Abstract
Introduction:
Primary leiomyosarcoma affecting the bone is an uncommon destructive tumor that primarily affects the elderly. If leiomyosarcoma is discovered in bone, it should be explored as a possible metastasis from a distant tumor. Surgical excision with broad margins is used as therapy.
Case Report:
A 50-year-old man reported to outpatient department with a 5-month chief complaint of a painful mass involving his left carpus that had grown. No history of trauma was present. Examination demonstrated a painful restriction of wrist motions, and ill-defined, immobile, tender hard mass measuring 5 × 3 cm along the ulnar border of the left wrist. All necessary investigations were done and were diagnosed as primary leiomyosarcoma of the distal ulna. Patient was managed surgically with resection with wide en bloc resection with a margin of at least 2 mm around the tumor and radioulnar stabilization with the help of 1 K-wire (2.5 mm). Post-operative period was uneventful.
Conclusion:
Osseous leiomyosarcoma is an uncommon tumor, it should be evaluated in the diagnosis of any solely lytic aggressive osseous lesion in a middle age, Furthermore, the existence of extraosseous main lesions should be ruled out for its diagnosis. At present, surgery is the most effective therapy option.
Keywords: Pleomorphic sarcoma, leiomyosarcoma, wide resection, ulna
Learning Point of the Article:
The key learning point from the article on primary leiomyosarcoma of the bone is the importance of considering this rare and aggressive tumor in the differential diagnosis of lytic bone lesions in middle-aged patients. Accurate diagnosis requires a combination of clinicoradiological and histopathological evaluation to distinguish it from other similar spindle cell tumors. Surgical excision with wide margins remains the most effective treatment option, and careful post-operative follow-up is essential due to the high risk of metastasis.
Introduction
Leiomyosarcoma of bone is distinguished by the presence of desmin [1] and other markers showing the presence of smooth muscle in the sarcoma but lacks osteoid formation [2]. This tumor has been shown to affect the metaphyseal area of long tubular bones, notably the lower end of femur and upper part of tibia. Radiologically other differential diagnoses includes such as aggressive lymphoma, plasma cell tumor, and dermatofibroma of bone [3]. Histologically, leiomyosarcoma can be confused with malignant dermatofibroma, fibrosarcoma, malignant sarcomatoid carcinoma, or inflammatory myofibrohistiocytic proliferation of bone [4-6]. Within 5 years, nearly 50% of leiomyosarcoma patients develop lung metastases [4]. Chemotherapy did not enhance prognosis, and radiation was not found to be useful in the treatment of leiomyosarcoma [3].
Case Report
A 50-year-old man reported to outpatient department with a 5-month chief complaint of a painful mass involving his left carpus that had grown. No history of trauma was present. Examination demonstrated a painful restriction of wrist motions, and ill-defined, immobile, tender hard mass measuring 5 × 3 cm along the ulnar border of the left wrist. Plain radiograph (Fig. 1) of forearm with wrist shows ill-defined permeative lytic lesion with thinning of the cortices involving the distal aspect of ulna.
Figure 1.
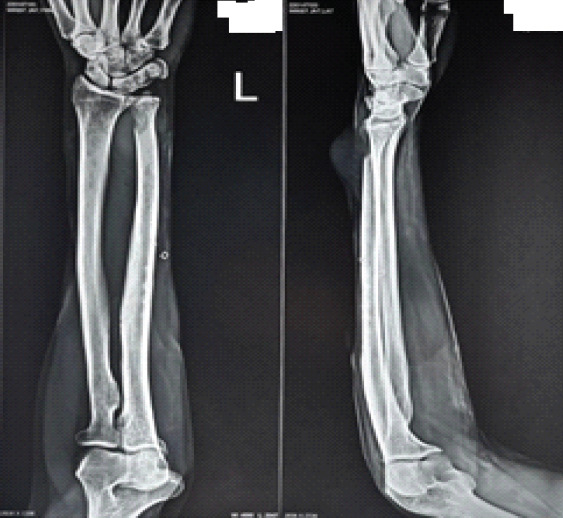
Pre-operative X-ray wrist with forearm showing ill-defined permeative lytic lesion with thinning of the cortices involving the distal aspect of ulna.
Magnetic resonance imaging (Fig. 2) suggestive of ill-defined lobulated soft-tissue lesion is seen in the dorsoulnar aspect of the distal forearm just adjacent to the carpus joint at the level of the lower end of ulna with extension of the lesion medial and lateral cortex of the distal ulna. Ulnar neurovascular bundle was closely abutted.
Figure 2.
