Previously unroofed anomalous right coronary artery translocated onto a pulmonary autograft.
Central Message.
We present a case of aortic insufficiency after anomalous right coronary artery unroofing, pulmonary arteriopexy, and multi-redo aortic valve repair successfully treated with a Ross procedure.
Anomalous aortic origin of a coronary artery (AAOCA) is a congenital anomaly associated with increased risk of sudden death that can be surgically managed with unroofing of the intramural segment.1,2 When the intramural segment is at or below the level of the commissure, this technique requires commissural detachment and resuspension, making aortic insufficiency (AI) a potential complication. Treatment of this condition also often entails extensive dissection of the aortopulmonary plane to delineate the extent of the intramural (and sometimes extramural) course of the AAOCA, as well as pulmonary arteriopexy to move the pulmonary artery (PA) away from the aortic root. These 2 maneuvers, multi-reoperative difficulties, and the additional challenge of reimplanting a long unroofed right coronary artery may complicate pulmonary autograft dissection, harvest, and proper implantation—and even relatively contraindicate a Ross procedure, an otherwise excellent option for aortic valve (AV) replacement in a young patient. Here we present a case of recurrent AI after an anomalous right coronary artery (ARCA) unroofing and then redo AV repair successfully treated with third-time redo sternotomy and the Ross procedure.
Case Presentation
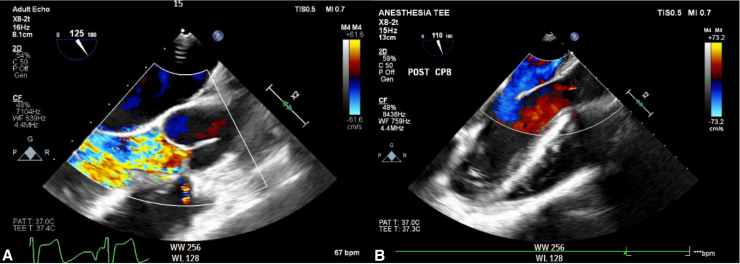
The patient is a 17-year-old male who was diagnosed at age 12 years with an ARCA originating from the left coronary sinus after presenting with chest pain. In 2018, he underwent unroofing with takedown and resuspension of the left–right commissure and pulmonary arteriopexy. He had immediate post-bypass AI, for which he underwent AV re-repair. In 2019, he developed progressive AI, for which he underwent redo sternotomy and AV re-repair. He was followed with slowly progressive recurrent AI until 2024, when he presented with severe recurrent AI, left ventricular (LV) dilatation, and low-normal systolic function on echocardiography (Figure 1, A, Video 1).
Figure 1.
A, Pre-cardiopulmonary bypass (CPB) transesophageal echocardiography (TEE) demonstrating severe, eccentric aortic insufficiency. B, Post-CPB TEE status post- Ross procedure demonstrating the pulmonary autograft with trivial residual regurgitation.
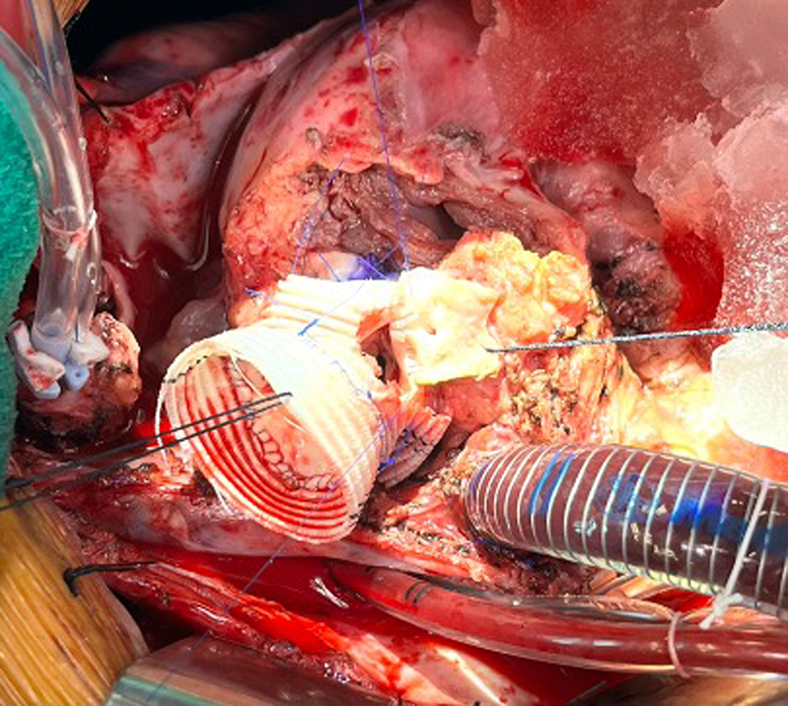
Given 2 prior unsuccessful AV repair attempts, the patient and parents specifically declined another AV repair operation. The patient was offered a possible Ross procedure. On sternal reentry, the repositioned PA was carefully dissected from the sternum, and the aorta and right atrium were cannulated for cardiopulmonary bypass (CPB). The PA was then dissected off the aorta. This area was densely adherent, given the 2 prior aortotomies and dissection for identification of the intramural ARCA. CPB was initiated to further facilitate dissection between the aortic root and the pulmonic root. The heart was then arrested with del Nido cardioplegia, and the dissection of the medial aspect of the pulmonary autograft was completed. The PA was opened just above the commissures, and the pulmonic valve was inspected to ensure cusp suitability for use as an autograft.
