Abstract
OBJECTIVES:
To explore older patients’ ICU admission preferences and their next-of-kins’ ability to predict these preferences.
DESIGN:
Self-administered survey.
SETTING:
Three outpatient clinics, urban tertiary teaching hospital, Norway.
PATIENTS:
Purposive sample of outpatients 80 years old or older regarded as potential ICU candidates and their next-of-kins.
INTERVENTIONS:
None.
MEASUREMENTS AND MAIN RESULTS:
We asked about the patients’ ICU admission preferences in three hypothetical scenarios of acute critical illness. Next-of-kin respondents were asked to make a proxy statement regarding the older respondents’ wishes regarding ICU admission. For each treatment choice, all respondents could provide their level of confidence. Additionally, we sought to identify demographic and healthcare-related characteristics that potentially influenced ICU admission preferences and proxy accuracy. Of 202 outpatients 80 years old or older, equal proportions opted for (39%; CI, 33–45%) and against (40%; CI, 34–46%) ICU admission, and one in five (21%; CI, 17–26%) did not wish to engage decision-making. Male gender, religiosity, and prior ICU experience increased the likelihood of older respondents opting for ICU admission. Although next-of-kins’ proxy statements only weakly agreed with the older respondents’ true ICU admission preferences (52%; CI, 45–59%), they agreed with the next-of-kins’ own ICU admission preferences (79%; CI, 73–84%) to a significantly higher degree. Decisional confidence was high for both the older and the next-of-kin respondents.
CONCLUSIONS:
In this purposive sample of Norwegian potential ICU candidates 80 years old or older, we found substantial variation in the ICU admission preferences of very old patients. The next-of-kins’ proxy statements did not align with the ICU admission preferences of the older respondents in half of the pairs, but next-of-kins’ and older respondents’ confidence levels in rendering these judgments were high.
Keywords: aged, 80 and over, critical illness, decision making, patient preference, proxy
KEY POINTS
Question: Do very old patients wish to be admitted to an ICU in the event of acute critical illness?
Findings: In this purposive sample of Norwegian potential ICU candidates 80 years old or older, ICU admission preferences showed significant individual variation unrelated to prognostic factors of ICU survival. Next-of-kins’ ability to predict these preferences was limited, contrasted by high levels of confidence.
Meaning: Even though subject to large individual and cultural variation, these findings call attention to the complexity and uncertainty inherent in treatment-intensity decisions for very old, critically ill patients.
Very old patients (in this context, ≥ 80 yr old or older and hereafter referred to as older) constitute 10–20% of all ICU admissions in Europe, and the proportion is expected to rise (1, 2). However, the benefit of ICU admission remains controversial for the older critically ill (3, 4). Cultural context and other factors unrelated to the patient have been shown to affect the treatment intensity offered to very old, critically ill patients (5, 6).
Patients’ preferences are paramount, especially when such invasive treatment’s benefits are unclear. Still, more than four in five older ICU patients are incapacitated within the first 24 hours of ICU admission (7). In these circumstances, the medical team typically makes decisions regarding treatment intensity in consultation with the patient’s next-of-kin, acting as a proxy for the patient. A large body of evidence has shown that proxy accuracy is weak regarding patient preferences for life-sustaining treatment (LST) (8–10). Notwithstanding, most studies were published over 20 years ago and had questionable validity (11). Measures to improve proxy accuracy have shown little effect (12).
Older patients’ and their proxies’ thoughts, wishes, and values about intensive care have yet to be well characterized. Hence, octogenarians’ LST preferences have been identified as a key research priority (13, 14). We sought to explore the ICU admission preferences of older Norwegians and their next-of-kin’s knowledge regarding these preferences using a self-administered questionnaire with hypothetical scenarios. Additionally, we aimed to describe the respondents’ confidence in their decisions and factors that may influence older patients’ ICU admission preferences and proxy accuracy.
MATERIALS AND METHODS
The questionnaires and methodology for this study were approved by the Regional Committee for Medical Research Ethics Western Norway (REK Vest) on September 08, 2021 (projectidentifier [ID] 277504, title “Intensivbehandling av eldre: Hva ønsker de selv?”). The study was carried out in accordance with the ethical standards of the responsible committee (REK Vest) and with the Helsinki Declaration of 1975. The respondents were given written information on the study and consented to participate by completing and returning the questionnaire. The study was preregistered on ClinicalTrials.gov NCT05149040 (October 31, 2021).
Target Population and Sampling Frame
We administered the questionnaire to a purposive sample of potential ICU candidates 80 years old or older. We excluded patients who would not typically be regarded as candidates for ICU admission in Norway (e.g., with very low physical and/or cognitive function) due to ethical concerns regarding exposure of older adults to hypothetical treatment choices that they would not be offered in real life. We had limited knowledge of whether older Norwegians may perceive a questionnaire addressing critical illness and treatment preferences as burdensome. Consequently, we selected an approach wherein informants had a short face-to-face encounter with one of the investigators upon enrollment, at which they could ask questions or express concern regarding the study. They were also offered an opportunity to reconnect by telephone or e-mail.
Recruitment of Survey Participants
Clinic receptionists and study personnel approached consecutive patients 80 years old or older at the orthopedic, ophthalmologic, and ear, nose, and throat outpatient clinics at Haukeland University Hospital between November 2021 and March 2023. We excluded patients who did not consent to participate, were blind, not fluent in Norwegian, living in permanent care facilities, or could not meet for in-person consultation without assistance. Patients with multiple appointments during the study period were only approached once. We recorded the age and gender of patients who were excluded or who did not respond.