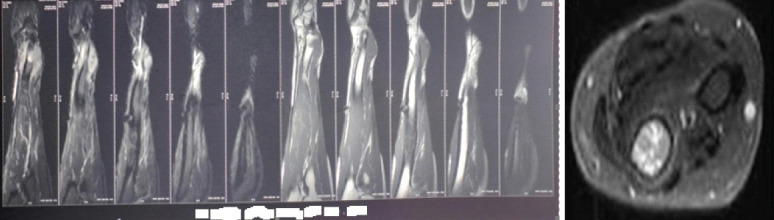
Pre-operative magnetic resonance imaging wrist with forearm showing of ill-defined lobulated soft-tissue lesion with the extension of the lesion medial and lateral cortex of the distal ulna.
Positron emission tomography-computed tomography scan suggestive of fluorodeoxyglucose avid lesion in the distal forearm and distal ulna, no other site of uptake.
Core needle biopsy and fine needle aspiration cytology are done for diagnosis suggestive of spindle cell tumor with intersecting fascicular pattern and focal prominent nuclear pleomorphism and necrosis is seen suggestive spindle cell sarcoma favor of leiomyosarcoma.
Based on clinicoradiological and histopathological examination, a diagnosis of primary leiomyosarcoma of the distal ulna was made.
Surgical resection with wide en bloc (Fig. 3) resection with a margin of at least 2 mm around the tumor and radioulnar stabilization with the help of 1 K-wire (2.5 mm) (Fig. 4) was performed and a sample was sent for histopathological examination. Postoperatively, Ifosfamide and Adriamycin were given.
Figure 3.

Intraoperative image.
Figure 4.

Post-operative X-ray.
Post-operative period was uneventful, and patient was discharged after 3 days of surgery and followed. In the 7-month period (Fig. 5) since surgery, there has been no local reoccurrence of the tumor.
Figure 5.

7 months follow-up (shows no recurrence of tumor).
Histopathological examination of the sample was done, and grossly sample was composed of part of distal ulna, tendon, and an attached globular soft-tissue tumor. Tumor measuring 5 × 5 × 3 cm, greyish white in color.
Microscopically, it shows malignant epithelioid to spindle cells with marked cytological atypia arranged in fascicles and bundles and are in storiform pattern which is consistent with leiomyosarcoma (Fig. 6).
Figure 6.
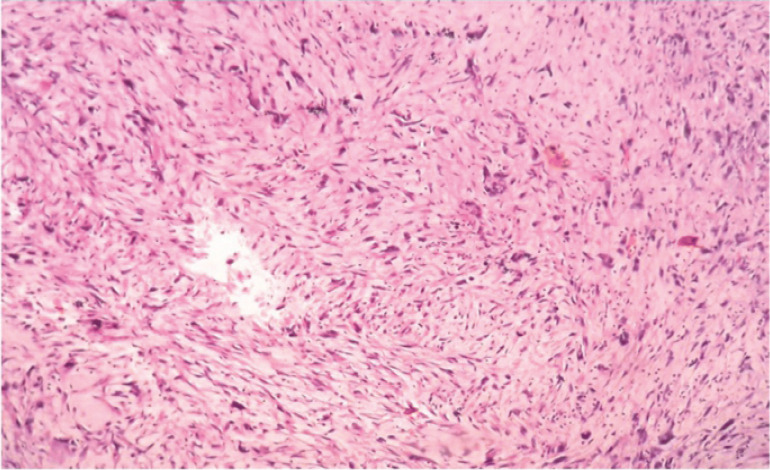
Histopathological examination shows malignant epithelioid to spindle cells with marked cytological atypia arranged in fascicles.
The differential diagnosis included: (a) Synovial sarcoma that can present with spindle cells and may be confused with leiomyosarcoma. Immunohistochemical staining for SYT-SSX fusion proteins can help differentiate it. (b) Fibrosarcoma presents with spindle cells but lacks smooth muscle differentiation markers such as smooth muscle actin (SMA) and desmin. (c) Rhabdomyosarcoma has spindle-shaped cells. However, rhabdomyosarcoma is typically positive for myogenin and MyoD1, unlike leiomyosarcoma. (d) Malignant fibrous histiocytoma/undifferentiated pleomorphic sarcoma present with pleomorphic spindle cells and might mimic leiomyosarcoma. Histological evaluation and immunohistochemistry are essential for differentiation.
Discussion
Leiomyosarcoma is a kind of aggressive tumor that develops from smooth muscle It is also one of the most uncommon primary malignant bone tumors and its etiology is unclear [7], cases with leiomyosarcoma affecting the bone typically presented with moderate pain and, in rare cases present with pathological fractures [8]. Both genders are equally impacted [2, 4]. The average age for this sarcoma is about 50 years [9, 10]. The femur and tibia are the most often implicated locations. Other unusual places have been documented, including the clavicle, ulna, radius, ribs, phalange, and pubic bone. If this tumor affects both bone and soft tissue, it is confusing to determine which one was the source which got first affected. If the mass of tumor tissue in bone is larger than in muscles or adjacent soft tissue, the tumor may be believed to have originated in the bone [2].
