Abstract
Background
Baseline right bundle branch block (RBBB) is an established predictor of permanent pacemaker (PPM) requirement after transcatheter aortic valve replacement (TAVR). There are limited data to support prophylactic PPM implantation in advance of TAVR. We aimed to evaluate the efficacy and safety of prophylactic PPM implantation in patients with RBBB prior to TAVR, and to identify the predictors of pacing dependence after TAVR.
Methods
This was a retrospective cohort study of patients undergoing prophylactic PPM implantation for baseline RBBB prior to TAVR at two high-volume UK centers between 2014 and 2022.
Results
Baseline RBBB was identified in 170/4580 (3.7%) patients undergoing TAVR during the study period. Of these, 106/170 (62.4%) underwent prophylactic PPM implantation. This group had a significantly shorter median length of hospital stay after TAVR compared to patients with RBBB undergoing TAVR without prophylactic PPM implantation (2 vs. 4 days, p = 0.028). Urgent PPM implantation after TAVR was required in 43/64 (67.2%) of patients with RBBB who underwent TAVR without a prophylactic PPM. Analysis of ventricular pacing over 12 months post-TAVR demonstrated a significant pacing requirement (ventricular pacing > 10%) in 50/79 (63%) of patients with a prophylactic PPM. Pacing requirement was independently predicted by baseline first-degree heart block (odds ratio 2.4, p = 0.03) and QRS duration >140 ms (odds ratio 4.3, p = 0.01).
Conclusions
In this retrospective two-center cohort study, prophylactic PPM implantation for patients with baseline RBBB was safe, effective, and reduced the length of hospital stay. First-degree atrioventricular block and broad RBBB (QRS > 140 ms) were independent baseline predictors of significant pacing requirements.
Keywords: Permanent pacemaker, Right bundle branch block, TAVR
Introduction
Injury to the cardiac conduction system resulting in high-grade atrioventricular block (HAVB) is a common complication of transcatheter aortic valve replacement (TAVR).1 In contemporary series, up to 15% of patients undergoing TAVR require implantation of a permanent pacemaker (PPM) prior to discharge.2 New-onset conduction disturbance with the requirement for urgent PPM is associated with immobility and prolonged hospitalization.3 Furthermore, late-onset HAVB within 30 days after TAVR has been reported in up to 5% of patients, and it may lead to urgent readmission or sudden cardiac death.4
Baseline right bundle branch block (RBBB) is associated with increased late mortality after TAVR, and it is an established predictor of HAVB necessitating PPM implantation after the TAVR procedure.2,5, 6, 7, 8, 9 Although some implanting centers have adopted a strategy of prophylactic PPM implantation before TAVR for patients with baseline RBBB, this is not currently recommended by European Society of Cardiology or American Society of Cardiology guidelines.2,4,10, 11, 12 In particular, there is uncertainty around whether there is a long-term requirement for pacing in this cohort, who may regain functional intrinsic conduction after they recover from TAVR.
The aims of this study were: (1) to analyze clinical efficacy and safety of prophylactic PPM implantation in TAVR patients with baseline RBBB; (2) to evaluate the 1-year longitudinal pacing requirement after TAVR in this cohort; and (3) to identify baseline predictors of ongoing pacing requirements after TAVR.
Methods
Study Population
All patients undergoing TAVR for severe symptomatic aortic stenosis in two high-volume UK centers (Oxford University Hospitals, Oxford, UK, and Leeds General Infirmary, Leeds, UK) between January 2014 and December 2022 were included in the study. TAVR registries at both centers were used to identify patients with baseline RBBB and ascertain whether prophylactic or inpatient post-TAVR pacemaker implantation was performed. The decision regarding prophylactic PPM implantation was at the discretion of the Heart Valve Team or the responsible clinician in discussion with the patient. Patients undergoing cardiac resynchronization therapy or PPM implantation before TAVR for indications other than prevention of TAVR-related HAVB were excluded from the study.