Questionnaire Development
The multidisciplinary study team designed the questionnaire assisted by a user advisory group of three laypeople representing senior interest organizations. To generate items, we conducted a mapping review of the existing literature on older patients’ treatment and end-of-life preferences and proxy accuracy. Additional items were identified from discussions among the investigators.
Questionnaire Testing
The questionnaire was tested and refined in four predefined steps: pre-testing, face-, and content-validity testing, pilot testing, and clinical sensibility testing (15). Supplement 2 (http://links.lww.com/CCX/B440) contains a detailed description of questionnaire development and testing.
Questionnaire Administration
All prospective respondents received an information leaflet about the study upon registration. If they expressed interest in participation, they received two questionnaires: one for the older participant and one for the next-of-kin identified by the older participant as the most likely to act as a proxy in the event of acute critical illness. The only exclusion criterion for next-of-kin was age younger than 18 years. The respondents were asked to complete the questionnaires independently and return them in a supplied stamped return envelope. No incentives or compensation were offered, and no reminders were sent.
Questionnaire Formatting
All participants were asked to make an ICU admission choice for each of three clinical scenarios describing escalation from ward care to intensive care in a case of acute critical illness in advanced age. Participants were instructed to assume they were the patient in the vignette but with their background and current health. Older participants were asked about “their own preferences,” while their next-of-kin were asked to indicate both the “likely preference of the older participant” (i.e., acting as a proxy) and “their own preference.” For each scenario, we provided three mutually exclusive response options: 1) wishing admission to intensive care, 2) not wishing admission to intensive care, and 3) wishing to not engage in the decision. Confidence in the choices made was assessed on a 5-point scale. For each participant/next-of-kin pair, the three vignettes were randomly chosen from 20 hypothetical patient histories of acute life-threatening illness causing organ failure.
To assess framing effects, the vignette patient’s gender was randomly framed to be either female or male. Similarly, the estimated short- and long-term outcomes were randomly framed as either mortality or survival. Additionally, the questionnaires included variables postulated to influence treatment preferences and proxy accuracy: demographic data (age, gender, country of birth, marital status, religion), education, profession, prior experience with intensive care (as a patient or a next-of-kin) and communication about serious illness, Comorbidity-Polypharmacy Score (16), Clinical Frailty Scale, Version 2 (17), and health-related quality of life (EuroQol 5D-5L, registration ID: 30864) (18). See Supplement 3 for questionnaire construction (http://links.lww.com/CCX/B440).
Statistical Analysis
Supplement 4 (http://links.lww.com/CCX/B440) contains a detailed description of the statistical analyses. Briefly, we report descriptive statistics for the survey participants, both for the overall cohort and stratified by ICU admission preference. The reported ICU admission preferences are marginal proportions with corresponding 95% CIs. Sample size calculations showed that with 200 older informants, we could estimate the preference proportions with an absolute margin of error of less than 7%, based on 95% CIs, which we deemed sufficient.
To investigate factors associated with ICU admission preferences, we fitted mixed-effect logistic regression models with “wanting ICU admission” as the outcome. Explanatory variables included the experimental framing effects and demographic and health-related characteristics of the older respondents, with the vignette included as a random intercept. In the main analysis, we report the results for the first scenario since we regard these answers to be least influenced by the responses to the other two scenarios. Missing answers were handled by complete-case analysis or by multiple imputation.
To assess the next-of-kins’ ability to predict their family member’s preference, we report the overall percentage agreement with corresponding 95% CIs between the next-of-kins’ proxy preference and the older patients’ actual preference (“proxy accuracy”). Similarly, we report percentage agreement between the next-of-kins’ proxy preference and their own preference (“assumed similarity”) and between the next-of-kins’ own preference and the older patient’s actual preference (“true similarity”).
Furthermore, we used mixed-effects logistic regression to examine factors associated with “correct prediction.” We included only responses where the older respondent had a preference (“wants ICU admission” or “does not want ICU admission”) (11).
All proportions were calculated using Generalized Estimating Equation models with an “exchangeable” correlation structure to account for the dependence between multiple vignettes per participant.
Analyses were conducted using statistical software R (Version 4.2.3; R Core Team, Vienna, Austria, 2023), and p values below 0.05 were considered statistically significant.
