Abstract
Introduction:
The menisci are a pair of fibrocartilaginous structures important for the normal biomechanical function of the knees. Tears are common, and multiple approaches have been used to repair meniscal tears. Of the approaches, the all-inside approach has historically been avoided for tears to the posterior aspect of the lateral meniscus (LM) due to the risk of popliteal and common peroneal neurovascular injury.
Case Report:
We reviewed the electronic medical records of all patients who underwent all-inside LM repair by our senior author from August 2022 through August 2023. Demographic, injury, and surgical data were collected to characterize surgical success and any complications attributed to the surgical approach. A literature review of MEDLINE was performed to investigate the current data regarding the all-inside approach and identify methods for improving safety and efficacy. Two cases were identified (one male and one female) who underwent all inside repair of the LM. No surgical complications were attributed to suture selection or placement, and no damage to the popliteal neurovascular structures was identified.
Conclusion:
The all-inside approach is a safe arthroscopic approach for the repair of the LM. The current literature demonstrates multiple considerations and guidelines to mitigate the risk of neurovascular injury and supports the efficacy of the all-inside approach when compared to other surgical approaches.
Keywords: Lateral meniscus, all-inside approach, peroneal nerve, popliteal artery, arthroscopy
Learning Point of the Article:
The all-inside approach is a relatively new method utilized to repair tears of the lateral meniscus. Some surgeons are concerned about the risk of damaging neurovascular structures surrounding the knee joint, but with proper considerations and planning, the all-inside approach can be safely used to manage tears throughout the lateral meniscus.
Introduction
The menisci are a pair of fibrocartilaginous structures important for the normal biomechanical function of the knees. Type I collagen is the predominant type found within the meniscus with two layers of fibers, arranged radially in the superficial layers and circumferentially arranged in the deep layers [1, 2]. The meniscus is naturally resistant to compressive forces due to the proteoglycan content of the extracellular matrix in the horns and interior free edge, areas that carry the most weight-bearing responsibility. Due to its size, the lateral meniscus (LM) is also responsible for bearing more weight than the medial meniscus in the lateral compartment [1]. The anterior horn inserts next to the insertion of the anterior cruciate ligament (ACL) on the intercondylar eminence and the posterior horn inserts posterior to the lateral tibial spine. The increased mobility of the LM is due to a region posterolaterally, near the popliteus tendon (PT), where the LM is not attached to the joint capsule [1]. The popliteus muscle separates the LM and lateral collateral ligament and functions mainly as a stabilizer of the knee [3].
The meniscus is largely avascular, with only 10–25% of the tissue receiving direct blood supply from the inferior lateral genicular arteries (ILGA) and inferior medial genicular arteries, respectively, branches of the popliteal artery (PA) [1]. The peripheral rim, anterior, and posterior horns/roots are well perfused by these arteries and a capillary plexus continuing from the synovial membrane surrounding the cruciate ligaments. There is also an extensive network of anastomoses surrounding the knee that receives further contributions from the femoral artery superiorly and the popliteal and tibial arteries inferiorly, protecting the relatively limited supply of blood to the meniscus [2-4]. The mechanical forces due to weight-bearing activities prevent this region from accessing the capillary network of the more LM tissue [4].
The menisci are innervated mainly by the posterior tibial nerve, femoral nerve, and common peroneal nerve (CPN). The recurrent peroneal branch from the CPN innervates the horns and LM. The anterior and posterior horns are highly innervated, which may be a consequence of their significant vascularization [1].
Meniscal tears are a common injury in orthopedics that is often treated with surgical intervention. While meniscectomy was a previously popular treatment, research has demonstrated significant improvement in clinical outcomes when the meniscus is repaired rather than resected [5]. Methods of repair include inside-out, outside-in, and all-inside techniques. The inside-out and outside-in approaches both utilize two incisions to pass sutures through both the meniscus and joint capsule with knots secured from outside the knee joint. Historically, the inside-out technique has been considered the gold standard, but recent advances in technology have popularized the all-inside approach among arthroscopic surgeons [6]. Unlike the former two approaches, the all-inside approach utilizes medical devices that allow for sutures or suture anchors to be placed in the meniscal tissue without the need for posterior knee incisions. The all-inside approach has been avoided by some for tears of the LM due to the potential for CPN or popliteal vasculature injury [7-12].
