Abstract
Introduction
The Pregnancy and Newborn Diagnostic Assessment (PANDA) system is a mobile application designed to facilitate diagnosis and decision-making by healthcare staff in antenatal care (ANC). This study aimed to evaluate its effectiveness in improving the quality of ANC.
Methods
This randomised controlled trial implemented the PANDA system in two groups of health facilities (intervention and comparison groups) using a matched-pair method in the Koupéla health district, Burkina Faso. Six health centres were included in each group. We included pregnant women presenting with more than 20 weeks of amenorrhea during their first antenatal consultation, and we followed them up until their sixth week postpartum. The primary outcome was a binary variable derived from the ANC quality score, coded yes or no. Six components of ANC quality were identified: welcoming the woman, history taking and dietary habits, physical examination, obstetric examination, preventive care, and counselling and advice. We used Poisson regression with robust variance to compare the unadjusted and adjusted primary outcomes results between the two study arms.
Results
We included 319 and 272 women in the intervention and comparison groups, respectively. In the intervention group, 15.67% (50 out of 319) of the women had at least 75% of the total ANC quality score, compared to 6.25% (17 out of 272) in the comparison group. Adjusted results showed that women in the intervention group were 2.71 times more likely to have an excellent total ANC quality score than women in the comparison group (RR = 2.71; 95% CI [1.60–4.60]; p < .001).
Conclusion
Although the proportion of women with good ANC quality was low, this study showed that the PANDA system significantly improves the ANC quality. These results are vital because Burkina Faso has decided to use these computerised clinical decision support systems for maternal and child health.
Keywords: Telemedicine, PANDA, quality of care, antenatal care, Burkina Faso, intervention
Introduction
The use of information and communication technologies in maternal and neonatal health has increased rapidly in recent years. One of the most widely covered aspects is the antenatal consultation (ANC) offered to pregnant women. Despite its importance, the indicators of the use of antenatal consultation services (percentage of women who start the first ANC in the first trimester, and percentage of women who perform at least four ANC) remain low in sub-Saharan Africa in general.1–3 This situation is found in Burkina Faso where, in 2021, according to the results of the Demographic and Health Survey, 72% of women have made at least four antenatal visits, and 53% of women began ANC during the first trimester of pregnancy. Among women who received ANC, the median number of months of pregnancy at the first antenatal visit was estimated at 3.9. 4 The consequences of this poor access to and use of maternal and child health services are high maternal and infant mortality rates. According to the United Nations Children's Fund, in 2017, the maternal mortality ratio was estimated to be 320 per 100,000 live births, the neonatal mortality rate was 26‰, and 52% of pregnant women had at least four antenatal consultations. 5
Several reasons can explain this low percentage of women attending at least four ANC, including poor quality of care and dissatisfaction among pregnant women with ANC, as shown by some authors. While some studies have shown that the various stages of ANC are not respected or are ignored or misunderstood by providers,6–11 others have shown that adherence to the guidelines for antenatal consultations is low.1,12–17 However, according to the World Health Organization (WHO), within the continuum of reproductive healthcare, ANC provides a platform for important healthcare functions including health promotion, screening and diagnosis, and disease prevention. It has been established that by implementing timely and appropriate evidence-based practices, ANC can save lives. 18 Therefore, it is necessary to improve the quality of ANC services based on their benefits.
One way to improve the quality of ANC is to improve provider's adherence to protocols, which requires healthcare staff to follow every stage of the antenatal consultation. Therefore, the use of mobile applications and telemedicine seems appropriate. The WHO has insisted on using mobile applications to provide maternal and child healthcare because, according to the WHO, their use is linked to reduced healthcare costs, improved quality, and equitable access to healthcare services. 19 There are numerous areas of application of information and communication technologies in the healthcare sector, ranging from customer education for behavioural change, medical records, electronic decision support, quality of care in healthcare services, human resources management, and supply chain management. 20
Over the last few decades, several electronic clinical decision-support systems have been implemented in Burkina Faso, such as the Integrated electronic-Diagnostic Approach (IeDA), developed to improve provider's adherence to protocols of Integrated Management of Childhood Illnesses. In 2019, the IeDA platform was expanded to include a Reproductive Health and Maternity Care e-registry (REC-Maternity).21–24
Regarding decision support and quality of care, ANC, in particular, has become a popular field in mobile applications around the world.25–30 The results of these different studies are mixed. In 2018, Chen et al. conducted a systematic review of the effectiveness and relevance of mobile apps for maternal and child health between 2011 and 2016. A total of 245 studies were included, including 51 randomised controlled trials. The results showed that almost half (43%) of the randomised controlled trials showed no effects of mobile apps on maternal and child health. 31 In addition to these mobile applications, computerised clinical decision-support systems have been developed. Haddad et al. 32 conducted a systematic review of these computerised systems in 2019. They found nine systems that met their eligibility criteria, including the Pregnancy and Newborn Diagnostic Assessment (PANDA) systems.33,34 The PANDA system was analysed as one of the most comprehensive applications and includes numerous functions. This is a mobile application designed to facilitate diagnosis and decision-making by healthcare staff in ANC. Feasibility and acceptability studies of this system have been conducted in Madagascar and Burkina Faso.35,36 However, the authors of the systematic review of computerised clinical decision support systems concluded that their usefulness for ANC was limited.32,37 Therefore, the added value of these systems remains to be proven. Although publications on the PANDA system have shown that it enables standardised ANC according to the WHO guidelines, 35 it is still essential to assess its effectiveness in improving ANC quality using a study with a high level of evidence. The overall objective of this study was to assess the effectiveness of the PANDA telemedicine system in improving the quality of ANC in Burkina Faso.
