Abstract
Background
Hypertension is the leading modifiable risk factor for premature death globally despite the existence of evidence-based and cost-effective treatments. Medication nonadherence is cited as the main cause of treatment failure for hypertension. In Peru, adherence to anti-hypertensive medications of individuals with both hypertension and type 2 diabetes (T2D) is not well studied. The few studies that have investigated differences in anti-hypertensive medication adherence among patients with and without T2D have demonstrated both positive and negative effects.
Methods
In a cross-sectional study in Puno, Peru, we compared anti-hypertensive medication adherence in individuals with hypertension between those with and without comorbid T2D. The primary outcome was adherence to anti-hypertensive medications as assessed by the Hill-Bone Compliance scale. The primary exposure variable was comorbidity status (i.e., having hypertension and diabetes vs. hypertension alone).
Results
Of the 204 participants with hypertension (mean age 67 ± 11 years, 60% female), 42 (21%) had comorbid diabetes. Participants with comorbid disease had higher overall anti-hypertensive adherence scores (49.5 ± 2.8 vs. 48.0 ± 4.1 points; p<0.001) and higher medication adherence scores (32.8 ± 2.2 vs. 31.3 ± 3.7 points; p<0.01) when compared to those with hypertension alone. In multivariable regression, comorbid diabetes and monthly income above 250 soles (68 USD) were associated with higher Hill-Bone Compliance scale scores by 1.5 ± 0.7 points (p=0.025) and 2.0 ± 0.7 points (p<0.01), respectively.
Conclusions
Participants with comorbid hypertension and diabetes exhibited higher adherence to anti-hypertensive medications when compared to those with hypertension alone, suggesting that individuals with comorbid disease are more likely to adhere to anti-hypertensive medications.
Keywords: hypertension, type 2 diabetes mellitus, medication adherence, Peru, Hill-Bone Scale
Introduction
Hypertension is the leading modifiable risk factor for premature death worldwide despite the existence of evidence-based and cost-effective treatment. 1 In 2021, hypertension control was reported at 8% in low-and-middle-income countries (LMICs). 2 Adherence studies conducted in LMICs including Colombia, Ghana, and Bangladesh have reported wide ranges of non-adherence to anti-hypertensive medications from 24 to 70%.3–5 Adherence has not been widely studied in Peru; however, in 2016, the CRONICAS cohort study found control rates remain low at an average of 30%, suggesting high rates of treatment noncompliance. 6
Additionally, studies have linked type 2 diabetes mellitus (T2D) to a higher probability of comorbid hypertension relative to other non-communicable diseases (NCDs).7,8 Many of the studies that have investigated the effect of comorbid hypertension and T2D on anti-hypertensive medication adherence have reported both higher or lower adherence rates 4,9–11 when compared to those who only have hypertension. Thus, understanding treatment adherence trends in patients with multiple NCDs is difficult.
In Peru, the 2019 Encuesta Demográfica y de Salud Familiar (ENDES), a national survey administered using direct interviews, estimated the national prevalence of hypertension and pre-hypertension at 20% and 34%, respectively.12,13 The CRONICAS study, which followed a Peruvian cohort for three years to characterize NCD prevalence and burden, reported a T2D prevalence of 6.7% in Peru. 14 The PERUDIAB study found that 40% of individuals with T2D were previously undiagnosed. 15 In Peru, changes in diet, behaviors, and environmental factors, coupled with an aging population, have led to an epidemiologic shift associated with higher rates of both hypertension and T2D. 13 Particularly vulnerable populations in Peru are indigenous Andean groups, including the Aymara and Quechua, who have the least access to care and a prevalence of hypertension over 18% in older adults. 16
The Addressing Hypertension and Diabetes through Community-Engaged Systems in Puno, Peru (ANDES) trial is investigating the use of a multi-component community health worker (CHW) intervention aimed at reducing hypertension in a high-risk, underrepresented population (NCT05524987). During formative work, we aimed to characterize anti-hypertensive medication adherence in participants with and without comorbid T2D. We hypothesized that adherence would be different between individuals with hypertension and those with hypertension and comorbid T2D.