Data Collection
Baseline patient demographics, 12-lead electrocardiogram (ECG), procedural, and clinical outcomes were retrospectively extracted from TAVR registries and electronic patient records at both centers. All patients provided written informed consent for their procedures. Collection and submission of these data to the UK National Institute for Cardiovascular Outcomes Research is approved by Section 251 of the National Health Service Act of 2006. Formal ethics approval was not required for this specific study as part of a service evaluation, which was conducted in compliance with the Declaration of Helsinki. ECG analysis was based on the last available ECG before TAVR. Longitudinal pacing data were collected from patients’ pacing reports. Only patients with a pacemaker base rate set at 50 to 60 beats per minute and at least two pacing reports in the first year after TAVR (separate from the TAVR admission) were included in the analysis.
Statistical Analysis
Categorical data were summarized by means of absolute and relative frequencies (counts and percentages). Continuous variables were reported as mean ± standard deviation or median with an interquartile range. The Kolmogorov-Smirnov test was applied to check for normality. The chi square (for categorical data, with Yates’ correction when n ≤ 5) and Student’s t-test (for continuous data) were used for the analysis of demographic and clinical factors. Binary logistic regression was used to evaluate the independent predictors of pacing dependence. All data were analyzed using SPSS (version 29.0, IBM, USA).
Results
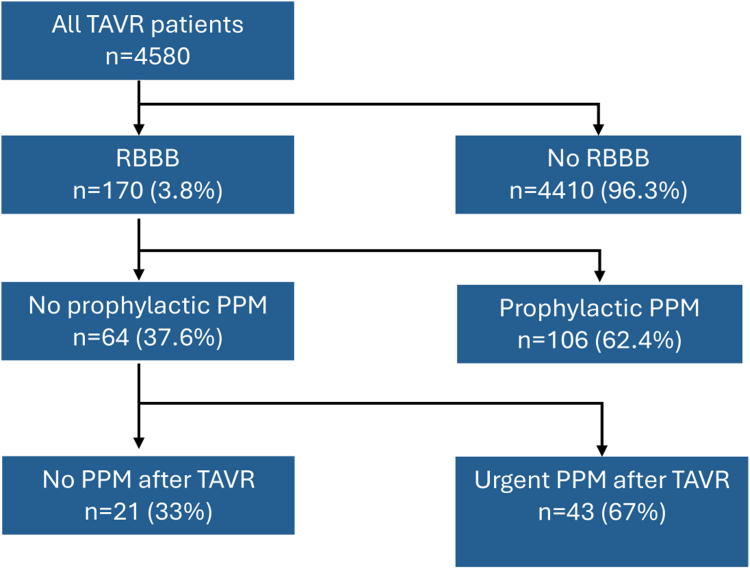
Four thousand five hundred eighty patients underwent TAVR between 2014 and 2022, of whom 170 (3.7%) had baseline RBBB (Figure 1). Of patients with baseline RBBB, 106/170 (62.4%) underwent implantation of a prophylactic PPM before TAVR. The median time period between prophylactic PPM implantation and TAVR was 42 days (95% CI 6-65 days). Patients with baseline RBBB were significantly more likely to receive a prophylactic PPM if they had first-degree heart block (34 vs. 6% of patients, p < 0.001; Supplementary Table 1). Compared with the remainder of the total TAVR cohort, patients who underwent prophylactic PPM implantation for baseline RBBB were more likely to be male (69 vs. 57%, p < 0.05), have first-degree heart block (34 vs. 6%, p < 0.001), and have impaired left ventricular function (46 vs. 32%, p < 0.05; Supplementary Table 2).
Figure 1.
Study flow chart.
Abbreviations: PPM, permanent pacemaker; RBBB, right bundle branch block; TAVR, transcatheter aortic valve replacement.
