Abstract
Osteoid Osteoma (OO) is a common primary bone tumor that often presents with night pain in younger orthopedic patients. Although typically extra-articular, intra-articular presentations may be difficult to diagnose. While magnetic resonance imaging (MRI) provides excellent detailed imaging of the articular surface, it has been reported to lead to occasional misdiagnosis given limitations in spatial resolution, particularly for smaller lesions. Computed tomography (CT) remains the gold standard imaging modality for OO. The treatment for osteoid osteoma consists of medical management, minimally invasive image guided techniques, and surgical resection in order of most conservative to most aggressive. We present the case of a 31-year-old male with persistent posterolateral knee pain after subchondroplasty. CT demonstrated an OO in the posterior tibial plateau. The patient was successfully treated with CT-guided percutaneous radiofrequency ablation with complete resolution of symptoms. We also provide a brief literature review of the diagnosis and treatment of OO to help heighten the awareness of this sometimes inconspicuous diagnosis.
Keywords: Osteoid osteoma, Subchondroplasty, Radiofrequency ablation, Computed tomography, Magnetic resonance imaging
Introduction
Osteoid osteoma (OO) is a common primary bone tumor affecting orthopedic patients [1]. Initially described in 1930, it was further characterized in 1935 and is pathologically described as a benign osteoblastic tumor made up of osteoid and woven bone with a sclerotic rim [2,3]. While relatively rare, OO makes up 2%-3% of all primary bone tumors and 10%-14% of all benign bone tumors [4,5]. The pathology primarily affects younger patients with the majority of patients presenting between the ages of 5 and 25 years old. Commonly, OO affects the metaphyseal regions of long and tubular bones such as the femur and tibia [6]. The vast majority of these are located near the hip or femoral shaft with very few localizing around the knee [7].
The typical presentation of OO is that of localized pain and night pain which responds well to nonsteroidal anti-inflammatory drugs (NSAIDs). The gold standard imaging modality for diagnosis is computed tomography (CT) which demonstrates a small lytic bone lesions with a diameter of <2cm [8]. For patients who fail to respond to noninvasive treatment options, en-bloc resection was a historical treatment option and remains a treatment option in some cases [9]. With improvement in image guided treatment and less invasive modalities, radiofrequency ablation techniques have recently become the mainstay of treatment [4].
We present a case of a young male who underwent successful radiofrequency ablation for a missed OO in the posterior lateral tibial plateau.
Case report
Chief complaint
A 31-year-old male presented to the outpatient orthopedic sports medicine office with a complaint of left posterolateral knee pain for 2 years.
Present medical history
The patient began to experience left lateral knee pain 2 years prior after a fall onto ice. His pain was persistent, but was managed with symptomatic treatment with NSAIDs for approximately 8 months. When the pain continued to persist, he presented to an orthopedic surgeon where he was diagnosed with a lateral tibial plateau subchondral fracture and underwent a left knee arthroscopy and cement subchondroplasty.
Following this procedure, he had no improvement in his knee pain and subsequently presented to the authors for a second opinion. He described his pain as sharp and located anteriorly and laterally at the proximal tibia. The pain was notably worsened with quick internal rotation of the lower leg and improved with rest. He denied mechanical symptoms, effusions, and instability.
Past medical history
The patient denied any past medical history, including history of infectious diseases. He denied any known allergies to medications. His only surgical history was that of the subchondroplasty he underwent for his current problem.
Physical examination
Physical exam of the lower extremities identified no deformity. He stood with neutral alignment and was able to walk with a nonantalgic gait. He was able to perform a pain free squat. He had excellent quadriceps tone and was able to perform a straight leg raise without an extensor lag. The range of motion of the affected leg was full extension to 135 degrees of flexion which was symmetric bilaterally. There was no periarticular tenderness to palpation. The knee was ligamentously stable in the coronal and sagittal planes. There was deep lateral pain with McMurrays testing without a palpable click. There was no Tinel's sign at the proximal fibula over the common peroneal nerve. Proximal tibiofibular joint translation was pain-free and symmetric bilaterally. He had full power with dorsiflexion, plantarflexion, inversion, eversion, and great toe flexion and extension. Light touch sensation was intact throughout the foot and there was a palpable dorsalis pedis pulse. There was no relief of symptoms following a diagnostic intra-articular lidocaine injection.
