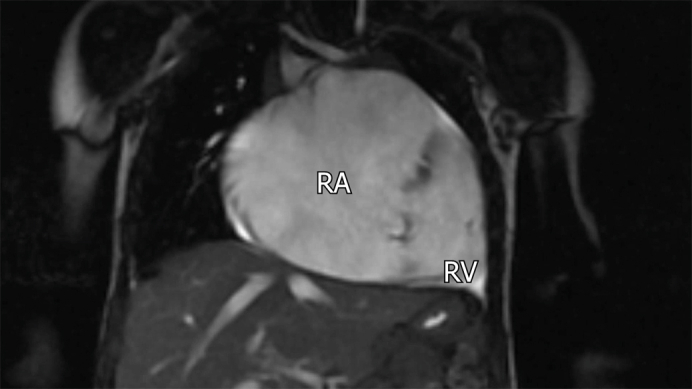
Preoperative cardiac magnetic resonance imaging showing the giant right atrium.
Central Message.
A large right atrium and tricuspid insufficiency on prenatal imaging should be closely followed to ensure an accurate diagnosis. Although rare, variations of Ebstein anomaly may be encountered.
Ebstein anomaly (EA) typically involves rotational displacement of the septal and inferior tricuspid leaflets and variable degrees of anterior leaflet tethering. Anterior leaflet displacement is rare. We report the case of a 17-month-old female who was referred for surgical treatment of moderate tricuspid valve (TV) insufficiency, severe right atrial (RA) enlargement, and atrial septal defect (ASD). We intraoperatively confirmed the presence of an EA variant with apical displacement of the anterior and inferior leaflets. This report and associated video describe a successful alternative approach to managing an anterior leaflet variation of EA.
Clinical Summary
Indication for Surgery
At the time of referral, this 17-month-old female presented with decreased exercise capacity compared with children of the same age and mild oxygen desaturation when crying. Preadmission echocardiography had indicated TV insufficiency, RA enlargement, and secundum ASD.
Subsequent echocardiography showed a dysplastic TV with moderate insufficiency, decreased mobility of the anterior leaflet, moderate ASD with left-to-right shunting, mild to moderately dilated right ventricle, and a giant right atrium. Echocardiography and magnetic resonance imaging findings raised a suspicion of downward displacement of the anterior tricuspid leaflet inside the right ventricle (Video 1). The patient's parents provided signed consent for medical data publication, and the Institutional Review Board at the University of Pittsburgh approved this study (20080084; approved June 1, 2022).
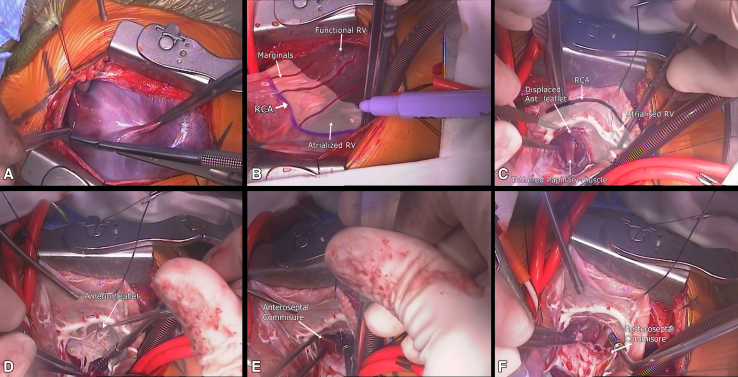
Operative Findings
Through a midline sternotomy, the giant right atrium was exposed. The right coronary artery (RCA) was identified internally and externally, running proximally to the hinge point of the anterior leaflet in the dilated atrialized RV wall (Figure 1, A). There was significant apical displacement of the anterior TV leaflet and mild displacement of the inferior leaflet inside the RV, consistent with EA (Figure 1, A and B). Additionally, tricuspid annulus dilation, tethering of the inferior papillary muscle, and poor coaptation between the inferior and septal leaflets contributed to moderate TV insufficiency.
Figure 1.
A, External view of the right atrium. B, The right coronary artery (RCA) is shown in blue with its marginals. The atrialized right ventricle is in white, and to the right is the functional right ventricle. C, Internal view of the right atrium showing the location of the anterior leaflet of the tricuspid valve (TV) in relation to the RCA. There was displacement of the anterior and inferior leaflets of the TV inside the ventricle, with a fibrous band dividing the atrialized right ventricle wall in the proximal and distal portions. D, The displaced anterior leaflet of the TV is shown. E, The anteroseptal and F, posteroseptal commissures are shown. RV, Right ventricular.
