Abstract
Introduction:
We experienced a rare case in which a bilateral snapping knee was caused by rheumatoid arthritis accompanied by Sjögren’s syndrome (SS), and the symptoms were resolved by arthroscopic surgery.
Case Report:
A 43-year-old Asian male presented at another hospital with finger, shoulder, and knee pain and was diagnosed with rheumatoid arthritis accompanied by SS. Two months later, he developed the snapping phenomenon in both knees and presented at our hospital. The patient was positive for rheumatoid factor, anti-Smith antibody, and anti-SS-A antibody. Arthroscopy revealed a hard scar-like tissue in the lateral patellofemoral joint in both knees. The scar-like tissue was excised arthroscopically. Post-operatively, the snapping phenomenon and pain during flexion of the bilateral knee joints had been resolved.
Conclusion:
In the present case, rheumatoid arthritis accompanied by SS caused inflammation of the knee joints and degeneration of the articular capsules, and snapping of the bilateral knees was caused by impingement of the scar tissue in the patellofemoral joints.
Keywords: Snapping knee, Rheumatoid arthritis, Sjögren’s syndrome, Arthroscopy
Learning Point of the Article:
Bilateral snapping knee caused by systemic inflammation due to rheumatic disease may require surgical intervention.
Introduction
Snapping knee is defined as the sound or feeling of snapping or popping of the knee joint during a specific activity [1, 2]. The causes of snapping knee include discoid meniscus [3], semitendinosus impingement [4], and intra-articular tumor [5]. Snapping knee secondary to rheumatoid arthritis has also been reported [6]. However, to the best of our knowledge, there have been no reports of patients with rheumatoid arthritis who developed snapping knee from causes other than rheumatoid nodules and myxomatous degeneration [6].
Most of the previous reports described unilateral snapping knee, and bilateral cases were rare [1-10]. We report a case in which a patient developed painful bilateral snapping knee secondary to rheumatoid arthritis accompanied by Sjögren’s syndrome (SS), and the symptoms were resolved by arthroscopic surgery.
Case Report
A 43-year-old Asian male presented to a local hospital with a 1-month history of finger swelling and pain, shoulder pain, and knee pain despite a lack of trauma, and several examinations for inflammatory diseases were performed. He was treated conservatively with oral analgesic, but the knee joint pain persisted. After a while, the bilateral snapping knee appeared. One month later, he was admitted to our hospital for treatment of bilateral snapping knee.
The patient had previously undergone meniscectomy on the left knee for a medial meniscus tear at 40 years of age and carpal tunnel release on both wrists at 42 years of age. He was a current smoker (20 cigarettes/day for 23 years) and had no family history of autoimmune disease.
Physical examination revealed snapping and pain in both knees upon flexion from the extended position (Supplementary Video 1). Bilateral shoulder pain as well as swelling and tenderness in the right first proximal interphalangeal joint, right fourth metacarpophalangeal joint, and left third and fourth metacarpophalangeal joints were present. The patient complained of morning stiffness. He had no obvious eye or oral dryness. The McMurray test, pivot shift test, and patella instability had negative findings. The range of motion for both knees was within the range of 0°–140°.
Laboratory data revealed that the patient had normal blood counts and renal function. Rheumatoid factor (RF) was 117 IU/mL (normal range: <15 IU/mL), matrix metalloproteinase-3 was 61.1 ng/mL (normal range: 36.9–121.0 ng/mL), erythrocyte sedimentation rate was 8 mm/h (normal range: 2–10 mm/h), C-reactive protein (CRP) was 0.3 mg/dL (normal range: <0.15 mg/dL), and anti-cyclic citrullinated peptide antibody was <0.1 U/mL (normal range: <4.5 U/mL). Anti-nuclear antibody (ANA) was 640-fold (normal range: <40-fold), and the staining pattern of ANA was speckled-type. Anti-SS-A antibody was >1200.0 U/mL (normal range: <10 U/mL), and anti-Smith (Sm) antibody was 11.2 U/mL (normal range: <10 U/mL).
Four joints had swelling and eight joints had tenderness, giving a disease activity score 28-CRP of 3.79.
On plain radiographs, the femorotibial angle was 178.6° in the right knee and 177.1° in the left knee, with no apparent pathologies (Fig. 1). Magnetic resonance images revealed synovial plica-like tissue on the lateral aspect of both patellofemoral joints (Fig. 2).
Figure 1.
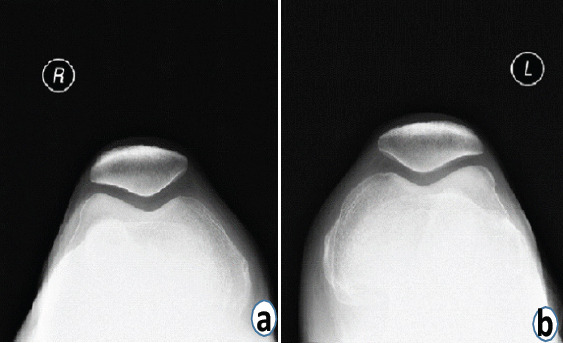
Plain radiographs of both knees. (a and b) No abnormalities were observed on the skyline views.
