Abstract
Unemployment has been associated with increased risk of cardiovascular disease (CVD) and all-cause mortality. However, factors behind this association remain unsettled. A primary care CVD prevention programme was conducted in two Finnish towns in 2005–07. Of the participants (n = 4450), a cohort of apparently healthy CVD risk subjects belonging to the labour force (n = 1487) was identified. Baseline depressive symptoms were assessed by Beck’s Depression Inventory. Data on employment status and mortality were obtained from official statistics. The effect of employment status and depressive symptoms on all-cause mortality after a median follow-up of 15 years was estimated in models adjusted for age, sex, body mass index, non-high-density lipoprotein cholesterol, physical activity, alcohol use, current smoking, glucose metabolism, and hypertension. In comparison to employed non-depressive subjects, fully adjusted hazard ratio (HR) for all-cause mortality was 3.53 (1.90–6.57) in unemployed subjects with increased depressive symptoms, 1.26 (0.68–2.34) in unemployed non-depressive subjects, and 1.09 (0.63–1.90) in employed depressive subjects. Factors independently associated with mortality were unemployment with increased depressive symptoms [HR 3.56 (95% CI 1.92–6.61)], screen-detected diabetes [HR 2.71 (95% CI 1.59–4.63)], current smoking [HR 1.77 (95% CI 1.19–2.65)], and higher age [HR 1.10 (95% CI 1.05–1.15)]. Unemployment in itself was not associated with all-cause mortality. If unemployment was accompanied with increased depressive symptoms, risk of death was significantly elevated.
Introduction
It has been estimated that 13.17 million persons in the European Union were unemployed in October 2024 [1]. In Finland, 6.8% of the total labour force was unemployed in 2022 [2]. At an individual level, the consequences of being unemployed can be devastating. Unemployment has been associated with increased risk of cardiovascular disease (CVD) and all-cause mortality in several studies [3–10]. However, the possible mediating and confounding factors behind this association remain unsettled.
It is known that unemployment may predispose to harmful health behaviours such as smoking and excess alcohol usage [11–14]. On the other hand, persons with adverse lifestyle habits may be more likely to become unemployed [15]. One explanation for the unemployment–mortality association is that individuals with pre-existing health conditions are more likely to become and remain unemployed [16, 17]. A survey conducted in 10 European Union countries revealed that a self-perceived poor health, some chronic diseases such as depression and diabetes, high body mass index (BMI), and lack of physical activity (PA) were more prevalent among unemployed and retired persons than among employed persons [18]. Moreover, unemployed individuals show more mental distress, depression, anxiety, and psychosomatic symptoms than employed persons [19]. CVD risk factor screening with behavioural counselling and stress-management interventions have been recommended for unemployed individuals to overcome adverse health outcomes [3].
The present study aims to assess if the association of unemployment and all-cause mortality is affected by depressive symptoms in apparently healthy CVD risk subjects who had participated a CVD prevention programme.
Methods
Study population
Study subjects were participants in a population survey, the Harmonica Project (Harjavalta Risk Monitoring for Cardiovascular Disease) conducted in two Finnish towns, Harjavalta and Kokemäki, in 2005–07. An information letter, a CVD risk factor survey, a tape for measuring waist circumference, and Type 2 diabetes risk assessment form (FINDRISC, Finnish Diabetes Risk Score) [20] were posted to all non-institutionalized 45–70-year-old inhabitants (n = 6103). All subjects were of Caucasian origin. Participation rate was 74% (n = 4450). A subject was considered to be at CVD risk if she/he had at least one of the assessed risk factors: waist circumference ≥80 cm in women and ≥94 cm in men (in Harjavalta), use of antihypertensive medication, latest measured blood pressure (BP) ≥140/90 mmHg, history of gestational diabetes or hypertension, FINDRISC-score ≥12 in Harjavalta or ≥15 in Kokemäki, family history of ischaemic heart disease, myocardial infarction, or stroke. In Kokemäki, more stringent inclusion criteria were applied for logistical reasons due to limited financial resources.
CVD risk subjects (n = 3072) attended laboratory tests and an appointment with a public health nurse. Patients with previously diagnosed CVD, diabetes, or chronic kidney disease were excluded. Participation and tests were free of charge for the study subjects.
