Abstract
Introduction:
Arthrofibrosis of the knee is an adverse outcome after anterior cruciate ligament (ACL) reconstruction. Definitions and classifications vary widely based on extension and flexion losses, patellar mobility, and location. In general, it is understood as a restricted range of motion (ROM) due to scar tissue, and it is often defined as symptomatic limitation in knee ROM compared to the opposite knee. The frequency of ACL injuries, and consequently arthrofibrosis, is rising among children and adolescents, with an incidence rate ranging from 2 to 14% in the pediatric population. Treatment options for arthrofibrosis include oral corticosteroids, physical therapy, casting, manipulation under anesthesia, and arthroscopic lysis of adhesions, with early recognition being a crucial intervention. To our knowledge, this is the first report in the literature to describe the development of chondromalacia after the resolution of arthrofibrosis with conservative measures in a pediatric patient.
Case Report:
A 17-year-old male developed arthrofibrosis after combined ACL reconstruction and autologous osteochondral graft transfer. Knee flexion was restored with a high-frequency, intensive physical therapy and home exercise program but at a cost of developing anterior knee and patellofemoral chondromalacia.
Conclusion:
Because complications can arise from the greater patellofemoral contact forces observed in arthrofibrosis, orthopaedic surgeons should consider early lysis of adhesions for the management of post-operative arthrofibrosis, particularly involving the parapatellar retinaculum, in adolescents who are non-responsive to conservative measures. In addition, restrictions on high levels of loading should be considered during the initial post-operative period in scenarios in which ROM has not been achieved.
Keywords: Arthrofibrosis, chondromalacia, patellofemoral arthritis, anterior cruciate ligament, arthroscopy, pediatrics
Learning Point of the Article:
A more aggressive approach to regaining range of motion, with stringent loading restrictions, should be considered when limitations in post-operative range of motion are present, especially beyond 4–6 months post-operatively.
Introduction
Arthrofibrosis of the knee is an adverse outcome after anterior cruciate ligament (ACL) reconstruction [1-7]. Definitions of arthrofibrosis vary widely in the literature, and ideal strategies for its prevention and management are unclear. Shelbourne et al. originally defined arthrofibrosis as a 15° loss of extension of the affected knee, later amending this definition to include four types based on extension and flexion losses as well as on patellar mobility and location [5]. The concept was broadly defined by Mayr et al. as restricted range of motion (ROM) due to scar tissue in at least 1 compartment of the knee [4]. Today, most clinicians agree that arthrofibrosis represents a wide spectrum of pathology and that the condition is broadly defined as a symptomatic limitation in knee ROM compared with the contralateral knee [2,5,8]. The frequency of ACL injury is increasing among children and adolescents as reconstruction procedures become more commonly performed in this cohort [9-12]. The incidence of arthrofibrosis among the pediatric population has been reported to be approximately 2–14% [1,13,14]. Whereas early recognition is likely the most important intervention, treatment for arthrofibrosis includes oral corticosteroids, physical therapy, casting, manipulation under anesthesia (MUA), and arthroscopic lysis of adhesions [6,15].
Initial use of physical therapy has successfully treated arthrofibrosis [15]; however, we have not found any study reporting complications associated with the sole use of conservative management in the pediatric population. In this report, we describe the development of patellar femoral chondromalacia in the setting of post-operative arthrofibrosis managed only with physical therapy and a home exercise program.
Case Report
The patient and his parents were informed that data concerning the case would be submitted for publication, and they provided consent. A 17-year-old male presented with right knee pain after landing on his knee during a rebound attempt while playing basketball. Magnetic resonance imaging showed an acute ACL tear with a lateral femoral condyle osteochondral fracture. Given his desire to continue with recreational sports, he underwent transphyseal ACL reconstruction and treatment of the osteochondral fracture. Initial diagnostic arthroscopy showed a parrot-beak tear of the inner 50% of the lateral meniscus midbody, a 15 × 15-mm osteochondral fracture, and an intrasubstance ACL tear. Of note, the chondral surfaces of the patella and trochlea were intact. The osteochondral loose body was not repairable and was removed in its entirety, and an osteochondral autograft/allograft transfer system (OATS) procedure was performed through a mini parapatellar incision. A partial meniscectomy was done with a shaver, and a quadrupled semitendinosus ACL reconstruction was performed using autograft tendon.
Postoperatively, passive and active knee ROM was initiated immediately. Unless rehabilitation exercise was being performed, the knee was maintained in extension with a knee brace, and crutches were used for 6 weeks of toe-touch weight-bearing. At the 4-month post-operative visit, he was noted to have lost 10° of extension and 55° of flexion compared to the contralateral knee, consistent with type 3 arthrofibrosis [5]. After thorough discussion regarding surgical lysis of adhesions, he elected to proceed with additional physical therapy and a home exercise program since he had not been consistent in working on knee flexion at home. Surgery could still be performed if ROM had not improved, and he was advised to follow up in 4 weeks.