Figure 2.
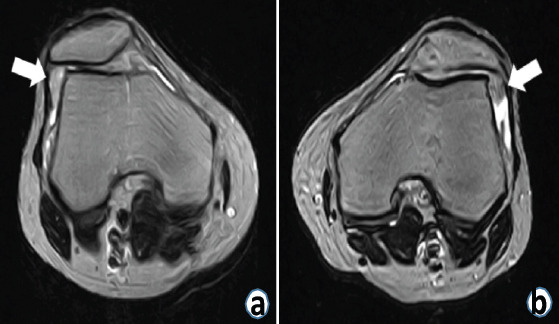
Axial T2-weighted magnetic resonance images of the knee joints. (a) Synovial plica-like tissue was observed in the lateral patellofemoral joints of the right knee (white arrow). (b) Synovial plica-like tissue was observed in the lateral patellofemoral joints of the left knee (white arrow).
At 2 months after onset of bilateral snapping knee, arthroscopy was performed for both knees. Arthroscopic probing of the tender points revealed a hard scar-like tissue in the joint capsule and impingement in the lateral patellofemoral joint in both knees (Fig. 3). The cord-like tissue was excised arthroscopically. Histopathological examination of the tissue revealed granulation tissue with inflammatory cell infiltration and vascular hyperplasia, but no tumor-like lesion with synovial proliferation was detected (Fig. 4).
Figure 3.
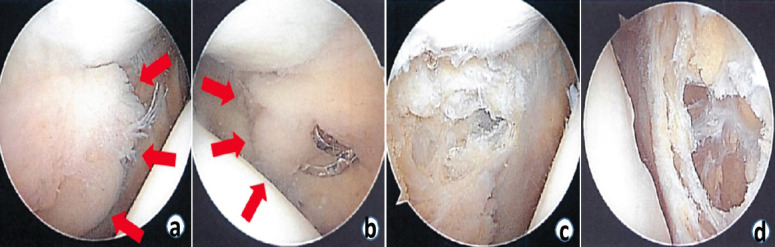
Arthroscopic image of the knee joints. (a) arthroscopic image showing hard scar-like tissue in the joint capsule of the right knee (red arrows). (b) Arthroscopic image showing hard scar-like tissue in the joint capsule of the left knee (red arrows). (c) The scar-like tissue in the right lateral patellofemoral joint was resected by arthroscopic surgery. (d) The scar-like tissue in the left lateral patellofemoral joint was resected by arthroscopic surgery.
Figure 4.
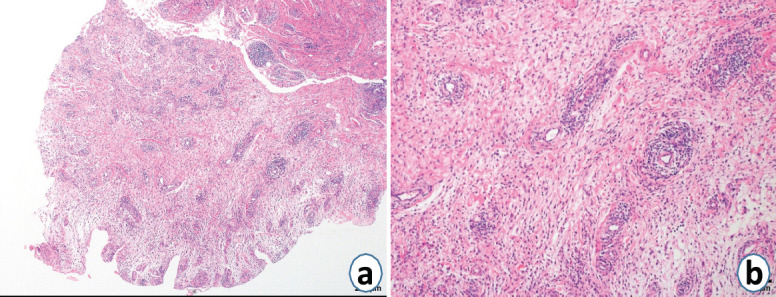
Histopathological examination of tissue collected from the left lateral patellofemoral joint. (a) Granulation tissue with inflammatory cell infiltration and vascular hyperplasia were observed, but a tumor-like lesion with synovial proliferation was not detected (hematoxylin and eosin; ×40). (b) Inflammatory cell infiltration, vascular hyperplasia, and fibrous tissue were observed, consistent with findings for granulation tissue (hematoxylin and eosin; ×100).
There were no restrictions on post-operative therapy for the patient. The snapping phenomenon and knee pain during flexion were resolved by the surgery in both knees. At 3 months post-operatively, there was no recurrence of the snapping phenomenon (Supplementary Video 2). At 4 months after surgery, pain on flexion of both knees disappeared. No recurrence of symptoms was observed at 2 years after surgery.
Discussion
The reported causes of the snapping knee include cyamella [1], synovial plica [2], discoid meniscus [3], semitendinosus impingement [4], intra-articular tumor [5, 8], lateral meniscus tear [7], and popliteus tendon [9, 10]. Most of the previous reports described unilateral snapping knee, and bilateral cases were rare [1- 10].
Torisu et al. [6] reported painful snapping caused by a solitary intra-articular nodular mass in 11 knee joints of eight patients with rheumatoid arthritis. On examination, the masses were a rheumatoid nodule in four knees and myxomatous degeneration in seven knees. In the present case, myxomatous degeneration was not observed. Rheumatoid nodules are commonly detected on the outside of joints, and exhibit fibrin deposition, necrosis, and containment by surrounding palisading macrophages [11,12]. These findings were not observed in the present case on histopathological examination.