Methods
Trial design
To implement this research, we implemented a cluster randomised trial. The rationale for implementing a cluster randomised trial is that the intervention (training and use of the PANDA system) cannot be implemented at the individual (pregnant woman) level but only at the health centre level. Health centres in the intervention group offered ANC using the PANDA system installed on tablets. Each health facility in this group received at least one tablet. Health centres in the comparison group offered the usual ANC.
Study settings
This study was conducted in the health district of Koupéla (Center-East region, Burkina Faso). This district was chosen because it is near Ouagadougou (the capital of Burkina Faso) and because there were no ongoing ANC interventions. It is equally important to note that the PANDA feasibility test was conducted in this district in 2016. 36
Health centres and participants’ eligibility criteria
Twelve primary health centres in the Koupèla district were selected for participation in the study. Health centres were selected by identifying six pairs of comparable health centres and randomising them using the matched-pair method. The matching criteria were (1) the number of total ANC visits in the year before the trial, (2) number of total deliveries in the year before the trial, (3) number of total postnatal care visits in the year before the trial, (4) number of women of childbearing age in the health centre area, (5) total number of healthcare workers in the health centre as well as the distribution by profile (midwives, nurses, and auxiliary birth attendants), and (6) size of the population served. These matching variables allow us to obtain facilities within each pair that are similar in terms of matching factors.
The participants were pregnant women with a gestational age between 14 and 20 weeks of amenorrhea, regardless of age, place of residence, or socio-economic status.
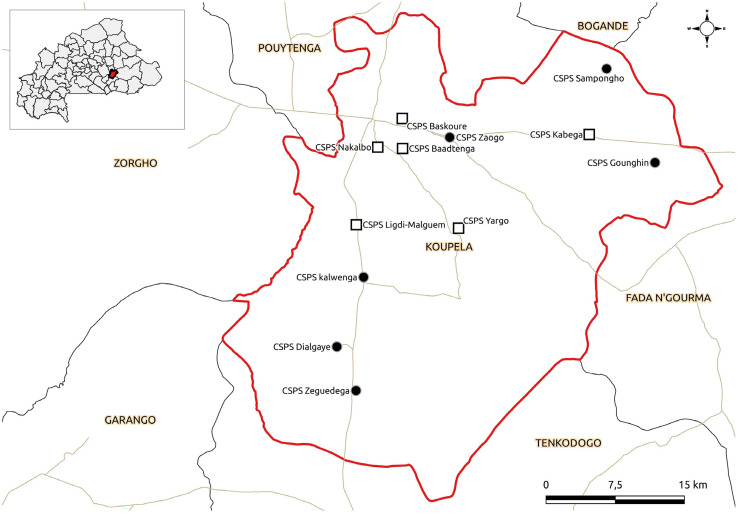
A full description of the health centres and participants’ eligibility criteria has already been detailed elsewhere. 38 The health centres included in this study are shown in Figure 1. The research team produced this figure using a quantum geographic information system. 39
Figure 1.
Health map of the PANDA study sites in Burkina Faso.
PANDA: Pregnancy and Newborn Diagnostic Assessment.
Interventions
PANDA is a telemedicine system designed to meet women's healthcare needs during pregnancy in resource-scarce contexts by extending and standardising ANC according to the WHO guidelines. A detailed description of the PANDA system is provided elsewhere. 38 We organised several training sessions for the intervention group health centre workers to better explain the use of the PANDA app (user training at the health centre and medical unit levels).
Outcomes
The primary outcome was the quality of ANC. This is an indicator in the form of a score that considers all the items of higher quality ANC according to the age of the pregnancy. The various items were grouped into components: (i) welcoming the woman, (ii) history-taking and dietary habits, (iii) physical examination, (iv) obstetrical examination, (v) preventive care, and (vi) counselling and advice. These items are based on Burkina Faso's ANC policy. 40 Categorisation means that each woman had a total score for each ANC (from the first to the last consultation). Depending on the age of the pregnancy, a certain number of items are not filled in. The construction of the indicator considered these specificities. The list of all the items has already been detailed elsewhere. 38 Thus, each woman had a total score for the quality of ANC that she received from her first consultation to her delivery.
Sample size
The calculation of the required sample size considered several statistical features inherent to the design of the study, such as the number of participants per cluster (set at 40 per health centre), the intraclass correlation coefficient (ICC, set at 0.015), the inflation factor (based on the value of the ICC, inflation factor was set at 1.585), the desired statistical power (80%), and the margin of error (5%).