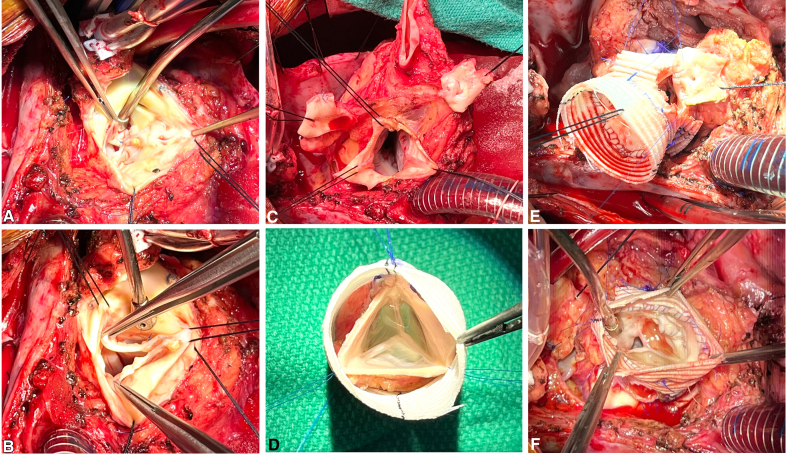
The AV was then inspected, noting pledgeted sutures at the left–right commissure from the prior repair and the tunnel of the unroofed ARCA (Figure 2, A). There was detachment of both the left and right cusps off the left–right commissure and significant fibrosis and thickening of the cusps in this region, making valve repair infeasible (Figure 2, B). The valve leaflets were excised, the left coronary button was mobilized, and the right tunnel was divided for planned translocation (Figure 2, C).
Figure 2.
Intraoperative photos of a Ross procedure performed for severe aortic insufficiency in a patient who had undergone prior unroofing of an anomalous right coronary artery (ARCA) and a prior aortic valve (AV) repair. A, Native AV, with pledgeted Prolene suture at the left–right commissure visualized from prior repair and intact tunnel of the unroofed ARCA. B, Native AV, with the left and right cusps detached from the left-right commissure and fibrotic, thickened cusps, making repair infeasible. C, The native AV leaflets have been excised, and the left and right coronary buttons have been mobilized. D, Inspection of the native pulmonic valve revealed a trileaflet valve without fenestrations, suitable for use as an autograft. Here the autograft is being prepared inside a tube graft using the modified inclusion technique. E, The proximal pulmonary autograft has been anastomosed to the aortic annulus, and the right coronary button is translocated to the proper sinus location. F, The pulmonary autograft in situ with left and right coronary buttons reimplanted.
Next, the autograft was harvested. The autograft was prepared using a modified inclusion technique (Figure 2, D).3, 4 Nonpledgeted horizontal mattress sutures were placed in the aortic annulus and then passed through the autograft composite. The left coronary button was reimplanted in orthotopic position, and the right coronary was translocated over to the proper sinus location, both using running 5-0 Prolene suture (Figure 2, E). The pulmonary homograft was brought onto the field and anastomosed to the distal PA, and the distal ascending aorta was anastomosed to the autograft, both with running 4-0 Prolene suture. The heart was deaired, the cross-clamp was removed, and the proximal anastomosis of the pulmonary homograft to the right ventricular was completed using running 3-0 Prolene suture. The heart was again deaired and weaned from CPB. Transesophageal echocardiography (TEE) demonstrated excellent autograft valve function with only trivial residual regurgitation (Figure 1, B, Video 2). The patient was taken to the intensive care unit postoperatively, where he was extubated on postoperative day (POD) 0. After an uneventful recovery, he was discharged to home on POD 5.
