviewer bias influencing response interpretation. Moreover, participants may have been susceptible to social desirability bias or other influences impacting response accuracy and completeness. They might have tailored their answers to align with perceived interviewer expectations rather than expressing genuine thoughts or experiences. Given the small sample size (n=8), the semi-structured interview findings may not readily apply to larger populations. Additionally, our study population represents only a single centre, with 100 participants completing the entire survey. Consequently, caution is advised when extrapolating these results to different contexts or demographics. In addition, using a quantitative scale can potentially leave out valuable information, although this risk was compensated for with the addition of a free-text option to the survey. Furthermore, it is uncertain whether the 12 SSC items we selected are sufficient enough to fully cover how OR staff perceive SSC.
Given our limited sample, we chose to do face validity testing since conducting a full psychometric evaluation that included explanatory factor analysis or confirmatory factor analysis would have been statistically underpowered and potentially misleading.
Lastly, we asked an overall general question about years of clinical experience and not specifically about participants’ years of experience in the Department of Gynaecology and Anaesthesiology. For future research, it is relevant to ask specifically about experience in the department in question since organisational culture affects psychological safety.4 Residents and gynaecologists have the fewest number of days in the OR per month, which is also considered a limitation when examining the culture in the OR.
Perspectives and future research
Future research must employ a variety of methodological approaches to gain a more in-depth understanding of the perceptions of various HCP groups have of SSC and of their level of psychological safety.
To expand the current understanding, the surveys should be distributed to other surgical specialties and be supported by qualitative studies. It would, for example, be interesting to look at specific cases and teams to observe how SSC is used and to determine the level of psychological safety. Any new knowledge acquired must be used to target and create interventions to establish and sustain a psychologically safe environment among all HCP groups51 but also to ensure a more compliant use of SSC.
Conclusion
In summary, an association was found between HCP perceptions of SSC and their level of psychological safety. Specifically, increased psychological safety was linked to more positive views on the checklist’s role in enhancing interdisciplinary teamwork, creating structure and the feeling of people listening when the checklist is reviewed. While perceptions of the checklist as time-consuming were associated with lower psychological safety ratings. These results suggest that psychological safety may impact views and actions related to patient safety measures like the checklist, highlighting the importance of fostering a supportive environment to optimise safety practices. However, these findings should be interpreted with caution by acknowledging the potential influence of other factors on psychological safety and SSC. Initiatives directed at fortifying psychological safety within healthcare teams have the potential to foster better team dynamics and instil greater trust in safety protocols.
supplementary material
Acknowledgements
The authors would like to thank the healthcare professionals at the Department of Gynaecology and the Department of Anaesthesiology at the Juliane Marie Centre, Copenhagen University Hospital – Rigshospitalet for their participation in this study. Sincere thanks to OWM for the work in developing the questions for this survey as part of your master thesis in medicine at the Faculty of Health and Medical Sciences - University of Copenhagen entitled "Operating room staff's perceptions of the World Health Organization's Surgical Safety Checklist and psychological safety: Development and validation of a scientific questionnaire".
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants and was approved by the Danish Data Protection Agency in May 2022 (P-2022-275). Approval was not required from the Danish National Committee on Health Research Ethics. Participants gave informed consent to participate in the study before taking part.
Data availability free text: The data can be shared upon reasonable request to the corresponding author.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Contributor Information
Kjestine Emilie Møller, Email: kjestine.emilie.moeller@regionh.dk.
Olivia Wisborg McLeskey, Email: olivia.wisborg.mcleskey@regionh.dk.
Susanne Rosthøj, Email: suro@cancer.dk.
Patricia Trbovich, Email: patricia.trbovich@uhn.ca.
Teodor Grantcharov, Email: teodor@stanford.edu.
Jette Led Sorensen, Email: jette.led.soerensen@regionh.dk.
Jeanett Strandbygaard, Email: jeanett.strandbygaard@regionh.dk.
