Abstract
Background
Drug-coated balloons (DCBs) offer an appealing therapeutic alternative for the treatment of patients with coronary in-stent restenosis (ISR). In-segment late lumen loss, translating into recurrent ISR and the clinical need for target lesion revascularization, represents a well-established and thoroughly investigated limitation of DCB in this setting. However, abrupt vessel occlusion, clinically presenting as ST-segment elevation myocardial infarction (STEMI), has not been previously described after DCB therapy for ISR.
Case summary
We herein present the case of a 70-year-old patient that underwent percutaneous coronary intervention (PCI) with DCB for ISR. Despite achieving an excellent acute angiographic result (with no flow-limiting dissection and minimal angiographic residual stenosis), the patient presented 3 months later with STEMI due to occlusion of the previously treated segment. After adequate lesion preparation, a drug-eluting stent was implanted with optimal final angiographic result. The patient was discharged 2 days after the PCI without any post-procedural complications and remained asymptomatic at 6-month clinical follow-up.
Discussion
This case report is the first description of an abrupt vessel occlusion presenting as STEMI following a DCB angioplasty for ISR. This exceptional presentation does not dismount the solid evidence supporting the long-term safety of DCB in these challenging patients.
Keywords: Drug-coated balloon, ST-segment elevation myocardial infarction, In-stent restenosis, Optical coherence tomography, Case report
Learning points.
To understand the role of drug-coated balloon (DCB) in the treatment of in-stent restenosis (ISR)
To understand the importance of proper lesion preparation and evaluation of the final angiographic result after DCB angioplasty
To illustrate the value of optical coherence tomography to unravel the underlying mechanical causes (i.e. infra-expansion) of ISR
Introduction
Drug-coated balloons (DCBs) offer an appealing therapeutic alternative for the treatment of coronary in-stent restenosis (ISR). The efficacy of DCBs in this clinical scenario has been substantiated by various randomized clinical trials, observational studies, and meta-analyses.1–5 Despite these promising results, target lesion failure (TLF) remains an important concern during mid- and long-term follow-up after DCB percutaneous coronary intervention (PCI).1 In-segment late lumen loss, translating into the need for target lesion revascularization (TLR), represents a well-established and thoroughly investigated complication after DCB treatment for ISR. However, the abrupt occlusion of the ISR segment previously treated with DCB, clinically presenting as ST-segment elevation myocardial infarction (STEMI), has not been previously described.
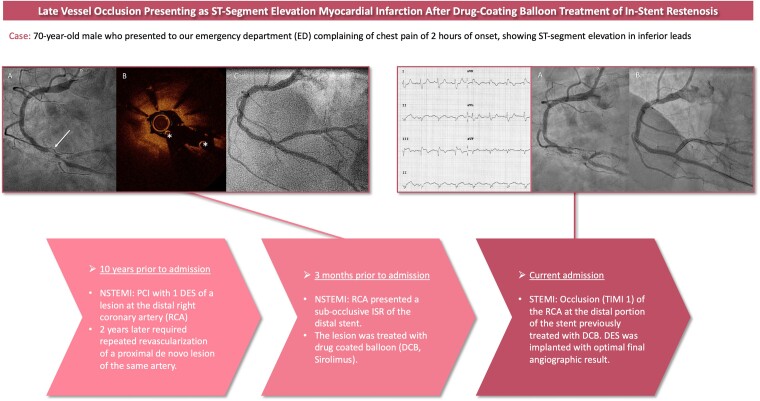
Summary figure
Case presentation
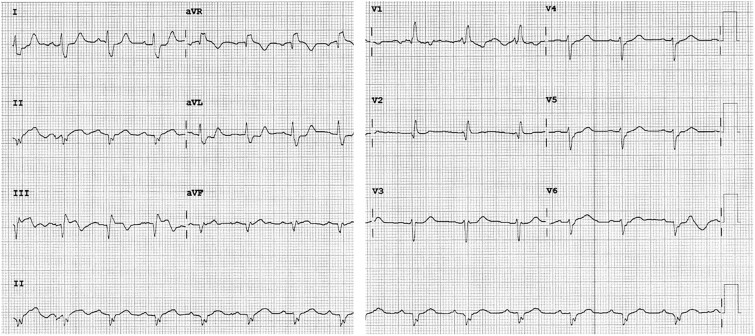
We report the case of a 70-year-old male who presented to our emergency department (ED) complaining of chest pain of 2 h of onset, showing ST-segment elevation in inferior leads (Figure 1).
Figure 1.
Twelve-lead electrocardiogram at admission, showing ST-segment elevation in inferior leads.