For this analysis, we included subjects aged 45–65 years belonging to the active labour force (currently employed or unemployed but actively seeking work) and who had completed Beck’s Depression Inventory (BDI) [21] (n = 1487).
Questionnaires and measurements
Self-administered questionnaires were filled in before the nurse’s appointment: sociodemographic factors, smoking status, PA, regular medication usage, BDI [21], Alcohol Use Disorders Identification Test (AUDIT) [22], dietary fat survey, self-rated health (Short-Form Health Survey, first question) [23], and health-related quality of life (EuroQol instrument EQ-5D-3L) [24].
The definition of increased depressive symptoms was a BDI-score ≥10 [25]. AUDIT score ≥8 was considered indicating increased risk for alcohol harm [22]. Frequency of PA was categorized as follows: (i) high: PA ≥30 min at a time for at least six times a week, (ii) moderate: PA ≥30 min at a time for four to five times a week, and (iii) low: PA ≥30 min at a time for maximum three times a week. Dietary fat survey (by the Finnish Heart Association) assessed the amount and quality of dietary fat with a score range of 0–28, the higher score indicating a healthier diet.
Laboratory tests were performed after at least 12-h fasting. Two-hour oral glucose tolerance test with a glucose load of 75 g was performed from capillary blood (HemoCue Glucose 201+ system). Venous plasma was used to measure total cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides enzymically (Olympus AU604). Non-HDL cholesterol was calculated as the difference between total cholesterol and HDL cholesterol. Low-density lipoprotein cholesterol was calculated according to the Friedewald’s formula. Glucose disorders were classified according to the World Health Organization (WHO) criteria [26]. Impaired fasting glucose and impaired glucose tolerance were classified as prediabetes.
Trained public health nurses performed clinical examination. Height and weight were measured with subjects in a standing position without shoes and outer garments. BMI was calculated by dividing weight (kg) by the square of height (m2). BP was measured with subjects in a sitting posture after resting at least for 5 min with the cuff placed on the arm. The mean of two BP measurements was used in the study. If the nurse measured systolic BP ≥140 mmHg or diastolic BP ≥90 mmHg and the subject did not have ongoing antihypertensive medication, a home BP device was lent to the subject. Duplicate BP measurements were instructed to be performed in the morning and evening for 1 week. Hypertension was defined as the subject having antihypertensive medication, or the mean of home BP measurements ≥135/85 mmHg.
Intervention
Public health nurses gave individual lifestyle counselling to all study subjects. The main goals were to reduce intake of saturated fat in the diet, to perform PA at least 30 min per day or 4 h per week, overweight and obese subjects (BMI ≥25.0 kg/m2) were encouraged to weight reduction of at least 5%, smokers and risk users of alcohol were encouraged to reduce these unhealthy habits.
A person was considered to be at high CVD risk if she/he had hypertension, diabetes, impaired glucose tolerance, metabolic syndrome [27], obesity (BMI ≥30.0 kg/m2), or 10-year risk for CVD death ≥5% estimated by the Systematic Coronary Risk Evaluation (SCORE) [28]. With such a risk for fatal CVD events, preventive medication for hypertension or dyslipidaemia and low-dose aspirin was prescribed. According to national guidelines at that time, antihypertensive medication was initiated if systolic BP ≥160 mmHg or diastolic BP ≥100 mmHg or target organ damage was diagnosed. Antihypertensive medication was intensified if systolic BP ≥140 mmHg or diastolic BP ≥85 mmHg (≥80 mmHg in patients with diabetes).
Register-based data
Data on socio-economic groups and mortality were obtained from the Official Statistics of Finland provided by Statistics Finland. Classification of socioeconomic groups was as follows: (i) self-employed persons, (ii) upper-level employees with administrative, managerial, professional, and related occupations, (iii) lower-level employees with administrative and clerical occupations, (iv) manual workers, and (v) long-term unemployed persons. Groups i–iv were pooled to form the employed group.
Subjects were defined as unemployed if their unemployment had lasted at least 6 months. For each subject, the date of the study visit was the start date of follow-up period, which ended on 31 December 2020.
Ethical approval
The study protocol and consent forms were reviewed and approved by the ethics committee of Satakunta hospital district. All participants provided written informed consent for the project and subsequent medical research.
