Home visits with a registered nurse did not affect postpartum contraceptive use or birth spacing.
Abstract
OBJECTIVE:
To evaluate the effect of an intensive nurse home visiting program on postpartum contraceptive use and birth spacing among individuals with a first pregnancy who were eligible for Medicaid insurance in South Carolina.
METHODS:
We conducted a nonblinded, randomized controlled trial of the Nurse-Family Partnership (NFP), an established intensive home visiting program that provides prenatal and postpartum home visits through 2 years after childbirth. The trial included patients who were eligible for Medicaid insurance with a first pregnancy at less than 28 weeks of gestation between April 1, 2016, and March 17, 2020, who were followed up through 2 years after childbirth. Participants were randomized 2:1 to NFP compared with standard of care treatment. The primary outcome was a birth interval of less than 21 months between the index pregnancy and a subsequent birth. The secondary outcomes were birth intervals of less than 15 and 24 months, receipt of a contraceptive implant or intrauterine device (IUD) immediately postpartum, any contraceptive use and receipt of a family planning visit (at both 6 weeks and 1 year postpartum), and IUD receipt at 1 year postpartum. We assessed outcomes using linked birth certificate records and Medicaid claims data.
RESULTS:
A total of 4,932 trial participants (3,295 in the intervention group and 1,637 in the control group) were included in the study analysis. Within 21 months of the study index birth, 11.0% of individuals in the NFP group and 12.2% of the usual care group had a subsequent birth. The NFP did not have a statistically significant effect on birth intervals of less than 21 months (adjusted coefficient −1.1, 95% CI, −2.9 to 0.8). There were no statistically significant differences between the NFP and control groups for any of the study's eight secondary outcomes related to birth spacing and postpartum contraceptive use.
CONCLUSION:
Home visits with a registered nurse did not affect postpartum contraceptive use or birth spacing.
CLINICAL TRIAL REGISTRATION:
In 2018, approximately 25% of pregnancies were either wanted later or unwanted.1 Unintended pregnancy is nearly four times higher among women with income less than 100% of the federal poverty level compared with women with income greater than 200% of the federal poverty level2 and is associated with depression during and after pregnancy, preterm birth, and low birth weight.3
Reducing unintended pregnancy has been part of the Healthy People national public health goals for the past 40 years.4 Programs offering home visits during pregnancy and postpartum such as the Nurse-Family Partnership (NFP) are a widely implemented intervention in the United States designed to increase pregnancy planning. Among other goals, the NFP aims to affect maternal life course, which encompasses family planning, educational achievement, and workforce participation.5
Existing evidence on the effect of NFP on birth intervals is mixed. In the earliest trials, NFP increased time to the next birth in Elmira, New York6; reduced pregnancies within 6 months in Memphis, Tennessee7; and increased birth intervals in Denver, Colorado.8 However, in more recent trials, NFP had no effect on subsequent pregnancy within 24 months in British Columbia9 and increased births within 36 months in Germany.10
Because of early program success, nurse home visiting programs have expanded widely in the United States, reaching 69,000 families in 56 states and territories by 2023.11,12 However, the evidence motivating this expansion comes from interventions that took place in the 1980s and 1990s. Since that time, the maternal and reproductive health landscape in the United States has changed dramatically in ways that could affect program outcomes. This objective of this study was to examine the effect of NFP in a contemporary context using a randomized controlled trial evaluating the scale-up of NFP in South Carolina on postpartum contraception and birth intervals.
METHODS
The NFP program began in South Carolina in 2009. Starting in 2016, the state obtained a 1915b Medicaid waiver, which provided the state with Medicaid funding to scale up the program to 32 counties, roughly doubling the number of women served.13,14 During the study, NFP care was delivered by 10 implementing agencies throughout the state; 9 of the 10 implementing agencies participated in the trial. The NFP nurses are trained in Colorado; however, local implementing NFP agencies are responsible for the monitoring and quality of the program. Participants in the NFP during the study were offered the standard package of NFP services, including up to 15 visits during pregnancy, eight during the first 60 days postpartum, and 17 between 61 days and 2 years after childbirth. Until the coronavirus disease 2019 (COVID-19) pandemic, all visits took place at the participant's home. After the start of the pandemic, visits transitioned to telehealth. The recommended length of each visit was between 60 and 90 minutes. The NFP visits focused on five domains: maternal health, the home environment, maternal life course development or goals for the future, mothers' role in the child's health and development, and strategies for leveraging social support.15 Nurses in the NFP also provided referrals for health care and social services. Services were provided in English and Spanish when bilingual nurses were available. For participants speaking other languages, translation services were available.15
The study is a randomized controlled trial of the NFP program in South Carolina. Recruitment, consent, and enrollment were conducted by existing NFP staff. Enrollment took place between April 1, 2016, and March 17, 2020. The following criteria was used for trial eligibility: 1) less than 28 weeks pregnant, 2) first-time mother, 3) income eligible for pregnancy Medicaid insurance in South Carolina, 4) at least 15 years old, 5) living in an area served by the NFP, 6) not incarcerated or living in a lockdown facility, and 7) sufficient English-language fluency to benefit from the program.15 The study sample size was selected to ensure statistical power to detect a 20% change for the primary outcome. We selected a 20% change on the basis of the magnitude of the effect size observed in previous NFP trials, which ranged from 20% to 58%.6–8 Potentially eligible participants were identified by community partners (eg, local health care clinics and schools), from South Carolina's Medicaid eligibility records, or through self-referral to the program. After participants provided consent, SurveyCTO was used to conduct on-the-spot randomization; two-thirds of trial participants were randomized into the treatment group, which was offered the NFP intervention, and one-third were randomized into the control group, who received standard of care in South Carolina. This ratio was chosen to maximize the number of referred individuals who could use NFP resources while maintaining sufficient statistical power. Additional details about the trial design are published in the study protocol.15 The study was approved by the Harvard T.H. Chan School of Public Health IRB (IRB15-2939).