RESULTS
Study Cohort
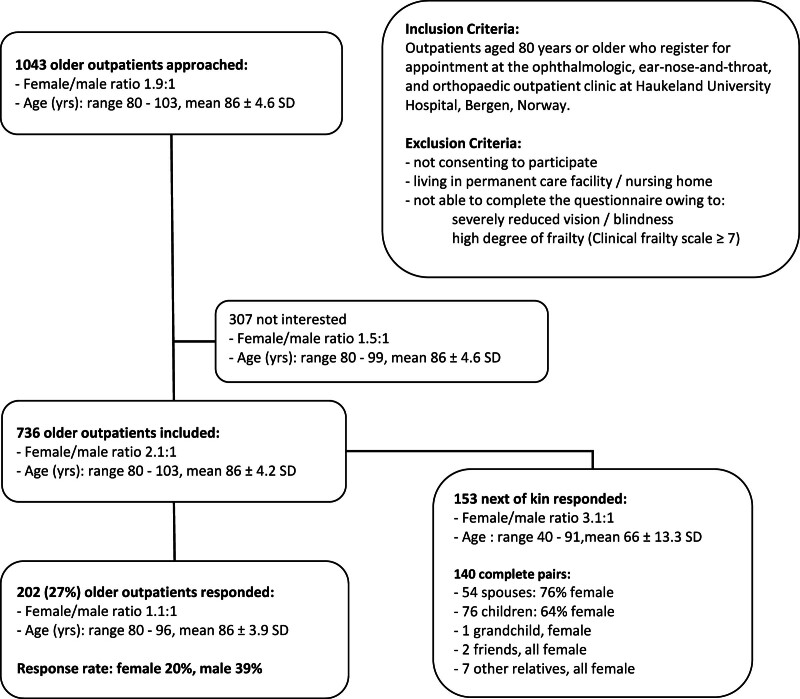
The study cohort included 202 older outpatients and 153 next-of-kin (140 complete pairs). The overall response rate was 27% (Fig. 1). Although significantly more women consented to participation (p = 0.02), significantly more men returned the completed questionnaire (p < 0.001). The age of the older respondents and nonrespondents was similar. In Supplement 5, eTable 5.1 (http://links.lww.com/CCX/B440), we present data on the representativeness of the study cohort.
Figure 1.
Study cohort derivation.
Missing Answers
Beforehand, a respondent was defined as a study participant who made at least one ICU admission choice. Of the 202 older respondents, 190 (94%), 8 (4%), and 4 (2%) completed three, two, and one scenarios, respectively. All next-of-kin answered all three scenario questions. Nearly two-thirds of the older participants (130/202, 64%) and slightly more next-of-kin (108/153, 71%) returned questionnaires without missing answers. For each variable, missing answers ranged from 0% to 6% for the older participants and from 1% to 14% for the next-of-kin, as more next-of-kin did not provide their own demographic data. Missing answers increased with respondent age, both among older and next-of-kin respondents.
Framing Effects
Based on the first scenario, framing the vignette patient’s gender as male was associated with a not statistically significant 34% reduction in the odds of the older participant opting for ICU admission. Framing the outcome in terms of survival was associated with a not statistically significant estimated 76% increase in the odds of opting for ICU admission. The survival/mortality framing effect estimates were quantitatively similar for the other two scenarios, while the estimates for the gender framing were inconsistent (Supplement 5, eTable 5.2, http://links.lww.com/CCX/B440).
ICU Admission Preferences of the Older Respondents
Similar proportions of the older respondents opted for (39%; CI, 33–45%) and against ICU admission (40%; CI, 34–46%), and a smaller proportion (21%; CI, 17–26%) did not wish to engage in decision-making. Of all older respondents, 130 of 190 (68%) made the same ICU admission choice in all three scenarios.
Table 1 presents the characteristics of older respondents for the study cohort, also stratified by ICU admission preferences. Male participant gender, being religious, and prior ICU experience were factors associated with an increase in the odds of opting for ICU admission among older participants with consistent effect and small (but not always reaching significance level) p values across all three scenarios (Supplement 5, eTable 5.2, http://links.lww.com/CCX/B440).
TABLE 1.
Demographic and Health-Related Characteristics of the Older Respondents and Their Answers Stratified by ICU Admission Preference
| Respondent Characteristics | Cohort (n = 202 Older Outpatients) | ICU Admission Preferences in Up To Three Hypothetical Scenarios (n = 590 Answers) | ||
|---|---|---|---|---|
| Opting for ICU Admission (n = 228) | Opting Against ICU Admission (n = 238) | Not Wishing to Engage in the Decision (n = 124) | ||
| Age | ||||
| Mean ± sd | 85.6 ± 3.9 | 84.9 ± 3.5 | 85.4 ± 4.0 | 86.9 ± 4.2 |
| 80–84 yr | 90 | 106 (41%) | 110 (42%) | 45 (17%) |