Data availability statement
Data are available upon reasonable request.
References
- 1.Lyndon A, Sexton JB, Simpson KR, et al. Predictors of likelihood of speaking up about safety concerns in labour and delivery. BMJ Qual Saf. 2012;21:791–9. doi: 10.1136/bmjqs-2010-050211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schwappach D, Richard A. Speak up-related climate and its association with healthcare workers’ speaking up and withholding voice behaviours: a cross-sectional survey in Switzerland. BMJ Qual Saf. 2018;27:827–35. doi: 10.1136/bmjqs-2017-007388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edmondson A. Psychological Safety and Learning Behavior in Work Teams. Adm Sci Q. 1999;44:350–83. doi: 10.2307/2666999. [DOI] [Google Scholar]
- 4.O’donovan R, Mcauliffe E. A systematic review of factors that enable psychological safety in healthcare teams. Int J Qual Health Care. 2020;32:240–50. doi: 10.1093/intqhc/mzaa025. [DOI] [PubMed] [Google Scholar]
- 5.Newman A, Donohue R, Eva N. Psychological safety: A systematic review of the literature. Hum Resour Manag Rev. 2017;27:521–35. doi: 10.1016/j.hrmr.2017.01.001. [DOI] [Google Scholar]
- 6.Appelbaum NP, Dow A, Mazmanian PE, et al. The effects of power, leadership and psychological safety on resident event reporting. Med Educ. 2016;50:343–50. doi: 10.1111/medu.12947. [DOI] [PubMed] [Google Scholar]
- 7.Edmondson AC, Lei Z. Psychological Safety: The History, Renaissance, and Future of an Interpersonal Construct. Annu Rev Organ Psychol Organ Behav. 2014;1:23–43. doi: 10.1146/annurev-orgpsych-031413-091305. [DOI] [Google Scholar]
- 8.Edmondson AC. Framing for Learning: Lessons in Successful Technology Implementation. Calif Manage Rev. 2003;45:34–54. doi: 10.2307/41166164. [DOI] [Google Scholar]
- 9.WHO [01-Jun-2023]. https://www.who.int/publications/i/item/9789240010338 Available. accessed.
- 10.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–9. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 11.Ramsay G, Haynes AB, Lipsitz SR, et al. Reducing surgical mortality in Scotland by use of the WHO Surgical Safety Checklist. Br J Surg. 2019;106:1005–11. doi: 10.1002/bjs.11151. [DOI] [PubMed] [Google Scholar]
- 12.de Vries EN, Prins HA, Crolla RMPH, et al. Effect of a comprehensive surgical safety system on patient outcomes. N Engl J Med. 2010;363:1928–37. doi: 10.1056/NEJMsa0911535. [DOI] [PubMed] [Google Scholar]
- 13.Bergs J, Hellings J, Cleemput I, et al. Systematic review and meta-analysis of the effect of the World Health Organization surgical safety checklist on postoperative complications. Br J Surg. 2014;101:150–8. doi: 10.1002/bjs.9381. [DOI] [PubMed] [Google Scholar]
- 14.Lübbeke A, Hovaguimian F, Wickboldt N, et al. Effectiveness of the surgical safety checklist in a high standard care environment. Med Care. 2013;51:425–9. doi: 10.1097/MLR.0b013e31828d1489. [DOI] [PubMed] [Google Scholar]
- 15.Urbach DR, Govindarajan A, Saskin R, et al. Introduction of surgical safety checklists in Ontario, Canada. N Engl J Med. 2014;370:1029–38. doi: 10.1056/NEJMsa1308261. [DOI] [PubMed] [Google Scholar]
- 16.Conley DM, Singer SJ, Edmondson L, et al. Effective surgical safety checklist implementation. J Am Coll Surg. 2011;212:873–9. doi: 10.1016/j.jamcollsurg.2011.01.052. [DOI] [PubMed] [Google Scholar]
- 17.Cullati S, Le Du S, Raë A-C, et al. Is the Surgical Safety Checklist successfully conducted? An observational study of social interactions in the operating rooms of a tertiary hospital. BMJ Qual Saf. 2013;22:639–46. doi: 10.1136/bmjqs-2012-001634. [DOI] [PubMed] [Google Scholar]