The NFP nurses administered a baseline survey before randomization that captured information on participants' demographic characteristics, health care and social service use, physical and mental health, and health behaviors. Using a probabilistic match based on name, race, Social Security number, birth date, and Medicaid program identification, we linked the baseline survey to the patient's program participation data, hospital discharge records, and Medicaid claims data.
To generate the analytical sample for this study, we first identified participants with an index live birth in matched vital records within 120 days of the expected delivery date reported on the baseline survey. Individuals who did not meet this criterion because of a suspected miscarriage or a failure in the matching process or who withdrew from the study were excluded. A CONSORT (Consolidated Standards of Reporting Trials) diagram providing additional details is available in Appendix 1, available online at http://links.lww.com/AOG/D903.
The preregistered primary outcome was a birth interval of less than 21 months between the NFP birth (ie, the birth associated with the pregnancy at trial enrollment, hereafter called the index birth) and a subsequent birth.15 The preregistered secondary outcomes relating to birth intervals were birth interval of less than 15 months and birth interval of less than 24 months. The preregistered secondary contraceptive use outcomes were receipt of immediate postpartum long-acting reversible contraception (contraceptive implant and intrauterine device [IUD]), any modern contraceptive use (at 6 weeks and 1 year postpartum), receipt of a family planning visit (at 6 weeks and 1 year postpartum), and IUD receipt at 1 year postpartum. In exploratory analyses, we also examined the receipt of each individual contraceptive method separately (patch or ring, oral contraceptive pill, contraceptive injectable, IUD, contraceptive implant, and female sterilization) at 6 weeks and 1 year postpartum.15
To measure birth intervals, we used birth certificate records to identify any subsequent live birth that occurred within 24 months of the index birth. To measure postpartum contraceptive outcomes, we used Medicaid inpatient, outpatient, professional, and pharmacy claims, as well as inpatient discharge records. Contraceptive methods were identified using International Classification of Diseases, Tenth Revision codes defined by the Office of Population Affairs.16 More details on the definitions of outcomes are available in Appendix 2, available online at http://links.lww.com/AOG/D903.
We used an intent-to-treat approach comparing outcomes for participants who were assigned to the NFP, regardless of whether they received NFP visits, with outcomes for those who were assigned to the control group. For all outcomes, we used unadjusted and adjusted ordinary least-squares regression models. Adjusted models included the following prespecified covariates to improve precision of the study estimates: age, education, race, ethnicity, gestational length, relationship with father of the child, employment, housing stability, and indicators of physical and mental health.15 We included observations missing data on covariates in the adjusted regression model by including a dummy variable indicating that a covariate was missing.17
We also conducted heterogeneity analysis to determine whether the effect of the program differed between two prespecified subgroups.15 The first was a group referred to as the socially vulnerable subgroup, composed of participants who were younger than age 19 years, had not finished high school, or had challenges with mental health, identified by a score of 3 or higher on the PHQ-2 (Patient Health Questionnaire-2)18 at baseline or reported receiving mental health treatment in the year before enrollment. We also compared the effect of the intervention between non-Hispanic Black and non-Hispanic White participants, because non-Hispanic Black women have higher rates of unintended pregnancy and less access to postpartum care than non-Hispanic White women.19,20 This analysis did not include other racial and ethnic groups, because the study population was made up primarily of non-Hispanic Black (55%) and White individuals (35%).