Methods
Study design and setting
We report a secondary analysis of data from the ANDES trial, including data from the formative pilot study (conducted between April and August 2022) and early baseline data from the trial (collected between March 2023 and September 2023). Puno, Peru is a rural, high-altitude Andean region with a significant indigenous population.13,17 Eligible participants were identified through a combination of health fairs and patient registries. 18 To be eligible, all ANDES participants had a previous diagnosis of hypertension and were on anti-hypertensive medication. We used the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines in preparing this work. 19
Data collection
Data for this analysis was collected by field staff during a baseline in-home visit. Surveys were administered by trained field staff in Spanish or translated to local languages as necessary. Participants self-reported their answers to field staff, who recorded responses using digital tablets. Other questionnaires and health measures were collected and reported separately. Blood pressure measurements were taken in triplicate by CHWs, and the average blood pressure measurement was used for analysis. We included all eligible participants from the pilot study as well as main trial participants who were enrolled before 19 September 2023. Those enrolled after this date were not included in this analysis, and when individuals participated in both the pilot and main trial, only the pilot data was retained for analysis. All data were collected and managed using Research Electronic Data Capture (REDCap).20,21
Questionnaires
Treatment adherence to anti-hypertensive medications, the primary outcome variable, was assessed using the Hill-Bone Compliance scale. This scale was developed and validated to assess anti-hypertensive therapy adherence. 22 It is widely used for research purposes, and it is free to use and easy to interpret. A Spanish-validated version does not currently exist. We independently translated and field tested the questionnaire before roll-out. Disagreements between two translators were resolved by discussion. All forms were field tested with CHWs in Puno to ensure understanding in the local context.
The Hill-Bone Compliance scale consists of 14 questions and three subscales that use a Likert scale to assess three key components of treatment compliance: reducing sodium intake, appointment keeping, and medication taking. The Hill-Bone Compliance scale ranges from 14 to 56 with higher scores indicating better medication adherence and expected greater compliance with blood pressure control behaviors. 22 Subscale analysis of medication adherence was calculated by summing nine of the 14 items with a maximum score of 36 points. 22 This subscale focuses on prescription filling habits, forgetfulness, and intentionally deciding not to take anti-hypertensive medications. Total scores for the dietary sodium and appointment keeping subscales can have a maximum score of eight and 12 points, respectively. 22
We assessed self-reported comorbid T2D via a health history questionnaire. This questionnaire was based on previous work in Puno. 14 The topics included previous diagnoses of various chronic diseases, time since diagnosis, and family history.
We collected sociodemographic characteristics using a modified version of the ENDES questionnaire. 17
Statistical analysis
The primary outcome of this analysis was adherence to anti-hypertensive medications using the Hill-Bone Compliance scale. Descriptive statistics were calculated using percentages and cross-tabulation of variables. Sample normality was assessed by comparing distributions of residuals and assumed normal by the Central Limit Theorem due to the sample size being over 100. 23 Any non-responses were noted during descriptive analysis and excluded from statistical analysis. For continuous (and ordinal approximating continuous) variables including age, adherence scores, and subset scores, Welch’s two sample t-tests were performed to determine differences between groups. A Chi-squared test was performed for categorical variables to determine significant differences between groups. Single variable and multivariable linear regression were performed to infer associations with adherence and disease status. The most parsimonious model was selected using the Akaike information criterion (AIC).24,25 This model included age, comorbid diabetes, and household income variables and excluded variables for district, sex, insurance type, education level, primary language, and marital status. We conducted data analysis in the statistical package R (version 4.2.1). 26
Ethical considerations
All participants provided written informed consent after research staff read the consent documents in their entirety, translated into local languages where appropriate. Informed consents were obtained by signature or fingerprint according to the participant’s level of literacy with an additional research staff member present as a witness. The pilot and main studies were approved by the institutional review boards of Universidad Peruana Cayetano Heredia (formative work and main trial: IRB104372), Washington University in St. Louis (formative work: IRB202108158; trial: IRB202301183), and Johns Hopkins University (formative work: IRB00345868; trial: IRB00405654).
Results
Validation of the medication adherence scores
The internal consistency of the Hill-Bone Compliance scale and medication adherence subscales were assessed using Cronbach’s alpha (α = 0.61 and α = 0.69, respectively).
Participant characteristics
A total of 217 participants completed the Hill-Bone Compliance scale; 13 records were excluded due to data collection errors in which field workers allowed non-standardized answers that invalidated some questionnaires. In total, data from 204 participants were analyzed; 79% (n = 162) had hypertension only and 21% (n = 42) had comorbid hypertension and T2D. All participants were prescribed medication to manage their hypertension. Population characteristics are presented in Table 1. Overall, the sample was 60% female (n = 122), with no significant difference in sex between groups. The mean age of the sample population was 67 ± 11 years. Most participants (67%; n = 137) were married, while some were widowed (19%; n = 39). Most participants (80%, n = 160) lived in a peri-urban district, 77% (n = 157) reported a monthly household income of 250 soles ($68 USD 27 ) or more, and 62% (n = 126) achieved higher than a secondary level of education. While 78% (n = 160) of participants spoke primarily Spanish, 9% (n = 19) and 12% (n = 25) spoke primarily Quechua and Aymara, respectively. A statistically significant positive trend was found between T2D and monthly household income greater than 250 soles. Among participants with T2D, 85.7% (n = 36) reported taking anti-hyperglycemic medications.