At 14-month follow-up, the patient reported knee swelling and pain after physical activities. He did not follow up as scheduled because he noticed gradual improvement in ROM with a high-frequency, intensive, self-guided exercise program at the gym. The rehabilitation protocol consisted of seated knee extensions, seated single-leg presses, and weighted squats. Each exercise was performed until failure, which was approximately 20 repetitions with a weight of 50% his body weight of 91.8 kg, and several sets of each exercise were completed during one session. This exercise protocol was performed once daily, 5 days/week. He reported no new injuries but noted that his primary exercise to regain flexion, weighted squatting (Fig. 1), had been moderately painful to perform. Physical examination demonstrated greatly improved ROM, with full extension to 0° and a 10° loss of flexion compared to the contralateral knee. Because of ongoing knee pain and swelling after activity, possibly secondary to residual arthrofibrosis-related stiffness and chondral irregularities from treatment of osteochondritis dissecans, he underwent right knee arthroscopy, which showed a well-healed graft of the osteochondral fracture, an incorporated ACL graft, and an intact partial meniscectomy and surrounding tibial plateau articular surface. However, he was noted to have developed new 15 × 20-mm grade 2 to grade 3 lesions of the patellar and trochlear chondral surfaces (Fig. 2a-e). Chondroplasty of the patella was performed with a shaver until there was a stable base.
Figure 1.

Knee range of motion. Range of motion after a high-frequency, intensive program of weighted squats, seated knee extensions, and seated single-leg presses. 0° extension (a); 135° flexion (b).
Figure 2.
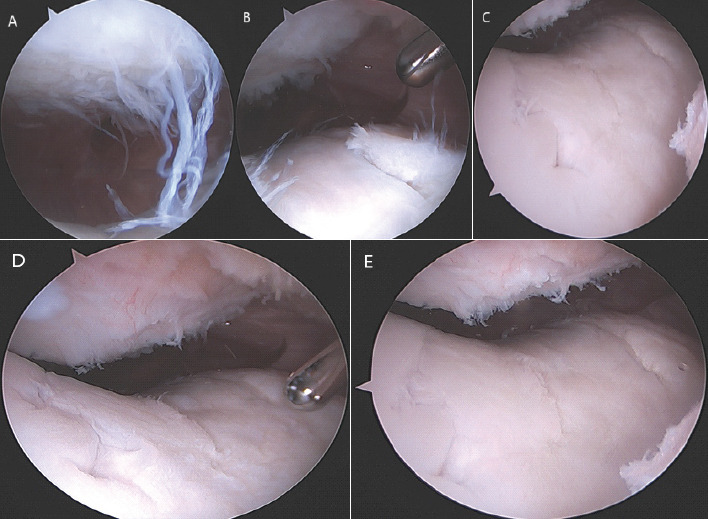
Patellar chondromalacia (A), trochlear chondromalacia (B and C), patella and trochlea (D and E).
Discussion
In a study of 933 knees in 902 children and adolescent patients, the incidence of arthrofibrosis was 8.3% (77 of 933) [1]. The risk of developing arthrofibrosis was 2 times greater for patients with than without concomitant meniscal repair and 3.5 times greater for patients aged 16 years and older than for younger patients [1]. In line with these findings, our patient was 17 years old at the time of ACL reconstruction with concomitant arthroscopic lateral meniscus repair and mini-open OATS procedure. Nwachukwu et al. hypothesized that the associations are explained by more slowly instituted post-operative rehabilitation programs for more extensive repairs [1]. Indeed, because of the osteochondral graft and because the patient began a concerted post-operative physical therapy and home exercise effort only after 4 months, after he developed ROM deficits, rehabilitation was delayed.
The average time to intervention for arthrofibrosis after ACL reconstruction ranges from 4 to 9 months [1, 16]. Although arthroscopic arthrolysis has been shown to produce the greatest improvements in flexion and extension, the impact of severity of arthrofibrosis on outcomes based on treatment modality is unclear [1, 4, 5, 15]. Furthermore, although some patients regain ROM without surgical intervention, the wide range of timelines in previous studies makes the effect of time to arthrolysis on return of ROM difficult to evaluate [15]. In a prospective study of 443 knees with ACL reconstruction, in which interventions of extension casting, MUA, and arthroscopic lysis of adhesions were applied within 30 weeks post-operatively using an algorithmic approach, Noyes et al. found that immediate knee motion and early treatment were effective [8]. In that study, 436 of 443 knees (98%) regained normal ROM, and no knee developed permanent arthrofibrosis [8]. All patients who did not respond to other treatment modalities regained full ROM after arthroscopic lysis of adhesions [8]. In support of several studies among adult populations [15], we recommend that adolescent patients who are non-responsive to conservative management, such as physical therapy, within 4 months postoperatively should be offered early surgical intervention.