We conducted stratified analysis by whether the participant's postpartum period was affected by the COVID-19 pandemic. Individuals whose first 6 weeks postpartum overlapped by at least 1 day with the pandemic were considered affected for the 6-week outcomes, and individuals whose first year postpartum overlapped by at least 1 day with the pandemic were considered affected for the 1-year outcomes.
During the hospital stay for childbirth, we used both inpatient data and Medicaid claims to measure contraceptive use. However, after hospital discharge, Medicaid claims were the study's only source of data on postpartum contraceptive use. Some individuals in the sample lost Medicaid coverage before the end of the 1-year postpartum follow-up. We examined whether Medicaid coverage at delivery and continuous Medicaid coverage through 60 days and 1 year postpartum differed between the study groups. In addition, as a robustness check, we considered analyses on a sample of participants who maintained Medicaid coverage through 1 year postpartum.
RESULTS
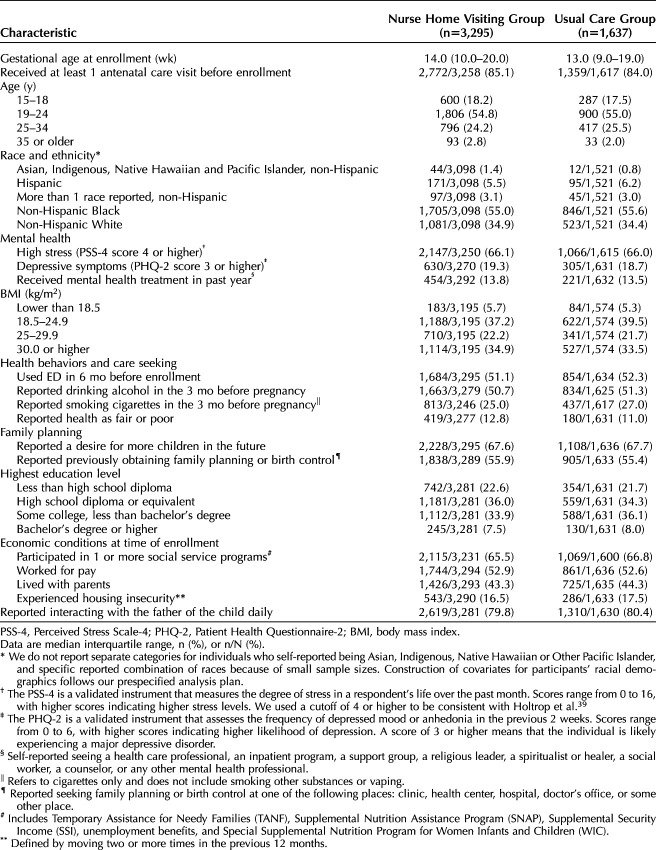
A total of 3,806 individuals were randomized to the NFP intervention; 3,721 received intervention services; and 3,295 were included in the study analysis. In the usual care group, 1,864 were randomized, 1,857 received usual care as randomized, and 1,637 were included in the study analysis (Appendix 1, http://links.lww.com/AOG/D903). On average, participants were enrolled at 13–14 weeks of pregnancy, and 84–85.1% had received at least one prenatal care visit by the time of enrollment (Table 1). The majority were aged 19–24 years (54.8–55%), 17.5–18.2% were aged 15–18 years, 24.2–25.5% were aged 25–34 years, and 2.0–2.8% were aged 35 years or older. Of NFP participants, 55.0% identified as non-Hispanic Black, 34.9% identified as non-Hispanic White, 5.5% identified as Hispanic, 3.1% reported another non-Hispanic racial identity, and 1.4% identified as non-Hispanic Asian, Indigenous, Native Hawaiian and Pacific Islander (Table 1). At the time of the survey, 21.7–22.6% of participants had not completed high school, 66–66.1% reported high stress levels, and 33.5–34.9% had body mass index (BMI, calculated as weight in kilograms divided by height in meters squared) of 30 or higher. Among participants, 51.1–52.3% used the emergency department in the 6 months before enrollment, 50.7–51.3% and 25.0–27.0% reported drinking alcohol and smoking, respectively, in the 3 months before pregnancy, and 11–12.8% reported their health as fair or poor. The majority (67.6–67.7%) reported a desire for more children in the future, and 55.4–55.9% reported having previously obtained birth control. At the time of enrollment, 65.5–66.8% of participants had received one or more social services, 52.6–52.9% worked for pay, 43.3–44.3% lived with their parents, 16.5–17.5% experienced housing insecurity, and 79.8–80.4% interacted with the father of the child daily (Table 1). Trial participants' baseline characteristics were well balanced between the study groups (Table 1).
Table 1.