Table 1.
Descriptive characteristics of 204 individuals with hypertension or comorbid hypertension and T2D in Puno, Peru.
| Characteristic | Overall, N = 204 1 | Hypertension Only, N = 162 1 | Comorbid Hypertension and T2D, N = 42 1 | p-value 2 |
|---|---|---|---|---|
| Age (years) | 67 (11) | 67 (12) | 67 (9) | 0.95 |
| Sex | 0.36 | |||
| Female | 60% (122) | 62% (100) | 52% (22) | |
| Male | 40% (82) | 38% (62) | 48% (20) | |
| District | 0.68 | |||
| Acora | 14% (29) | 16% (25) | 9.8% (4) | |
| Chucuito | 5.5% (11) | 5.6% (9) | 4.9% (2) | |
| Puno | 80% (161) | 79% (126) | 85% (35) | |
| Insurance | 0.63 | |||
| EsSalud | 70% (142) | 69% (111) | 74% (31) | |
| SIS | 30% (62) | 31% (51) | 26% (11) | |
| Educational Attainment | 0.58 | |||
| Secondary or less | 38% (78) | 40% (64) | 33% (14) | |
| Over secondary | 62% (126) | 60% (98) | 67% (28) | |
| Household Income | 0.63 | |||
| <250 soles | 23% (47) | 24% (39) | 19% (8) | |
| 250 soles or more | 77% (157) | 76% (123) | 81% (34) | |
| Primary Language | 0.05* | |||
| Indigenous + | 21% (42) | 23% (41) | 3.8% (1) | |
| Spanish | 79% (162) | 77% (137) | 96% (25) | |
| Marital status | 0.21 | |||
| Married | 67% (137) | 70% (113) | 57% (24) | |
| Separated/Divorced | 6.9% (14) | 6.2% (10) | 9.5% (4) | |
| Single | 6.4% (13) | 6.2% (10) | 7.1% (3) | |
| Widowed | 19% (39) | 18% (29) | 24% (10) | |
| No response | 0.5% (1) | 0% (0) | 2.4% (1) |
1Mean (SD); % (n),
2*p < 0.05; **p < 0.01; ***p < 0.001.
+In total, 9% (19) of participants spoke Quechua (9% of those with hypertension and 10% of those with comorbid hypertension and T2D) and 12% (25) spoke Aymara (15% of those with hypertension and 2% of those with comorbid hypertension and T2D).
Adherence to hypertension treatment
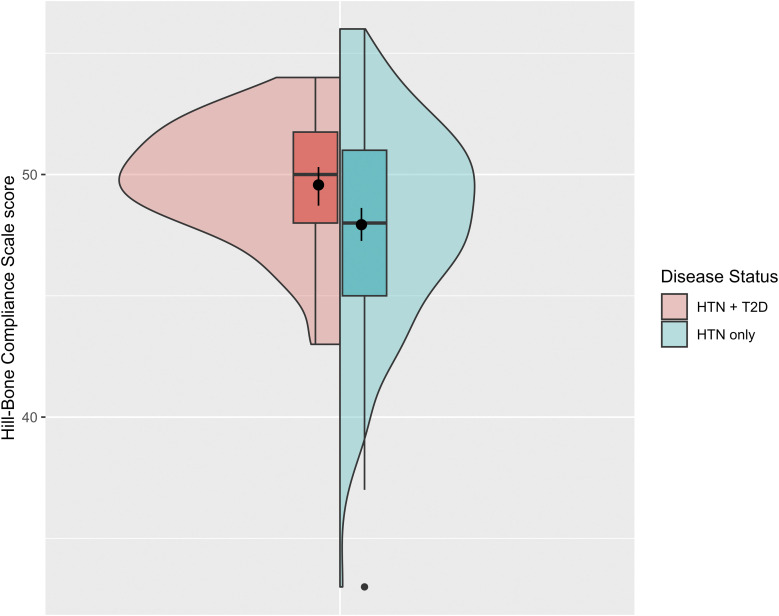
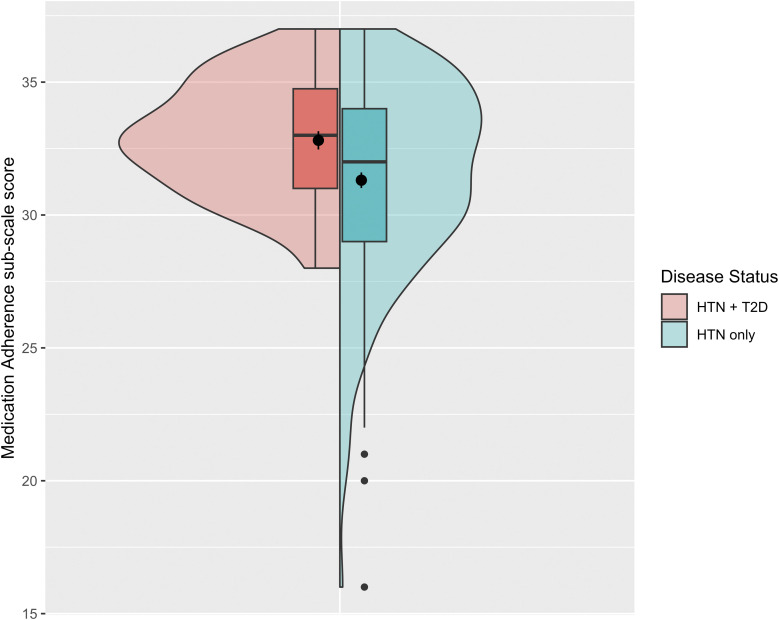
The mean Hill-Bone Compliance scale score measuring adherence to anti-hypertensive treatment was 49.6 ± 2.6 points and 47.9 ± 4.3 points in the comorbid hypertension and T2D group and hypertension only group, respectively (p <0.001) (Figure 1). Mean anti-hypertensive Medication Adherence sub-scale scores were 31.3 ± 3.7 points for the hypertension only group and 32.8 ± 2.2 points for the comorbid hypertension and T2D group (p <0.01) (Figure 2). Systolic blood pressure and diastolic blood pressure were lower in the comorbid hypertension and T2D group when compared to hypertension alone, however this difference was not found to be statistically significant. In both analyses, variability of the range was reduced in the comorbid hypertension and T2D group. The two additional sub-scales, appointment keeping and reduced salt intake, did not demonstrate significant differences between groups. These outcomes are presented in Table 2.
