Abstract
Coronary artery aneurysm (CAA) is a rare form of coronary artery disease characterized by abnormal dilation of a coronary artery segment. While CAAs can present with various symptoms, syncope is notably uncommon, with limited documented cases. We present the case of a 24-year-old woman with a 2-month history of recurrent syncope, occurring in the absence of other symptoms. Initial evaluations, including MRI and cardiac examinations, revealed no abnormalities. However, a transthoracic echocardiogram identified a ring-like structure adjacent to the tricuspid valve, and subsequent computed tomography angiography confirmed a large right coronary artery aneurysm. This case highlights the rare presentation of recurrent syncope as a manifestation of CAA, emphasizing the need for timely diagnosis and intervention in similar cases.
Keywords: Coronary artery aneurysm, Syncope, Cardiac CT angiography
Introduction
CAAs are serious cardiovascular conditions that need to be addressed cautiously to reduce morbidity and death. Atherosclerosis, congenital conditions, connective tissue disease, dynamic wall stress, and viral etiologies are among the causes of their formation. [1,2]. The incidence of CAAs ranges from 0.3% to 5%. With a reported frequency of 0.02% in the population after cardiac surgery, giant CAAs are incredibly uncommon [3,4]. The most frequently affected coronary artery by CAAs appears to be the right coronary artery (40%) followed by the left anterior descending artery (32%), and the left main coronary artery (3.5%) less frequently [5].
CAAs can manifest with various symptoms; however, syncope is notably rare, and there is only a few reports of coronary artery aneurysms presenting with syncope [2,6]. In this report, we detail a case where unexplained syncope was linked to a right coronary artery aneurysm.
Case presentation
A 24-year-old woman who had been active and healthy sought medical care in the neurology department due to 2-month history of recurrent syncope. She claimed to have experienced syncope episodes in the absence of any prior symptoms, including chest pain, shortness of breath, seizures, or excruciating headaches. Her family history was unremarkable for cardiovascular disease or syncope. She was a nonsmoker, did