Self-Reported Baseline Characteristics of Mothers With an Index Birth
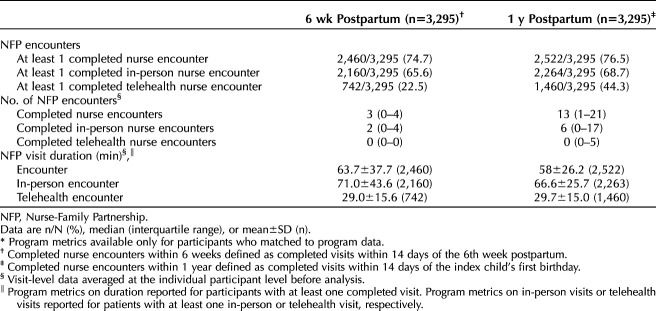
In the NFP group, 74.7% and 76.5% of individuals received at least one nurse encounter by 6 weeks and 1 year postpartum, respectively. By 6 weeks, 22.5% of NFP participants had received a telehealth encounter, and 65.6% had received an in-person encounter. By 1 year, 44.3% of participants had received a telehealth encounter, and 68.7% had received an in-person encounter (Table 2). The NFP participants had a median of three encounters by 6 weeks and a median of 13 encounters by 1 year postpartum. Most encounters by 6 weeks (median 2) and 1 year (median 6) took place in person (Table 2). Average encounter duration was 63.7 minutes at 6 weeks and 58.0 minutes at 1 year. Average duration was more than twice as long for in-person encounters compared with telehealth encounters (71.0 minutes vs 29.0 minutes for visits taking place by 6 weeks, 66.6 minutes vs 29.7 minutes for visits taking place by 1 year) (Table 2).
Table 2.
Program Implementation Metrics for the Treatment Group During the Postpartum Period*
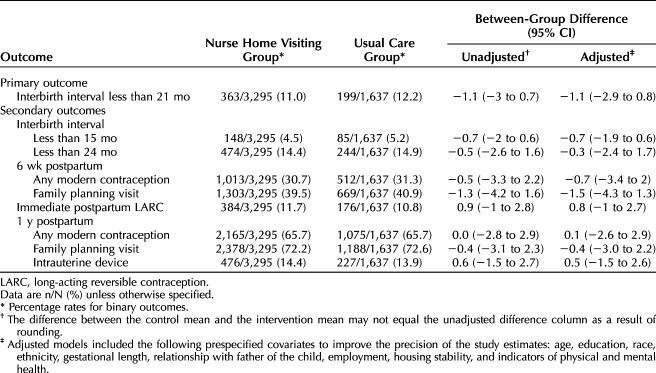
Eleven percent of individuals in the NFP group and 12.2% of the usual care group had a subsequent birth within 21 months of the study index birth. The NFP did not have a statistically significant effect on birth intervals of less than 21 months (adjusted coefficient −1.1, 95% CI, −2.9 to 0.8) (Table 3). There were no statistically significant differences between the NFP and control groups for any of the study's eight secondary outcomes related to birth spacing and postpartum contraceptive use or in the time to postpartum contraceptive take-up (Table 3) (Appendix 3, available online at http://links.lww.com/AOG/D903).
Table 3.
Effect of Nurse-Family Partnership Participation on Primary and Secondary Outcomes Related to Birth Spacing and Postpartum Contraceptive Use
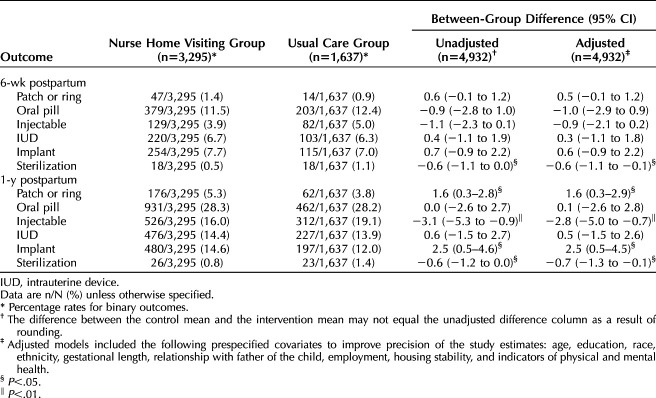
In exploratory analyses, we found that, at 6 weeks postpartum, NFP participation decreased female sterilization by 0.6 percentage points (95% CI, −1.1 to −0.1) relative to the comparison group (Table 4). At 1 year postpartum, NFP participation decreased use of the contraceptive injectable by 2.8 percentage points (95% CI, −5.0 to −0.7) and female sterilization by 0.7 percentage points (95% CI, −1.3 to −0.1) and increased patch or ring use by 1.6 percentage points (95% CI, 0.3–2.9) and implant use by 2.5 percentage points (95% CI, 0.5–4.5) (Table 4).
Table 4.