Statistical analysis
Summary statistics were described using mean and standard deviation, median and interquartile range, or numbers as percentages. The baseline characteristics between employed and unemployed groups were analysed by using Student’s t-test, Mann–Whitney U-test, and Pearson’s chi-squared test. Relative survival, the ratio between the observed survival proportion in a patient group and the expected survival proportion, was calculated by the Ederer II method. The ratio between observed and expected number of deaths, standardized mortality ratio (SMR), was calculated using subject-years methods with 95% confidence intervals (CIs), assuming a Poisson distribution. The expected number of deaths was calculated on the basis of sex-, age-, and calendar-period-specific mortality rates in the Finnish population (Official Statistics of Finland). The expected number was determined by multiplying the person-years of observation by the appropriate mortality rate in the general population according to categories of sex, 1-year age group, and calendar period. The relative SMR (rSMR) was defined as the ratio of the BDI (rSMR – BDI ≥ 10/SMR – BDI < 10). Relative SMRs were estimated using Poisson regression models. Crude cumulative rate of all-cause mortality was estimated using Kaplan–Meier method and compared between groups with the log-rank test. Cox proportional hazards regression was used to estimate the adjusted hazard ratios (HR) and their 95% CIs. Age, sex, education years, BMI, non-HDL cholesterol, PA, AUDIT score, current smoking, glucose metabolism, and hypertension were used as covariates in these models when appropriate. A possible nonlinear relationship between employment status and the BDI summary score was assessed by using three-knot restricted cubic spline Cox regression models. The length of the distribution of knots was located at the 10th, 50th, and 90th percentiles. For restricted cubic splines, also known as natural splines, knot locations are based on Harrell’s recommended percentiles. All analyses were performed using STATA 18.0 (StataCorp LP, College Station, TX).
Results
Characteristics of the study subjects
We evaluated 1487 subjects in the active labour force, of whom 156 (10.4%) were unemployed at baseline. The prevalence of increased depressive symptoms (BDI ≥10) was 14.6% (194/1331) among employed and 26.9% (42/156) among unemployed subjects (P < .001). Unemployed individuals were on an average older, more often living alone, less educated, used more alcohol, and performed more PA than employed subjects. Health-related quality of life and self-rated health were worse among unemployed than among employed subjects. BMI, BP, and triglyceride concentration were higher in unemployed subjects who also had more often hypertension, antidepressive medication, and a higher amount of regular medication than employed subjects at baseline (Table 1).
Table 1.
Characteristics of the study subjects at baseline
| Employed N = 1331 | Unemployed N = 156 | P-value | |
|---|---|---|---|
| Women, n (%) | 603 (45) | 71 (46) | .96 |
| Age (years), mean (SD) | 54 (5) | 55 (5) | <.001 |
| Cohabiting, n (%) | 1086 (82) | 115 (74) | .018 |
| Education (years), median (IQR) | 11.3 (2.5) | 10.0 (2.1) | <.001 |
| Current smoker, n (%) | 269 (20) | 40 (26) | .11 |
| AUDIT score, median (IQR) | 5.2 (4.8) | 6.6 (6.9) | <.001 |
| Physical activity, n (%) | <.001 | ||
| Low | 261 (20) | 29 (19) | |
| Moderate | 770 (58) | 66 (42) | |