This case series and literature review aim to summarize the recent literature that has shown the all-inside approach to be safe and effective for repairing tears of the posterior regions of the LM [13-16]. Using PT as a sort of backstop for the popliteal hiatus can help prevent neurovascular injury when repairing this region [16-18]. Utilization of the all-inside approach for LM repairs can lead to more efficient and safer surgical outcomes with fewer incisions, fewer wound complications, and better overall success [7, 8, 10, 13-15, 19, 20].
Case Report
Patient 1 is a 43-year-old male, non-smoker, body mass index (BMI) of 26.58, who presented to the clinic in November 2022 for evaluation of lateral left knee pain and swelling, described as feeling “unstable” and occasionally locking while playing sports. Physical therapy was ordered with follow-up if symptoms persisted. In December 2022, an MRI revealed a posterior horn medial meniscus tear and an anterior horn LM tear. Surgery occurred on February 3, 2023, with initial arthroscopic exploration of the left knee revealed synovitis of the medial, lateral, and patellofemoral compartments. Further exploration of the medial compartment confirmed a posterior horn vertical tear at the red-red border, which was repaired using 2 Mitek truespan vertical mattress sutures. Exploration of the lateral compartment revealed a complete vertical tear at the body of the LM, which was repaired with 2 Mitek truespan horizontal mattress sutures (Fig. 1). The ACL was also completely torn, which was reconstructed through a semitendinosus/gracilis hamstring graft. Gentamicin was added to the arthroscopy fluid during ACL graft placement. The total time in surgery was 115 min due to the combined ACL and medial meniscus repair. The patient was prescribed oral aspirin, ibuprofen, and oxycodone-acetaminophen for analgesia and deep vein thrombosis (DVT)/pulmonary embolus (PE) prevention.
Figure 1.
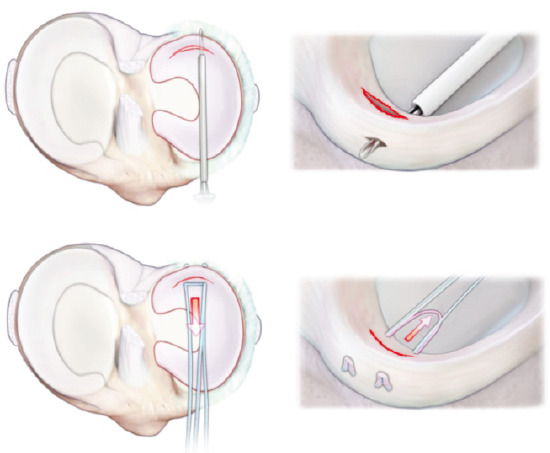
Suture placement for all inside lateral meniscus repair. The top two panels illustrate suture passing. The bottom two panels illustrate suture tensioning.
The patient underwent physical therapy and returned to the clinic post-operative week 5 demonstrating a full range of motion of the left knee. Some distal paresthesias were noted, attributed to the long leg brace, as indicated by excellent distal motor function. At this point, the patient was transitioned from a long leg brace to an ACL brace. At 7 weeks post-operative the patient returned to the clinic for signs of a suture abscess of the tibial incision. The distal aspect of the incision was opened, residual suture material was removed, and a 10-day course of doxycycline was prescribed. No other complications occurred, and the patient continued to progress positively at 5 months post-operative.
Patient 2 is a 28-year-old female, non-smoker, BMI 45.52, who presented to the clinic with persistent left knee pain 9 months after being struck by a car at low speed. MRI showed a detached anterior horn of the LM of the left knee floating above the tibial plateau by 2 mm. This area also suffered a significant tibial contusion following the initial injury. During surgical repair, synovitis was noted in the lateral and patellofemoral compartments, which were debrided before repair. Exploration of the lateral compartment revealed a tear of the anterior horn and anterior root of the LM. This was repaired using a Griffen suture anchor. No cartilage damage was noted. Patellar cartilage showed a grade 2 tear of the cartilage measuring 5 mm, which was treated with gentle chondroplasty. The incision sites were closed, with a total time in surgery of 65 min. The patient was prescribed oral aspirin, ibuprofen, and oxycodone-acetaminophen for analgesia and DVT/PE prevention. The patient was instructed to remain non-weight-bearing until instructed otherwise.