The complications associated with implantation of a prophylactic PPM prior to TAVR are shown in Table 1. The incidence of hematoma and pneumothorax was 0/106 (0%), and lead revision was required in 2/106 (1.9%) of cases. Compared to patients undergoing urgent PPM implantation after TAVR, there was no significant difference in the rate of pacing-related complications (prophylactic PPM 3/106 [7.3%] vs. 9/429 [2.1%], p = 0.713).
Table 1.
Pacing complications in patients with prophylactic PPM implantation prior to TAVR, compared to urgent PPM implantation after TAVR
| Pacing complication | Prophylactic PPM before TAVR (n = 106) | Urgent PPM after TAVR (n = 429) | p Value |
|---|---|---|---|
| Pneumothorax | 0 (0%) | 3 (0.7%)∗ | 0.635 |
| Hematoma requiring evacuation | 0 (0%) | 1 (0.2%) | 0.520 |
| Pericardial effusion | 0 (0%) | 1 (0.2%)∗ | 0.520 |
| Lead displacement | 2 (1.9%) | 3 (0.7%) | 0.869 |
| Myocardial perforation | 0 (0%) | 0 (0%) | N/A |
| Infective endocarditis | 0 (0%) | 1 (0.2%) | 0.520 |
| Phrenic stimulation | 1 (0.9%) | 0 (0%) | 0.427 |
| Total number of pacing complications | 3 (7.3%) | 9 (2.1%) | 0.194 |
Abbreviations: PPM, permanent pacemaker; TAVR, transcatheter aortic valve replacement.
All managed conservatively.
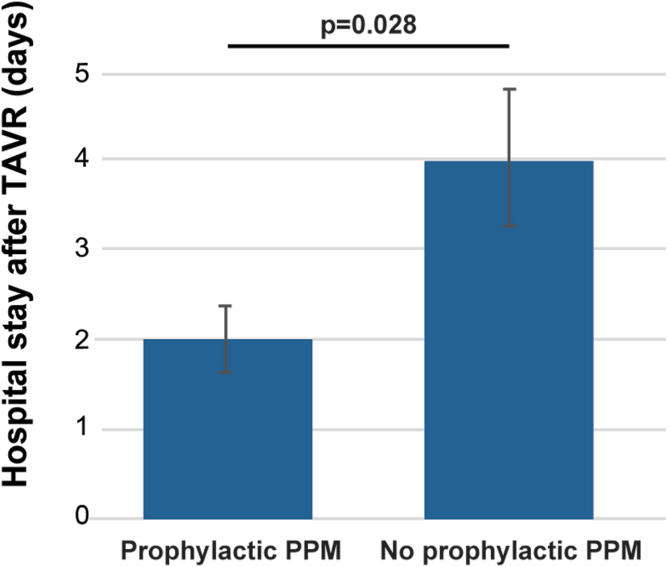
Compared to patients with RBBB who did not undergo implantation of a prophylactic PPM, the prophylactic PPM group had a significantly shorter median length of hospital stay after TAVR (2 vs. 4 days, p = 0.028; Figure 2). Furthermore, in the group of patients with RBBB but no prophylactic PPM implant, 43/64 (67%) required an unplanned PPM after TAVR. Of these, 29/43 (67%) patients required an urgent PPM on the same admission as their TAVR procedure, 8/43 (19%) patients within 30 days after TAVR (separate from the index admission), 2/43 (5%) patients between 30 days and 1 year after TAVR, and 4/43 (9%) more than 1 year after TAVR.
Figure 2.
Median length of stay after TAVR in RBBB patients undergoing prophylactic PPM implantation, compared to those without prophylactic PPM.
Abbreviations: PPM, permanent pacemaker; RBBB, right bundle branch block; TAVR, transcatheter aortic valve replacement.