| High | 300 (23) | 61 (39) | |
| Dietary fat score, mean (SD) | 17.7 (5.3) | 17.4 (5.3) | .55 |
| EQ-5D, mean (SD) | 0.858 (0.152) | 0.823 (0.167) | .009 |
| Self-rated health good, n (%) | 957 (72) | 92 (59) | <.001 |
| Beck’s Depression Inventory score, mean (SD) | 5.1 (5.3) | 6.9 (6.3) | <.001 |
| Body mass index (kg/m2), mean (SD) | 28.3 (4.6) | 29.4 (5.4) | .007 |
| Blood pressure (mmHg), mean (SD) | |||
| Systolic | 137 (18) | 140 (17) | .022 |
| Diastolic | 85 (10) | 87 (11) | .051 |
| Plasma glucose (mmol/l), mean (SD) | |||
| Fasting | 5.54 (1.09) | 5.62 (1.12) | .38 |
| 2-h postload | 7.01 (1.97) | 7.26 (2.40) | .15 |
| Plasma lipids (mmol/l), mean (SD) | |||
| Total cholesterol | 5.41 (0.94) | 5.42 (0.90) | .87 |
| LDL cholesterol | 3.27 (0.85) | 3.26 (0.82) | .90 |
| HDL cholesterol | 1.55 (0.43) | 1.50 (0.43) | .15 |
| Non-HDL cholesterol | 3.85 (0.94) | 3.92 (0.89) | .42 |
| Triglycerides | 1.35 (0.75) | 1.51 (0.72) | .010 |
| Hypertension, n (%) | 773 (58) | 105 (67) | .027 |
| Glucose metabolism, n (%) | .090 | ||
| Normal | 1012 (76) | 106 (68) | |
| Prediabetes | 129 (10) | 17 (11) | |
| Diabetes | 116 (9) | 18 (12) | |
| Regular medication, n (%) | |||
| Antilipids | 109 (8) | 17 (11) | .25 |
| Antihypertensives | 348 (26) | 47 (30) | .29 |
| Antidepressants | 38 (3) | 14 (9) | <.001 |
| Number of medications, mean (SD) | 0.8 (1.3) | 1.2 (1.8) | <.001 |
IQR, interquartile range; AUDIT, Alcohol Use Disorders Identification Test; EQ-5D, EuroQol; LDL, low-density lipoprotein; HDL, high-density lipoprotein.
Mortality
There were 121 deaths during the 14-year follow-up. Table 2 shows data on median follow-up time, number of deaths, person-years followed-up, number of retired subjects during follow-up, crude mortality rate, and SMR according to employment status and depressive symptoms. Crude mortality rate was higher among unemployed subjects with increased depressive symptoms than in other study groups. Compared to the aged-matched general population of Finland, mortality was 2.48 times higher in unemployed and depressive subjects.
Table 2.
Mortality data according to employment status and depressive symptoms
| Employed |
Unemployed |
P-value (multiple comparison) | |||
|---|---|---|---|---|---|
| BDI <10 | BDI ≥10 | BDI <10 | BDI ≥10 | ||
| N = 1137 | N = 194 | N = 114 | N = 42 | ||
| Follow-up time (years), median (IQR) | 15.4 | 15.4 | 15.6 | 15.0 | – |
| (14.9–15.9) | (14.9–15.9) | (14.9–16.0) | (13.5–15.9) | ||
| Number of deaths | 80 | 16 | 12 | 13 | – |
| Person years of follow-up | 17 124 | 2898 | 1703 | 566 | – |
| Retired during follow-up, n (%) | 836 (74) | 153 (79) | 95 (83) | 32 (76) | .069 |
| Mortality at end of follow-up, % (95% confidence interval)* | 7.7 | 8.1 | 12.8 | 34.1 | <.001a |
| (6.2–9.7) | (4.9–13.1) | (7.1–22.4) | (20.6–53.0) | ||
| Standardized mortality ratio (95% confidence interval) | 0.53 | 0.69 | 0.69 | 2.48 | <.001b |
| (0.43–0.66) | (0.43–1.13) | (0.39–1.22) | (1.43–4.27) | ||
BDI, Beck’s depression inventory; IQR, interquartile range.
Kaplan–Meier estimate.
Unemployed subjects with increased depressive symptoms differ from other groups after Sidak correction (multiple testing) to control Type-I error across comparisons (P < .05).
Cumulative all-cause mortality
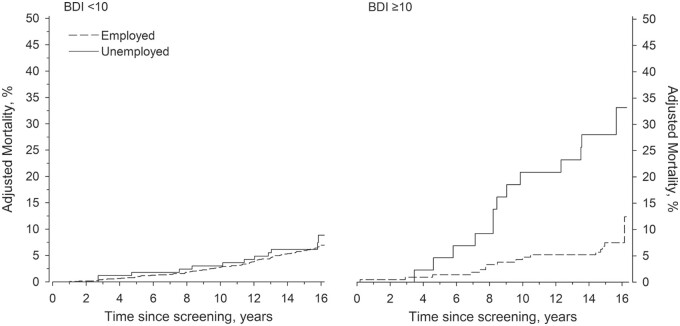
Age- and sex-adjusted cumulative all-cause mortality was significantly higher in unemployed individuals with increased depressive symptoms than without (Fig. 1).