| 85–89 yr | 76 | 93 (42%) | 89 (40%) | 41 (18%) |
| ≥ 90 yr | 34 | 23 (23%) | 39 (39%) | 38 (38%) |
| Gender | ||||
| Female | 100 | 73 (25%) | 151 (52%) | 69 (24%) |
| Male | 94 | 139 (51%) | 83 (30%) | 52 (20%) |
| Marital status | ||||
| Single | 12 | 12 (35%) | 17 (50%) | 5 (15%) |
| Married/partner | 99 | 128 (44%) | 106 (37%) | 54 (19%) |
| Widowed | 76 | 66 (29%) | 103 (45%) | 60 (26%) |
| Separated/divorced | 9 | 14 (52%) | 9 (33%) | 4 (15%) |
| Religion | ||||
| Christian | 151 | 181 (41%) | 174 (40%) | 84 (19%) |
| Other religion | 2 | 3 (50%) | 3 (50%) | 0 (0%) |
| No religion | 41 | 35 (29%) | 52 (43%) | 34 (28%) |
| Highest education | ||||
| Primary school | 39 | 41 (37%) | 37 (34%) | 32 (29%) |
| Secondary school | 31 | 30 (33%) | 45 (50%) | 16 (18%) |
| Vocational college | 51 | 60 (40%) | 61 (40%) | 30 (20%) |
| University | 78 | 93 (41%) | 93 (41%) | 43 (19%) |
| Healthcare professional | ||||
| No | 156 | 190 (42%) | 168 (37%) | 98 (22%) |
| Yes | 35 | 25 (24%) | 57 (55%) | 21 (20%) |
| CPS | ||||
| Mean ± sd | 6.4 ± 4.0 | 6.8 ± 4.6 | 6.0 ± 3.5 | 6.5 ± 3.6 |
| Mild (CPS 0–7) | 126 | 145 (39%) | 152 (41%) | 73 (20%) |
| Moderate (CPS 8–14) | 56 | 65 (39%) | 68 (41%) | 33 (20%) |
| Morbid (CPS ≥ 15) | 9 | 16 (67%) | 6 (25%) | 2 (8%) |
| Hospital admission within last year | ||||
| No | 134 | 138 (35%) | 163 (42%) | 91 (23%) |
| Yes | 68 | 90 (46%) | 75 (38%) | 33 (17%) |
| CFS | ||||
| Mean ± sd | 3.0 ± 1.3 | 3.0 ± 1.3 | 3.0 ± 1.3 | 2.8 ± 1.3 |
| Fit (CFS 1–3) | 133 | 149 (38%) | 154 (39%) | 89 (23%) |
| Vulnerable (CFS 4) | 28 | 30 (37%) | 42 (51%) | 10 (12%) |
| Frail (CFS ≥ 5) | 28 | 38 (47%) | 28 (35%) | 14 (18%) |
| Health-related quality of life (EuroQoL 5D Visual Analogue Scale) | ||||
| Mean ± sd | 71.7 ± 18.2 | 71.2 ± 19.3 | 72.1 ± 18.0 | 74.6 ± 15.5 |
| ICU experience (as patient or relative)a | ||||
| No | 124 | 121 (33%) | 165 (46%) | 76 (21%) |
| Yes | 68 | 97 (49%) | 64 (32%) | 39 (20%) |
| Communicated end-of-life preferences to nest-of-kin | ||||
| No | 137 | 162 (41%) | 138 (35%) | 200 (25%) |
| Yes | 60 | 60 (34%) | 93 (53%) | 23 (13%) |
CFS = Clinical Frailty Scale, CPS = Comorbidity-Polypharmacy Score.
The effect of prior ICU experience was similar regardless of the respondent having been a patient or a relative.
ICU Admission Preferences, As Stated by the Next-of-Kins
Almost all older and next-of-kin respondents (98% in each group) wished for family involvement during the discussion about treatment intensity in case the older patient should fall acutely critically ill. The next-of-kins’ proxy statements aligned in half of the pairs with the older participants’ true ICU admission preferences and, to a significantly larger extent, with the next-of-kins’ “own” preferences.
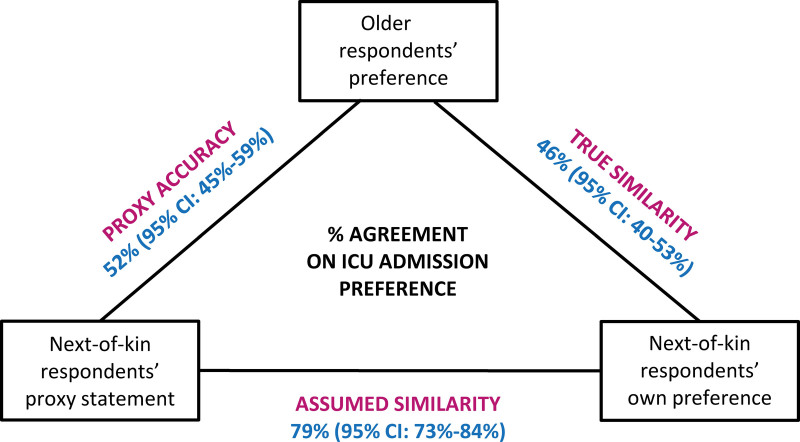
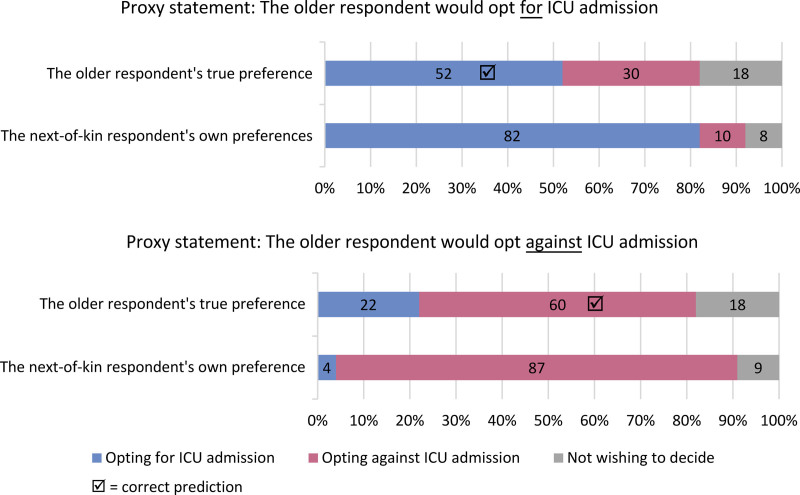
Figure 2 shows percentage agreement alongside 95% CIs for ICU admission preferences of: 1) the older respondents, 2) the next-of-kins acting as proxies on behalf of the older participants, and 3) the next-of-kins on their own behalf. Figure 3 illustrates the percentage distributions of the older respondents’ ICU admission preferences vs. the next-of-kin respondents’ own ICU admission preferences, stratified by the next-of-kins’ proxy statements.