On post-operative day 10, the patient was experiencing 6/10 pain that was improving, with a passive range of motion of 0–90°. The patient was instructed to remain non-weight bearing and follow up in 4 weeks. At 5 weeks post-operative, the patient’s pain was steadily improving, and she remained non-weight bearing with the assistance of a walker. There were no signs of numbness, tingling, or weakness of the lower extremity. The patient was permitted to begin weight bearing at 6 weeks post-operative, as tolerated, and begin physical therapy. All restrictions were removed by 12 weeks post-operative, and the patient returned to work at 13 weeks.
Discussion
Due to LM tears being less common than their medial counterparts, the number of cases of LM tears localized to the posterior regions was limited in the current case series. The operating time in the cases presented was also longer than those in an isolated LM repair due to the need for additional repairs of related structures, including the medial meniscus and ACL. While post-operative complications included one case of prolonged pain and one case of a suture abscess, these results are not attributable to a neurovascular cause resulting from the all-inside repair device. The current authors have switched to using the all-inside approach for all applicable meniscal tears due to shorter operative times and excellent clinical results.
There are multiple advantages that make the all-inside approach favorable for LM repairs. First, fewer incisions make for a less invasive and quicker surgery, decreasing the risk of post-operative infection and complications [8, 10, 14, 21, 22]. Second, an inside-out or outside-in approach may require extracapsular knot tying, which effectively entraps the LM within the suture knot to the joint capsule. This greatly hinders the natural motion of the LM and can lead to negative biomechanical side effects [11, 15, 23, 24].
The all-inside approach to LM repairs can be equally effective as alternative approaches if the proper precautions are taken to avoid iatrogenic injury. The major structures to be aware of are the CPN, PA, and ILGA (Fig. 2). While the PA has been shown to lie lateral to the midline in over 90% of patients, it is only at risk of injury when operating on the far medial aspect of the dorsal horn of the LM [25]. Regardless of the tear location, the risk of neurovascular damage decreases when the knee is placed in flexion [7]. As the knee is flexed, the neurovascular structures move posteriorly away from the knee capsule, decreasing the chance of needle penetration. The distance of these structures from the knee capsule is also greater in male patients, older patients, and in the presence of joint effusion, with some mixed results regarding a correlation with weight/BMI [22, 26].
Figure 2.
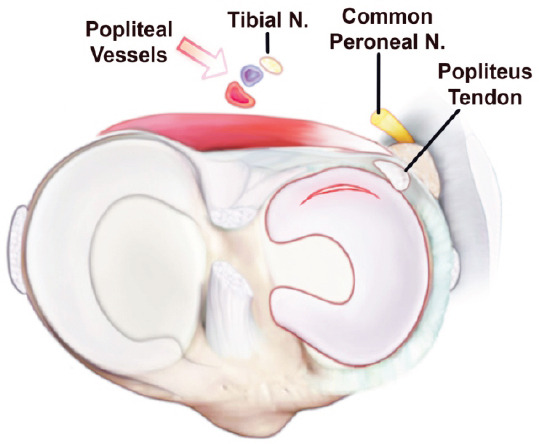
Relationship of neurovascular structures surrounding the knee joint. The figure illustrates the position of the popliteal vessels, tibial nerve, common peroneal nerve, and popliteus tendon.