Effect of Nurse-Family Partnership Participation on Exploratory Outcomes Related to Birth Spacing and Postpartum Contraceptive Use
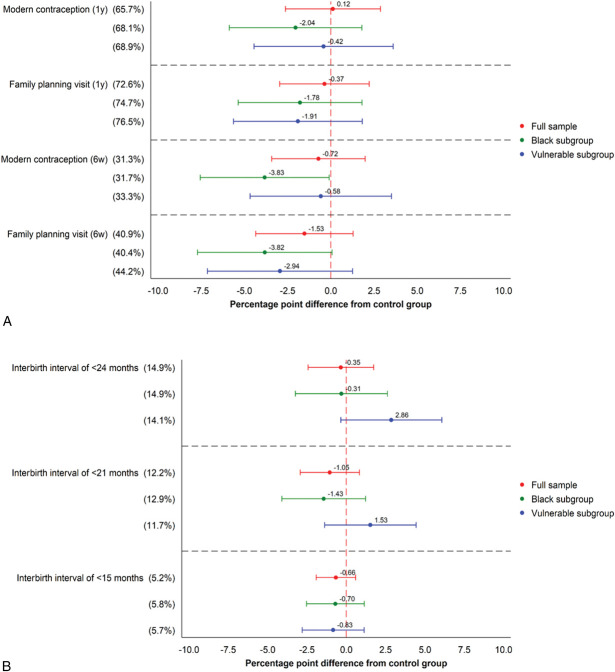
The NFP did not have a statistically significant effect on the study's primary outcome among the vulnerable population subgroup or among non-Hispanic Black participants (Fig. 1) (Appendices 4 and 5, available online at http://links.lww.com/AOG/D903). Participation in the NFP decreased any contraceptive use at 6 weeks postpartum by −3.8 percentage points (95% CI, −7.6 to −0.1) and having a family planning visit by −3.8 percentage points (95% CI, −7.7 to 0.1) among non-Hispanic Black participants but did not affect any of the other secondary outcomes in either subgroup. In addition, the effect of NFP participation did not differ between non-Hispanic Black and non-Hispanic White participants (Appendix 6, available online at http://links.lww.com/AOG/D903) or between individuals in the vulnerable compared with the nonvulnerable group (Appendix 7, available online at http://links.lww.com/AOG/D903).
Fig. 1. Effect heterogeneity: percentage rates for binary outcomes. Contraceptive outcomes (A) and birth spacing outcomes (B).
Steenland. Nurse Home Visits, Contraception Use, and Birth Spacing. Obstet Gynecol 2025.
Overall program use combining in-person and telehealth encounters was similar among individuals who were affected and those who were unaffected by the COVID-19 pandemic. However, the percentage of encounters that took place through telehealth was much higher among individuals affected by the COVID-19 pandemic (Appendix 8, available online at http://links.lww.com/AOG/D903). There were no statistical differences between groups in Medicaid coverage at any of the three time points assessed. Nearly all trial participants were enrolled in Medicaid at the time of delivery (99.0% in the NFP group and 98.7% in the usual care group). Enrollment at 60 days postpartum was also very similar between groups (93.9% in the NFP group and 93.5% in the usual care group), as was enrollment at 365 days postpartum (54.9% in the NFP group and 55.0% in the usual care group) (Appendix 9, available online at http://links.lww.com/AOG/D903).
There were no statistically significant differences for any preregistered outcomes in analyses that separated the sample based on exposure to the COVID-19 pandemic (Appendix 10, available online at http://links.lww.com/AOG/D903) or in analysis that separated the sample according to continuous Medicaid enrollment (Appendix 11, available online at http://links.lww.com/AOG/D903). There were some differences in estimated treatment effects before and after the pandemic and by continuous enrollment for some of the contraceptive methods in exploratory analyses (Appendices 12 and 13, available online at http://links.lww.com/AOG/D903).
DISCUSSION
In this trial, we found that assignment to the NFP did not affect any of the study's preregistered primary or secondary outcomes related to birth spacing or postpartum contraceptive use. We also found little evidence that NFP participation affected the study outcomes among trial participants in the study's two subgroups of interest: non-Hispanic Black individuals and individuals in the socially vulnerable subgroup. Participation in the NFP did have statistically significant effects on use of several specific methods of contraception; however, because these outcomes were not predefined and have not been adjusted for multiple hypothesis testing, the robustness of these exploratory findings should be explored in future work.
The study's main finding that NFP participation did not affect birth spacing is inconsistent with most6–8,21–24 but not all9,10,25,26 of the available evidence on the effect of NFP programs on the timing of subsequent births. Relative to earlier NFP trials, this study was larger, was conducted in a contemporary context, included a wider population base (a state rather than a town or city), and used more rigorous randomized controlled trial design features (eg, practices in preregistration of outcomes). Of the earlier NFP trials, two of the three measured birth spacing among participants who went on to have a subsequent birth at longer follow-up time points (15 and 4 years in New York and Colorado, respectively). Our trial outcomes included the full study population and focused on short birth intervals because of their association with adverse infant health outcomes.
