Abstract
Clear cell acanthoma (CCA) is an uncommon benign epidermal tumor of unknown origin and etiology. It is often solitary, and the presence of multiple CCAs in the same individual is rare. Typically, it presents as a slowly growing plaque or nodule located on the legs with a peripheral scaling collarette. Diagnosis is primarily based on clinical and histopathological findings, with dermoscopy enhancing diagnostic accuracy. The differential diagnosis includes various skin tumors and inflammatory dermatoses. The preferred treatment is surgical excision, as these lesions do not regress spontaneously. We describe a case of a large CCA on the right thigh associated with multiple small nodular lesions scattered across the legs.
Key words: giant clear cell acanthoma, multiple lesions, dermoscopy, histopathology
Introduction
Clear cell acanthoma (CCA), also known as “Degos acanthoma” or “pale acanthoma”, was first described by Degos in 1962 as a benign epidermal tumor.1 CCA usually affects people aged 50-70 years without gender predilection, and it is characterized by a marked variability of the morphological findings.2 Usually, it appears as a slowly growing plaque or nodule, sharply demarcated and slightly elevated, from 3 to 20 mm in diameter. Color of CCA can vary from pink to brown but is commonly red and shiny. At the periphery of the lesion, a wafer-like crusty scale and/or a serous exudate may be observed; the surface can be smooth. Frequently asymptomatic and solitary, it is typically located on the legs, although all parts of the body can be affected. Presence of multiple CCAs in the same individual is rare. Interestingly, there are several variants of CAA, including giant, polypoid, pigmented and eruptive.3 Even though CCA has a non-specific clinical appearance, it has a relatively specific and easy-to-recognize dermoscopic finding called “string of pearls,” referring to dotted vessels that are arranged in a linear or serpiginous pattern.4,5 The linear formations tend to coalesce into a reticular pattern, covering the whole or part of the lesion. Dermoscopy may also show pale pink background, shiny white lines, glomerular vessels, collarette of translucent scale around the periphery of the lesion, hemorrhagic areas, and orange crusts.6 Histology of CCA is very characteristic and shows marked acanthotic epidermis with clear and glycogen-containing epidermal cells with positivity for periodic-acid– Schiff. Parakeratosis, neutrophilic exocytosis with microabscesses, and dilated blood vessels in the upper dermis may be present. The phosphorylase enzyme (that is necessary for degradation of glycogen) is absent in the keratinocytes within the CCA lesion.7 Electron microscopy studies revealed glycogen granules in the cytoplasm of the keratinocytes.8 Clinical differential diagnosis of CCA includes basal cell or squamous cell carcinoma, Kaposi’s sarcoma, clear cell hidradenoma, metastasis, angioma, pyogenic granuloma, eccrine poroma, seborrheic keratosis, histiocytoma and amelanotic melanoma.9 Dermoscopic differential diagnoses include irritated seborrheic keratose, basal-cell carcinoma, Bowen′s disease, squamous-cell carcinoma, keratoacanthoma, amelanotic melanoma and nodular melanoma. Preferred treatments are traditional surgical excision, curettage, cryotherapy or carbon dioxide laser, which is particularly indicated for large and multiple lesions. Number of treatments depends on the size and number of the lesions and the technique used. There are only a few reported cases of recurrence after excision. We described a patient with multiple CCAs also presenting giant lesions.
Case Report
A 78-year-old Caucasian man presented with multiple small exophytic nodular lesions on both thighs and legs and an exophytic, sharply demarcated, asymptomatic, ulcerated, red nodule (40x35 mm) on the right thigh (Figure 1 A-C). The lesions appeared ten years before and were slowly growing in dimension and increasing in number. The patient was taking Olmesartan and Amlodipine for blood hypertension; at physical examination no gross alterations were recorded.
Dermatoscopic examination of the nodule showed dotted vessels following a linear distribution form and an overall reticular appearance (Figure 2A); all the lesions showed common findings, namely-pinky background with glomerular and punctiform vessels with a “pearl necklace” distribution (Figure 2A-F).
Clinical differential diagnoses of the larger lesion included basal cell or squamous cell carcinoma, Kaposi’s sarcoma, clear cell hidradenoma, metastasis, angioma, pyogenic granuloma, eccrine poroma, seborrheic keratosis, histiocytoma and amelanotic melanoma; dermoscopic differential diagnoses included irritated seborrheic keratose, basal-cell carcinoma, Bowen′s disease, squamous-cell carcinoma, keratoacanthoma, amelanotic melanoma and nodular melanoma.
The large lesion on the thigh was excised, and multiple shave biopsies were performed on ten other lesions. In all specimens, histology showed a marked hyperplastic irregular (partly ulcerated) epidermis with clear and glycogen-containing epidermal cells, strongly PAS-positive; in the superficial dermis, dilated vessels and a mild lymph-histiocytic infiltrate were present (Figure 3). For all biopsies, the clinical and dermoscopic diagnosis of CCA was confirmed. About dermoscopic-pathologic correlation, the ‘string of pearls’ corresponds to the capillaries oriented perpendicular within the elongated dermal papillae.