Imaging evaluation
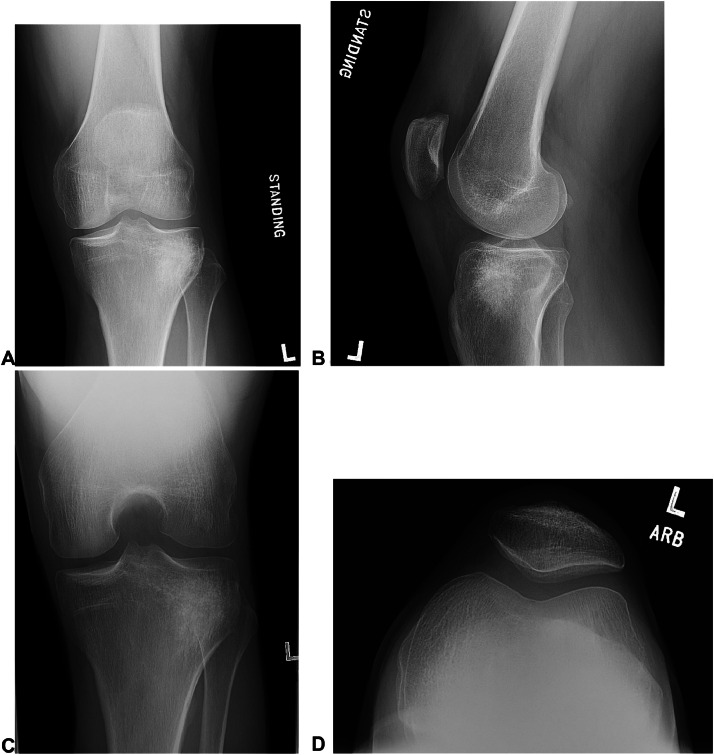
Radiographs of the left knee (Fig. 1) showed evidence of the prior subchondroplasty in the lateral tibial plateau. Given the absence of acute findings on radiography and persistent pain, MRI was subsequently performed.
Fig. 1.
PA (A), lateral (B), tunnel (C), and sunrise (D) radiographic views of the left knee demonstrates a geographic region of hyperdensity within the proximal lateral tibial metaphysis consistent with prior cement subchondroplasty.
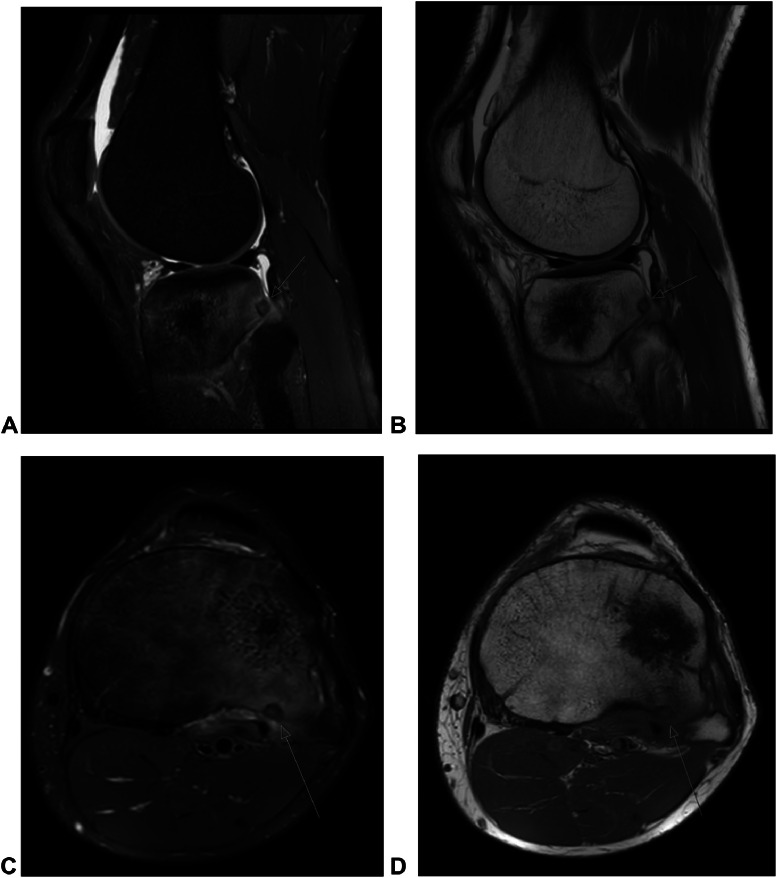
MRI of the left knee (Fig. 2) demonstrates a round cortically based lesion withing the posterior lateral tibial plateau, although a follow up CT was recommended for more definitive confirmation.