Figure 1.
Hill-Bone Compliance scale scores by disease status. Mean Hill-Bone Score was higher in those with hypertension (HTN) and type 2 diabetes (T2D) when compared to those with only hypertension (49.6 vs. 47.9 points, respectively). There was also more variability in the HTN only group (range of scores from 33 to 56 points) when compared to the HTN + T2D group (range of scores from 43 to 54 points). We displayed boxplots and overlaid density plots for each group. We also plotted mean scores and corresponding 95% confidence intervals with a filled circle and vertical line for each group.
Figure 2.
Medication Adherence sub-scale scores by disease status. Similar to the Hill-Bone Compliance scale, Medication Adherence sub-scale scores were higher in those with hypertension (HTN) and T2D compared to those with only hypertension (32.8 vs. 31.3 points, respectively). There was again a larger degree of variability in the HTN only group (range of scores from 16 to 37 points) when compared to the HTN + T2D group (range of scores 28 to 37 points). We also plotted mean scores and corresponding 95% confidence intervals with a filled circle and vertical lines for each group.
Table 2.
Mean adherence scores and blood pressure by group.
| Outcome | Overall, N = 204 1 | Hypertension Only, N = 162 1 | Comorbid Hypertension and T2D, N = 42 1 | p-value 2 |
|---|---|---|---|---|
| Hill-Bone Compliance scale score (points) | 48.3 (4.0) | 47.9 (4.3) | 49.6 (2.6) | <0.01* |
| Subscales (points) | ||||
| Medication adherence | 31.6 (3.5) | 31.3 (3.7) | 32.8 (2.2) | <0.01* |
| Appointment keeping | 5.98 (1.27) | 5.98 (1.33) | 5.98 (1.05) | 0.98 |
| Reduced salt | 10.67 (1.18) | 10.64 (1.17) | 10.79 (1.24) | 0.50 |
| Blood pressure (mm Hg) | ||||
| Systolic | 137.8 (20.8) | 138.5 (20.7) | 133.2 (21.3) | 0.33 |
| Diastolic | 77.0 (13.2) | 77.6 (13.7) | 74.7 (10.9) | 0.15 |
1Mean (SD);
2*p < 0.05; **p < 0.01; ***p < 0.001.
Means and standard deviations of both groups independently and combined between groups. The main outcome of Hill-Bone Compliance score and the sub-scale medication adherence scores are both statistically different between groups, with increased variability in the hypertension only group.