Our patient had a previous history of diabetes mellitus (DM), arterial hypertension, and dyslipidaemia. Additionally, he suffered from advanced chronic kidney disease (stage IV) with a baseline creatinine of 3.0–3.5 mg/dL (estimated glomerular filtration rate: 19.0 mL/min/1.73 m²). Moreover, the patient had long-standing chronic coronary syndrome and had experienced three ischaemic events prior to the current clinical presentation:
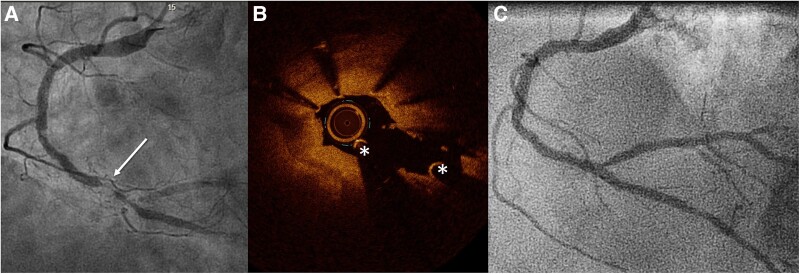
First, the patient’s coronary artery disease debuted over a decade prior to the current admission with a non-STEMI (NSTEMI). At this point, he underwent PCI with one drug-eluting stent (DES) of a lesion at the distal right coronary artery (RCA). Second, 2 years later, the patient required repeated PCI (using one DES) of a de novo proximal lesion of the same artery. Third, 3 months prior to the current admission, the patient was admitted to our ED for a new NSTEMI. This time, urgent coronary angiography (see Supplementary material online, Videos S1 and S2) revealed diffuse atheromatous disease but without significant narrowing of the left coronary system. However, the RCA presented a sub-occlusive ISR of the distal stent involving the bifurcation with the posterolateral branch (Figure 2A; Supplementary material online, Video S3). Optical coherence tomography (OCT) (Figure 2B; Supplementary material online, Video S4) revealed an occlusive ISR with severe infra-expansion of the distal edge of the stent. Pre-dilatation was performed by inflating a 2.75 mm non-compliant balloon at pressures of up to 24 atm. Following the assurance of optimal lesion preparation, with no flow-limiting dissection and minimal angiographic residual stenosis, a 3.0 mm × 20 mm DCB (sirolimus) was then inflated at 12 atm for 60 s. The final angiographic result (Figure 2C; Supplementary material online, Video S5) was excellent. The patient was discharged uneventfully 2 days later.
Figure 2.
Coronary angiography and optical coherence tomography findings of the right coronary artery. (A) Coronary angiography of the right coronary artery pre-percutaneous coronary intervention, showing sub-occlusive in-stent restenosis of the distal stent involving the bifurcation with the posterolateral branch (arrowhead). (B) Optical coherence tomography of the lesion showing homogeneous sub-occlusive in-stent restenosis and severe infra-expansion of its distal segment. (C) Final angiographic result of the right coronary artery after drug-coated balloon angioplasty. *Guidewire artefact.
At the time of the current presentation, the patient exhibited a STEMI, prompting an immediate transfer to the catheterization laboratory for primary angioplasty. On admission, the patient was haemodynamically stable with and did not require vasoactive drugs or respiratory support. He presented a blood pressure of 110/90 mmHg, a pulse rate of 92 b.p.m. and oxygen saturation of 99% (ambient air). On further physical examination, the patient did not present any relevant findings. The emergent coronary angiography (Figure 3A; Supplementary material online, Video S6) revealed an occlusion (TIMI 1) of the RCA at the distal portion of the stent previously treated with DCB. After adequate lesion preparation with pre-dilatation with a 2.5 mm × 12 mm semi-compliant balloon at a pressure of 16 atm, a 3.0 mm × 20 mm DES was implanted at 16 atm (Figure 3B; Supplementary material online, Video S7) with optimal final angiographic result. A comprehensive echocardiographic evaluation revealed normal left ventricular ejection fraction and hypokinesia of inferior segments. Laboratory findings showed adequate control of cardiovascular risk factors, such as DM and dyslipidaemia (HbA1c: 5.9%, LDL 37 mg/dL). Relevant medical therapy during hospitalization and at discharge included double antiplatelet therapy with aspirin and ticagrelor; intensive lipid-lowering therapy, including atorvastatin, ezetimibe, and evolocumab; and antidiabetic therapy, such as an intensive insulin regimen and semaglutide.
Figure 3.