Fig. 2.
Sagittal proton density fat-saturated (A), sagittal proton density (B), axial T2 fat-saturated (C), and axial T1 sequences of the left knee at the level of the tibial plateau demonstrates a round cortically based lesion within the posterior lateral tibial plateau (orange arrow). There is reactive surrounding edema-like marrow signal changes and internal intralesional area of heterogenous T1 hypointensity and heterogenous T2 hyperintensity. The lesion measures approximately 0.5 by 0.5 by 0.7 cm in transaxial by crainocaudual dimensions, and is suspect for osteoid osteoma. Anterior to the subcentimeter lesion in the lateral tibial plateau is a geographic T1 and T2 hypointense region of signal abnormality with few foci of preserved marrow fat centrally consistent with cement material from prior subchondroplasty.
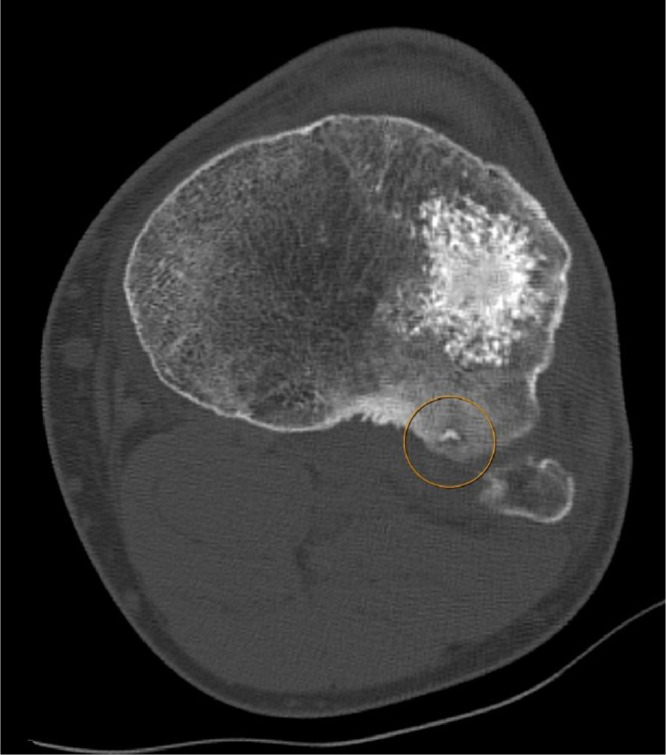
CT of the left knee (Fig. 3) confirms a cortical based lesion within the posterior lateral tibial plateau with internal nidus.
Fig. 3.
Axial CT of the left knee at the level of the tibial plateau demonstrates a posteriorly oriented lateral tibial plateau cortically based subcentimeter lucency with internal nidus of mineralization consistent with osteoid osteoma (orange circle). Anterior to the osteoid osteoma is a geographic region of hyperdensity with ill-defined margins consistent with cement material from the prior lateral tibial plateau subchondroplasty.
Final diagnosis
The location and persistence of symptoms with the imaging findings of the posterior lateral tibial plateau lesion on multiple modalities led to the final diagnosis of OO. Given its subchondral location in the region of the popliteal hiatus, it is likely that his posterolateral pain that was aggravated by quick internal rotation of the tibia, and was likely the result of the popliteus tendon directly rubbing over the OO at the rim of the tibial plateau. It is understandable that the subchondral fracture would have initially been thought to be the pain generator as it was in a similar location as to the OO in the posterior lateral tibia. The OO may have been missed from the outside facility since perhaps at that time, the OO was smaller in size and less conspicuous on their imaging, resulting in misidentifying the true pain generator. Additionally, at that time, the subacute findings of the subchondral fracture and reactive marrow signal changes would have most likely masked the reactive marrow signal changes of the OO, further confounding the diagnosis.