Figure 1.
Cumulative all-cause mortality according to employment status in subjects without and with increased depressive symptoms. Adjustments were made for age and sex. BDI, Beck’s Depression Inventory.
HR for all-cause mortality
Age- and sex-adjusted HR for all-cause mortality was 1.30 (95% CI 0.71–2.39) among subjects with BDI < 10, and 3.75 (95% CI 1.78–7.93) among those with BDI ≥10.
In comparison to employed non-depressive subjects, HR for all-cause mortality was 3.53 (1.90–6.57) in unemployed subjects with increased depressive symptoms, 1.26 (0.68–2.34) in unemployed non-depressive subjects, and 1.09 (0.63–1.90) in employed depressive subjects after adjustments for age, sex, education years, BMI, non-HDL cholesterol, PA, AUDIT score, current smoking, glucose metabolism, and presence of hypertension.
Regarding HR for all-cause mortality between unemployed and employed subjects according to continuous BDI summary score, see Supplementary Fig. S1.
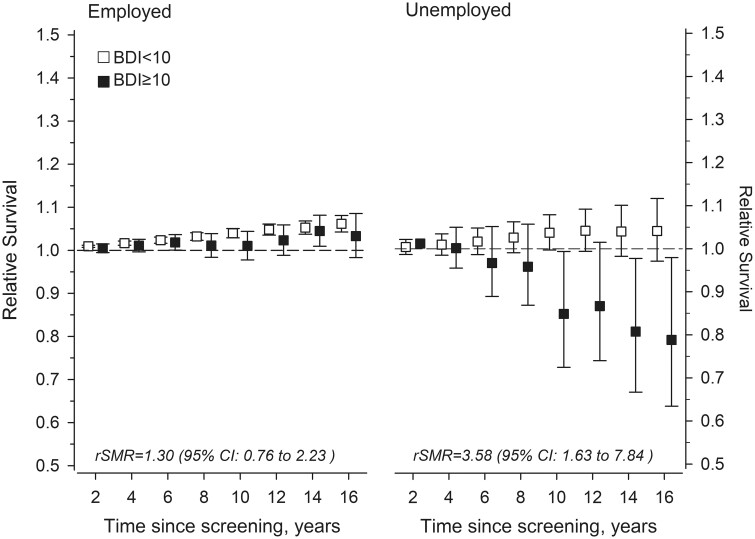
Relative survival and SMR
Relative survival among non-depressed employed individuals was higher than in the age-matched general population during the follow-up. There was no difference in survival between non-depressed and depressed employed subjects. In unemployed individuals with increased depressive symptoms, relative survival decreased almost linearly during follow-up and was eventually lower than in the general population. Survival among non-depressed unemployed persons was comparable to the general population (Fig. 2).
Figure 2.
Relative survival and relative standardized mortality ratios (rSMR) according to employment status and depressive symptoms. BDI, Beck’s Depression Inventory.
Multivariable adjusted HRs for all-cause mortality
Factors independently associated with mortality were unemployment with increased depressive symptoms [HR 3.56 (95% CI 1.92–6.61)], screen-detected diabetes [HR 2.71 (95% CI 1.59–4.63)], current smoking [HR 1.77 (95% CI 1.19–2.65)], risk usage of alcohol [HR 1.54 (95% CI 1.00–2.36)], and higher age [HR 1.10 (95% CI 1.05–1.15)] (Supplementary Fig. S2).
Discussion
This study suggests that depressive symptoms modify the association between unemployment and all-cause mortality. Risk of death was elevated in unemployed subjects with increased depressive symptoms, but not among unemployed non-depressive subjects when compared to employed non-depressive individuals after adjustment for socioeconomic, lifestyle-related, and cardiometabolic risk factors. Unemployment and increased depressive symptoms were even more powerful predictors of mortality than screen-detected diabetes or smoking.