Leiomyosarcoma may spread to other areas, the most common site of which are the lungs, lumbar spine and liver. On X-rays, osseous leiomyosarcoma manifests as an irregular tumor border, lytic lesion, endosteal lysis, cortical erosion, and permeative pattern the tumor is mostly intramedullary; however, it can spread to the soft tissues. Typically, there is no response or a slight periosteal reaction [9]. Osseous leiomyosarcoma is indistinguishable to muscle on T1 sequence and distinguished intensity on T2 images. On traditional and rapid spin-echo sequences, the tumor can produce hypo- or isointensity in proportion to fat. Gadolinium injection often enhances the tumor’s periphery [4]. Biopsy, immunohistology (SMA, Vimentin, Desmin and low molecular weight keratin) and electron microscopy are required to diagnose a leiomyosarcoma [2, 4]. The primary treatment of osseous leiomyosarcoma is excision with clear margins [2], in our patient wide excision with at least 2−3 mm of clear margin was performed, and post-operative adjuvant chemotherapy and radiotherapy were given.
Conclusion
Osseous leiomyosarcoma is an uncommon tumor; it should be evaluated in the diagnosis of any solely lytic aggressive osseous lesion in a middle age. Furthermore, the existence of extraosseous main lesions should be ruled out for its diagnosis. At present, surgery is the most effective therapy option. A large surgical margin may be difficult to acquire in aggressive tumors in the peripheries with adjacent tissue involvement.
Clinical Message.
Primary leiomyosarcoma of the bone, though rare, should be considered in the differential diagnosis of lytic bone lesions in middle-aged patients presenting with persistent pain and a growing mass. Accurate diagnosis requires a multidisciplinary approach, including imaging, histopathology, and immunohistochemistry. Surgical excision with wide margins remains the cornerstone of treatment, with adjuvant chemotherapy playing a supportive role. Early diagnosis and appropriate management are essential to prevent metastasis and improve outcomes.
Biography




Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Gilbert NF, Cannon CP, Lin PP, Lewis VO. Soft-tissue sarcoma. J Am Acad Orthop Surg. 2009;17:40–7. doi: 10.5435/00124635-200901000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Antonescu CR, Erlandson RA, Huvos AG. Primary leiomyosarcoma of bone:A clinicopathologic, immunohistochemical, and ultrastructural study of 33 patients and a literature review. Am J Surg Pathol. 1997;21:1281–94. doi: 10.1097/00000478-199711000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Endo K, Takahashi M, Matsui Y, Hasegawa T, Yasui N. Minimally invasive taskforce of the American Association of Hip and Knee Surgeons. Bone tumor of the distal femur in a 67-year-old woman. Clin Orthop. 2005;440:262–8. doi: 10.1097/01.blo.0000180897.97203.42. [DOI] [PubMed] [Google Scholar]
- 4.Goto T, Ishida T, Motoi N, Yokokura S, Kawano H, Yamamoto A, et al. Primary leiomyosarcoma of the femur. J Orthop Sci. 2002;7:267–73. doi: 10.1007/s007760200045. [DOI] [PubMed] [Google Scholar]
- 5.Angervall L, Berlin O, Kindblom LG, Stener B. Primary leiomyosarcoma of bone:A study of five cases. Cancer. 1980;46:1270–9. doi: 10.1002/1097-0142(19800901)46:5<1270::aid-cncr2820460531>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 6.Enzinger FM, Weiss SW. Leiomyosarcoma. In: Enzinger FM, Weiss SW, editors. Soft Tissue Tumors. 3rd ed. St. Louis: Mosby; 1995. pp. 491–510. [Google Scholar]
- 7.Miura K, Hatori M, Hosaka M, Kokubun S, Watanabe M, Ehara S. Primary leiomyosarcoma with the invasion into the intertrabecular space of bone:A case report and the review of the literatures. Clin Imaging. 2001;25:209–14. doi: 10.1016/s0899-7071(01)00249-2. [DOI] [PubMed] [Google Scholar]
- 8.Berlin O, Angervall L, Kindblom LG, Berlin IC, Stener B. Primary leiomyosarcoma of bone. A clinical, radiographic, pathologic-anatomic and prognostic study of 16 cases. Skeletal Radiol. 1987;16:364–76. doi: 10.1007/BF00350962. [DOI] [PubMed] [Google Scholar]
- 9.Jundt G, Moll C, Nidecker A, Schilt R, Remagen W. Primary leiomyosarcoma of bone:Report of eight cases. Hum Pathol. 1994;25:1205–12. doi: 10.1016/0046-8177(94)90038-8. [DOI] [PubMed] [Google Scholar]
- 10.Wendum D, Sautet A, Prevot S, Martel D, Apoil A, De Saint Maur PP, et al. Primary leiomyosarcoma of bone:A clinico-pathologic and immunohistochemical study of 3 cases. Ann Pathol. 1996;16:115–9. [PubMed] [Google Scholar]