Although differences in trial design may partially explain the differences in our findings relative to the earlier evidence, we expect that the differences are driven mainly by changes in characteristics of the population and access to health care over the past two decades. For example, the share of U.S. births to adolescents, the population with the highest risk of unintended and shortly spaced births,27 has declined dramatically over the past two decades from 61.8 per 1,000 to 17.4 per 1,000 between 1990 and 2018.28 In addition, in the late 1980s, Medicaid expansions increased income eligibility for pregnant women, resulting in increased rates of insurance and health care access in the pregnant population with low-income.29 South Carolina in particular has been the focus of a series of population-level efforts to increase access to long-acting reversible contraception methods that were hard to access before the 2010s.30–32
The goals of contraceptive care have also shifted since the original NFP trials. Much of the public health discourse in the 1980s and 1990s was focused on reducing teen pregnancy and unintended pregnancy.33 In the current context, when the goals of family planning counseling are increasingly patient centered, it is possible that NFP participation helped patients chose a method that was consistent with their needs and preferences. Improved patient-centered counseling has uncertain effects on method choice and birth spacing because some women prefer not to use contraception34 and for others efficacy is not the primary factor influencing method choice.35,36
This study has several limitations. First, only approximately 55% of individuals in the sample maintained Medicaid coverage through the full first postpartum year. However, this is unlikely to cause bias because the treatment and control groups had nearly equivalent percentages of Medicaid coverage at 60 and 365 days. Second, the study data sources do not contain a measure of preferred method use,37,38 an outcome that is more consistent with the goals of contraceptive service provision. Third, the study data sets do not contain information on induced abortion, so we cannot capture changes in subsequent pregnancy resulting from a change in abortion rates. Although we conducted stratified analysis among the COVID-19–affected and the COVID-19–unaffected study participants, this analysis was not prespecified and had limited statistical power. Fifth, there may be other areas where NFP participation has had a positive effect on the maternal life course that our data collection does not allow us to measure. Finally, for the study's primary outcome, the CI of the estimate is large enough that we cannot rule out moderate-sized reductions for the full sample, although we can rule them out in the socially vulnerable subgroup.
In sum, we noted that home visits with a registered nurse did not affect postpartum contraceptive use or birth spacing. A better understanding of how to design interventions to tailor postpartum support to enable families to reach their personal family planning goals would be valuable.
Authors' Data Sharing Statement
Will individual participant data be available (including data dictionaries)? No.
What data in particular will be shared? Not available.
What other documents will be available? Not available.
When will data be available (start and end dates)? Not applicable.
By what access criteria will data be shared (including with whom, for what types of analyses, and by what mechanism)? Not applicable.
Footnotes
Supported by the Children's Trust of South Carolina, Arnold Ventures, The Duke Endowment, BlueCross BlueShield Foundation of South Carolina, and J- PAL North America Health Care Delivery Initiative.
Financial Disclosure Katherine Baicker reports receiving payments from Eli Lilly and the National Institute for Healthcare Management. She is also a trustee of the Mayo Clinic (uncompensated). The other authors did not report any potential conflicts of interest.
Editor's Note: The clinical trial was first submitted to ClinicalTrials.gov on November 28, 2017. The first patients were enrolled on April 1, 2016. The study was registered in the AEA RCT Registry on February 20, 2016, as AEARCTR-0001039.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/D904.