- 18.Pickering SP, Robertson ER, Griffin D, et al. Compliance and use of the World Health Organization checklist in U.K. operating theatres. Br J Surg. 2013;100:1664–70. doi: 10.1002/bjs.9305. [DOI] [PubMed] [Google Scholar]
- 19.Riley MS, Etheridge J, Palter V, et al. Remote Assessment of Real-World Surgical Safety Checklist Performance Using the OR Black Box: A Multi-Institutional Evaluation. J Am Coll Surg. 2024;238:206–15. doi: 10.1097/XCS.0000000000000893. [DOI] [PubMed] [Google Scholar]
- 20.Al Abbas AI, Sankaranarayanan G, Polanco PM, et al. The Operating Room Black Box: Understanding Adherence to Surgical Checklists. Ann Surg. 2022;276:995–1001. doi: 10.1097/SLA.0000000000005695. [DOI] [PubMed] [Google Scholar]
- 21.Muensterer OJ, Kreutz H, Poplawski A, et al. Timeout procedure in paediatric surgery: effective tool or lip service? A randomised prospective observational study. BMJ Qual Saf. 2021;30:622–7. doi: 10.1136/bmjqs-2020-012001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sendlhofer G, Lumenta DB, Pregartner G, et al. Reality check of using the surgical safety checklist: A qualitative study to observe application errors during snapshot audits. PLoS ONE. 2018;13:e0203544. doi: 10.1371/journal.pone.0203544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown B, Bermingham S, Vermeulen M, et al. Surgical safety checklist audits may be misleading! Improving the implementation and adherence of the surgical safety checklist: a quality improvement project. BMJ Open Qual. 2021;10:e001593. doi: 10.1136/bmjoq-2021-001593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gillespie BM, Withers TK, Lavin J, et al. Factors that drive team participation in surgical safety checks: a prospective study. Pat Saf Surg. 2016;10:3. doi: 10.1186/s13037-015-0090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paterson C, Mckie A, Turner M, et al. Barriers and facilitators associated with the implementation of surgical safety checklists: A qualitative systematic review. J Adv Nurs. 2024;80:465–83. doi: 10.1111/jan.15841. [DOI] [PubMed] [Google Scholar]
- 26.Elm E von, Altman DG, Egger M, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kallio H, Pietilä A-M, Johnson M, et al. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016;72:2954–65. doi: 10.1111/jan.13031. [DOI] [PubMed] [Google Scholar]
- 28.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 29.WHO [-Mar-2024]. https://www.coursehero.com/file/30372721/WHO-Process-of-translation-and-adaptation-of-instrumentspdf Available. accessed.
- 30.Fayers PM, Machin D. Quality of Life: The Assessment, Analysis and Reporting of Patient-Reported Outcomes. 3rd. Newark: John Wiley & Sons, Incorporated; 2016. edn. [Google Scholar]
- 31.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Austria: R Foundation for Statistical Computing V; A language and environment for statistical computing.https://www.R-project.org Available. [Google Scholar]
- 34.Urban D, Burian BK, Patel K, et al. Surgical Teams’ Attitudes About Surgical Safety and the Surgical Safety Checklist at 10 Years: A Multinational Survey. Ann Surg Open. 2021;2:e075. doi: 10.1097/AS9.0000000000000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pugel AE, Simianu VV, Flum DR, et al. Use of the surgical safety checklist to improve communication and reduce complications. J Infect Public Health. 2015;8:219–25. doi: 10.1016/j.jiph.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nationale kompetencekort for nyansatte operationssygeplejersker uden operationserfaring In Danish. https://dsr.dk/media/ws3p4xp1/national_kompetencekort_-_operationssygeplejersker_uden_operationserfaring_gaeldende_4.pdf n.d. Available.