Association between adherence to anti-hypertensive medications, comorbid T2D, and household income
A regression model including comorbid hypertension and T2D, age, and household income was judged to be the most parsimonious model. Having comorbid hypertension and T2D was associated with a higher adherence score. Having a monthly household income greater than or equal to 250 soles was also positively associated with higher adherence scores (Table 3). Equivalent regression models investigated these factors related to the Medication Adherence sub-scale score with comparable results (Table 4).
Table 3.
Linear regression coefficients for age, disease status, and household income on Hill-Bone Compliance scores.
| Characteristic | Mean difference in score | SE 2 | p-value 3 | 95% CI 4 |
|---|---|---|---|---|
| Age 1 in years | 0.04 | 0.40 | 0.93 | [-0.74, 0.82] |
| Comorbid diabetes (hypertension alone is reference) | 1.5 | 0.68 | 0.025* | [0.19, 2.9] |
| Household income 250 soles or more (< 250 soles is reference) | 2.0 | 0.68 | <0.01** | [0.61, 3.3] |
1Coefficient presented in terms of covariate interquartile range (15.5 years);
2SE = Standard Error;
3*p < 0.05; **p < 0.01; ***p < 0.001;
4CI = Confidence Interval.
Regression coefficients from the model determined to have best predictive value by AIC are presented with 95% confidence intervals and p-values. There is a statistically significant positive trend with T2D diagnosis and household income greater than 250 soles.
Table 4.
Linear regression coefficients for age, disease status, and household income on Medication Adherence sub-scale scores.
| Characteristic | Mean difference in score | SE 2 | p-value 3 | 95% CI 4 |
|---|---|---|---|---|
| Age 1 in years | 0.10 | 0.34 | 0.77 | [-0.57, 0.77] |
| Comorbid diabetes (hypertension alone is reference) | 1.4 | 0.59 | 0.02* | [0.24, 2.6] |
| Household income 250 soles or more (< 250 soles is reference) | 2.0 | 0.59 | <0.001*** | [0.87, 3.2] |
1Coefficient presented in terms of covariate interquartile range (15.5 years);
2SE = Standard Error;
3*p < 0.05; **p < 0.01; ***p < 0.001;
4CI = Confidence Interval.
Regression coefficients from the model determined to have best predictive value by AIC are presented with 95% confidence intervals and p-values.
Discussion
In this study, we found higher adherence to hypertension treatment in participants with comorbid T2D compared to that in participants with hypertension only. A reduction in variability may indicate that not only is adherence better in the comorbid group, but that comorbid patients are more consistent in their adherence behaviors as a group.
Several adherence studies in LMICs have shown that individuals with hypertension do not understand the risk associated with nonadherence because they do not generally experience symptoms without medication.28,29 Individuals with untreated T2D, by contrast, likely experience symptoms without treatment leading them to be more adherent.11,29 Additionally, individuals with T2D and hypertension are more likely to experience worse cardiovascular outcomes than those who only have hypertension, likely encouraging them to be adherent to treatment4,11,29. Better adherence is also often linked to higher socioeconomic status.9,30 Household income greater than or equal to 250 soles monthly was associated with improved adherence scores by regression analysis. Sub-scale analysis revealed that this difference is primarily related to hypertension medication adherence. Higher wealth index also allows for improved access to medications and providers.9,29 While this study did not see significant differences in household income between groups, many studies cite higher wealth as a risk factor for T2D and a facilitator to treatment access.9,30,31 This analysis was unable to examine interaction between comorbid T2D and household income due to sample size, except to say they are related. This warrants further exploration of the impact of household income on adherence, and how it may interact with different chronic diseases.