Figure 2.
Percentage agreement with 95% CIs for ICU admission preferences of: 1) the older respondents, 2) the next-of-kins acting as proxies on behalf of the older respondents, and 3) the next-of-kins for themselves.
Figure 3.
Percentage agreement of the next of kins’ proxy prediction with the very old respondents’ true ICU admission preference (proxy accuracy) and the next of kins’ own ICU admission preference (assumed similarity).
Of all factors investigated, only the next-of-kin’s certainty regarding their proxy statement (higher certainty: higher proxy accuracy) and the age of the older respondents (higher age: lower proxy accuracy) significantly affected the odds of the next-of-kin predicting correctly. Prior communication about treatment preferences had no effect (Supplement 5, eTable 5.8, http://links.lww.com/CCX/B440). Furthermore, only 22% (28/127) of all older/next-of-kin pairs agreed that they had had such a conversation before participating in the study. The remaining stated either that they had no communication on the topic (44%) or did not agree on whether they had such a conversation (34%).
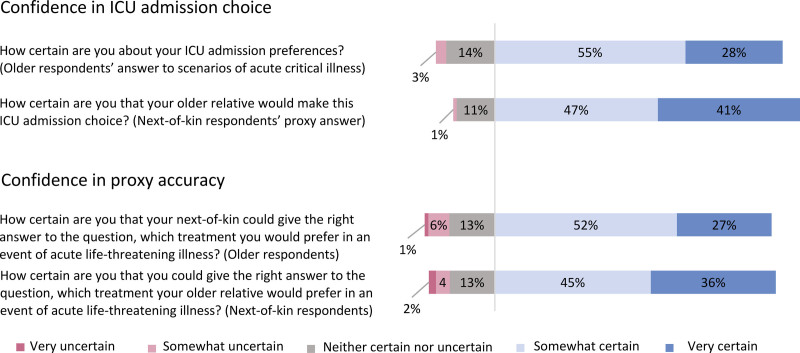
Confidence Regarding ICU Admission Choices and Proxy Accuracy
Most older participants and their next-of-kin stated being either “very confident” or “somewhat confident” both in their ICU admission choices and in proxy accuracy (Fig. 4). We show confidence levels stratified by ICU admission preference in Supplement 5, eTable 5.9 (http://links.lww.com/CCX/B440).
Figure 4.
Percentage distribution of very old and next-of-kin respondents’ confidence in their ICU admission choices and in proxy accuracy on a 5-point scale.
DISCUSSION
In this cross-sectional survey of a purposive sample of Norwegian outpatients’ 80 years old or older, the majority had a clear and consistent ICU admission preference. In hypothetical scenarios of acute critical illness, they opted for and against ICU admission equally often (approximately 40%), while a minor proportion (21%) preferred to leave the decision to somebody else. Among respondent characteristics, only male gender, religiosity, and prior ICU experience increased the likelihood of opting for ICU admission. The proxy statements of the next-of-kin respondents aligned significantly more with the proxies’ own treatment preferences than with the older respondents’ true preferences. Overall, confidence levels were high in the choices made and in proxy accuracy.
Variations in Older Adults’ ICU Admission Preferences
The older respondents of this study expressed a large variation in ICU admission preferences, with two-thirds having a consistent preference regardless of the acute illness scenario presented. Our findings align with evidence from other studies addressing treatment intensity preferences of older patients in different healthcare settings (19–21). Surprisingly, the most robust prognostic markers of ICU survival, such as age, frailty, and comorbidity (22, 23), did not significantly alter the older respondents’ own ICU admission preferences.
We observed gender differences, with male gender increasing the odds of opting for ICU admission more than two-fold, which also persisted when adjusted for age, marital status, healthcare professional background, and other factors. Despite females living longer than men, more men vs. women are admitted to ICUs worldwide. Male predominance in ICU utilization is mainly explained by biological and social differences (24). A systematic review also found that women are more likely to have LST limitations (25). Few studies have addressed gender differences in patients’ treatment preferences. Two studies have shown that older women and female cancer patients wished for lower treatment intensity than their male counterparts (26, 27).
Additionally, in our study, there was some evidence of religious respondents being more likely to opt for ICU admission, which corresponds to existing literature showing that religiosity correlates with treatment intensity regarding both patients, healthcare professionals, and healthcare context characteristics (28–31).
Finally, healthcare experience (especially ICU exposure as a patient or relative) greatly impacted the likelihood of opting for ICU admission. The relationship between healthcare experience and treatment intensity preferences has been barely addressed so far; however, a recent study showed that most older survivors of major acute abdominal surgery would choose to undergo the same procedure once again (32).
Proxy Accuracy, Assumed Similarity, and Family Involvement
Proxy accuracy was weak in our study, which aligns with existing evidence (9, 10). Paradoxically, this evidence, alongside ethical concerns related to the substituted judgment standard (33, 34), has remained largely unrecognized in clinical practice and healthcare governance, where proxy statements are frequently instrumentalized to bolster the autonomy of incapacitated patients.