Discussion
AAOCA is a congenital anomaly with an estimated incidence of 0.1% to 0.3% and an associated risk of sudden cardiac death.1,2 Surgical management options include unroofing, translocation, and coronary artery bypass grafting. When the intramural segment runs at or below the level of the commissure, unroofing requires takedown and resuspension of the commissure, creating a potential risk for AI, as was the case in our patient.
In the Ross procedure, the patient's pulmonary valve is used to replace a diseased AV. Its benefits include improved survival, lack of need for anticoagulation, and low rates of valve-related complications.2,5,6 It is a longer and more technically complex operation, however. Contraindications to the Ross procedure include connective tissue disorders and pulmonary valve fenestrations.5,6 The majority of AAOCAs, including an ARCA originating from the left sinus as in our patient, do not represent a contraindication.5,6 Pawale and colleagues2 reported their Ross experience in 7 AAOCA patients and concluded that it can be safely performed, with no major postoperative complications and no ischemic symptoms, with mean follow-up of 7.8 years. Notably, these AAOCA patients represented just 1.25% of 570 Ross patients over a 27-year period, speaking to the rarity of this combination and the need to perform it at high-volume specialized centers, as other authors have suggested.2,6
Here we report a successful Ross procedure in a reoperative patient who had undergone previous unroofing with resuspension of the AV commissure followed by redo repair of the AV. Although AAOCA is not a contraindication for a Ross procedure and has been performed successfully, to our knowledge, this is the first report of a Ross performed in a patient who had previously undergone unroofing. Romp and colleagues1 reported their outcomes of 9 AAOCA unroofing patients, including 1 patient who developed severe AI treated with a Ross at 44 months after the initial operation, although they did not provide details of that operation. Although the plane fusion between the aorta and PA certainly made the dissection more challenging in our patient, we do not believe that this should be considered an absolute contraindication, and we advocate for the expansion of Ross eligibility at experienced centers.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Footnotes
The patient and his mother provided informed consent for this report. Institutional Review Board approval was not required, in accordance with institutional policy.
Supplementary Data
Pre-cardiopulmonary bypass transesophageal echocardiography demonstrating severe, eccentric aortic insufficiency. Video available at: https://www.jtcvs.org/article/S2666-2507(24)00369-9/fulltext.
Post-cardiopulmonary bypass transesophageal echocardiography status post-Ross procedure demonstrating the pulmonary autograft with trivial residual regurgitation. Video available at: https://www.jtcvs.org/article/S2666-2507(24)00369-9/fulltext.
References
- 1.Romp R.L., Herlong J.R., Landolfo C.K., et al. Outcome of unroofing procedure for repair of anomalous aortic origin of left or right coronary artery. Ann Thorac Surg. 2003;76(2):589–595. doi: 10.1016/s0003-4975(03)00436-3. [DOI] [PubMed] [Google Scholar]
- 2.Pawale A., Yanagawa B., Varghese R., Stelzer P. Ross procedure in the setting of anomalous aortic origin of a coronary artery. J Thorac Cardiovasc Surg. 2015;150(4):1000–1002. doi: 10.1016/j.jtcvs.2015.07.055. [DOI] [PubMed] [Google Scholar]
- 3.Zhu Y., Wang H., Woo Y.J. Beating heart pulmonary autograft harvest and modified inclusion technique with anti-commissural plication for the Ross procedure. JTCVS Tech. 2023;17:52–55. doi: 10.1016/j.xjtc.2022.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Starnes VA, Bowdish ME, Cohen RG, Baker CJ, Elsayed RS. The Ross procedure utilizing the pulmonary autograft inclusion technique in adults. JTCVS Tech. 2021;10:372–376. doi: 10.1016/j.xjtc.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chauvette V., Lefebvre L., Chamberland M.È., Williams E.E., El-Hamamsy I. Contemporary review of the Ross procedure. Struct Heart. 2021;5(1):11–23. doi: 10.1080/24748706.2020.1838016. [DOI] [Google Scholar]
- 6.El-Hamamsy I., Laurin C., Williams E.E. The Ross procedure in adolescence and beyond: are there still contraindications? Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2023;26:50–55. doi: 10.1053/j.pcsu.2022.12.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Pre-cardiopulmonary bypass transesophageal echocardiography demonstrating severe, eccentric aortic insufficiency. Video available at: https://www.jtcvs.org/article/S2666-2507(24)00369-9/fulltext.
Post-cardiopulmonary bypass transesophageal echocardiography status post-Ross procedure demonstrating the pulmonary autograft with trivial residual regurgitation. Video available at: https://www.jtcvs.org/article/S2666-2507(24)00369-9/fulltext.