We postulate that our patient’s patellar chondromalacia was due to the biomechanics of altered patellofemoral contact observed with intra-articular arthrofibrosis of the knee [17-20]. Using ten cadaveric specimens with simulated arthrofibrosis, Mikula et al. found that patellofemoral contact forces across all flexion angles were significantly increased by suprapatellar and anterior interval adhesions by a mean of 80 and 36 Newtons, respectively [19]. This alteration of patellofemoral biomechanics may lead to anterior knee pain and chondral damage to the patella and trochlea. Furthermore, joint kinematic studies have shown that patellofemoral joint stress increases with greater flexion angle of the knee [19, 21-24] and that the addition of external resistance, such as weighted squats, further increases joint stress [25,26]. Given the gradual improvement in ROM, it is likely that the patient’s high-frequency weightlifting exercise program led to degradation of the adhesions; however, the contact pressures sustained to get to that point resulted in significant patellar and trochlear chondral damage. Earlier lysis of adhesions may have decreased patellofemoral contact forces and prevented the development of patellofemoral osteoarthritis.
Conclusion
This report demonstrates the importance of both consideration of earlier intervention and adherence to an appropriate rehabilitation exercise protocol prescribed by a licensed physical therapist to prevent large contact forces and their detrimental effects.
Clinical Message.
A more aggressive, earlier approach to regain ROM should be considered for pediatric patients when limitations in post-operative ROM are present after arthroscopic ACL repair.
Biography

Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Nwachukwu BU, McFeely ED, Nasreddine A, Udall JH, Finlayson C, Shearer DW, et al. Arthrofibrosis after anterior cruciate ligament reconstruction in children and adolescents. J Pediatr Orthop. 2011;31:811–7. doi: 10.1097/BPO.0b013e31822e0291. [DOI] [PubMed] [Google Scholar]
- 2.Shelbourne KD, Patel DV. Treatment of limited motion after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1999;7:85–92. doi: 10.1007/s001670050127. [DOI] [PubMed] [Google Scholar]
- 3.Shelbourne KD, Johnson GE. Outpatient surgical management of arthrofibrosis after anterior cruciate ligament surgery. Am J Sports Med. 1994;22:192–7. doi: 10.1177/036354659402200207. [DOI] [PubMed] [Google Scholar]
- 4.Mayr HO, Weig TG, Plitz W. Arthrofibrosis following ACL reconstruction--reasons and outcome. Arch Orthop Trauma Surg. 2004;124:518–22. doi: 10.1007/s00402-004-0718-x. [DOI] [PubMed] [Google Scholar]
- 5.Shelbourne KD, Patel DV, Martini DJ. Classification and management of arthrofibrosis of the knee after anterior cruciate ligament reconstruction. Am J Sports Med. 1996;24:857–62. doi: 10.1177/036354659602400625. [DOI] [PubMed] [Google Scholar]
- 6.Magit D, Wolff A, Sutton K, Medvecky MJ. Arthrofibrosis of the knee. J Am Acad Orthop Surg. 2007;15:682–94. doi: 10.5435/00124635-200711000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19:332–6. doi: 10.1177/036354659101900402. [DOI] [PubMed] [Google Scholar]
- 8.Noyes FR, Berrios-Torres S, Barber-Westin SD, Heckmann TP. Prevention of permanent arthrofibrosis after anterior cruciate ligament reconstruction alone or combined with associated procedures:A prospective study in 443 knees. Knee Surg Sports Traumatol Arthrosc. 2000;8:196–206. doi: 10.1007/s001670000126. [DOI] [PubMed] [Google Scholar]
- 9.Fabricant PD, Kocher MS. Management of ACL injuries in children and adolescents. J Bone Joint Surg Am. 2017;99:600–12. doi: 10.2106/JBJS.16.00953. [DOI] [PubMed] [Google Scholar]
- 10.Pavlovich R, Jr, Goldberg SH, Bach BR. Adolescent ACL injury:Treatment considerations. J Knee Surg. 2004;17:79–93. doi: 10.1055/s-0030-1248203. [DOI] [PubMed] [Google Scholar]