not consume alcohol, and denied any illicit drug use. There was no history of medications or recent drug use. The physical examination of other systems was unremarkable. Laboratory data, including routine blood tests and biomarkers, were within normal limits. Following a comprehensive neurological examination, An MRI was conducted by the neurologist to investigate into the syncope more thoroughly; the results were normal.
The physician made the decision to refer her to the cardiology department for additional evaluation of her syncope episodes. The Cardiologist discovered no notable abnormalities during the cardiac examination, and the electrocardiogram (ECG) revealed a typical sinus rhythm devoid of arrhythmias.
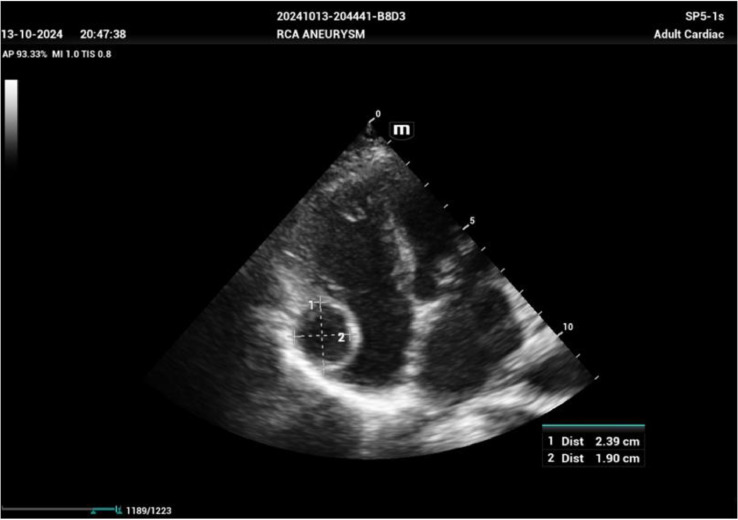
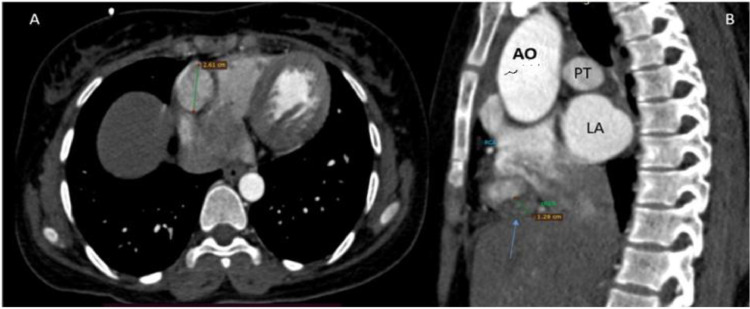
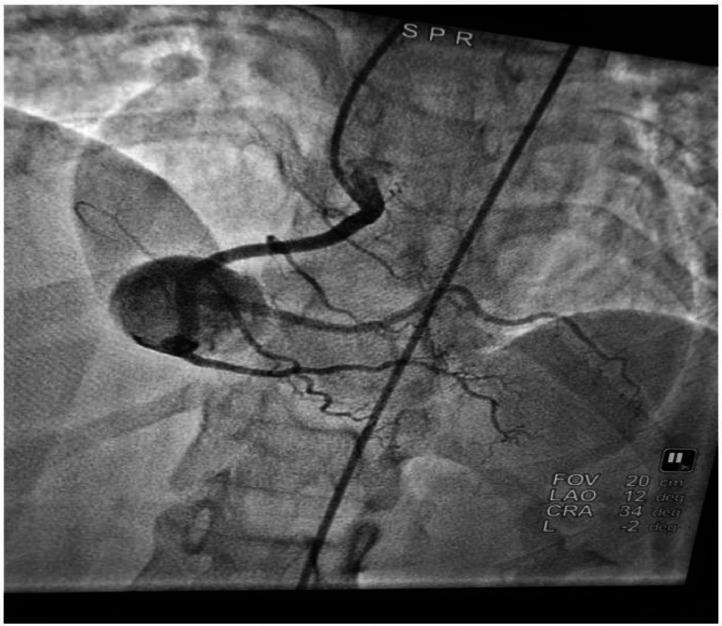
A transthoracic echocardiogram was subsequently conducted, which identified a ring-like structure adjacent to the tricuspid valve in the right atrium. The mass was described as cystic in the center and solid in the periphery, with color Doppler imaging showing no notable blood flow within the sac (Fig. 1). After that a was computed tomography angiogram (CTA) requested for further confirmation and the (CTA) revealed an enhanced mass arising from the crux of the right coronary artery (Fig. 2). To further assess this finding, conventional angiography confirmed the presence of a large right coronary artery aneurysm (Fig. 3). Given the complexity of her condition, the patient was scheduled for referral to a higher-level specialized center for advanced management.
Fig. 1.
2D Echocardiography apical 4 chamber view showing ring like cyst lesion below the tricuspid annulus measuring 2.39 × 1.90 cm.
Fig. 2.
(A) CTA-axial plane, the right coronary artery exhibited a dilatation in its atrioventricular course. An aneurysm measuring 2.6 cm in diameter was identified in the posterior branch of the right coronary artery with extension to the proximal to the bifurcation. (B) CTA-Sagittal view revealed a 1.28 cm thick mural thrombus in the inferior anteromedial wall of the aneurysm.
AO (Descended Aorta), PT (Pulmonary Trunk), LA (Left Atrium).
Fig. 3.
RAO Caudal view showing RCA aneurysm. RAO (right anterior oblique).