The present case had tenderness in four small joints, high positive RF, abnormal CRP, and symptom duration exceeding 6 weeks, and rheumatoid arthritis was diagnosed in accordance with seven points in the 2010 American College of Rheumatology/the European League Against Rheumatism rheumatoid arthritis classification criteria [13].
In addition, speckled-type antinuclear antibody, anti-SS-A antibody, and anti-Sm antibody which are the characteristics of SS were positive, and SS was considered to be present [14].
We considered that rheumatoid arthritis with SS caused systemic inflammation, and degeneration and thickening of both knee joints, resulting in impingement at the patellofemoral joint during knee flexion and bilateral snapping knees. Furthermore, we considered that the arthroscopic surgery removed the degenerated and thickened joint capsule, thus preventing impingement during knee flexion, eliminating knee joint pain and preventing the snapping phenomena from recurring.
Conclusion
We experienced a case of bilateral snapping knee arising from systemic inflammation associated with rheumatoid arthritis accompanied by SS. The bilateral snapping knee phenomena were caused by impingement of the lateral patellofemoral joints, and the symptoms were resolved by arthroscopic surgery.
Clinical Message.
Patients with rheumatoid arthritis accompanied by SS may present with bilateral snapping knee due to systemic inflammation. The snapping symptoms may not improve with conservative treatment and could require surgical intervention, such as arthroscopic surgery.
Biography



Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Su S, Lu Y, Chen Y, Li Z. A symptomatic cyamella in the popliteus tendon causing snapping knee:A case report and literature review. BMC Musculoskelet Disord. 2019;20:495. doi: 10.1186/s12891-019-2882-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marchand AJ, Proisy M, Ropars M, Cohen M, Duvauferrier R, Guillin R. Snapping knee:Imaging findings with an emphasis on dynamic sonography. AJR Am J Roentgenol. 2012;199:142–50. doi: 10.2214/AJR.11.7817. [DOI] [PubMed] [Google Scholar]
- 3.Chen LX, Ao YF, Yu JK, Miao Y, Leung KK, Wang HJ, et al. Clinical features and prognosis of discoid medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2013;21:398–402. doi: 10.1007/s00167-012-1979-5. [DOI] [PubMed] [Google Scholar]
- 4.von Dercks N, Theopold JD, Marquass B, Josten C, Hepp P. Snapping knee syndrome caused by semitendinosus and semimembranosus tendons. A case report. Knee. 2016;23:1168–71. doi: 10.1016/j.knee.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Mine T, Ihara K, Taguchi T, Tanaka H, Suzuki H, Hashimoto T, et al. Snapping knee caused by intra-articular tumors. Arthroscopy. 2003;19:E21. doi: 10.1053/jars.2003.50072. [DOI] [PubMed] [Google Scholar]
- 6.Torisu T, Yosida S, Takasita M. Painful snapping in rheumatoid knees. Int Orthop. 1997;21:361–3. doi: 10.1007/s002640050185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi NH, Victoroff BN. Anterior horn tears of the lateral meniscus in soccer players. Arthroscopy. 2006;22:484–8. doi: 10.1016/j.arthro.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 8.Liu PC, Chen CH, Huang HT, Chang JK, Chen JC, Tien YC, et al. Snapping knee symptoms caused by an intra-articular ganglion cyst. Knee. 2007;14:167–8. doi: 10.1016/j.knee.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Mariani PP, Mauro CS, Margheritini F. Arthroscopic diagnosis of the snapping popliteus tendon. Arthroscopy. 2005;21:888–92. doi: 10.1016/j.arthro.2005.04.103. [DOI] [PubMed] [Google Scholar]
- 10.Krause DA, Stuart MJ. Snapping popliteus tendon in a 21-year-old female. J Orthop Sports Phys Ther. 2008;38:191–5. doi: 10.2519/jospt.2008.2698. [DOI] [PubMed] [Google Scholar]
- 11.Tilstra JS, Lienesch DW. Rheumatoid nodules. Dermatol Clin. 2015;33:361–71. doi: 10.1016/j.det.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Ziff M. The rheumatoid nodule. Arthritis Rheum. 1990;33:761–7. doi: 10.1002/art.1780330601. [DOI] [PubMed] [Google Scholar]
- 13.Kay J, Upchurch KS. ACR/EULAR 2010 rheumatoid arthritis classification criteria. Rheumatology (Oxford) 2012;51(Suppl 6):vi5–9. doi: 10.1093/rheumatology/kes279. [DOI] [PubMed] [Google Scholar]
- 14.Shiboski SC, Shiboski CH, Criswell LA, Baer AN, Challacombe S, Lanfranchi H, et al. American College of Rheumatology classification criteria for Sjögren's syndrome:A data-driven, expert consensus approach in the Sjögren's International Collaborative Clinical Alliance cohort. Arthritis Care Res (Hoboken) 2012;64:475–87. doi: 10.1002/acr.21591. [DOI] [PMC free article] [PubMed] [Google Scholar]