Operative Technique
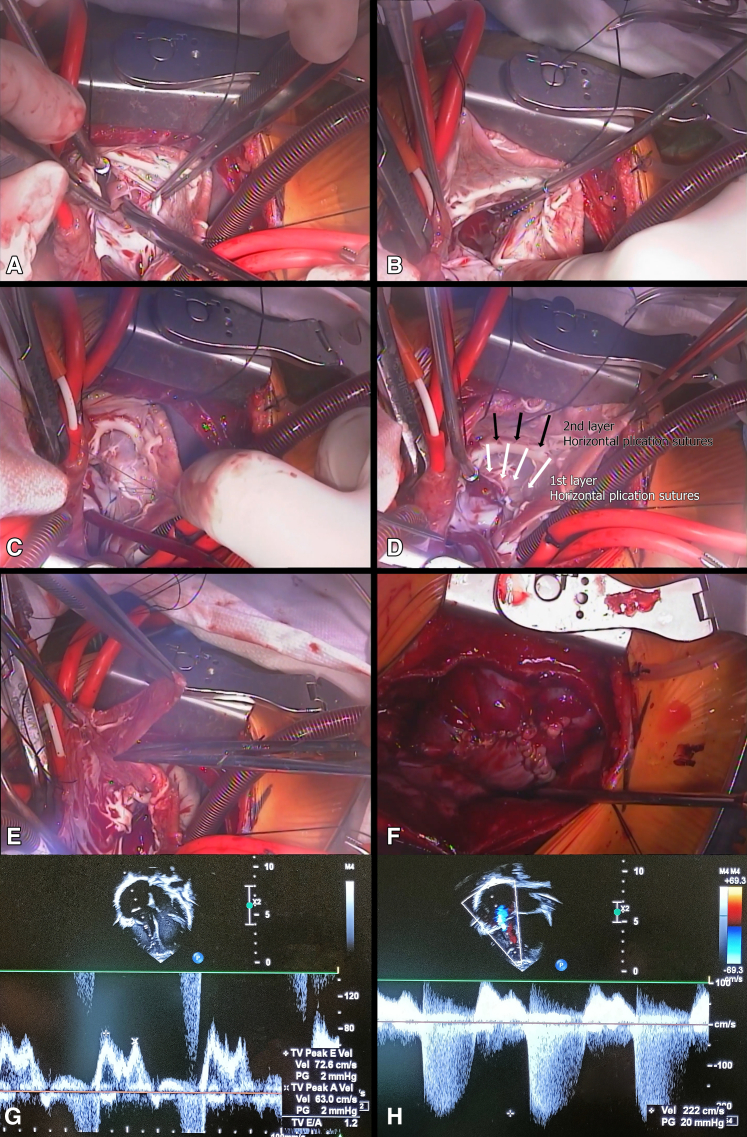
The repair was performed under cardiopulmonary bypass, bicaval and aortic cannulation, cardioplegia, and moderate hypothermia. The anterior and inferior leaflet movement was improved by freeing the papillary muscle and cutting its abnormal tethering to the RV wall (Figure 2, A). The anteroseptal and posteroseptal commissures were approximated with interrupted sutures (Figure 2, B). A reduction annuloplasty was performed with polypropylene sutures in 3 regions (Figure 2, C).
Figure 2.
A, An abnormal tethering of the papillary muscle to the right ventricular wall was released, allowing broader excursion of the leaflets. B, The anteroseptal and posteroseptal commissures were approximated with interrupted sutures. C, Polypropylene sutures in 3 different regions reduced the tricuspid valve annulus. D, Plication of the atrialized portion of the right ventricle inside the heart was done in 2 layers. Interrupted U sutures were applied in the fibrous tissue and to the displaced tricuspid annulus in the first layer. Then the right coronary artery (RCA) wass visualized in the external wall, and another layer of U suture was applied in the wall proximal to the RCA and the fibrous tissue. This technique repositioned the valvar hinge point and the RCA to the atrioventricular junction together without kinking the marginal branches of the RCA. E, Regions of the right atrial (RA) wall that were thin and dilated were trimmed. F, The RA reduction was completed with the atrial closure. G, A 2-year postoperative transthoracic echocardiogram shows mild tricuspid regurgitation with unrestricted flow (mean gradient, 2 mm Hg). H, A 2-year postoperative transthoracic echocardiogram shows a color Doppler tricuspid regurgitant gradient of 20 mm Hg.
Horizontal plication of the atrialized RV was performed using 5-0 polypropylene interrupted U sutures in 2 individualized layers, reapproximating the valvar leaflets to the atrioventricular (AV) junction (Figure 2, D). The 2-layer plication allowed the inferior and anterior leaflets to relocate to the level of the AV groove, demarcated by the location of the RCA, simultaneously preventing RCA branches from kinking.