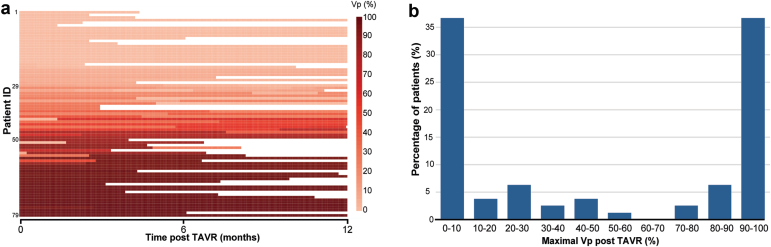
Longitudinal ventricular pacing (Vp) rate data for the first year after TAVR were available for 79/106 (75%) of these patients (Figure 3). The mean number of pacing checks in the first year after TAVR was 2.7, with a mean time to the first, second, and third pacing checks of 2.1, 4.6, and 8.9 months, respectively. High pacing requirement was defined as a Vp rate of >10% at any pacing check after discharge following the TAVR admission.13 Vp > 10% during pacing follow-up was identified in 42/79 (53%) of patients. The histogram of maximal Vp requirement at any pacing check in the first 12 months after TAVR is shown in Figure 3. Of patients, 23/79 (29%) demonstrated no pacing requirement (Vp < 1%). An absolute change in Vp of more than 10% over the 1 year study period was detected in 11 (14%) patients. All of these patients had a high initial pacing requirement (Vp > 70%), and in none of these patients did the Vp requirement fall under 10% at any point during the study. Conversely, 2 patients with a low initial pacing requirement (Vp < 10%) developed a high requirement (Vp > 10%), but their absolute change in Vp during the study was less than 5%.
Figure 3.
Longitudinal pacing requirements of patients with baseline RBBB who received a prophylactic PPM before TAVR. (a) Heat map of longitudinal ventricular pacing (Vp) requirements over time. The Vp values for each patient are based on at least two electrophysiological device reports in the first year after TAVR that were separate from the TAVR admission. Darker red colors correspond to higher Vp requirements. (b) Distribution of maximal Vp dependence in the first year after TAVR.
Abbreviations: Patient ID, patient identification; PPM, permanent pacemaker; RBBB, right bundle branch block; TAVR, transcatheter aortic valve replacement.
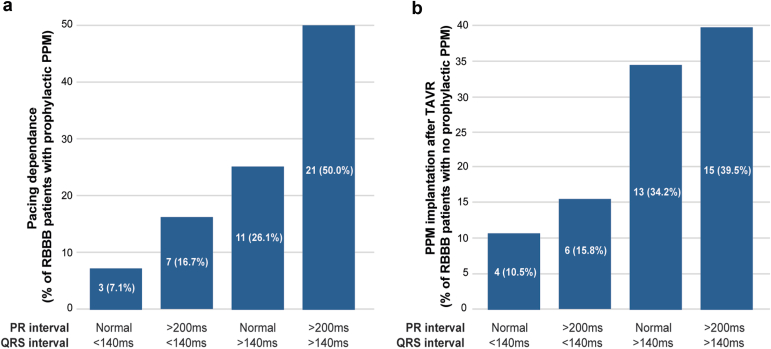
To identify the predictors of pacing dependence after TAVR in patients with baseline RBBB who had undergone prophylactic PPM implantation, we compared the demographic and procedural characteristics of patients with high (maximal Vp > 10%, n = 50) and low (maximal Vp < 10%, n = 29) pacing requirement in the first year after TAVR (Table 2). High pacing requirement was associated with a higher prevalence of peripheral vascular disease (52 vs. 18%, p = 0.01), atrial fibrillation (36 vs. 6%, p = 0.01), longer average PR interval (199 vs. 178 ms, p = 0.03), and average QRS interval (146 vs. 135 ms, p = 0.03). The association between left axis deviation and high pacing requiremenent was not significant (odds ratio [OR] 1.11, 95% CI 0.80-1.42, p = 0.79). In a multivariate binomial logistic regression model, first-degree heart block (OR 2.4, 95% CI 1.7-3.1, p = 0.04) and QRS duration of >140 ms (OR 3.4, 95% CI 2.9-3.9, p = 0.01) retained significance as independent predictors of high requirement (Vp > 10%) in the first year after TAVR (Table 2). In line with the above, a subgroup analysis of prophylactically paced patients with baseline RBBB who exhibited high pacing requirement (i.e., maximal Vp > 10%) revealed normal PR and QRS <140 ms intervals in 3/42 (7.1%) patients, first-degree heart block and QRS <140 ms in 7/42 (16.7%) of patients, normal PR interval and QRS >140 ms in 11/42 (26.1%) patients, and a combination of first-degree heart block together with QRS >140 ms in 21/42 (50.0%) of patients (Figure 4a). In a separate subanalysis of patients with baseline RBBB without a prophylactic PPM before TAVR who required urgent PPM after TAVR (data available for 38 patients), a combination of normal PR interval and QRS <140 ms was seen in 4/38 (10.5%) patients, first-degree heart block and QRS <140 ms in 6/38 (15.8%) patients, normal PR interval and QRS >140 ms in 13/38 (34.2%) patients, and a combination of first-degree heart block with QRS >140 ms in 15/38 (39.5%) of patients (Figure 4b).