Treatment
Given the persistence of long-standing knee pain refractory to conservative measures, including NSAID medications, the patient elected for ablation of the osteoid osteoma within the posterior lateral tibial plateau.
The patient was sedated under general anesthesia for the procedure. First, an anterolateral incisional approach was confirmed for the course of the CT-guided procedure, with posteromedial guidance of the biopsy and ablation devices to the posterior lateral tibial plateau. CT-fluoroscopy was utilized for real-time localization throughout the procedure. Prior to ablation, core biopsy specimens of the osteoid osteoma nidus were taken utilizing a 10-gauge introducer needle with an 11-gauge core biopsy device (Fig. 4). After biopsy was performed, a 1.1cm radiofrequency ablation needle was then advanced into the nidus of the lesion (Fig. 5). Ablation was performed at 70 degrees Celsius for two 5-minute cycles. 70 degrees Celsius was chosen as to optimally ablate the lesion and to avoid a potential complication of fracturing the cortex given its intraarticular location.
Fig. 4.
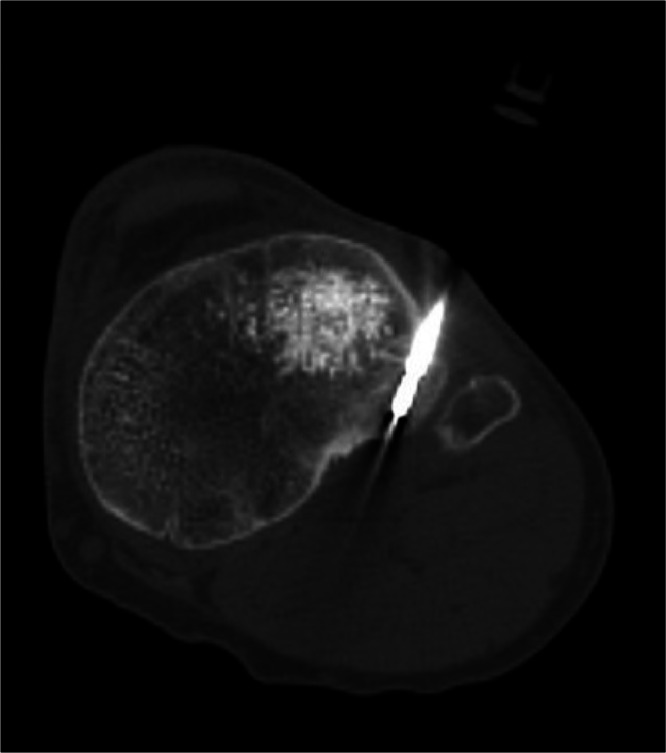
Intraprocedural CT-fluoroscopy image demonstrates the co-axial biopsy system in the center of the posterior lateral tibial plateau lesion. The nidus was specifically targeted for biopsy to histopathologically confirm the diagnosis of osteoid osteoma.
Fig. 5.
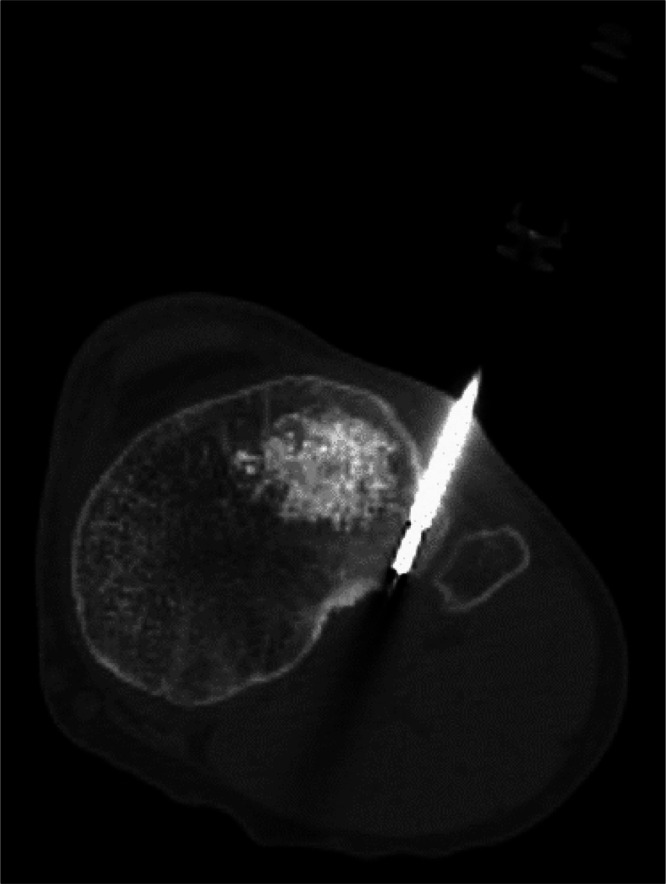
Intraprocedural CT-fluoroscopy image demonstrates the distal tip of the ablation device within the nidus of the lesion.