The secundum ASD was primarily closed in a valved manner to allow right-to-left flow in the event of RV dysfunction during the postoperative period. Regions of the RA wall that were thin and dilated were resected, and the remnant atrial wall was plicated internally and externally (Figure 2, E). The RA reduction was completed, and the RA wall was closed (Figure 2, F).
The patient's postoperative course was uneventful. She was extubated in the operating room, intravenous medications were discontinued by postoperative day 1, and she was discharged from the intensive care unit on day 2. Two-week postoperative echocardiography showed trivial TV regurgitation. Two-year postoperative echocardiography showed mild tricuspid regurgitation, with unrestricted flow (mean gradient 2 mm Hg), a tricuspid regurgitant gradient of 20 mm Hg, with normal biventricular size and function (Figure 2, G and H).
Discussion
Effective treatment for EA include complex repairs that have a significant learning curve.1,2 However, the operative approach may be simplified in cases in which the anomaly consists of primary anterior displacement. Wu and colleagues3 described their experience with isolated anterior leaflet displacement in 6 patients with an approach involving detachment and reconstruction of the leaflet. In another case of isolated anterior TV displacement, Tsujii and colleagues4 reported that reduction atrioplasty was sufficient.
We describe a 2-layer plication to bring the anterior leaflet to the level of the TV annulus at the anatomic AV groove, where the RCA was located. Additionally, tricuspid annuloplasty, papillary muscle tethering release, and a reduction of the gap between the inferior and septal leaflets resulted in improved coaptation. Early echocardiographic results have shown a successful repair in this case.
This new approach is easy to perform, avoiding the detachment of the delicate leaflets from the annulus, and the double-layer horizontal plication avoids distortion of the coronary artery. This is especially critical in small children with tricuspid insufficiency.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Footnotes
Dr Ashraf is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health (Grant F32HL165847). The University of Pittsburgh holds a Physician-Scientist Institutional Award from the Burroughs Wellcome Fund (S.F.A.).
The patient's parents provided signed consent for medical data publication, and the Institutional Review Board of the University of Pittsburgh approved this study (20080084; approved June 1, 2022).
Supplementary Data
This video begins by describing the patient's presenting history and preoperative transthoracic echocardiogram and cardiac magnetic resonance imaging scan. The intraoperative section shows the cardiac anatomy encountered, particularly the tricuspid valve leaflets in relation to the right coronary artery, as seen externally on the right atrium and internally. The operative repair steps are then shown, culminating with the patient's postoperative course and discharge transthoracic echocardiogram showing a successful repair. ASD, Atrial septal defect; RV, right ventricle; RA, right atrium; LV, left ventricle; PA, pulmonary artery; RCA, right coronary artery; OR, operating room; ICU, intensive care unit; POD, postoperative day. Video available at: https://www.jtcvs.org/article/S2666-2507(24)00426-7/fulltext.
References
- 1.da Silva J.P., Baumgratz J.F., da Fonseca L., et al. The cone reconstruction of the tricuspid valve in Ebstein’s anomaly. The operation: early and midterm results. J Thorac Cardiovasc Surg. 2007;133(1):215–223. doi: 10.1016/j.jtcvs.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 2.Dearani J.A., Bacha E., da Silva J.P. Cone reconstruction of the tricuspid valve for Ebstein’s anomaly: anatomic repair. Oper Tech Thorac Cardiovasc Surg. 2008;13(2):109–225. [Google Scholar]
- 3.Wu Q., Pan G., Li H., Kong X. Anatomic repair of Ebstein’s anomaly with isolated anterior leaflet downward displacement. J Thorac Cardiovasc Surg. 2014;148(4):1454–1458.e1. doi: 10.1016/j.jtcvs.2014.02.075. [DOI] [PubMed] [Google Scholar]
- 4.Tsujii N., Kurosaki K., Yasuda K., et al. Displacement of the anterior leaflet of the tricuspid valve: rare variant of Ebstein’s anomaly. Pediatr Int. 2016;58(8):775–777. doi: 10.1111/ped.12962. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video begins by describing the patient's presenting history and preoperative transthoracic echocardiogram and cardiac magnetic resonance imaging scan. The intraoperative section shows the cardiac anatomy encountered, particularly the tricuspid valve leaflets in relation to the right coronary artery, as seen externally on the right atrium and internally. The operative repair steps are then shown, culminating with the patient's postoperative course and discharge transthoracic echocardiogram showing a successful repair. ASD, Atrial septal defect; RV, right ventricle; RA, right atrium; LV, left ventricle; PA, pulmonary artery; RCA, right coronary artery; OR, operating room; ICU, intensive care unit; POD, postoperative day. Video available at: https://www.jtcvs.org/article/S2666-2507(24)00426-7/fulltext.