The Hill-Bone Compliance scale measures treatment compliance across several facets, however, only medication adherence differed significantly between groups. The comorbid group had higher medication adherence scores with a similar trend in range variability, suggesting that differences in overall adherence between these two groups can be explained by medication adherence. This may be explained by exacerbated symptoms in comorbid patients, as previously described, but this may not be the whole picture. Some of the most common reasons for non-adherence to hypertension medication are side effects.5,9,11 Although we did not measure side-effects in this study, these include dizziness, headaches, lower limb swelling, stomach discomfort, and/or reduced sexual drive.5,11 If a patient experiences side effects, but no noticeable worsening of hypertension symptoms without medication, they are less inclined to adhere. 30 Recent studies have linked drug type to patient adherence, with angiotensin-converting enzyme (ACE) inhibitors and diuretics being the most tolerable hypertension medications.5,28 Generally, in patients with comorbid hypertension and T2D, the official recommendation from the Peruvian Ministry of Health (MINSA, for the Spanish acronym) is for ACE inhibitors over calcium channel blockers, which could contribute to why these patients are more tolerant and adherent to their medication.32–34
Historically, research has shown that a higher disease burden contributes to reduced treatment adherence.4,10,29 The increased pressure to comply can be overwhelming, often contributing to higher rates of depression among patients with multiple NCDs, which in turn adds to treatment nonadherence.28–30 However, more recent studies have linked poly-pill treatment plans and co-existing NCDs to higher rates of adherence.28,30 Patients with multiple NCDs, when compared to those with one illness, are more likely to have prior hospitalizations and perceive high risk of disability and/or death from treatment noncompliance.4,10 Previous studies suggest that these patients often have built relationships with providers and are more likely to trust their treatment recommendations. 11
Furthermore, a key non-modifiable risk factor for nonadherence is older age. Older patients are more likely to have multiple NCDs, yet there is an emerging divide on how this affects adherence.9,10 The participants had no significant difference in age between groups. Several studies cite older age as negatively impacting adherence due to a higher likelihood of cognitive decline, forgetfulness, and frailty.10,29 However, younger age has also demonstrated negative impact given difficulty coming to terms with a chronic treatment course. 3 The differing trends could be explained by differences in the definition of adherence between studies. 30 Several use self-reported scores, like ours, while others review hypertension medication used; all present significant variability.10,30,31 In general, adherence trends are highly context specific and based on more than sociodemographic factors.10,31
A strength of this study is the use of the Hill-Bone Compliance scale, a reliable measure of compliance validated across populations and contexts. 22 However, since both hypertension and T2D status were both self-reported, there is the potential for bias; therefore, a secondary, objective method for measuring adherence, such as blood or urine spectrometry analysis, is recommended for future work. In this participant group, 21% of participants did not speak Spanish as their primary language, instead they spoke Quechua or Aymara (indigenous languages). Thus, the sample size was too small to examine the impact of indigenous background on adherence. Another limitation was that we were unable to use a standardized version of the Hill Bone Compliance scale translated and validated in either Aymara or Quechua when we interviewed participants; however, it is important to note that most participants also spoke Spanish. For these participants, we relied on our community health workers who spoke Aymara and Quechua to help with Spanish words that required translation. Indeed, since the proportion of participants who spoke Spanish as their first language was high (79%), this effect was likely limited. Future studies, particularly those in regions with significant populations of indigenous speaking communities, should consider language as a variable and explore the impact on risk perception, provider engagement, and treatment adherence. Additionally, the small sample size of this analysis limits generalizability to a larger population. However, our analysis highlights potential trends in the relationship between comorbid hypertension and T2D and treatment adherence, which can be further explored in future work. Also, this study, like many others, only considers adherence to hypertension treatment even though both hypertension and T2D require life-long treatment.32,34 Research has shown that while individuals may be adherent to one treatment, they may not be adherent to all when having multiple chronic diseases.29,30 This leads to gaps in knowledge regarding the dynamic interactions between chronic diseases, patient behaviors, and health outcomes. The small sample size of this study also limits generalizability beyond the Puno population and did not allow for further stratification into participants who had hypertension and other comorbid conditions beyond T2D. Since other comorbid conditions in participants could contribute to differences in medication adherence between groups, this should be studied during the main ANDES trial. Additionally, due to wanting to avoid excessive burden to the participants during formative research, we did not collect some information that would have been interesting to study. For example, information on the number of medications participants were taking could have added additional variables to the analysis.
It is also important to consider the direct impact of each disease on an individual given that hypertension often does not have a significant impact on daily life, while T2D presents concerning symptoms that may deter delays in treatment. Understanding what level of symptoms and side effects patients find tolerable may help health professionals identify key opportunities to inspire adherence. Other patient level explanations for improved medication adherence in comorbid patients may be the impact of provider relationships, perception of CVD risk, or direct hypertension medication related factors such as side effects.
Our findings add to the growing body of evidence that hypertension medication adherence — especially among individuals with multiple NCDs is complex and increasingly important. A better understanding the drivers of adherence in individuals with complex care regimens is essential to develop health systems and practices such as educational plans and policies.