- 37.Dixon JL, Mukhopadhyay D, Hunt J, et al. Enhancing surgical safety using digital multimedia technology. Am J Surg. 2016;211:1095–8. doi: 10.1016/j.amjsurg.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 38.Martis WR, Hannam JA, Lee T, et al. Improved compliance with the World Health Organization Surgical Safety Checklist is associated with reduced surgical specimen labelling errors. N Z Med J. 2016;129:63–7. [PubMed] [Google Scholar]
- 39.Haugen AS, Sevdalis N, Søfteland E. Impact of the World Health Organization Surgical Safety Checklist on Patient Safety. Anesthesiology. 2019;131:420–5. doi: 10.1097/ALN.0000000000002674. [DOI] [PubMed] [Google Scholar]
- 40.Weiser TG, Haynes AB. Ten years of the Surgical Safety Checklist. Br J Surg. 2018;105:927–9. doi: 10.1002/bjs.10907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behavior. 2006;27:941–66. doi: 10.1002/job.413. [DOI] [Google Scholar]
- 42.Strandbygaard J, Dose N, Moeller KE, et al. Healthcare professionals’ perception of safety culture and the Operating Room (OR) Black Box technology before clinical implementation: a cross-sectional survey. BMJ Open Qual. 2022;11:e001819. doi: 10.1136/bmjoq-2022-001819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu RQ, Davidson J, Van Hooren TA, et al. Impostorism and anxiety contribute to burnout among resident physicians. Med Teach. 2022;44:758–64. doi: 10.1080/0142159X.2022.2028751. [DOI] [PubMed] [Google Scholar]
- 44.McClintock AH, Fainstad T, Blau K, et al. Psychological safety in medical education: A scoping review and synthesis of the literature. Med Teach. 2023;45:1290–9. doi: 10.1080/0142159X.2023.2216863. [DOI] [PubMed] [Google Scholar]
- 45.Lases LSS, Arah OA, Busch ORC, et al. Learning climate positively influences residents’ work-related well-being. Adv Health Sci Educ Theory Pract. 2019;24:317–30. doi: 10.1007/s10459-018-9868-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.O’Donovan R, McAuliffe E. Exploring psychological safety in healthcare teams to inform the development of interventions: combining observational, survey and interview data. BMC Health Serv Res. 2020;20:810. doi: 10.1186/s12913-020-05646-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schwappach D, Sendlhofer G, Häsler L, et al. Speaking up behaviors and safety climate in an Austrian university hospital. Int J Qual Health Care. 2018;30:701–7. doi: 10.1093/intqhc/mzy089. [DOI] [PubMed] [Google Scholar]
- 48.Arad D, Finkelstein A, Rozenblum R, et al. Patient safety and staff psychological safety: A mixed methods study on aspects of teamwork in the operating room. Front Public Health. 2022;10:1060473. doi: 10.3389/fpubh.2022.1060473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Etherington C, Burns JK, Kitto S, et al. Barriers and enablers to effective interprofessional teamwork in the operating room: A qualitative study using the Theoretical Domains Framework. PLoS ONE. 2021;16:e0249576. doi: 10.1371/journal.pone.0249576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cho YI, Johnson TP, Vangeest JB. Enhancing surveys of health care professionals: a meta-analysis of techniques to improve response. Eval Health Prof. 2013;36:382–407. doi: 10.1177/0163278713496425. [DOI] [PubMed] [Google Scholar]
- 51.O’Donovan R, McAuliffe E. A systematic review exploring the content and outcomes of interventions to improve psychological safety, speaking up and voice behaviour. BMC Health Serv Res. 2020;20:101. doi: 10.1186/s12913-020-4931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request.