Outcome and follow-up
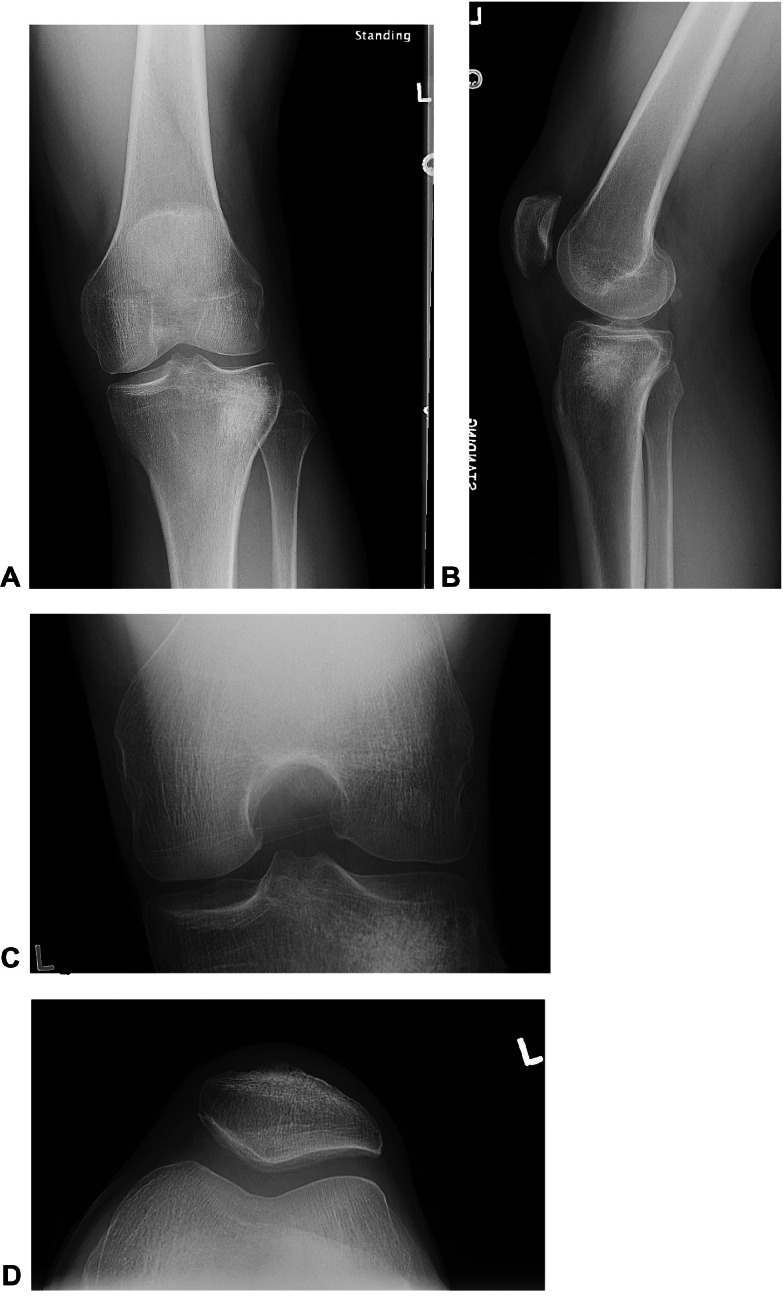
The histopathological assessment of the biopsy specimen confirmed the diagnosis of OO. At his last follow-up 3.5 months postprocedure, the patient reported complete resolution of knee pain. In fact, the patient reported that his knee recovered quickly after the procedure and he was able to lift heavy machinery equipment 3 days following the ablation. In the ensuing 3 months, he had been able to return to sprinting and lifting weights without pain. He denied any recurrent effusions. His Knee Osteoarthritis Outcome Score (KOOS) was 100% (global and in all subdomains) and his Single Alpha Numeric Evaluation (SANE) score was 100%. On follow-up examination he had pain free range of motion from 5 degrees of hyperextension to 140 degrees of flexion. There was no pain with McMurray testing or forced internal tibial rotation. He reported his knee feeling better than it has in over 3 years. Three month follow up postprocedure radiographs did not demonstrate any acute findings and were stable (Fig. 6).
