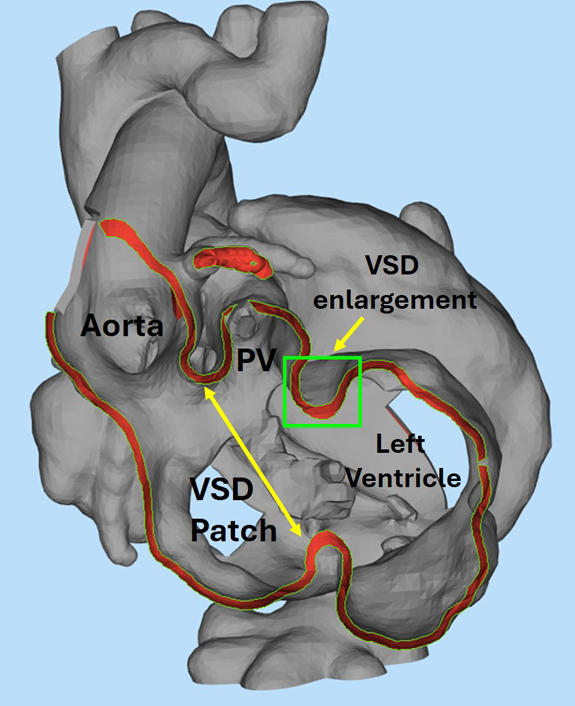
3D model showing aorta, pulmonary valve, VSD baffle pathway, and VSD enlargement area.
Central Message.
Consider staged biventricular repair in older patients with complex canal defects, particularly those with failing Glenn or Fontan physiology.
Heterotaxy syndrome with associated congenital defects such as double-outlet right ventricle (DORV), complete atrioventricular canal (CAVC), and transposition of the great arteries (TGA) presents significant surgical challenges. Traditional management often involves single-ventricle palliation, but advances in surgical techniques have made complex biventricular repair a viable option.1 This Case Report describes the technical aspects of staged biventricular repair in a patient initially deemed unsuitable for such an intervention. Written informed consent was obtained from the patient's parent to publish this case report; institutional review board approval was not required.
Clinical Summary
Patient Information
The patient was a 5-year-old boy with a diagnosis of heterotaxy syndrome, DORV, mildly unbalanced right-dominant CAVC defect, and TGA. Venous anatomy included a right superior vena cava and left-sided inferior vena cava. The patient was not considered a candidate for biventricular repair as an infant, given the complex DORV/CAVC/TGA anatomy with the aorta far remote from the left ventricle (LV). Initial palliations included pulmonary artery (PA) banding and bidirectional Glenn shunt. By age 4 years, the patient exhibited moderate-severe atrioventricular (AV) valve regurgitation and was not considered a candidate for Fontan palliation. Instead, staged biventricular repair was pursued.
First Operation
The first operation aimed to determine whether the common AV valve could be septated into 2 well-functioning valves capable of supporting a 2-ventricle repair. The zone of coaptation between the anterior and superior bridging leaflets was approximated, yielding 2 adequately sized AV valves with improved regurgitation (Video 1). The atrium was septated using a primum atrial septal defect patch that was swung inferiorly to exclude the left-sided inferior vena cava, effectively completing half of the biventricular repair. Cardiopulmonary bypass time was 109 minutes, and crossclamp time was 69 minutes. The patient was discharged on postoperative day 7.
Second Operation
Nine months later, 3-dimensional heart models were created for surgical planning (Figure 1). Despite 5 years of banding, the pulmonary valve was adequate size with good mobility, and it was closest in proximity to the inlet ventricular septal defect (VSD). The baffle pathway was planned, and a VSD enlargement site was identified on the superior outlet septum.
Figure 1.
Three-dimensional model of baseline anatomy highlighting aorta, pulmonary valve (PV), proposed VSD baffle pathway, and target area for VSD enlargement. VSD, Ventricular septal defect.
During the operation, the aortic and pulmonic roots were transected to inspect the pulmonary valve, confirming its suitability. The VSD was visualized through the tricuspid valve and right ventriculotomy, and the VSD enlargement was performed. A comma-shaped Dacron patch was fashioned for the LV to neo-aorta baffle. The tricuspid valve was taken down from the primum atrial septal defect patch, obstructing secondary cords were resected, and the inferior portion of the VSD was closed. The superior portion of the baffle was then completed, terminating at the junction with the superior bridging leaflet, and the tricuspid valve was resuspended to the top of the VSD patch.