Discussion
A coronary artery aneurysm typically has no symptoms and is discovered by accident during angiography. It affects the RCA in 50% of cases and has an incidence of 1.2%-4.9% [7]. Based on its form or distribution in the coronary arteries, CAA can be categorized, with 50% of cases being secondary to atherosclerosis [8]. Kawasaki disease among infants and children is responsible for 17% of cases which may appear in adulthood. Rarer causes accounting for 11% of CAA include mycotic and infectious septic emboli from infections such as syphilis and borreliosis. Marfan's syndrome, arteritis such as polyarteritis nodosa, Takayasu's disease and systemic lupus erythematosus, neurofibromatosis, primary cardiac lymphoma and congenital are all even rarer causes of CAA [9]. It is yet unknown what causes coronary artery aneurysms. Though the final unifying mechanism is assumed to be similar to that of larger vessels with weakening of the artery wall, increased wall stress, dilatation, and aneurysm formation, the underlying pathophysiological processes vary depending on the underlying causal etiology [10].
The “gold standard” for identifying and assessing coronary artery aneurysms is coronary angiography. When it comes to noninvasive diagnostic methods, computed tomography The best technique for determining the size, shape, composition, and location of coronary arteries and anomalies is coronary angiography. Echocardiography, on the other hand, might be a trustworthy technique to identify and describe the masses in the event of big coronary anomalies, enabling a differential diagnosis [5]. In our case, both coronary cardiac CT and coronary angiography were performed to comprehensively evaluate the patient's condition and confirm the diagnosis of the aneurysm.
Coronary aneurysms typically don't cause any symptoms. Patients experiencing symptoms such as angina pectoris, congestive heart failure, myocardial infarction, and even unexpected death are indicative of coronary artery disease (CAD) [11]. There few reports on the literature as initial presentation of recurrent syncope in coronary artery aneurysm [2,6]. In our case, the patient's recurrent episodes of syncope were likely attributable to mechanical compression exerted by the giant right coronary artery aneurysm. It is plausible that the aneurysm's size and location caused intermittent obstruction of the right ventricular outflow tract (RVOT), especially during times of increased cardiac demand or positional changes. This obstruction could transiently reduce cardiac output, thereby compromising cerebral perfusion and causing syncope. Similar mechanisms have been observed in other case reports where large coronary aneurysms compress adjacent cardiac structures, contributing to hemodynamic instability and syncope [2]. There is debate on the best course of treatment for a CAA; many methods, including as conservative management with anticoagulant medication, catheter intervention or surgery, and urgent or elective intervention, have been documented [12]. For aneurysms smaller than 20 mm, anticoagulation has historically been the main therapeutic option; however, surgery is still the most effective method for addressing large CAAs [13]. In many situations, surgery is necessary to treat CAAs, especially when no other treatment is effective. These include CAAs situated within the left main stem, proximal to significant branch bifurcations, and severe coronary artery disease combined with valve dysfunction. Furthermore, a significant risk of rupture, mechanical problems including fistula formation or compression of nearby cardiac or vascular structures, and several or noticeably larger CAAs all call for surgical therapy. Surgery should also be considered for CAAs resulting from Kawasaki illness, especially those with specialized features such ostial, numerous, or long-segment stenosis, or those that are exacerbated by infection. Additionally, in order to minimize potential problems and guarantee the best possible outcomes for patients, surgical intervention is frequently necessary for aortocoronary saphenous vein graft aneurysms exhibiting symptoms or considerable growth, as well as reduced graft flow [14].
In conclusion, this case illustrates a unique presentation of coronary artery aneurysm (CAA), specifically through recurrent syncope. This report makes a valuable addition to the limited literature on CAAs, particularly in terms of their clinical manifestations and treatment strategies.
Conclusion
Syncope is a rare symptom of coronary artery aneurysm (CAA). This case highlights the unusual presentation of CAA with recurrent syncope, stressing the need to consider CAA in unexplained syncope cases. Multimodality imaging, including echocardiography, CTA, and coronary angiography, plays a crucial role in accurate diagnosis and management.
Author contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Patient consent
Written informed consent for the publication of this case report was obtained from the patient.
We, the authors of the case confirm that we have obtained informed consent from the patient, a 24-year-old female, to publish the details of her case. The patient has been informed about the nature of this publication, including the use of her medical information, and her right to confidentiality.