Fig. 6.
PA (A), lateral (B), tunnel (C), and sunrise (D) radiographic views of the left knee status post osteoid osteoma biopsy and ablation does not demonstrate postprocedural complication such as fracture or complex large joint effusion. The lateral subchondral tibial plateau demonstrates similar hyperdensity consistent with known subchondroplasty material.
Discussion
Clinical presentation and diagnosis of osteoid osteoma
In the original classification of OO, Edeiken classified the lesion into cortical, cancellous, and subperiosteal subtypes with a cortically based lesion being the most common presentation [5,10]. The presentation typically correlated with the second and third decade of life and more often affected males [11,12]. These lesions tend to localize to the diaphysis and metaphysis of long bones and are rarely reported intra-articularly [13,14]. The clinical presentation of extra-articular OO often involves night pain, swelling and restricted motion, with night time pain being a cardinal symptom [15,16]. Lesions that present intra-articularly may present with synovitis and limping [17].
Imaging modalities of osteoid osteoma
The current, standardized imaging modalities employed in the diagnosis of OO include radiographs, MRI, nuclear bone scans, and CT. The radiographic appearance of OO includes a lesion surrounded by sclerosis that is often juxtacortical and has been reported to be prone to misdiagnosis [18,19]. MRI provides a more detailed view of intra-articular structures and tends to be the default imaging tool for nonspecific joint pain. While providing a more detailed view of the joint and surrounding structures, MRI's high sensitivity in detecting joint effusions, bony edema, and synovial inflammation may lead to misdiagnosis for OO given limitations in spatial resolution [14,15]. The current gold standard for the diagnosis of OO remains CT which has reported high sensitivity and specificity [19].
Treatment of osteoid osteoma
The treatment of OO includes an algorithmic approach which involves medical management, minimally invasive image guided approaches, and surgical resection in order from most conservative to most aggressive. While symptoms from OO tend to be self-resolving with time, oral salicylates have been demonstrated to provide effective pain control. When medical management fails, surgical resection of the entirety of the lesion and surrounding reactive bone can be successful. The first reported excision of OO was performed and reported by Jaffe in 1935 [3]. Depending upon lesion size and location, surgical resection can be difficult and morbid, and can lead to significant bone voids requiring stabilization [20]. Recent arthroscopic techniques have been employed in the excision of intra-articular lesions, however, dependent upon lesion location, these procedures can be tedious and risk incomplete excision [21].
Due to the limitations of medical and surgical management, percutaneous image-guided treatment has become the treatment of choice for OO. First reported by Tilloston in 1989, radiofrequency ablation employs the localized delivery of high-frequency alternative currents which can invoke localized tissue necrosis [22]. Its reported success is equivalent to surgical resection and it is more safely employed in difficult to access locations [[23], [24], [25]]. The procedure has also proven to be safe and effective in intra-articular and juxta-articular lesions with careful probe placement [26]. Limitations to this technique involve lesions that are relatively subcutaneous with locations <1cm from skin and neurovascular structures to avoid burns and iatrogenic injuries [22,27]. Radiofrequency ablation also has the added advantages of reduced hospital stay for the patient and overall cost-savings relative to surgical interventions [28].