REFERENCES
- 1.Robbins CL, Zapata LB, D'Angelo D, Brewer LI, Pazol K. Pregnancy intention: associations with maternal behaviors and experiences during and after pregnancy. J Womens Health (Larchmt) 2021;30:1440–7. doi: 10.1089/jwh.2021.0051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Guttmacher Institute. Fact sheet; unintended pregnancy in the United States. Accessed March 30, 2024. https://guttmacher.org/fact-sheet/unintended-pregnancy-united-states [Google Scholar]
- 3.Nelson HD, Darney BG, Ahrens K, Burgess A, Jungbauer RM, Cantor A, et al. Associations of unintended pregnancy with maternal and infant health outcomes: a systematic review and meta-analysis. JAMA 2022;328:1714–29. doi: 10.1001/jama.2022.19097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Center for Health Statistics. Publications & releases related to Healthy People. Accessed May 28, 2024. https://cdc.gov/nchs/products/hp_pubs.htm [Google Scholar]
- 5.Olds DL, Kitzman H. Review of research on home visiting for pregnant women and parents of young children. Future Child 1993;3:53–92. doi: 10.2307/1602543 [DOI] [Google Scholar]
- 6.Olds DL, Eckenrode J, Henderson CR, Jr., Kitzman H, Powers J, Cole R, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect: fifteen-year follow-up of a randomized trial. JAMA 1997;278:637–43. doi: 10.1001/jama.1997.03550080047038 [DOI] [PubMed] [Google Scholar]
- 7.Kitzman H, Olds DL, Sidora K, Henderson CR, Jr, Hanks C, Cole R, et al. Enduring effects of nurse home visitation on maternal life course: a 3-year follow-up of a randomized trial. JAMA 2000;283:1983–9. doi: 10.1001/jama.283.15.1983 [DOI] [PubMed] [Google Scholar]
- 8.Olds DL, Robinson J, Pettitt L, Luckey DW, Holmberg J, Ng RK, et al. Effects of home visits by paraprofessionals and by nurses: age 4 follow-up results of a randomized trial. Pediatrics 2004;114:1560–8. doi: 10.1542/peds.2004-0961 [DOI] [PubMed] [Google Scholar]
- 9.Catherine NLA, MacMillan H, Cullen A, Zheng Y, Xie H, Boyle M, et al. Effectiveness of nurse-home visiting in improving child and maternal outcomes prenatally to age two years: a randomised controlled trial (British Columbia Healthy Connections Project). J Child Psychol Psychiatry 2024;65:644–55. doi: 10.1111/jcpp.13846 [DOI] [PubMed] [Google Scholar]
- 10.Sandner M. Effects of early childhood intervention on fertility and maternal employment: evidence from a randomized controlled trial. J Health Econ 2019;63:159–81. doi: 10.1016/j.jhealeco.2018.11.003 [DOI] [PubMed] [Google Scholar]
- 11.Health Resources & Services Administration Maternal and Child Health. The maternal, infant, and early childhood home visiting program brief. Accessed February 23, 2024. https://mchb.hrsa.gov/sites/default/files/mchb/about-us/program-brief.pdf [Google Scholar]
- 12.Health Resources & Services Administration Maternal and Child Health. FY 2023 maternal, infant, and early childhood home visiting awards. Accessed February 23, 2024. https://mchb.hrsa.gov/programs-impact/programs/home-visiting/fy-2023-miechv-awards [Google Scholar]
- 13.Abdul Latif Jameel Poverty Action Lab. Randomized evaluation of the Nurse Family Partnership in South Carolina. Accessed March 15, 2024. https://povertyactionlab.org/evaluation/randomized-evaluation-nurse-family-partnership-south-carolina [Google Scholar]
- 14.Nurse-Family Partnership. Pay for success South Carolina. Accessed March 15, 2024. https://nursefamilypartnership.org/public-policy-and-advocacy/sc-pfs/ [Google Scholar]
- 15.McConnell MA, Zhou RA, Martin MW, Gourevitch RA, Steenland M, Bates MA, et al. Protocol for a randomized controlled trial evaluating the impact of the Nurse-Family Partnership's home visiting program in South Carolina on maternal and child health outcomes. Trials 2020;21:997. doi: 10.1186/s13063-020-04916-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Office of Population Affairs. Contraceptive care measures. Accessed February 19, 2024. https://opa.hhs.gov/research-evaluation/title-x-services-research/contraceptive-care-measures [Google Scholar]
- 17.McConnell M, Bates MA, Baicker K, Zhou A, Woodford M. Randomized evaluation of the Nurse Family Partnership in South Carolina. Accessed April 8, 2024. https://www.socialscienceregistry.org/trials/1039
- 18.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care 2003;41:1284–92. doi: 10.1097/01.Mlr.0000093487.78664.3c [DOI] [PubMed] [Google Scholar]
- 19.Bellerose M, Steenland MW. Association between the coronavirus disease 2019 (COVID-19) pandemic and national disparities in postpartum visit attendance. Obstet Gynecol 2023;141:170–2. doi: 10.1097/aog.0000000000005014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim TY, Dagher RK, Chen J. Racial/ethnic differences in unintended pregnancy: evidence from a national sample of U.S. women. Am J Prev Med 2016;50:427–35. doi: 10.1016/j.amepre.2015.09.027 [DOI] [PubMed] [Google Scholar]