Table 2.
Predictors of pacing dependence (Vp > 10%) after TAVR in patients with baseline RBBB undergoing prophylactic PPM implantation
| Predictors of pacing dependence | Univariate analysis |
Multivariate analysis |
||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age (y) | 1.03 (0.92-1.14) | 0.87 | ||
| Sex (M:F) | 1.50 (0.81-2.19) | 0.29 | ||
| BMI (kg/m2) | 0.77 (0.12-1.42) | 0.24 | ||
| Hypertension | 0.91 (0.58-1.24) | 0.37 | ||
| Diabetes | 0.78 (0.39-1.17) | 0.08 | ||
| Smoker (incl ex) | 0.91 (0.71-1.11) | 0.90 | ||
| Creatinine (mmol/L) | 1.19 (0.82-1.56) | 0.52 | ||
| Previous MI | 2.3 (0.72-3.88) | 0.29 | ||
| Previous PCI | 1.23 (0.81-1.65) | 0.72 | ||
| Previous CABG | 1.9 (0.6-2.2) | 0.22 | ||
| Atrial fibrillation | 4.01 (2.47-5.55) | 0.01 | 2.5 (0.6-3.1) | 0.10 |
| Peripheral vascular disease | 2.92 (1.81-4.03) | 0.01 | 3.2 (0.4-3.9) | 0.26 |
| Aortic valve mean gradient (mmHg) | 1.02 (0.93-1.11) | 0.90 | ||
| Aortic valve peak gradient (mmHg) | 1.06 (0.91-1.21) | 0.82 | ||
| LV EF <50% before TAVR | 1.28 (0.71-1.85) | 0.44 | ||
| Left axis deviation | 1.11 (0.80-1.42) | 0.79 | ||
| First-degree heart block | 4.34 (2.91-5.77) | 0.04 | 2.4 (1.5-3.2) | 0.04 |
| QRS interval before TAVR >140 ms | 2.72 (1.99-3.45) | 0.03 | 3.4 (2.9-4.7) | 0.01 |
Abbreviations: BMI, body mass index; CABG, coronary artery bypass grafting; EF, ejection fraction; LV, left ventricle; MI, myocardial infarction; OR, odds ratio; PCI, percutaneous coronary intervention; PPM, permanent pacemaker; RBBB, right bundle branch block; TAVR, transcatheter aortic valve replacement; Vp, ventricular pacing.
Figure 4.
(a) Subgroup analysis of pacing dependence (Vp > 10%) in RBBB patients with prophylactic PPM. (b) Subgroup analysis of RBBB patients with no prophylactic PPM who required urgent PPM after TAVR. ECG data were available for 38 out of 43 TAVR patients with baseline RBBB and no prophylactic PPM who required PPM within 30 days after TAVR.