Conclusion
In summary, we present a rare case of posterior tibial plateau OO whose symptoms did not improve following initial treatment with subchondroplasty for suspected subchondral fracture. Osteoid osteomas can be difficult to diagnose due to inconsistent symptomatology, specifically in intra-articular lesions. In our case, the utilization of multiple imaging modalities to arrive at the diagnosis of OO with histopathological confirmation, followed by CT-guided radiofrequency ablation, led to the successful treatment of this patient with complete resolution of symptoms and full return to function.
Patient consent
Informed consent was obtained from the subject described in this report. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Institutional review board protocol review was exempt per our institutional review board policies for this type of manuscript and since these examinations were clinically indicated. Our study complied with the Health Insurance Portability and Accountability Act.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments: No funding sources to disclose.
References
- 1.Sharma S, Rajnish RK, Prakash M, Agarwal S, Dhillon MS. Patellar osteoid osteoma as a cause of intractable anterior knee pain: a case report and systematic review of literature. J Orthop Case Rep. 2020;10(2):29–34. doi: 10.13107/jocr.2020.v10.i02.1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uuber Eine Eigenartige H.B. Wahrscheinlich bisher nicht beschriebene osteoblastiche krankheit in den langen knochen der hand und des fusses. Acta Radiol. 1930;11 596-13. [Google Scholar]
- 3.HL J. Osteoid-Osteoma: a benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg. 1935;31:709–728. [Google Scholar]
- 4.Tepelenis K, Skandalakis GP, Papathanakos G, Kefala MA, Kitsouli A, Barbouti A, et al. Osteoid osteoma: an updated review of epidemiology, pathogenesis, clinical presentation, radiological features, and treatment option. In Vivo. 2021;35(4):1929–1938. doi: 10.21873/invivo.12459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cortese MC, Albano D, Messina C, Perrucchini G, Gallazzi E, Gallazzi MB, et al. Multicentric, multifocal, and recurrent osteoid osteoma of the hip: first case report. BMC Musculoskelet Disord. 2019;20(1):171. doi: 10.1186/s12891-019-2552-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Napora J, Walejko S, Mazurek T. Osteoid osteoma, a diagnostic problem: a series of atypical and mimicking presentations and review of the recent literature. J Clin Med. 2023;12(7):2721. doi: 10.3390/jcm12072721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Plecko M, Mahnik A, Dimnjakovic D, Bojanic I. Arthroscopic removal as an effective treatment option for intra-articular osteoid osteoma of the knee. World J Orthop. 2021;12(7):505–514. doi: 10.5312/wjo.v12.i7.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chai JW, Hong SH, Choi JY, Koh YH, Lee JW, Choi JA, et al. Radiologic diagnosis of osteoid osteoma: from simple to challenging findings. Radiographics. 2010;30(3):737–749. doi: 10.1148/rg.303095120. [DOI] [PubMed] [Google Scholar]
- 9.Motamedi D, Learch TJ, Ishimitsu DN, Motamedi K, Katz MD, Brien EW, et al. Thermal ablation of osteoid osteoma: overview and step-by-step guide. Radiographics. 2009;29(7):2127–2141. doi: 10.1148/rg.297095081. [DOI] [PubMed] [Google Scholar]
- 10.Edeiken J, DePalma AF, Hodes PJ. Osteoid osteoma. (Roentgenographic emphasis) Clin Orthop Relat Res. 1966;49:201–206. [PubMed] [Google Scholar]
- 11.Zhang Y, Rosenberg AE. Bone-forming tumors. Surg Pathol Clin. 2017;10(3):513–535. doi: 10.1016/j.path.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 12.Ward WG, Eckardt JJ, Shayestehfar S, Mirra J, Grogan T, Oppenheim W. Osteoid osteoma diagnosis and management with low morbidity. Clin Orthop Relat Res. 1993;(291):229–235. [PubMed] [Google Scholar]