- 11.McIntosh AL, Dahm DL, Stuart MJ. Anterior cruciate ligament reconstruction in the skeletally immature patient. Arthroscopy. 2006;22:1325–30. doi: 10.1016/j.arthro.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Schachter AK, Rokito AS. ACL injuries in the skeletally immature patient. Orthopedics. 2007;30:365–70. doi: 10.3928/01477447-20070501-01. quiz 371-2. [DOI] [PubMed] [Google Scholar]
- 13.Kocher MS, Heyworth BE, Fabricant PD, Tepolt FA, Micheli LJ. Outcomes of physeal-sparing ACL reconstruction with iliotibial band autograft in skeletally immature prepubescent children. J Bone Joint Surg Am. 2018;100:1087–94. doi: 10.2106/JBJS.17.01327. [DOI] [PubMed] [Google Scholar]
- 14.Calvo R, Figueroa D, Gili F, Vaisman A, Mocoçain P, Espinosa M, et al. Transphyseal anterior cruciate ligament reconstruction in patients with open physes:10-year follow-up study. Am J Sports Med. 2015;43:289–94. doi: 10.1177/0363546514557939. [DOI] [PubMed] [Google Scholar]
- 15.Ekhtiari S, Horner NS, De Sa D, Simunovic N, Hirschmann MT, Ogilvie R, et al. Arthrofibrosis after ACL reconstruction is best treated in a step-wise approach with early recognition and intervention:A systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25:3929–37. doi: 10.1007/s00167-017-4482-1. [DOI] [PubMed] [Google Scholar]
- 16.Sanders TL, Kremers HM, Bryan AJ, Kremers WK, Stuart MJ, Krych AJ. Procedural intervention for arthrofibrosis after ACL reconstruction:Trends over two decades. Knee Surg Sports Traumatol Arthrosc. 2017;25:532–7. doi: 10.1007/s00167-015-3799-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steadman JR, Dragoo JL, Hines SL, Briggs KK. Arthroscopic release for symptomatic scarring of the anterior interval of the knee. Am J Sports Med. 2008;36:1763–9. doi: 10.1177/0363546508320480. [DOI] [PubMed] [Google Scholar]
- 18.Murakami S, Muneta T, Ezura Y, Furuya K, Yamamoto H. Quantitative analysis of synovial fibrosis in the infrapatellar fat pad before and after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25:29–34. doi: 10.1177/036354659702500106. [DOI] [PubMed] [Google Scholar]
- 19.Mikula JD, Slette EL, Dahl KD, Montgomery SR, Dornan GJ, O'Brien L, et al. Intraarticular arthrofibrosis of the knee alters patellofemoral contact biomechanics. J Exp Orthop. 2017;4:40. doi: 10.1186/s40634-017-0110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmad CS, Kwak SD, Ateshian GA, Warden WH, Steadman JR, Mow VC. Effects of patellar tendon adhesion to the anterior tibia on knee mechanics. Am J Sports Med. 1998;26:715–24. doi: 10.1177/03635465980260051901. [DOI] [PubMed] [Google Scholar]
- 21.Ostermeier S, Holst M, Bohnsack M, Hurschler C, Stukenborg-Colsman C, Wirth CJ. Dynamic measurement of patellofemoral contact pressure following reconstruction of the medial patellofemoral ligament:An in vitro study. Clin Biomech (Bristol, Avon) 2007;22:327–35. doi: 10.1016/j.clinbiomech.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Nomura E, Inoue M, Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2005;13:510–5. doi: 10.1007/s00167-004-0607-4. [DOI] [PubMed] [Google Scholar]
- 23.Beck P, Brown NA, Greis PE, Burks RT. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:1557–63. doi: 10.1177/0363546507300872. [DOI] [PubMed] [Google Scholar]
- 24.Rood A, Hannink G, Lenting A, Groenen K, Koëter S, Verdonschot N, et al. Patellofemoral pressure changes after static and dynamic medial patellofemoral ligament reconstructions. Am J Sports Med. 2015;43:2538–44. doi: 10.1177/0363546515594447. [DOI] [PubMed] [Google Scholar]
- 25.Wallace DA, Salem GJ, Salinas R, Powers CM. Patellofemoral joint kinetics while squatting with and without an external load. J Orthop Sports Phys Ther. 2002;32:141–8. doi: 10.2519/jospt.2002.32.4.141. [DOI] [PubMed] [Google Scholar]
- 26.Zavala L, Flores V, Cotter JA, Becker J. Patellofemoral joint kinetics in females when using different depths and loads during the barbell back squat. Eur J Sport Sci. 2021;21:976–84. doi: 10.1080/17461391.2020.1806935. [DOI] [PubMed] [Google Scholar]