Discussion and Conclusions
In 1966, Duperrat et al. reported a giant variety of CCA (45×40x5 mm) located on the leg.10 Since then, the “giant” variant has been considered any CCA greater than 30 to 40 mm. The largest lesion was described by Grossin et al., who reported a 70 mm locally infiltrating clear cell acanthoma on the external side of the left knee in a 90-year-old man.11 There are few reports of giant CCA in literature, which have been reported especially on the leg, mostly regarded elderly patients (Supplementary Table 1).
Roytman et al. described an 83-year-old man who had for 35 years an asymptomatic lesion on the posterior lower leg. The patient suffered from mild type 2 diabetes mellitus and varicose veins of the right leg. He reported a slow growth of the lesion, especially in the last years. Physical examination revealed a 50x50x6 mm round exophytic, brown-gray lesion, with slightly papillomatous surface covered by a serous crust, without scale or red puncta. The entire lesion was removed by shave excision and the histological examination confirmed diagnosis of CCA.12
Arida et al. described a 73-year-old Caucasian man who presented from several years an asymptomatic 4 cm strawberry-like, red-purple plaque on his right ankle, with a fine collarette of scale. He denied personal or familiar history of melanoma. On dermoscopy, a red/purple-colored lesion with curved white lines and dot vessels distributed in a serpiginous pattern was described. A biopsy was performed, and histopathological examination confirmed the diagnosis of CCA. The lesion was treated with cryotherapy and curettage.13
Figure 1.
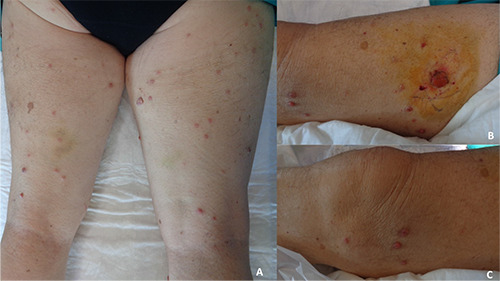
A) Multiple small nodular lesions on both thighs and legs; B) an exophytic, sharply demarcated, asymptomatic, ulcerated, red nodule (40x35 mm) on the right thigh; C) multiple small exophitic nodules on the left knee.
Figure 2.
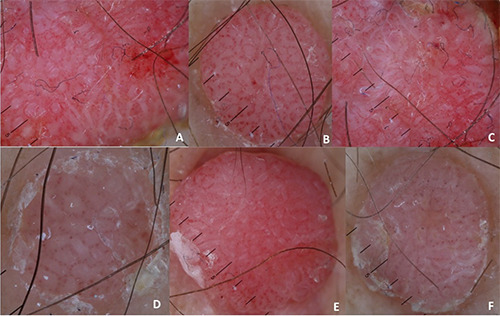
A) Dermatoscopic examination of the large nodule showed dotted vessels following a linear distribution form and an overall reticular appearance; A-F) all the lesions showed common findings, namely-pinky background with glomerular and punctiform vessels with a “string of pearl” pattern.
Figure 3.
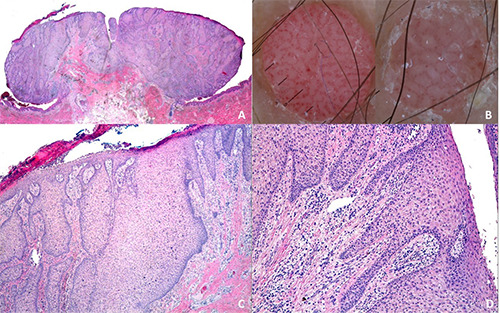
A-C-D) hyperplastic irregular epidermis with clear and glycogen-containing epidermal cells and positive PAS; dilated vessels and a mild lymph-histiocytic infiltrate in the superficial dermis. (H&E; original magnification A: 20x; B: 100x; C: 200x); B) dermoscopy of CCA showing “string of pearl” pattern.
Su et al. described an 81-year-old woman with itchy papules and nodules on both lower extremities, first appearing on the right calf about several years ago. The larger nodule was (40 mm×30 mm) red, sharply demarcated and surrounded by smaller similar lesions. Symptoms were itching and bleeding. There was no history of similar lesions among her family members. Three biopsies of lesions of both legs were performed, confirming the diagnosis of CCA. The lesion was treated with cryotherapy.14
Cavicchini et al. described a 50-year-old patient, affected by severe psoriasis since the age of 16, treated with infiximab 5 mg/Kg every 8 weeks. Five years after the beginning of this therapy, he presented on the leg a red, dome-shaped plaque of 40 mm diameter, with a peripheral collarette of thin scales. On dermoscopy vessels in a string-like pattern, peripheral white scales mixed with small blood crusts were observed. Other dermoscopic findings were hairpin vessels on the periphery surrounded by whitish haloes in a regular radial arrangement. The lesion was completely excised in the suspect of a CCA and the histological examination confirmed the diagnosis.15
Ching-Chi Chi et al. described a 6-year-old girl who presented a 50x45x3 mm firm and erythematous plaque with thin crusts on her right leg, which appeared after a trauma 1 month before. An incisional skin biopsy was performed and confirmed the diagnosis of CCA, treated with a Carbon Dioxide Laser.16
Giant CCA in different location have also been described. Langtry et al. described the lesion (40x40mm) on the buttock of an 87-year-old woman.17 Also Murphy described a lesion (60x40 x20 mm) on the buttock of 78 years old woman.18 Kim et al. described a lesion (20x32 mm) located on the perineum of a 14-year-old girl.19 These lesions presented a color from pink to red, a velvety surface, and sharply demarcated edges. In all these cases, a biopsy specimen revealed the diagnosis of CCA.