The patient has given her explicit consent for the use of identifying details, images, and clinical information related to her case in this report. We assure that all necessary measures have been taken to protect her privacy and that her identity will remain confidential in accordance with relevant ethical guidelines and regulations.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Crawley PD, Mahlow WJ, Huntsinger DR, Afiniwala S, Wortham DC. Giant coronary artery aneurysms: review and update. Tex Heart Inst J. 2014;41(6):603–608. doi: 10.14503/THIJ-13-3896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Papadopoulos K, Christophides T, Eftychiou C, Eteokleous N, Mitsis A, Zittis I, et al. Syncope in a patient with giant left main coronary aneurysm: is there a link with ventricular arrhythmias. Tex Heart Inst J. 2022;49(5) doi: 10.14503/THIJ-21-7557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gottesfeld S, Makaryus AN, Singh B, Kaplan B, Stephen B, Steinberg B, et al. Thrombosed right coronary artery aneurysm presenting as a myocardial mass. J Am Soc Echocardiogr. 2004;17(12):1319–1322. doi: 10.1016/j.echo.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Chauhan A, Musunuru H, Hallett RL, Walsh M, Szabo S, Halloran W. An unruptured, thrombosed 10 cm right coronary artery aneurysm mimicking a pericardial cyst. J Cardiothorac Surg. 2013;8:1–3. doi: 10.1186/1749-8090-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kawsara A, Núñez Gil IJ, Alqahtani F, Moreland J, Rihal CS, Alkhouli M. Management of coronary artery aneurysms. JACC. 2018;11(13):1211–1223. doi: 10.1016/j.jcin.2018.02.041. [DOI] [PubMed] [Google Scholar]
- 6.Feng J, Miao Q, Zhang C. Giant coronary aneurysm of Behcet's disease with sudden syncope: a case report. BMC Cardiovasc Disord. 2023;23(1):463. doi: 10.1186/s12872-023-03501-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bajaj A, Sehgal V, Bajwa SJ, Sethi A, Pancholy SB. Expanding giant right coronary artery aneurysm: an acute need for new management strategies. Heart Views. 2014;15(1):13–15. doi: 10.4103/1995-705X.132139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.PS P. Coronary artery aneurysm: a review. Clin Cardiol. 2006;29:439–443. doi: 10.1002/clc.4960291005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aghajanzadeh M, Pourbahador R, Hassanzadeh R, Ebrahimi H. Giant right coronary artery aneurysm mimicking a mediastinal cyst with compression effects: a case report. Res Cardiovasc Med. 2016;5(3):e32086. doi: 10.5812/cardiovascmed.32086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mata KM, Fernandes CR, Floriano EM, Martins AP, Rossi MA, Ramos SG. Vol. 29. InTech; Rijeka, Croatia: 2012. pp. 381–404. (Coronary artery aneurysms: an update. Novel strategies in ischemic heart disease). [Google Scholar]
- 11.Nazareth J, Weinberg L, Fernandes J, Peyton P, Seevanayagam S. Giant right coronary artery aneurysm presenting with non-ST elevation myocardial infarction and severe mitral regurgitation: a case report. J Med Case Rep. 2011;5:1–4. doi: 10.1186/1752-1947-5-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheikh AS, Hailan A, Kinnaird T, Choudhury A, Smith D. Coronary artery aneurysm: evaluation, prognosis, and proposed treatment strategies. Heart Views. 2019;20(3):101–108. doi: 10.4103/HEARTVIEWS.HEARTVIEWS_1_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schussler JM, Jones WH, Vallabhan RC. InBaylor University Medical Center Proceedings. Vol. 15. Taylor & Francis; 2002. Management of a single coronary artery aneurysm by use of a stent; pp. 255–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bharath K, Parvathareddy KM, Nagula P, Avinash B. Right coronary artery aneurysm masquerading as a pericardial cyst: a case report. Ind J Cardiovasc Dis Women. 2024;9(2):112–115. [Google Scholar]