At baseline, all study subjects were apparently healthy CVD risk persons who received lifestyle counselling accompanied by preventive CVD medication if indicated. This multifactorial CVD risk factor intervention has been associated with a 13-year mortality rate comparable to the respondents who had no CVD risk factors at baseline, and significantly lower mortality rate compared to the Finnish general population [29]. Nevertheless, the impact of the intervention was not evident in unemployed subjects with increased depressive symptoms. Depression has many effects on physical health, social, and lifestyle factors. It has been associated with increased mortality risk even when symptomatology is subthreshold [30]. However, causality in the association between depression and all-cause mortality has remained unproven, in part due to inadequate adjustments for confounding factors [31, 32]. It has been reported that depression and depressive symptoms may negatively affect adherence to healthy lifestyle and to medical treatment [33, 34]. Depression has been related to many somatic consequences because of dysregulations of metabolic, autonomic, immune-inflammatory, and hypothalamic–pituitary–adrenal-axis pathways associated with its pathogenesis [35]. Furthermore, unemployment is known to impair treatment prognosis of depression [36] and thus it might prolong the negative effects of depressive symptoms. However, our adjusted analyses suggest that the increased mortality risk of unemployed depressive individuals is not solely driven by lifestyle nor metabolic risk factors.
The prevalence of increased depressive symptoms among the unemployed subjects was 27%, which is strikingly higher than that of the employed individuals among our study population. It is nevertheless in line with a recent meta-analysis suggesting that the prevalence of depressive symptoms is ∼24% among unemployed individuals [37]. There is some evidence of a bidirectional relationship between unemployment and depressive symptoms [38]. Both unemployment and depression are often ashamed conditions and thus silent and even denied. Unemployment accompanied by depressive symptoms seems to be a very toxic combination leading to poor health outcomes. Clinicians would be wise to consider depression as a modifiable risk factor, which is worth screening at least among unemployed individuals.
The main limitation of our study is the lack of exposure data during the follow-up. Evaluations of employment status, self-reported depressive symptoms, and CVD risk factors were made only at baseline. Still, depressive symptoms have been found to be rather stable over time, especially when symptomatology is mild, such as in our study, is considered [39]. Almost 80% of the study subjects retired during the long follow-up limiting consideration of employment history overtime. Although response rate to the Harmonica Project was good, there might have been non-response bias since non-respondents in preventive programmes often have a less healthy lifestyle and may have lower socioeconomic position than active participants [40]. When comparing the employed or actively work-seeking population with the general population, a possible healthy worker effect might affect the results. Although the number of unemployed persons at baseline was quite low, the follow-up time of 15 years was long enough to accumulate a sufficient number of outcome events. Furthermore, data on employment status and mortality were obtained from national registers that have high validity in Finland.
In conclusion, unemployment in itself was not associated with all-cause mortality. But if unemployment was accompanied with increased depressive symptoms, the risk of death was three times higher than among employed non-depressive persons with elevated CVD risk. Screening and treating traditional CVD risk factors is not enough to reduce mortality risk associated with unemployment. More attention should be paid to alleviate the depressive symptoms of unemployed individuals.
Supplementary Material
Contributor Information
Päivi E Korhonen, Department of General Practice, University of Turku and Southwest Finland Wellbeing Services County, Turku, Finland.
Hannu Kautiainen, Primary Health Care Unit, Kuopio University Hospital, Kuopio, Finland; Folkhälsan Research Center, Helsinki, Finland.
Ansa T Rantanen, Department of General Practice, University of Turku and Southwest Finland Wellbeing Services County, Turku, Finland.
Supplementary data
Supplementary data are available at EURPUB online.
Conflict of interest: None declared.
Funding
This study was supported by the Finnish Cultural Foundation Satakunta Regional Fund.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Key points.
Unemployment in itself was not associated with all-cause mortality.
If unemployment was accompanied with increased depressive symptoms.
Risk of death was three times higher than among employed non-depressive persons.
Screening and treating traditional CVD risk factors is not enough to reduce mortality riskassociated with unemployment.
More attention should be paid to screen and treat depressive symptoms of unemployed individuals.
References
- 1. Eurostat. The Eurostat regional yearbook 2023. https://ec.europa.eu/eurostat/en/web/products-flagship-publications/w/ks-ha-23-001 (16 June 2024, date last accessed).
- 2. International Labour Organization. ILO Modelled Estimates and Projections database (ILOEST). ilosstat.ilo.org/data (16 June 2024, date last accessed).