In conclusion, giant CCA represents a rare observation. Dermoscopy may help in the differential diagnoses and correct management of small lesions, but larger ones need a proper surgical approach.
Acknowledgments
informed consensus was signed by the patient for the acquisition of photographic material and publication of medical data.
Availability of data and materials
All data underlying the findings are fully available.
References
- 1.Degos R, Delort J, Civatte J, Poiares Baptista A. Epidermal tumor with an unusual appearance: clear cell acanthoma. Ann Dermatol Syphiligr (Paris) 1962;89:361–71. [PubMed] [Google Scholar]
- 2.Degos R, Civatte J. Clear-cell acanthoma. Experience of 8 years. Br J Dermatol 1970;83:248–54 [DOI] [PubMed] [Google Scholar]
- 3.Morrison LK, Duffey M, Janik M, Shamma HN. Clear cell acanthoma: Arare clinical diagnosis prior to biopsy. Int J Dermatol 2010;49:100811. [DOI] [PubMed] [Google Scholar]
- 4.Blum A, Metzler G, Bauer J, et al. The dermatoscopic pattern of clear-cell acanthoma resembles psoriasis vulgaris. Dermatology 2001;203:50–2. [DOI] [PubMed] [Google Scholar]
- 5.Tiodorovic-Zivkovic D, Lallas A, Longo C, et al. Dermoscopy of clear cell acanthoma. J Am Acad Dermatol 2015;72:S47-9. [DOI] [PubMed] [Google Scholar]
- 6.Lyons G, Chamberlain AJ, Kelly JW. Dermoscopic features of clear cell acanthoma: five new cases and a review of existing published cases. Australas J Dermatol 2015;56:206-11. [DOI] [PubMed] [Google Scholar]
- 7.Wang SH, Chi CC. Clear cell acanthoma occurring in a split-thickness skin graft. Plast Reconstr Surg 2005;116:146e-9e. [DOI] [PubMed] [Google Scholar]
- 8.Desmons F, Breuillard F, Thomas P, et al. Multiple clear-cell acanthoma (Degos): histochemical and ultrastructural study of two cases. Int J Dermatol 1977;16:203–13. [DOI] [PubMed] [Google Scholar]
- 9.Breer WA. Asymptomatic papule on the lower leg. Clearcell acanthoma. Arch Dermatol 1993;129:9–10. [DOI] [PubMed] [Google Scholar]
- 10.Duperrat B, Vanbremeersch F, David V, et al. Giant form of the acanthoma of Degos. Bull Soc r Dermatol Syphiligr 1966;73:884–6. [PubMed] [Google Scholar]
- 11.Grossin M, Mazer JM, Auffret N, et al. Formes rares de l'acan-thome h cellules cfaires. Ann Dermatol Venereol 1983;110:721-2. [PubMed] [Google Scholar]
- 12.Roytman M, Frumkin A, Everett MA. Giant clear cell acanthoma. J Am Acad Dermatol 1987;17:513–4. [DOI] [PubMed] [Google Scholar]
- 13.Arida M, English JC 3rd, Mully TW. Giant clear-cell acanthoma with keratoacanthoma-like changes: A case report. Dermatol Online J 2006;12:11. [PubMed] [Google Scholar]
- 14.Su O, Dizman D, Onsun N, et al. Multiple giant clear cell acanthomas. Indian J Dermatol Venereol Leprol 2016;82:218–21. [DOI] [PubMed] [Google Scholar]
- 15.S. Cavicchini, Nazzaro G., Marchetti S. JEADV 2015;29:1641–57. [Google Scholar]
- 16.Chi CC, Wang SH, Huang HS. Dermatol Surg 2005;31:1355-58. [DOI] [PubMed] [Google Scholar]
- 17.Langtry JA, Torras H, Palou J, et al. Giant clear cell acanthoma in an atypical location. J Am Acad Dermatol 1989;21:313–5. [DOI] [PubMed] [Google Scholar]
- 18.Murphy R, Kesseler ME, Slater DN. British Association of Dermatologists. Br J Dermatol 2000;143:1114-15. [DOI] [PubMed] [Google Scholar]
- 19.Kim DH, Kim CW, Kang SJ, Kim TY. A case of clear cell acanthoma presenting as nipple eczema. Br J Dermatol 1999;141:950–1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data underlying the findings are fully available.