Abbreviations: ECG, electrocardiogram; PPM, permanent pacemaker; RBBB, right bundle branch block; TAVR, transcatheter aortic valve replacement; Vp, ventricular pacing.
Discussion
To our knowledge, this is the largest study reporting the safety, efficacy, and long-term pacing requirement associated with prophylactic pacemaker implantation before TAVR in patients with baseline RBBB. We found that this strategy is both safe and effective and was associated with a reduction in the length of hospital stay after TAVR. Baseline ECG characteristics, specifically first-degree atrioventricular block and broad RBBB (QRS > 140 ms) were independent predictors of high pacing requirements over long-term follow-up. In the absence of prophylactic pacing, urgent pacemaker implantation after TAVR was required in two-thirds of patients with RBBB.
Conduction Disturbance After TAVR
Despite the advances with newer-generation valves, HAVB remains a common procedural complication, and urgent PPM implantation is required after 2.3% to 36.1% of TAVR procedures.1,14, 15, 16, 17 Baseline RBBB is a strong predictor of HAVB and PPM implantation after TAVR and an independent predictor of cardiovascular mortality.5, 6, 7, 8,18 While baseline RBBB confers a 4.86-fold risk of PPM implantation after TAVR in all patients,18 there are few studies reporting on the predictors of pacing dependence within the subpopulation of TAVR patients with baseline RBBB.11,19, 20, 21 Our analysis identified peripheral vascular disease, atrial fibrillation, PR, and QRS interval duration as significant univariate predictors of pacing dependence in patients with baseline RBBB. Importantly, left axis deviation/left anterior fascicular block showed no significant association with pacing dependence. In multivariate analysis, first-degree heart block and QRS interval duration >140 ms were validated as independent predictors of high pacing requirement.
Prophylactic PPM Implantation Before TAVR
There are no randomized or prospective studies examining the efficacy and safety of prophylactic PPM implantation before TAVR. Recently, Pavitt et al. found that 56% of patients with baseline RBBB who underwent TAVR without a prophylactic PPM required an urgent PPM on their index admission. The rate of pacing-associated complications between prophylactic and urgent PPM implants were comparable, and prophylactic PPM implantation was associated with a shorter length of hospital stay after TAVR (from an average of 4.3 to 2.5 days).20 Similarly, Fukotomi et al. reported that 55/102 (53%) of patients with baseline RBBB and no prophylactic PPM required urgent PPM after TAVR. In their study, prophylactic PPM implantation was associated with shorter procedural time and length of hospital stay, and no significant difference in all-cause mortality was found between patients with baseline RBBB who received PPM before vs. after TAVR.10
Long-Term Pacing Requirement
Conduction disturbance after TAVR may resolve or result in long-term pacing requirement. In a study of 261 patients with baseline RBBB, Isogai et al.19 reported that the majority (76.7%) of HAVB events occur during the TAVR procedure with a further 8.3% incidence in the first 30 days after TAVR. Complete recovery of HAVB after PPM implantation was only seen in 7.1% of cases. Our longitudinal pacing analysis supports the idea that once established, the pacing requirement in patients with baseline RBBB remains relatively stable: only 11/79 (14%) of patients showed an absolute change in Vp of more than 10% over 1 year after TAVR. Importantly, all of these patients had a high initial pacing requirement (Vp > 70%), and in none of these patients, the Vp requirement was reduced to below 10% at any point during the study.
Implications for Practice
Prophylactic PPM implantation in patients with baseline RBBB is a safe and effective clinical strategy that reduces the length of hospital stay after TAVR. The majority of patients undergoing prophylactic PPM implantation will require ongoing pacing over time; without prophylactic pacing, urgent PPM implantation will be required in two-thirds of cases. Based on these data, an increasing number of patients with baseline RBBB in our practice have undergone prophylactic PPM implantation before TAVR over recent years, and this has become a standard recommendation in our current practice.