Emergent coronary angiography of the right coronary artery. (A) Angiographic finding of the right coronary artery showing a reduced antegrade flow with sub-occlusion of the right coronary artery at the distal portion of the previously segment treated with drug-coated balloon. (B) Final angiographic result.
In collaboration with the nephrology department, which evaluated the patient during hospitalization, the patient was discharged 2 days after the PCI without any post-procedural complications. A follow-up clinical evaluation was scheduled 5 days post-discharge at our cardiology and nephrology outpatient clinics. The patient remained asymptomatic at 6-month clinical follow-up.
Written informed consent for the publication of this case was obtained from the patient.
Discussion
The ISR, traditionally defined as a reduction in luminal diameter of ≥50% within a previously stented segment, remains the primary cause for late PCI failure.6,7 The DCB offers an appealing therapeutic alternative in this unique anatomical scenario. The efficacy of DCB in this setting has been substantiated by various randomized clinical trials, observational studies, and meta-analyses.2,5,8 Currently, both DES and DCB are recommended (IA) by clinical practice guidelines in the treatment of ISR. The DAEDALUS study, a large and comprehensive individual patient data meta-analysis, supported an equal efficacy of DCB and DES for the treatment of bare metal stent (BMS) ISR. However, DES was moderately more effective in reducing the clinical need of target lesion revascularization than DCB for patients with DES-ISR (although at the cost of a numerical excess in all-cause death and myocardial infarctions).1
Avoiding the implantation of a new metal layer is the main rationale to favour the use of DCB in patients with ISR. Permanent metallic implants suffer from a low but persistent risk of future target lesion-related events. Of particular concern is the risk of late and very late stent thrombosis after DES that theoretically is prevented by the use of ‘leave nothing behind strategies’ as DCB. While in-segment late lumen loss is a thoroughly investigated complication on long-term follow-up after DCB for ISR, TLF presenting as acute STEMI has not been previously described in this scenario. Therefore, to the best of our knowledge, our case is the first detailed description of this devastating complication in a patient previously treated with DCB for ISR.
Ensuring proper lesion preparation is crucial for attaining an optimal long-term outcome with DCB angioplasty. As a case in point, the DCB treatment algorithm advocated by the international DCB consensus group designates pre-dilatation as a mandatory step.9 Moreover, to proceed with DCB-only angioplasty, it is imperative to achieve an adequate angiographic result, characterized by the absence of flow-limiting dissections and residual stenosis not exceeding 30%, after the initial lesion preparation.9 In our case, lesion preparation was meticulously carried out after OCT guidance and the final angiographic result was excellent. In addition to proper lesion preparation, enough delivery time and sufficient inflation time are recommended in order to guarantee adequate delivery of the antiproliferative drug.9 Again, in our case, deployment time was adequate and the duration of inflation of 60 s aligns with the current recommendations.9 Thus, in light of the optimal lesion preparation and the proper deployment of the DCB, favourable conditions for a positive long-term outcome were established in this case.
Stent thrombosis is a feared major complication after PCI, and most of these patients present as STEMI. The pathophysiological mechanism behind stent thrombosis is rooted in the activation of the inflammatory response, thrombus formation, and delayed endothelial healing induced by both BMSs and DES.10 Whether the same pathophysiological mechanisms for vessel occlusion causing STEMI after DES may also apply to our case of DCB angioplasty remains unsettled. Alternatively, a progressive, severe, and eventually sub-occlusive neointimal proliferation may have been a major factor contributing to the abrupt vessel closure in our patient. Unfortunately, OCT was not repeated at the time of STEMI. This was because the complete occlusion of the vessel prevented the creation of a blood-free coronary lumen, which is necessary to obtain adequate OCT insights into the underlying causes of the vessel occlusion. Additionally, given the patient’s history of advanced chronic kidney disease, we sought to avoid additional contrast administration.
When it comes to patients with high ischaemic risk and repeated ischaemic events during follow-up, prolonging dual antiplatelet therapy for extended long-term secondary prevention has shown to be a feasible option in many cases.11 However, due to our patient’s high bleeding risk, this approach was not considered optimal.
Our case demonstrates the occurrence of abrupt vessel thrombosis causing a STEMI in a patient treated with DCB for ISR. It is exceptional and has not been previously described in the literature as compared with the well-known risk of stent thrombosis after DES. However, this unique case should not be used to challenge the robust evidence, stemming from large registries and randomized trials, supporting the safety and efficacy of DCB in patients with ISR.
Conclusion
This case report is the first description of an abrupt vessel occlusion presenting as STEMI following a DCB angioplasty for ISR. This exceptional presentation does not dismount the solid evidence supporting the long-term safety of DCB in these challenging patients.