- 21.Kitzman H, Olds DL, Henderson CR, Jr., Hanks C, Cole R, Tatelbaum R, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing: a randomized controlled trial. JAMA 1997;278:644–52. doi: 10.1001/jama.1997.03550080054039 [DOI] [PubMed] [Google Scholar]
- 22.Olds DL, Kitzman H, Hanks C, Cole R, Anson E, Sidora-Arcoleo K, et al. Effects of nurse home visiting on maternal and child functioning: age-9 follow-up of a randomized trial. Pediatrics 2007;120:e832–45. doi: 10.1542/peds.2006-2111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Olds DL, Robinson J, O'Brien R, Luckey DW, Pettitt LM, Henderson CR, Jr, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics 2002;110:486–96. doi: 10.1542/peds.110.3.486 [DOI] [PubMed] [Google Scholar]
- 24.Yun K, Chesnokova A, Matone M, Luan X, Localio AR, Rubin DM. Effect of maternal-child home visitation on pregnancy spacing for first-time Latina mothers. Am J Public Health 2014;104(suppl 1):S152–8. doi: 10.2105/ajph.2013.301505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jacobs F, Easterbrooks MA, Goldberg J, Mistry J, Bumgarner E, Raskin M, et al. Improving adolescent parenting: results from a randomized controlled trial of a home visiting program for young families. Am J Public Health 2016;106:342–9. doi: 10.2105/ajph.2015.302919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.LeCroy CW, Lopez D. A randomized controlled trial of healthy families: 6-month and 1-year follow-up. Prev Sci 2020;21:25–35. doi: 10.1007/s11121-018-0931-4 [DOI] [PubMed] [Google Scholar]
- 27.Gemmill A, Lindberg LD. Short interpregnancy intervals in the United States. Obstet Gynecol 2013;122:64–71. doi: 10.1097/AOG.0b013e3182955e58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Livingston G, Thomas D. Why is the teen birth rate falling? Accessed March 1, 2024. https://pewresearch.org/short-reads/2019/08/02/why-is-the-teen-birth-rate-falling/ [Google Scholar]
- 29.Dave DM, Decker SL, Kaestner R, Simon KI. The effect of Medicaid expansions on the health insurance coverage of pregnant women: an analysis using deliveries. Inq J Med Care Organ Provision Financ 2010;47:315–30. doi: 10.5034/inquiryjrnl_47.04.315 [DOI] [PubMed] [Google Scholar]
- 30.Kaiser Family Foundation. Intrauterine devices (IUDs): access for women in the U.S. Accessed March 19, 2024. Https://Kff.Org/Womens-Health-Policy/Fact-Sheet/Intrauterine-Devices-Iuds-Access-For-Women-In-The-U-S/ [Google Scholar]
- 31.Steenland MW, Pace LE, Sinaiko AD, Cohen JL. Medicaid payments for immediate postpartum long-acting reversible contraception: evidence from South Carolina. Health Aff (Millwood) 2021;40:334–42. doi: 10.1377/hlthaff.2020.00254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith MG, Hale N, Kelley S, Satterfield K, Beatty KE, Khoury AJ. South Carolina's Choose Well initiative to reduce unintended pregnancy: rationale, implementation design, and evaluation methodology. Am J Public Health 2022;112:S484–9. doi: 10.2105/ajph.2022.306889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McGinnis JM, Lee PR. Healthy People 2000 at mid decade. JAMA 1995;273:1123–9. doi: 10.1001/jama.1995.03520380059036 [DOI] [PubMed] [Google Scholar]
- 34.Richards NK, Morley CP, Wojtowycz MA, Bevec E, Levandowski BA. Use of open-text responses to recode categorical survey data on postpartum contraception use among women in the United States: a mixed-methods inquiry of Pregnancy Risk Assessment Monitoring System data. PLoS Med 2022;19:e1003878. doi: 10.1371/journal.pmed.1003878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jackson AV, Karasek D, Dehlendorf C, Foster DG. Racial and ethnic differences in women's preferences for features of contraceptive methods. Contraception 2016;93:406–11. doi: 10.1016/j.contraception.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 36.Lessard LN, Karasek D, Ma S, Darney P, Deardorff J, Lahiff M, et al. Contraceptive features preferred by women at high risk of unintended pregnancy. Perspect Sex Reprod Health 2012;44:194–200. doi: 10.1363/4419412 [DOI] [PubMed] [Google Scholar]
- 37.Gomez AM, Bennett AH, Arcara J, Stern L, Bardwell J, Cadena D, et al. Estimates of use of preferred contraceptive method in the United States: a population-based study. Lancet Reg Health Am 2024;30:100662. doi: 10.1016/j.lana.2023.100662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hopkins K, Yarger J, Rossetto I, Sanchez A, Brown E, Elmes S, et al. Use of preferred contraceptive method among young adults in Texas and California: a comparison by state and insurance coverage. PLoS One 2023;18:e0290726. doi: 10.1371/journal.pone.0290726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Holtrop JS, Meghea C, Raffo JE, Biery L, Chartkoff SB, Roman L. Smoking among pregnant women with Medicaid insurance: are mental health factors related? Matern Child Health J 2010;14:971–977. doi: 10.1007/s10995-009-0530-x [DOI] [PubMed] [Google Scholar]