After completing the baffle, we proceeded with coronary transfer, LeCompte, and aortic reconstruction. PA reconstruction was completed, preserving the Glenn connection to simplify the operation and off-load the right ventricle (RV) if the DORV baffle impinged on tricuspid valve flow. The LeCompte was revised with a T-patch to augment the supravalvar region and both branch PAs as the result of posterior compression from the aorta. Cardiopulmonary bypass time was 382 minutes, and crossclamp time was 210 minutes.
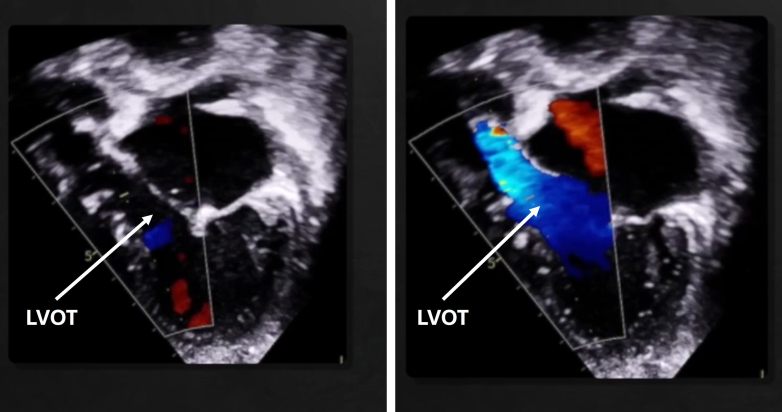
Postoperatively, the patient had excellent ventricular function, mild mitral and tricuspid regurgitation without stenosis, a widely patent LV to neo-aorta baffle (Figure 2), and excellent semi-lunar valve function. The patient was discharged on postoperative 7.
Figure 2.
Color compare echocardiogram showing unobstructed left ventricular outflow tract (LVOT).
Discussion
The DORV/CAVC repair with arterial switch is an exceptionally rare procedure, with few documented cases and technical reports.2, 3, 4 This case demonstrates the feasibility and importance of considering complex biventricular repair in patients with heterotaxy and complex cardiac anatomy. We prefer the staged approach to complex canal repair in order to limit perfusion time, allow greater attention to technical detail at each stage, and improve postoperative convalescence. However, others may elect to perform a single-stage repair in similar patients with 2 adequately sized ventricles who do not require a period of ventricular recruitment. In addition, alternative approaches could have included Rastelli, Yasui, or Nikaidoh operations with use of an RV-PA conduit. Notably, we successfully used the pulmonary valve as the systemic semilunar valve despite it being banded for 5 years, allowing for complete repair without the need for an RV-PA conduit. This highlights the importance of preserving pulmonary valve leaflets during PA banding in single-ventricle patients if there is any consideration for future biventricular repair.
Conclusions
This case highlights the potential for complex biventricular repair in older patients with AV canal defects and complex cardiac anatomy, especially those with failing Glenn or Fontan physiology.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Supplementary Data
Technical video of the biventricular repair. Video available at: https://www.jtcvs.org/article/S2666-2507(24)00362-6/fulltext.
References
- 1.Andersen N.D., Overbey D.M., Prabhu N.K., et al. Staged repair of borderline hypoplastic heart disease with early biventricular conversion. J Thoracic Cardiovasc Surg Tech. 2024;24:150–163. doi: 10.1016/j.xjtc.2024.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Imamura M., Drummond-Webb J.J., Sarris G.E., Murphy D.J., Jr., Mee R.B. Double-outlet right ventricle with complete atrioventricular canal. Ann Thorac Surg. 1998;66(3):942–944. doi: 10.1016/s0003-4975(98)00625-0. [DOI] [PubMed] [Google Scholar]
- 3.Hongu H., Nomura K., Hamaya I., et al. A case of successful biventricular repair of the transposition of the great arteries with a coronary anomaly associated with an atrioventricular septal defect. Pediatr Cardiol. 2023 doi: 10.1007/s00246-023-03276-w. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sakamoto K., Galletti L., Touchot A., Piot J.D., Bruniaux J., Planche C. Two-stage correction of transposition of great arteries with complete atrioventricular canal. Ann Thorac Surg. 1998;65(1):250–252. doi: 10.1016/s0003-4975(97)01262-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technical video of the biventricular repair. Video available at: https://www.jtcvs.org/article/S2666-2507(24)00362-6/fulltext.