Working portal choice for arthroscopic all-inside LM repair is often decided by tear location, but considerations regarding the location of the CPN and PA relative to the portal trajectory are important (Fig. 2). Most of the literature discusses anteromedial and anterolateral portals placed within 1 cm of the patellar tendon. An anterolateral portal provides easy access to the posterior root of the LM but puts the PA at greater risk of damage. The PA can lie as close as 5 mm from the meniscocapsular border when the knee is in extension, increasing the risk of needle penetration by a suture device deployed from an anterolateral portal [7, 27]. An anteromedial portal is significantly safer when repairing posterior horn tears, but tears within 3 mm of the posterior collateral ligament may be better suited for a far lateral portal due to the limitations of the portal trajectory [22, 28, 29]. An anteromedial portal also allows for better access to the lateral aspect of the LM, but operating medial to the popliteal hiatus with an anteromedial portal has a higher risk of CPN injury. Switching to an anterolateral portal for tears medial to the popliteal hiatus decreases the risk. Thus, when operating on the lateral body of the LM, an anteromedial working portal may be safer for repairs lateral to the PT, while an anterolateral portal provides less risk when operating on the lateral body medial to the PT [7, 17].
Many suture devices used today for all-inside repairs have a depth stop to limit the risk of overpenetration. Studies have shown that maintaining a ratio < 20:1 for knee circumference (mm) to needle penetration (mm) can decrease the risk of neurovascular injury in LM repairs, with ratios > 20:1 showing significantly more risk [10, 30]. Using a curved needle can reduce the risk of neurovascular injury, ideally directing the needlepoint in a lateral direction when penetrating the meniscus [30, 31].
Because the CPN is particularly at risk when operating near the popliteal tendon (PT), some researchers have attempted to define a danger zone, an area where the CPN is at particular risk of iatrogenic injury. The danger zone has been calculated to be 1.82 mm lateral and 3.13 mm medial to the PT through an anteromedial portal and 2.81 mm lateral and 1.39 mm medial to the PT through an anterolateral portal [17, 28]. Operating within these zones is inherently risky and should be avoided if possible, and when unavoidable, extreme caution should be used. This concept of the danger zone reinforces the concept that an anteromedial portal is the safer option for lateral body tears lateral to the PT, and an anterolateral portal is safer when operating near or just medial to the PT.
Conclusion
The all-inside approach is a fast, effective, and safe method for arthroscopic repair of LM tears. Equipment choice and leg position are important when planning surgery, and with proper consideration, the risk of injury to the PA and related neurovascular structures is not significant. Knowledge of these risk factors and adequate training make the all-inside approach the superior method for surgical intervention of the LM. Our facility has switched to exclusive use of this approach, with none of the associated complications reported in previous literature studying the all-inside approach.
Clinical Message.
The all-inside approach is a fast, practical, and effective approach for repairing tears of the LM, including tears localized to the posterior. With proper considerations and planning outlined in this manuscript, the all-inside approach can provide good surgical outcomes.
Acknowledgement:
Special thanks to Jenna Gunn for her work getting IRB approval for this project and Aidan Maxwell for his help in formatting the final manuscript. We could not have completed this project without their assistance.
Biography





Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Fox AJ, Bedi A, Rodeo SA. The basic science of human knee menisci:Structure, composition, and function. Sports Health. 2012;4:340–51. doi: 10.1177/1941738111429419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perelli S, Morales Avalos R, Masferrer-Pino A, Carlos Monllau J. Anatomy of lateral meniscus. Ann Jt. 2021;7:16. doi: 10.21037/aoj-20-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nyland J, Lachman N, Kocabey Y, Brosky J, Altun R, Caborn D. Anatomy, function, and rehabilitation of the popliteus musculotendinous complex. J Orthop Sports Phys Ther. 2005;35:165–79. doi: 10.2519/jospt.2005.35.3.165. [DOI] [PubMed] [Google Scholar]
- 4.Shim SS, Leung G. Blood supply of the knee joint. A microangiographic study in children and adults. Clin Orthop Relat Res. 1986;208:119–25. [PubMed] [Google Scholar]
- 5.Bottomley J, Al-Dadah O. Arthroscopic meniscectomy vs meniscal repair:Comparison of clinical outcomes. Cureus. 2023;15:e44122. doi: 10.7759/cureus.44122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears:A systematic review. Am J Sports Med. 2012;40:459–68. doi: 10.1177/0363546511411701. [DOI] [PubMed] [Google Scholar]
- 7.Cuéllar A, Cuéllar R, Cuéllar A, Garcia-Alonso I, Ruiz-Ibán MA. The effect of knee flexion angle on the neurovascular safety of all-inside lateral meniscus repair:A cadaveric study. Arthroscopy. 2015;31:2138–44. doi: 10.1016/j.arthro.2015.04.100. [DOI] [PubMed] [Google Scholar]
- 8.Fang C, Liu H, Di Z, Zhang JH. Arthroscopic all-inside repair with suture hook for horizontal tear of the lateral meniscus at the popliteal hiatus region:A preliminary report. BMC Musculoskelet Disord. 2020;21:52. doi: 10.1186/s12891-020-3066-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ouanezar H, Blakeney W, Latrobe C, Saithna A, Fernandes LR, Delaloye JR, et al. The popliteus tendon provides a safe and reliable location for all-inside meniscal repair device placement. Knee Surg Sports Traumatol Arthrosc. 2018;26:3611–9. doi: 10.1007/s00167-018-4889-3. [DOI] [PubMed] [Google Scholar]
- 10.Koiwa K, Oshiba H, Yamazaki H. Common peroneal nerve injury due to an all-inside repair of the posterior horn of lateral meniscus:A case report. JBJS Case Connect. 2023;13(1):e22.00460. doi: 10.2106/JBJS.CC.22.00460. [DOI] [PubMed] [Google Scholar]
- 11.Uchida R, Horibe S, Shiozaki Y, Shino K. All-inside suture repair for isolated radial tears at the midbody of the lateral meniscus. Arthrosc Tech. 2019;8:e1451–6. doi: 10.1016/j.eats.2019.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meng X, Zhu Y, Wang D, Dou Y, Zhang Z, Jiang D. An all-inside repair technique for unstable Type-IV lateral meniscal posterior root tear. Arthrosc Tech. 2022;11:e1317–20. doi: 10.1016/j.eats.2022.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Espejo-Baena A, Figueroa-Mata A, Serrano-Fernández J, de la Torre-Solís F. All-inside suture technique using anterior portals in posterior horn tears of lateral meniscus. Arthroscopy. 2008;24:369.e1–4. doi: 10.1016/j.arthro.2007.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Ahn J, Oh I. Arthroscopic all-inside lateral meniscus suture using posterolateral portal. Arthroscopy. 2006;22:572.e1–4. doi: 10.1016/j.arthro.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 15.Kim SJ, Jung KA, Kim JM, Kwun JD, Baek SH, Han JN. Arthroscopic all-inside repair of tears of the anterior horn of the lateral meniscus. Arthroscopy. 2005;21:1399. doi: 10.1016/j.arthro.2005.08.027. [DOI] [PubMed] [Google Scholar]
- 16.Mhaskar VA, Agrahari H, Maheshwari J. True all inside meniscus repair using the popliteus tendon. Eur J Orthop Surg Traumatol. 2023;33:2151–7. doi: 10.1007/s00590-022-03332-w. [DOI] [PubMed] [Google Scholar]
- 17.Chuaychoosakoon C, Wuttimanop W, Tangjatsakow P, Charoenrattanawat S, Parinyakhup W, Boonriong T, et al. The Danger Zone for iatrogenic neurovascular injury in all-inside lateral meniscal repair in relation to the popliteal tendon:An MRI study. Orthop J Sports Med. 2021;9(10):23259671211038397. doi: 10.1177/23259671211038397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asavanapakas P, Boonsri P, Parinyakhup W, Boonriong T, Chuaychoosakoon C. No risk of iatrogenic peroneal nerve injury in all-inside lateral meniscal repair with either 14- or 18-mm needles through the popliteus tendon in the standard arthroscopic knee conditions. Knee Surg Sports Traumatol Arthrosc. 2023;31:2331–7. doi: 10.1007/s00167-022-07297-5. [DOI] [PubMed] [Google Scholar]