- 3. Roelfs DJ, Shor E, Davidson KW et al. Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Soc Sci Med 2011;72:840–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dupre ME, George LK, Liu G et al. The cumulative effect of unemployment on risks for acute myocardial infarction. Arch Intern Med 2012;172:1731–7. [DOI] [PubMed] [Google Scholar]
- 5. Méjean C, Droomers M, van der Schouw YT et al. The contribution of diet and lifestyle to socioeconomic inequalities in cardiovascular morbidity and mortality. Int J Cardiol 2013;168:5190–5. 10.1016/j.ijcard.2013.07.188 [DOI] [PubMed] [Google Scholar]
- 6. Tapia Granados JA, House JS, Ionides EL et al. Individual joblessness, contextual unemployment, and mortality risk. Am J Epidemiol 2014;180:280–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Meneton P, Kesse-Guyot E, Méjean C et al. Unemployment is associated with high cardiovascular event rate and increased all-cause mortality in middle-aged socially privileged individuals. Int Arch Occup Environ Health 2015;88:707–16. 10.1007/s00420-014-0997-7 [DOI] [PubMed] [Google Scholar]
- 8. Mosquera PA, San Sebastian M, Waenerlund AK et al. Income-related inequalities in cardiovascular disease from mid-life to old age in a Northern Swedish cohort: a decomposition analysis. Soc Sci Med 2016;149:135–44. 10.1016/j.socscimed.2015.12.017 [DOI] [PubMed] [Google Scholar]
- 9. Dunlavy AC, Juárez S, Rostila M. Employment status and risk of all-cause mortality among native- and foreign-origin persons in Sweden. Eur J Public Health 2018;28:891–7. [DOI] [PubMed] [Google Scholar]
- 10. Nie J, Wang J, Aune D et al. Association between employment status and risk of all-cause and cause-specific mortality: a population-based prospective cohort study. J Epidemiol Community Health 2020;74:428–36. [DOI] [PubMed] [Google Scholar]
- 11. Montgomery SM, Cook DG, Bartley MJ et al. Unemployment, cigarette smoking, alcohol consumption and body weight in young British men. Eur J Public Health 1998;8:21–7. [Google Scholar]
- 12. Hammarstrom A, Janlert U. Unemployment—an important predictor for future smoking: a 14-year follow-up study of school leavers. Scand J Public Health 2003;31:229–32. [DOI] [PubMed] [Google Scholar]
- 13. Reine I, Novo M, Hammarstrom A. Does the association between ill health and unemployment differ between young people and adults? Results from a 14-year follow-up study with a focus on psychological health and smoking. Public Health 2004;118:337–45. [DOI] [PubMed] [Google Scholar]
- 14. Virtanen P, Vahtera J, Broms U et al. Employment trajectory as determinant of change in health-related lifestyle: the prospective HeSsup study. Eur J Public Health 2008;18:504–8. [DOI] [PubMed] [Google Scholar]
- 15. Leino-Arjas P, Liira J, Mutanen P et al. Predictors and consequences of unemployment among construction workers: prospective cohort study. BMJ 1999;319:600–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bartley M, Owen C. Relation between socioeconomic status, employment, and health during economic change, 1973-93. BMJ 1996;313:445–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bockerman P, Ilmakunnas P. Unemployment and self-assessed health: evidence from panel data. Health Economics 2009;18:161–79. [DOI] [PubMed] [Google Scholar]
- 18. Alavinia SM, Burdorf A. Unemployment and retirement and ill-health: a cross-sectional analysis across European countries. Int Arch Occup Environ Health 2008;82:39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Paul KI, Moser K. Unemployment impairs mental health: meta-analyses. J Vocat Behav 2009;74:264–82. 10.1016/j.jvb.2009.01.001 [DOI] [Google Scholar]
- 20. Lindström J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care 2003;26:725–31. http://care.diabetesjournals.org/content/26/3/725.abstract (16 June 2024, date last accessed). [DOI] [PubMed] [Google Scholar]
- 21. Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York: Guilford Press, 1979. [Google Scholar]
- 22. Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Healthcare. Geneva: World Health Organization, 1989. [Google Scholar]
- 23. Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Ann Med 2001;33:350–7. http://www.tandfonline.com/doi/full/10.3109/07853890109002089 (16 June 2024, date last accessed). [DOI] [PubMed] [Google Scholar]
- 24. Rabin R, De Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337–43. [DOI] [PubMed] [Google Scholar]
- 25. Koponen H, Jokelainen J, Keinänen-Kiukaanniemi S et al. Depressive symptoms and 10-year risk for cardiovascular morbidity and mortality. World J Biol Psychiatry 2010;11:834–9. 10.3109/15622975.2010.486842 [DOI] [PubMed] [Google Scholar]
- 26.Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia. Report of a WHO/IDF consultation, 2006. http://care.diabetesjournals.org/content/26/3/725 (16 June 2024, date last accessed).