Limitations
High pacing requirement/pacing dependence was defined as maximal Vp > 10% over 1 year after TAVR.13 In the absence of a unifying definition of pacing dependence, the thresholds across the existing literature vary from 1% to 40%.20,22 All data were analyzed retrospectively. Randomized clinical trials are needed to further evaluate the practice of prophylactic PPM implantation.
Conclusions
Prophylactic PPM implantation for patients with baseline RBBB is a safe and effective strategy that reduces the length of hospital stay after TAVR. ECG characteristics of first-degree atrioventricular block and broad RBBB (QRS > 140 ms) are independent baseline predictors of pacing high pacing requirement (Vp > 10%) in the first year after TAVR.
Ethics Statement
The project was approved by Oxford University Hospitals Institutional and Departmental Board review.
Funding
The authors have no funding to report.
Disclosure Statement
The authors report no conflict of interest.
Footnotes
Supplemental data for this article can be accessed on the publisher’s website.
Supplementary Material
References
- 1.Khatri P.J., Webb J.G., Rodés-Cabau J., et al. Adverse effects associated with transcatheter aortic valve implantation: a meta-analysis of contemporary studies. Ann Intern Med. 2013;158(1):35–46. doi: 10.7326/0003-4819-158-1-201301010-00007. [DOI] [PubMed] [Google Scholar]
- 2.Glikson M., Nielsen J.C., Kronborg M.B., et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: developed by the Task Force on cardiac pacing and cardiac resynchronization therapy of the European Society of Cardiology (ESC) with the special contribution of the European Heart Rhythm Association (EHRA) Eur Heart J. 2021;42(35):3427–3520. doi: 10.1093/EURHEARTJ/EHAB364. [DOI] [PubMed] [Google Scholar]
- 3.Al-Ogaili A., Fugar S., Okoh A., et al. Trends in complete heart block after transcatheter aortic valve replacement: a population based analysis. Catheter Cardiovasc Interv. 2019;94(6):773–780. doi: 10.1002/CCD.28156. [DOI] [PubMed] [Google Scholar]
- 4.Lilly S.M., Deshmukh A.J., Epstein A.E., et al. 2020 ACC expert consensus decision pathway on management of conduction disturbances in patients undergoing transcatheter aortic valve replacement: a report of the American college of Cardiology solution set oversight committee. J Am Coll Cardiol. 2020;76(20):2391–2411. doi: 10.1016/J.JACC.2020.08.050/SUPPL_FILE/MMC2.PDF. [DOI] [PubMed] [Google Scholar]
- 5.Sammour Y., Krishnaswamy A., Kumar A., et al. Incidence, predictors, and implications of permanent pacemaker requirement after transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2021;14(2):115–134. doi: 10.1016/J.JCIN.2020.09.063. [DOI] [PubMed] [Google Scholar]
- 6.Siontis G.C.M., Jüni P., Pilgrim T., et al. Predictors of permanent pacemaker implantation in patients with severe aortic stenosis undergoing TAVR: a meta-analysis. J Am Coll Cardiol. 2014;64(2):129–140. doi: 10.1016/J.JACC.2014.04.033. [DOI] [PubMed] [Google Scholar]
- 7.Saint Croix G.R., Lacy S.C., Hrachian H., Beohar N. Clinical impact of preexisting right bundle branch block after transcatheter aortic valve replacement: a systematic review and meta-analysis. J Interv Cardiol. 2020;2020:1789516. doi: 10.1155/2020/1789516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watanabe Y., Kozuma K., Hioki H., et al. Pre-existing right bundle branch block increases risk for death after transcatheter aortic valve replacement with a balloon-expandable valve. JACC Cardiovasc Interv. 2016;9(21):2210–2216. doi: 10.1016/J.JCIN.2016.08.035. [DOI] [PubMed] [Google Scholar]
- 9.Auffret V., Webb J.G., Eltchaninoff H., et al. Clinical impact of baseline right bundle branch block in patients undergoing transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2017;10(15):1564–1574. doi: 10.1016/J.JCIN.2017.05.030. [DOI] [PubMed] [Google Scholar]