- 19.Zuke WA, Cvetanovich G, Go B, Forsythe B. Arthroscopic saucerization and all-inside repair of a delaminated discoid lateral meniscus. Arthrosc Tech. 2017;6:e1387–91. doi: 10.1016/j.eats.2017.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanada T, Iwaso H, Honda E, Yoshitomi H, Inagawa M. All-inside repair for radial tear at the posterior horn of the lateral meniscus:A figure-8 suture technique. Arthroscopy Tech. 2021;10:e1973–7. doi: 10.1016/j.eats.2021.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choi NH. Meniscal repair for anterior horn tear of the lateral meniscus. Arthroscopy. 2006;22:1132.e1–2. doi: 10.1016/j.arthro.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 22.Oehler N, Foerg A, Haenle M, Blanke F, Vogt S. Assessment of popliteal neurovascular safety during all-inside suturing of the posterior horn of the lateral meniscus using Upright MRIs of the knee joint. Knee. 2021;33:234–42. doi: 10.1016/j.knee.2021.10.003. [DOI] [PubMed] [Google Scholar]
- 23.Malinowski K, Ebisz M, Góralczyk A, LaPrade RF, Hermanowicz K. You can repair more tears than you think-tricks for all-inside lateral meniscal repair with nonabsorbable sutures. Arthrosc Tech. 2020;9:e979–86. doi: 10.1016/j.eats.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Soejima T, Tabuchi K, Noguchi K, Inoue T, Katouda M, Murakami H, et al. An all-inside repair for full radial posterior lateral meniscus tears. Arthrosc Tech. 2016;5:e133–8. doi: 10.1016/j.eats.2015.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanz-Pérez M, García-Germán D, Ruiz-Díaz J, Navas-Pernía I, Campo-Loarte J. Location of the popliteal artery and its relationship with the vascular risk in the suture of the posterior horn of the lateral meniscus. Rev Esp Cir Ortop Traumatol. 2015;59:165–71. doi: 10.1016/j.recot.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Beck J, Shifflett K, Greig D, Ebramzadeh E, Bowen RE. Defining a safe zone for all-inside lateral meniscal repairs in pediatric patients:A magnetic resonance imaging study. Arthroscopy. 2019;35:166–70. doi: 10.1016/j.arthro.2018.07.046. [DOI] [PubMed] [Google Scholar]
- 27.Schachne JM, Heath MR, Yen YM, Shea KG, Green DW, Peter D, et al. The safe distance to the popliteal neurovascular bundle in pediatric knee arthroscopic surgery:An age-based magnetic resonance imaging anatomic study. Orthop J Sports Med. 2019;7(7):2325967119855027. doi: 10.1177/2325967119855027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chuaychoosakoon C, Boonsri P, Tanutit P, Laohawiriyakamol T, Boonriong T, Parinyakhup W. The risk of iatrogenic peroneal nerve injury in lateral meniscal repair and safe zone to minimize the risk based on actual arthroscopic position:An MRI study. Am J Sports Med. 2022;50:1858–66. doi: 10.1177/03635465221093075. [DOI] [PubMed] [Google Scholar]
- 29.Mao DW, Upadhyay U, Thalanki S, Lee DY. All-inside lateral meniscal repair via anterolateral portal increases risk of vascular injury:A cadaveric study. Arthroscopy. 2020;36:225–32. doi: 10.1016/j.arthro.2019.07.023. [DOI] [PubMed] [Google Scholar]
- 30.Abouheif MM, Shibuya H, Niimoto T, Kongcharoensombat W, Deie M, Adachi N, et al. Determination of the safe penetration depth during all-inside meniscal repair of the posterior part of the lateral meniscus using the FasT-Fix suture repair system. Knee Surg Sports Traumatol Arthrosc. 2011;19:1868–75. doi: 10.1007/s00167-011-1489-x. [DOI] [PubMed] [Google Scholar]
- 31.Nishimura A, Fukuda A, Kato K, Fujisawa K, Uchida A, Sudo A. Vascular safety during arthroscopic all-inside meniscus suture. Knee Surg Sports Traumatol Arthrosc. 2015;23:975–80. doi: 10.1007/s00167-013-2774-7. [DOI] [PubMed] [Google Scholar]