Additionally, we found that the next-of-kins’ proxy statements aligned more with their own preferences than with the older respondents’ preferences. This observation indicates an underlying cognitive error frequently referred to as “assumed similarity,” a term describing the convergence of how we perceive ourselves and other individuals (35). Assumed similarity has been recognized in many areas of human interactions but only infrequently in medical research (36, 37). Its extent might still be underestimated in our sample, as we could not control interactions within respondent pairs during survey completion.
We found a marked incongruence between limited proxy accuracy and high levels of confidence in proxy judgments among both older respondents and their next-of-kin. However, acknowledging the weaknesses of proxy statements regarding treatment preferences should not devalue family involvement. Instead, family conferences might become an arena of shared uncertainty management (38) and shared best-interest assessment when the patient’s treatment preferences remain unknown (39). Time-limited ICU trials may include these aspects (40). Furthermore, involving family members at earlier stages in advance care planning might improve the likelihood that they will know the older patient’s treatment intensity preferences in the event of critical illness (19).
Limitations
Our study has several weaknesses. First, although hypothetical scenario research is an acknowledged method for exploring decision-making, it is based on counterfactual conditionals and its validity has been debated (41–43). Second, the internal validity of the presented data may have been negatively affected by sampling and response bias, especially concerning gender differences and ICU experience. Third, the external validity of these findings in other contexts and settings is unknown and may be limited. The Norwegian healthcare context is characterized by extraordinarily high levels of societal trust (44), and rates of ICU death after LST limitations are among the highest in the world (45, 46). Additionally, we excluded immigrants with low levels of fluency in Norwegian, incapacitated patients, severely frail patients, and permanent nursing home residents from study participation. Further research is needed to study this unique and exceptionally vulnerable patient population.
Implications
The findings of our study illustrate the complexity and multidimensional uncertainty clinicians’ face when making ICU admission decisions for older critically ill patients (47). They also elicit reflections on the ethical determinants of decision-making regarding treatment intensity for this large patient group (48, 49).
The survey instrument proved feasible and may be adapted to address this topic on larger random samples. Given anticipated demographic changes and ICU resource constraints (47), more research into older patients’ treatment intensity preferences and strategies for integrating these preferences in clinical decision-making will be increasingly important. Future studies addressing cultural differences between units, countries, and regions may yield interesting results.
Furthermore, geriatric intermediate care may offer more personally tailored treatment intensity with similar outcomes at lower costs compared with intensive care (50). Patients’ and next-of-kins’ knowledge and perception of geriatric intermediate care and noninvasive organ-support are not well described and may be explored with an adaptation of the presented instrument.
CONCLUSIONS
Many older respondents in this study had a clear and consistent ICU admission preference. We found large variations in their ICU admission preferences unrelated to their medical condition and other prognostic markers of ICU outcome. However, gender, religiosity, and prior ICU experience seemed to affect their ICU admission choices. The next-of-kin respondents’ ability to state the older participants’ ICU admission preferences was limited. Since most older patients do not retain capacity at the time of ICU admission, and proxy statements are prone to large errors, the older patients’ treatment preferences may remain unknown in the event of critical illness. Even though these findings are derived from a selected Norwegian sample with limited generalizability, they illustrate the universal human quandary faced in geriatric intensive care, where treatment-intensity decisions are made under a wide range of uncertainty regarding the outcome of intensive care and the patient’s likely will.
ACKNOWLEDGMENTS
We thank our user advisory group, consisting of Randi Hag, Ranveig Skjønborg, and Odd Himle, for generously providing insights into their perception of the research objective and for their important input during all stages of this project. We are also indebted to all focus group participants, volunteering senior citizens, and their next-of-kins for their valuable contributions to questionnaire development, testing, and validation. Finally, we thank Brit Sjøbø for her commitment to the project as a research nurse and sparring partner.
Supplementary Material
Footnotes
Dr. Schwarz is currently receiving a PhD fellowship grant from the Western Norway Regional Health Authority (Helse Vest RHF) No. F-12588/4800005953 (2021–2026). Dr. Flaatten received an open research grant for another project on a related topic (Intensive Care of Very Old Patients) from 2019 to 2023, awarded by Helse Vest RHF. The remaining authors have disclosed that they do not have any potential conflicts of interest.
ClinicalTrials.gov NCT05149040 (October 31, 2021).
Preprint: doi.org/10.21203/rs.3.rs-4142290/v1 (Research Square).
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Contributor Information
Elisabeth Skaar, Email: elisabeth.skaar@helse-bergen.no.
Ingrid Miljeteig, Email: Ingrid.Miljeteig@uib.no.
Karl Ove Hufthammer, Email: karl.ove.hufthammer@hvl.no.
Karen E. A. Burns, Email: Karen.Burns@unityhealth.to.
Reidar Kvåle, Email: reidar.kvale@helse-bergen.no.
Hans Flaatten, Email: hans.kristian.flaatten@helse-bergen.no.
Margrethe A. Schaufel, Email: margrethe.aase.schaufel@helse-bergen.no.