- 27. Alberti K, Zimmet P, Shaw J. Consensus Group IETF. the metabolic syndrome—a new worldwide definition. Lancet 2005;366:1059–62. [DOI] [PubMed] [Google Scholar]
- 28. Conroy RM, Pyörälä K, Fitzgerald AP et al. ; SCORE Project Group. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003;24:987–1003. http://www.ncbi.nlm.nih.gov/pubmed/12788299 [DOI] [PubMed] [Google Scholar]
- 29. Kuneinen SM, Eriksson JG, Kautiainen H et al. The feasibility and outcome of a community-based primary prevention program for cardiovascular disease in the 21st century. Scand J Prim Health Care 2021;39:157–65. 10.1080/02813432.2021.1913893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cuijpers P, Vogelzangs N, Twisk J et al. Differential mortality rates in major and subthreshold depression: meta-analysis of studies that measured both. Br J Psychiatry 2013;202:22–7. 10.1192/bjp.bp.112.112169 [DOI] [PubMed] [Google Scholar]
- 31. Machado MO, Veronese N, Sanches M et al. The association of depression and all-cause and cause-specific mortality: an umbrella review of systematic reviews and meta-analyses. BMC Med 2018;16:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Miloyan B, Fried E. A reassessment of the relationship between depression and all-cause mortality in 3,604,005 participants from 293 studies. World Psychiatry 2017;16:219–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wang X, Arafa A, Liu K et al. Combined healthy lifestyle and depressive symptoms: a meta-analysis of observational studies. J Affect Disord 2021;289:144–50. [DOI] [PubMed] [Google Scholar]
- 34. Berntson J, Stewart KR, Vrany E et al. Depressive symptoms and self-reported adherence to medical recommendations to prevent cardiovascular disease: NHANES 2005–2010. Soc Sci Med 2015;138:74–81. [DOI] [PubMed] [Google Scholar]
- 35. Penninx BWJH, Milaneschi Y, Lamers F et al. Understanding the somatic consequences of depression: biological mechanisms and the role of depression symptom profile. BMC Med 2013;11:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Buckman JEJ, Saunders R, Stott J et al. Socioeconomic indicators of treatment prognosis for adults with depression. JAMA Psychiatry 2022;79:406–16. 10.1001/jamapsychiatry.2022.0100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Amiri S. Unemployment associated with major depression disorder and depressive symptoms: a systematic review and meta-analysis. Int J Occup Saf Ergon 2022;28:2080–92. 10.1080/10803548.2021.1954793 [DOI] [PubMed] [Google Scholar]
- 38. Jefferis BJ, Nazareth I, Marston L et al. Associations between unemployment and major depressive disorder: evidence from an international, prospective study (the predict cohort). Soc Sci Med 2011;73:1627–34. 10.1016/j.socscimed.2011.09.029 [DOI] [PubMed] [Google Scholar]
- 39. Musliner KL, Munk-Olsen T, Eaton WW et al. Heterogeneity in long-term trajectories of depressive symptoms: patterns, predictors and outcomes. J Affect Disord 2016;192:199–211. 10.1016/j.jad.2015.12.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bender AM, Jørgensen T, Helbech B et al. Socioeconomic position and participation in baseline and follow-up visits: the Inter99 study. Eur J Prev Cardiol 2014;21:899–905. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.
Key points.
Unemployment in itself was not associated with all-cause mortality.
If unemployment was accompanied with increased depressive symptoms.
Risk of death was three times higher than among employed non-depressive persons.
Screening and treating traditional CVD risk factors is not enough to reduce mortality riskassociated with unemployment.
More attention should be paid to screen and treat depressive symptoms of unemployed individuals.