Acknowledgements
The authors wish to acknowledge healthcare system partners (MINSA, DIRESA, and EsSalud) and teams at the participating public health centers, as well as the A.B. PRISMA field staff.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by the National Heart, Lung, and Blood Institute (UG3 HL152371) U.S. National Institutes of Health (NIH), Bethesda, MD, U.S. (Multiple Principal Investigators: Hartinger, Checkley, Dávila-Román, Geng). This work was also supported in part by a research training grant in chronic, non-communicable respiratory diseases in Peru (D43TW011502; PI: Checkley) from the Fogarty International Center, NIH. This research represents the NIH's contribution to the Global Alliance for Chronic Diseases coordinated call on scaling-up evidence-based interventions. The funders were not involved in the development of the study design or collection, management, analysis, or interpretation of data. The program officer representing the National Heart, Lung, and Blood Institute participated in Data and Safety Monitoring Board activities.
Disclaimer: The content is solely the responsibility of the authors and does not represent the policy of the National Heart, Lung, and Blood Institute, National Institutes of Health, United States (U.S.) Department of Health and Human Services, or the U.S. Government.
Research material access: Please contact the corresponding author for any research material requests.
ORCID iDs
Parker K Acevedo https://orcid.org/0009-0007-9522-7038
Katherine E Lord https://orcid.org/0009-0000-7719-9108
Kendra N Williams https://orcid.org/0000-0001-9697-048X
Lucy Cordova-Ascona https://orcid.org/0000-0001-9262-9807
Gonzalo Cuentas https://orcid.org/0000-0002-5699-5030
William Checkley https://orcid.org/0000-0003-1106-8812
References
- 1.Guerrero-Díaz DV, Hernández-Vásquez A, Montoya-Rivera WC, et al. Undiagnosed hypertension in Peru: analysis of associated factors and socioeconomic inequalities, 2019. Heliyon. 2021; 7(7): e07516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schutte AE, Srinivasapura Venkateshmurthy N, Mohan S, et al. Hypertension in Low- and Middle-Income Countries. Circ Res. 2021; 128(7): 808–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khanam MA, Lindeboom W, Koehlmoos TL, et al. Hypertension: adherence to treatment in rural Bangladesh – findings from a population-based study. Glob Health Action. 2014; 7: 25028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parra DI, Romero Guevara SL, Rojas LZ. Influential Factors in Adherence to the Therapeutic Regime in Hypertension and Diabetes. Invest Educ Enferm. 2019; 37(3): e02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Woode E, Boakye‐Gyasi E, Obirikorang Y, et al. Predictors of medication nonadherence among hypertensive clients in a Ghanaian population: Application of the Hill‐Bone and Perceived Barriers to Treatment Compliance Scale. Health Sci Rep. 2022; 5(3): e584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quispe R, Benziger CP, Bazo-Alvarez JC, et al. The Relationship Between Socioeconomic Status and CV Risk Factors. Glob Heart. 2016; 11(1): 121–130.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lam AA, Lepe A, Wild SH, et al. Diabetes comorbidities in low- and middle-income countries: An umbrella review. J Glob Health. 2021;11:04040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen TN, Chow CK. Global and national high blood pressure burden and control. Lancet. 2021; 398(10304): 932–933. [DOI] [PubMed] [Google Scholar]
- 9.Hamrahian SM, Maarouf OH, Fülöp T. A Critical Review of Medication Adherence in Hypertension: Barriers and Facilitators Clinicians Should Consider. Patient Prefer Adherence. 2022; 16: 2749–2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jankowska-Polańska B, Świątoniowska-Lonc N, Karniej P, et al. Influential factors in adherence to the therapeutic regime in patients with type 2 diabetes and hypertension. Diabetes Res Clin Pract. 2021; 173: 108693. [DOI] [PubMed] [Google Scholar]
- 11.Schoenthaler A, Leon M, Butler M, et al. Development and Evaluation of a Tailored Mobile Health Intervention to Improve Medication Adherence in Black Patients With Uncontrolled Hypertension and Type 2 Diabetes: Pilot Randomized Feasibility Trial. JMIR Mhealth Uhealth. 2020; 8(9): e17135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chambergo-Michilot D, Rebatta-Acuña A, Delgado-Flores CJ, et al. Socioeconomic determinants of hypertension and prehypertension in Peru: Evidence from the Peruvian Demographic and Health Survey. Plos One. 2021; 16(1): e0245730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Instituto Nacional de Estadística e Informática del Perú: Enfermedades No Transmisibles y Transmisibles , 2019. [Internet] [Accessed March 7 2024] Available from: https://proyectos.inei.gob.pe/endes/2019/SALUD/ENFERMEDADES_ENDES_2019.pdf [Google Scholar]