REFERENCES
- 1.Boumendil A, Somme D, Garrouste-Orgeas M, et al. : Should elderly patients be admitted to the intensive care unit? Intensive Care Med 2007; 33:1252. [DOI] [PubMed] [Google Scholar]
- 2.Laake JH, Dybwik K, Flaatten HK, et al. : Impact of the post-World War II generation on intensive care needs in Norway. Acta Anaesthesiol Scand 2010; 54:479–484 [DOI] [PubMed] [Google Scholar]
- 3.Guidet B, Leblanc G, Simon T, et al. ; ICE-CUB 2 Study Network: Effect of systematic intensive care unit triage on long-term mortality among critically ill elderly patients in France: A randomized clinical trial. JAMA 2017; 318:1450–1459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heyland D, Cook D, Bagshaw SM, et al. ; Canadian Critical Care Trials Group: The very elderly admitted to ICU: A quality finish? Crit Care Med 2015; 43:1352–1360 [DOI] [PubMed] [Google Scholar]
- 5.Garrouste-Orgeas M, Tabah A, Vesin A, et al. : The ETHICA study (part II): Simulation study of determinants and variability of ICU physician decisions in patients aged 80 or over. Intensive Care Med 2013; 39:1574–1583 [DOI] [PubMed] [Google Scholar]
- 6.Mousai O, Tafoureau L, Yovell T, et al. : The role of clinical phenotypes in decisions to limit life-sustaining treatment for very old patients in the ICU. Ann Intensive Care 2023; 13:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferrand E, Bachoud-Levi AC, Rodrigues M, et al. : Decision-making capacity and surrogate designation in French ICU patients. Intensive Care Med 2001; 27:1360–1364 [DOI] [PubMed] [Google Scholar]
- 8.Neumann PJ, Araki SS, Gutterman EM: The use of proxy respondents in studies of older adults: Lessons, challenges, and opportunities. J Am Geriatr Soc 2000; 48:1646–1654 [DOI] [PubMed] [Google Scholar]
- 9.Shalowitz DI, Garrett-Mayer E, Wendler D: The accuracy of surrogate decision makers: A systematic review. Arch Intern Med 2006; 166:493–497 [DOI] [PubMed] [Google Scholar]
- 10.Spalding R: Accuracy in surrogate end-of-life medical decision-making: A critical review. Appl Psychol Health Well Being 2021; 13:3–33 [DOI] [PubMed] [Google Scholar]
- 11.Johansson M, Broström L, Brostrom L: Turning failures into successes: A methodological shortcoming in empirical research on surrogate accuracy. Theor Med Bioeth 2008; 29:17–26 [DOI] [PubMed] [Google Scholar]
- 12.Pearlman RA, Starks H, Cain KC, et al. : Improvements in advance care planning in the Veterans affairs system: Results of a multifaceted intervention. Arch Intern Med 2005; 165:667–674 [DOI] [PubMed] [Google Scholar]
- 13.Flaatten H, de Lange DW, Artigas A, et al. : The status of intensive care medicine research and a future agenda for very old patients in the ICU. Intensive Care Med 2017; 43:1319–1328 [DOI] [PubMed] [Google Scholar]
- 14.Burns KEA, Cook DJ, Xu K, et al. ; Canadian Critical Care Trials Group: Differences in directives to limit treatment and discontinue mechanical ventilation between elderly and very elderly patients: A substudy of a multinational observational study. Intensive Care Med 2023; 49:1181–1190 [DOI] [PubMed] [Google Scholar]
- 15.Burns KE, Duffett M, Kho ME, et al. ; ACCADEMY Group: A guide for the design and conduct of self-administered surveys of clinicians. CMAJ 2008; 179:245–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stawicki S, Kalra S, Jones C, et al. : Comorbidity polypharmacy score and its clinical utility: A pragmatic practitioner′s perspective. J Emerg Trauma Shock 2015; 8:224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rockwood K, Theou O: Using the clinical frailty scale in allocating scarce health care resources. Can Geriatr J 2020; 23:210–215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herdman M, Gudex C, Lloyd A, et al. : Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011; 20:1727–1736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Detering KM, Hancock AD, Reade MC, et al. : The impact of advance care planning on end of life care in elderly patients: Randomised controlled trial. BMJ 2010; 340:c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Philippart F, Vesin A, Bruel C, et al. : The ETHICA study (part I): Elderly’s thoughts about intensive care unit admission for life-sustaining treatments. Intensive Care Med 2013; 39:1565–1573 [DOI] [PubMed] [Google Scholar]
- 21.Le Guen J, Boumendil A, Guidet B, et al. : Are elderly patients’ opinions sought before admission to an intensive care unit? Results of the ICE-CUB study. Age Ageing 2016; 45:303–309 [DOI] [PubMed] [Google Scholar]
- 22.Muscedere J, Waters B, Varambally A, et al. : The impact of frailty on intensive care unit outcomes: A systematic review and meta-analysis. Intensive Care Med 2017; 43:1105–1122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guidet B, de Lange DW, Boumendil A, et al. ; VIP2 study group: The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: The VIP2 study. Intensive Care Med 2020; 46:57–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Merdji H, Long MT, Ostermann M, et al. : Sex and gender differences in intensive care medicine. Intensive Care Med 2023; 49:1155–1167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McPherson K, Carlos WG, 3rd, Emmett TW, et al. : Limitation of life-sustaining care in the critically ill: A systematic review of the literature. J Hosp Med 2019; 14:303–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bookwala J, Coppola KM, Ditto PH, et al. : Gender differences in older adults’ preferences for life-sustaining medical treatments and end-of-life values. Death Stud 2001; 25:127–149 [DOI] [PubMed] [Google Scholar]