- 10.Fukutomi M., Hokken T., Wong I., et al. Prophylactic permanent pacemaker implantation in patients with right bundle branch block undergoing TAVR. JACC Cardiovasc Interv. 2021;14(11):1272–1274. doi: 10.1016/J.JCIN.2021.03.043. [DOI] [PubMed] [Google Scholar]
- 11.Tovia-Brodie O., Letourneau-Shesaf S., Hochstadt A., et al. The utility of prophylactic pacemaker implantation in right bundle branch block patients pre-transcatheter aortic valve implantation. Isr Med Assoc J. 2019;21(12):790–795. [PubMed] [Google Scholar]
- 12.Rodés-Cabau J., Ellenbogen K.A., Krahn A.D., et al. Management of conduction disturbances associated with transcatheter aortic valve replacement: JACC scientific expert panel. J Am Coll Cardiol. 2019;74(8):1086–1106. doi: 10.1016/J.JACC.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Patel K.P., Lim W.Y., Pavithran A., et al. Early pacemaker implantation for transcatheter aortic valve implantation is safe and effective. Pacing Clin Electrophysiol. 2022;45(1):103–110. doi: 10.1111/PACE.14397. [DOI] [PubMed] [Google Scholar]
- 14.Ullah W., Zahid S., Zaidi S.R., et al. Predictors of permanent pacemaker implantation in patients undergoing transcatheter aortic valve replacement - A systematic review and meta-analysis. J Am Heart Assoc. 2021;10(14) doi: 10.1161/JAHA.121.020906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nazif T.M., Dizon J.M., Hahn R.T., et al. Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: the PARTNER (Placement of AoRtic TraNscathetER Valves) trial and registry. JACC Cardiovasc Interv. 2015;8(1 Pt A):60–69. doi: 10.1016/J.JCIN.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 16.De Carlo M., Giannini C., Bedogni F., et al. Safety of a conservative strategy of permanent pacemaker implantation after transcatheter aortic CoreValve implantation. Am Heart J. 2012;163(3):492–499. doi: 10.1016/J.AHJ.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Van Rosendael P.J., Delgado V., Bax J.J. Pacemaker implantation rate after transcatheter aortic valve implantation with early and new-generation devices: a systematic review. Eur Heart J. 2018;39(21):2003–2013. doi: 10.1093/EURHEARTJ/EHX785. [DOI] [PubMed] [Google Scholar]
- 18.Ravaux J.M., Di Mauro M., Vernooy K., et al. Impact of bundle branch block on permanent pacemaker implantation after transcatheter aortic valve implantation: a meta-analysis. J Clin Med. 2021;10(12):1–20. doi: 10.3390/JCM10122719/S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Isogai T., Dykun I., Agrawal A., et al. Risk stratification and management of advanced conduction disturbances following TAVI in patients with pre-existing RBBB. Structural Heart. 2022;6(1) doi: 10.1016/J.SHJ.2022.100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pavitt C., Waleed M., Arunothayaraj S., et al. Transcatheter aortic valve implantation in patients with right bundle-branch block: should prophylactic pacing Be undertaken? J Invasive Cardiol. 2023;35(1):E37–E45. doi: 10.25270/jic/22.00261. [DOI] [PubMed] [Google Scholar]
- 21.Ravaux J.M., Di Mauro M., Vernooy K., et al. One-year pacing dependency after pacemaker implantation in patients undergoing transcatheter aortic valve implantation: systematic review and meta-analysis. JTCVS Open. 2021;6:41. doi: 10.1016/J.XJON.2021.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bruno F., Munoz Pousa I., Saia F., et al. Impact of right ventricular pacing in patients with TAVR undergoing permanent pacemaker implantation. JACC Cardiovasc Interv. 2023;16(9):1081–1091. doi: 10.1016/J.JCIN.2023.02.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.