- 13.Bhure U, Roos JE, Strobel K. Osteoid osteoma: multimodality imaging with focus on hybrid imaging. Eur J Nucl Med Mol Imaging. 2019;46(4):1019–1036. doi: 10.1007/s00259-018-4181-2. [DOI] [PubMed] [Google Scholar]
- 14.Light J, Retrouvey M, Conran RM. Educational case: osteoid osteoma. Acad Pathol. 2021;8 doi: 10.1177/23742895211060536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Germann T, Weber MA, Lehner B, Kintzele L, Burkholder I, Kauczor HU, et al. Intraarticular osteoid osteoma: MRI characteristics and clinical presentation before and after radiofrequency ablation compared to extraarticular osteoid osteoma. Rofo. 2020;192(12):1190–1199. doi: 10.1055/a-1181-9041. [DOI] [PubMed] [Google Scholar]
- 16.Cohen MD, Harrington TM, Ginsburg WW. Osteoid osteoma: 95 cases and a review of the literature. Semin Arthritis Rheum. 1983;12(3):265–281. doi: 10.1016/0049-0172(83)90010-0. [DOI] [PubMed] [Google Scholar]
- 17.Davis J. Intraepiphyseal osteoid osteoma of proximal tibial epiphysis treated by en bloc excision under ct guidance: a case report. J Orthoped Oncol. 2021;7(6):155. [Google Scholar]
- 18.Rolvien T, Zustin J, Mussawy H, Schmidt T, Pogoda P, Ueblacker P. Intra-articular osteoid osteoma as a differential diagnosis of diffuse mono-articular joint pain. BMC Musculoskelet Disord. 2016;17(1):455. doi: 10.1186/s12891-016-1313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Papagrigorakis E, Benetos IS, Bakalakos M, Rozis M, Pneumaticos S. A rare cause of anterior knee pain in a young athlete and a delayed diagnosis: osteoid osteoma of the patella. Cureus. 2019;11(12):e6420. doi: 10.7759/cureus.6420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park JH, Jung HW, Jang WY. Excision of intramedullary osteoid osteomas in the posterior tibial area via medulloscopy: a case report. Medicina (Kaunas) 2021;57(2):163. doi: 10.3390/medicina57020163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He Y, Li X, Tu ZX, Chen HW, Zeng H, Peng Q, et al. Arthroscopic treatment of osteoid osteoma in the posterior proximal tibia: a case report and literature review. Medicine (Baltimore) 2024;103(5):e37076. doi: 10.1097/MD.0000000000037076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tillotson CL, Rosenberg AE, Rosenthal DI. Controlled thermal injury of bone. Report of a percutaneous technique using radiofrequency electrode and generator. Invest Radiol. 1989;24(11):888–892. doi: 10.1097/00004424-198911000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Singh DK, Kumar N, Rustagi A, Jalan D, Krishna LG, Sharma A. Percutaneous CT-guided radiofrequency ablation of osteoid osteoma: potential pitfalls and complications and how to avoid them. J Clin Orthop Trauma. 2022;28 doi: 10.1016/j.jcot.2022.101869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Noordin S, Allana S, Hilal K, Nadeem N, Lakdawala R, Sadruddin A, et al. Osteoid osteoma: contemporary management. Orthop Rev (Pavia) 2018;10(3):7496. doi: 10.4081/or.2018.7496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cakar M, Esenyel CZ, Seyran M, Tekin AC, Adas M, Bayraktar MK, et al. Osteoid osteoma treated with radiofrequency ablation. Adv Orthop. 2015;2015 doi: 10.1155/2015/807274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elnaggar ME, Albastaki A, Rashwan M, Ebrahim WH. Epiphyseal osteoid osteoma of the proximal tibial epiphysis treated by CT-guided radiofrequency ablation: a case report. Radiol Case Rep. 2023;18(8):2607–2611. doi: 10.1016/j.radcr.2023.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alkadumi M, Duggal N, Kaur S, Dobtsis J. Chondroblastoma of the knee in a teenager. Radiol Case Rep. 2021;16(12):3729–3733. doi: 10.1016/j.radcr.2021.08.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.De Filippo M, Russo U, Papapietro VR, Ceccarelli F, Pogliacomi F, Vaienti E, et al. Radiofrequency ablation of osteoid osteoma. Acta Biomed. 2018;19(89):175–185. doi: 10.23750/abm.v89i1-S.7021. [DOI] [PMC free article] [PubMed] [Google Scholar]