- 14.Bernabé-Ortiz A, Carrillo-Larco RM, Gilman RH, et al. Contribution of modifiable risk factors for hypertension and type-2 diabetes in Peruvian resource-limited settings. J Epidemiol Community Health. 2016; 70(1): 49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seclen SN, Rosas ME, Arias AJ, et al. Prevalence of diabetes and impaired fasting glucose in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diabetes Res Care. 2015; 3(1): e000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sandes LFF, Freitas DA, de Souza MFNS, et al. Primary health care for South-American indigenous peoples: an integrative review of the literature. Rev Panam Salud Publica. 2018; 42: e163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Instituto Nacional de Estadística e Informática del Perú: Encuesta Demográfica y de Salud Familiar, 2019. Nacional y Regional . [Internet] [Accessed March 7 2024]. Available from: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Endes2019/ [Google Scholar]
- 18.Underhill LJ, Williams KN, Cordova-Ascona L, et al. Addressing Hypertension and Diabetes through Community-Engaged Systems in Puno, Peru (ANDES): rationale and study protocol for a hybrid type 3 effectiveness and implementation randomized controlled trial. Trials. 2024; 25(1): 747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007; 335(7624): 806–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42(2): 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019; 95: 103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim MT, Hill MN, Bone LR, et al. Development and testing of the Hill-Bone Compliance to High Blood Pressure Therapy Scale. Prog Cardiovasc Nurs 2000;15(3):90–96. [DOI] [PubMed] [Google Scholar]
- 23.Schmidt AF, Finan C. Linear regression and the normality assumption. J Clin Epidemiol. 2018; 98: 146–151. [DOI] [PubMed] [Google Scholar]
- 24.Akaike H. Information Theory and an Extension of the Maximum Likelihood Principle. In: Parzen E, Tanabe K, Kitagawa G, editors. Selected Papers of Hirotugu Akaike [Internet]. New York, NY: Springer; 1998. [cited 2024 Mar 7]. p. 199–213. (Springer Series in Statistics). Available from: 10.1007/978-1-4612-1694-0_15 [DOI] [Google Scholar]
- 25.Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–723. [Google Scholar]
- 26.R: The R Project for Statistical Computing. https://www.r-project.org/ [Internet]. [cited 2024 Mar 7]. Available from:
- 27.Sol to US-Dollar Conversion | PEN to USD Exchange Rate Calculator | Markets Insider [Internet]. [cited 2024 Mar 7]. Available from: https://markets.businessinsider.com/currency-converter/peruvian-nuevo-sol_united-states-dollar
- 28.Lombardi N, Crescioli G, Simonetti M, et al. Adherence to Triple-Free-Drug Combination Therapies Among Patients With Cardiovascular Disease. Am J Cardiol. 2020; 125(9): 1429–1435. [DOI] [PubMed] [Google Scholar]
- 29.Paranjpe R, Chen H, Johnson ML, et al. Adherence to concomitant diabetes, hypertension, and hyperlipidemia treatments among older patients. J Am Pharm Assoc. 2022; 62(4): 1351–1358. [DOI] [PubMed] [Google Scholar]
- 30.Lemstra M, Alsabbagh MW. Proportion and risk indicators of nonadherence to antihypertensive therapy: a meta-analysis. Patient Prefer Adherence. 2014; 8: 211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schmittdiel JA, Nichols GA, Dyer W, et al. Health care system-level factors associated with performance on Medicare STAR adherence metrics in a large, integrated delivery system. Med Care. 2015; 53(4): 332–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ministerio de Salud del Perú. Guía técnica: Guía de práctica clínica para la prevención y control de la enfermedad hipertensiva en el primer nivel de atención. Resolución Ministerial; No. 491-2009/MINSA. [Published July 21 2009] [Internet] [Accessed November 24 2024]. Available from: https://www.gob.pe/institucion/minsa/normas-legales/246435-491-2009-minsa [Google Scholar]
- 33.Instituto de Evaluación de Tecnologías en Salud e Investigación, EsSalud. Guìa de Práctica Clínica Para el Manejo de la Hipertensión Arterial Esencial . [Published December 22 2022] [Internet] [Accessed November 24 2024]. Available from: https://ietsi.essalud.gob,pe/wp-content/uploads/2022/12/GPC-HTA-esencial_Version-corta.pdf [Google Scholar]
- 34.Ministerio de Salud del Perú. Guía técnica: Guía de práctica clínica para el diagnóstico, tratamiento y control de la diabetes mellitus tipo 2 en el primer nivel de atención. Resolución Ministerial No.242412 710-2015/MINSA. [Published November 2025] [Internet] [Accessed November 2024] Available from: https://www.gob.pe/institucion/minsa/normas-legales/193275-719-2015-minsa [Google Scholar]