- 27.Saeed F, Hoerger M, Norton SA, et al. : Preference for palliative care in cancer patients: Are men and women alike? J Pain Symptom Manage 2018; 56:1–6.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Halvorsen K, Førde R, Nortvedt P: Value choices and considerations when limiting intensive care treatment: A qualitative study. Acta Anaesthes Scand 2009; 53:10–17 [DOI] [PubMed] [Google Scholar]
- 29.Bülow H-H, Sprung CL, Baras M, et al. : Are religion and religiosity important to end-of-life decisions and patient autonomy in the ICU? The Ethicatt study. Intensive Care Med 2012; 38:1126–1133 [DOI] [PubMed] [Google Scholar]
- 30.Sprung CL, Cohen SL, Sjokvist P, et al. ; Ethicus Study Group: End-of-life practices in European intensive care units: The Ethicus study. JAMA 2003; 290:790–797 [DOI] [PubMed] [Google Scholar]
- 31.Guidet B, Flaatten H, Boumendil A, et al. ; VIP1 study group: Withholding or withdrawing of life-sustaining therapy in older adults (>/= 80 years) admitted to the intensive care unit. Intensive Care Med 2018; 44:1027–1038 [DOI] [PubMed] [Google Scholar]
- 32.Tengberg LT, Foss NB, Lauritsen ML, et al. : The impact of acute high-risk abdominal surgery on quality of life in elderly patients. Dan Med J 2017; 64:A5371. [PubMed] [Google Scholar]
- 33.Brostrom L, Johansson M, Nielsen MK: “What the patient would have decided”: A fundamental problem with the substituted judgment standard. Med Health Care Philos 2007; 10:265–278 [DOI] [PubMed] [Google Scholar]
- 34.Johansson M, Brostrom L: Empirical fallacies in the debate on substituted judgment. Health Care Anal 2014; 22:73–81 [DOI] [PubMed] [Google Scholar]
- 35.Thielmann I, Hilbig BE: Assumed similarity. In: Cognitive Illusions: Intriguing Phenomena in Thinking, Judgment, and Memory. Pohl RF. (Ed). London, United Kingdom, Routledge, 2022, pp 272–286 [Google Scholar]
- 36.Fagerlin A, Ditto PH, Danks JH, et al. : Projection in surrogate decisions about life-sustaining medical treatments. Health Psychol 2001; 20:166–175 [PubMed] [Google Scholar]
- 37.McDade-Montez E, Watson D, Beer A: Similarity, agreement, and assumed similarity in proxy end-of-life decision making. Fam Syst Health 2013; 31:366–381 [DOI] [PubMed] [Google Scholar]
- 38.Han PKJ: Uncertainty in Medicine: A Framework for Tolerance. New York, NY, Oxford University Press, 2021 [Google Scholar]
- 39.Wrigley A: Proxy consent: Moral authority misconceived. J Med Ethics 2007; 33:527–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chang DW, Neville TH, Parrish J, et al. : Evaluation of time-limited trials among critically ill patients with advanced medical illnesses and reduction of nonbeneficial ICU treatments. JAMA Intern Med 2021; 181:786–794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wiseman DB, Levin IP: Comparing risky decision making under conditions of real and hypothetical consequences. Organ Behav Hum Decis Process 1996; 66:241–250 [Google Scholar]
- 42.Kühberger A, Schulte-Mecklenbeck M, Perner J: Framing decisions: Hypothetical and real. Organ Behav Hum Decis Process 2002; 89:1162–1175 [Google Scholar]
- 43.Exum ML, Bouffard JA: Testing theories of criminal decision making: Some empirical questions about hypothetical scenarios. In: Handbook of Quantitative Criminology. Piquero AR, Weisburd D. (Eds). New York, NY, Springer Science+Business Media, 2010, pp 581–594 [Google Scholar]
- 44.Ortiz-Ospina E, Roser M, Arriagada P: Trust. Our World in Data. 2016. Available at: https://ourworldindata.org/trust. Accessed November 9, 2023 [Google Scholar]
- 45.Andersen FH, Ariansen Haaland O, Klepstad P, et al. : Frailty and survival in elderly intensive care patients in Norway. Acta Anaesthesiol Scand 2021; 65:1065–1072 [DOI] [PubMed] [Google Scholar]
- 46.Mark NM, Rayner SG, Lee NJ, et al. : Global variability in withholding and withdrawal of life-sustaining treatment in the intensive care unit: A systematic review. Intensive Care Med 2015; 41:1572–1585 [DOI] [PubMed] [Google Scholar]
- 47.Guidet B, Vallet H, Flaatten H, et al. : The trajectory of very old critically ill patients. Intensive Care Med 2024; 50:181–194 [DOI] [PubMed] [Google Scholar]
- 48.Sullivan MD: The illusion of patient choice in end-of-life decisions. Am J Geriatr Psychiatry 2002; 10:365–372 [PubMed] [Google Scholar]
- 49.Dreyer A, Forde R, Nortvedt P: Autonomy at the end of life: Life-prolonging treatment in nursing homes—relatives’ role in the decision-making process. J Med Ethics 2009; 35:672–677 [DOI] [PubMed] [Google Scholar]
- 50.Thietart S, Boumendil A, Pateron D, et al. ; ICE-CUB2 Study Network: Impact on 6-month outcomes of hospital trajectory in critically ill older patients: Analysis of the ICE-CUB2 clinical trial. Ann Intensive Care 2022; 12:65. [DOI] [PMC free article] [PubMed] [Google Scholar]