Lead author biography

Alexander Marschall, MD, studied medicine at the Medical University Graz (Austria). He completed his cardiology residency at the Central Defense Hospital, Madrid, in 2023 and since then, he is an interventional cardiology fellow at the Hospital Universitario de La Princesa, Madrid, Spain.
Supplementary Material
Contributor Information
Alexander Marschall, Department of Cardiology, Servicio de Cardiología, Hospital Universitario de la Princesa, IIS-IP, Universidad Autónoma de Madrid, Calle Diego de Leon 62, Madrid 28006, Spain.
David del Val, Department of Cardiology, Servicio de Cardiología, Hospital Universitario de la Princesa, IIS-IP, Universidad Autónoma de Madrid, Calle Diego de Leon 62, Madrid 28006, Spain.
Teresa Bastante, Department of Cardiology, Servicio de Cardiología, Hospital Universitario de la Princesa, IIS-IP, Universidad Autónoma de Madrid, Calle Diego de Leon 62, Madrid 28006, Spain.
Fernando Rivero, Department of Cardiology, Servicio de Cardiología, Hospital Universitario de la Princesa, IIS-IP, Universidad Autónoma de Madrid, Calle Diego de Leon 62, Madrid 28006, Spain.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports online.
Consent: The authors confirm that written consent for submission and publication of this case report associated text has been obtained from the patient in line with the COPE guidelines.
Funding: None declared.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Giacoppo D, Alfonso F, Xu B, Claessen BEPM, Adriaenssens T, Jensen C, et al. Paclitaxel-coated balloon angioplasty vs. drug-eluting stenting for the treatment of coronary in-stent restenosis: a comprehensive, collaborative, individual patient data meta-analysis of 10 randomized clinical trials (DAEDALUS study). Eur Heart J 2020;41:3715–3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Siontis GC, Stefanini GG, Mavridis D, Siontis KC, Alfonso F, Pérez-Vizcayno MJ, et al. Percutaneous coronary interventional strategies for treatment of in-stent restenosis: a network meta-analysis. Lancet 2015;386:655–664. [DOI] [PubMed] [Google Scholar]
- 3. Unverdorben M, Vallbracht C, Cremers B, Heuer H, Hengstenberg C, Maikowski C, et al. Paclitaxel-coated balloon catheter versus paclitaxel-coated stent for the treatment of coronary in-stent restenosis. Circulation 2009;119:2986–2994. [DOI] [PubMed] [Google Scholar]
- 4. Rittger H, Brachmann J, Sinha AM, Waliszewski M, Ohlow M, Brugger A, et al. A randomized, multicenter, single-blinded trial comparing paclitaxel-coated balloon angioplasty with plain balloon angioplasty in drug-eluting stent restenosis: the PEPCAD-DES study. J Am Coll Cardiol 2012;59:1377–1382. [DOI] [PubMed] [Google Scholar]
- 5. Byrne RA, Joner M, Alfonso F, Kastrati A. Drug-coated balloon therapy in coronary and peripheral artery disease. Nat Rev Cardiol 2014;11:13–23. [DOI] [PubMed] [Google Scholar]
- 6. Alfonso F, Kastrati A. Clinical burden and implications of coronary interventions for in-stent restenosis. EuroIntervention 2021;17:E355–E357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moussa ID, Mohananey D, Saucedo J, Stone GW, Yeh RW, Kennedy KF, et al. Trends and outcomes of restenosis after coronary stent implantation in the United States. J Am Coll Cardiol 2020;76:1521–1531. [DOI] [PubMed] [Google Scholar]
- 8. Alfonso F, Pérez-Vizcayno MJ, Cárdenas A, García del Blanco B, García-Touchard A, López-Minguéz JR, et al. A prospective randomized trial of drug-eluting balloons versus everolimus-eluting stents in patients with in-stent restenosis of drug-eluting stents: the RIBS IV randomized clinical trial. J Am Coll Cardiol 2015;66:23–33. [DOI] [PubMed] [Google Scholar]
- 9. Jeger RV, Eccleshall S, Wan Ahmad WA, Ge J, Poerner TC, Shin ES, et al. Drug-Coated balloons for coronary artery disease: third report of the international DCB consensus group. JACC Cardiovasc Interv 2020;13:1391–1402. [DOI] [PubMed] [Google Scholar]
- 10. Gopalakrishnan M, Lotfi AS. Stent thrombosis. Semin Thromb Hemost 2018;44:46–51. [DOI] [PubMed] [Google Scholar]
- 11. Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J 2023;44:3720–3826. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.