Using Stata software, the number of health centres required to detect a difference of at least 15% (80% in the intervention group versus 65% in the control group) in the proportion of women with an excellent ANC quality score was six health centres in each group (240 women). Considering the proportion of women lost to follow-up at 10%, the final sample size required was 264 women in each group for a total of 12 health centres. The hypothetical proportion of 65% in the comparison group was based on the results of a study conducted in Ghana by Baafi et al. in 2019. 41
Recruitment
Providers recruited participants during ANC sessions after the history-taking and physical examination. After identifying potentially eligible women, their written consent to participate in the study was obtained after obtaining all the necessary information for a free and informed decision to participate.
Randomisation
We selected six pairs of health centres, and within each pair, the centre that received the PANDA system was chosen randomly using a draw from one health centre for each pair. The names of the health centres were previously placed in individual sealed envelopes. The drawer was different from the person who prepared the envelopes and was absent when the envelopes were sealed. Therefore, the drawing was performed six times. All eligible consecutive participants were included in the study.
Blinding
Given the nature of our intervention, blinding was not possible.
Data collection methods
Data were collected from women on the day of inclusion and then each time the woman returned for an antenatal visit until the sixth week after delivery. A data collector was assigned to two health centres for the duration of the study (one health centre in the intervention group and one in the comparison group). The questionnaires were administered to the women immediately after the antenatal consultation. The interviewer visited the health centres according to an antenatal consultation schedule. For this study, data were collected using a closed questionnaire by directly interviewing the woman (for some items) and extracting data from ANC and delivery registers, ANC records, and health diaries. A field coordinator was recruited and was responsible for checking the interviewers’ work.
Other authors have not previously used the questionnaire we used because it aligns with the recommendations of the Ministry of Health of Burkina Faso on ANC provision to women. 40 However, during the interviewers’ training, before data collection, we conducted a two-day pilot test to improve the version of the questionnaire.
Statistical methods
All analyses of the cluster randomised trial were performed on an intention-to-treat basis using Stata 18. 42 The unit of analysis was the woman. We compared the unadjusted and adjusted effect of the PANDA system on ANC quality between the intervention and comparison groups. Unbalanced sociodemographic characteristics between the two study groups were used to adjust the intervention effects on the study outcome. Poisson regression with robust variance was used with a threshold of 5%. We also compared the intervention effect on the various dimensions of ANC quality.
Ethics approval
This trial was registered with the Pan-African Clinical Trials Registry under PACTR202009861550402 on 21 September 2020. The Burkina Faso Health Research Ethics Committee approved the research protocol for this trial under approval number 2020-3-051. After obtaining their written informed consent, adult participants (at least 18 years old) were included. Minor participants were included after obtaining their written assent and parental written consent. Interviewers assigned to the various health centres were responsible for obtaining consent. The research team carefully monitored this process during the field supervision. None of the questions in the database contained information that could be used to formally identify women.
Results
Flow chart
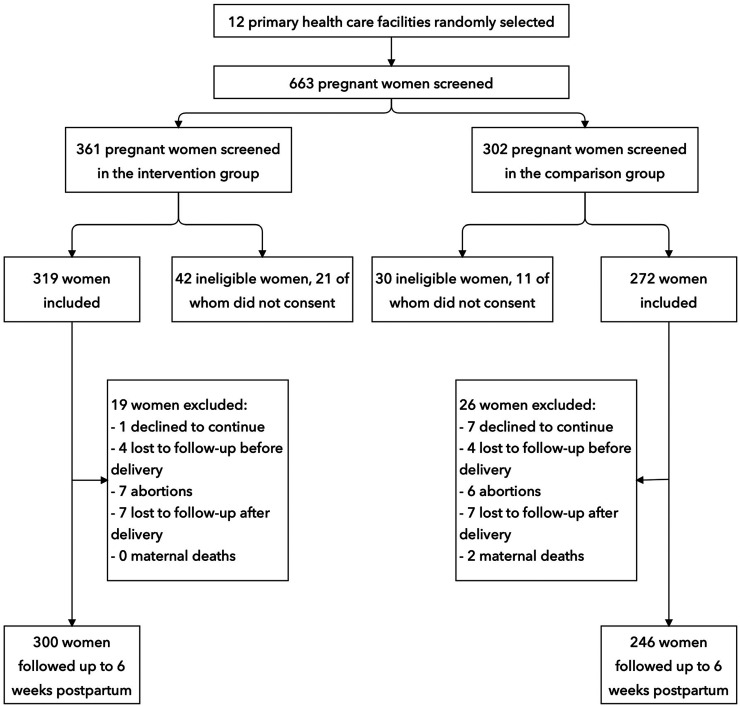
In this study, 663 women were pre-selected, 319 and 272 were included, and 300 and 246 women were followed up until six weeks postpartum in the intervention and comparison groups, respectively (Figure 2).
Figure 2.
Flow chart.
Recruitment
Inclusion began on 12 July 2020 and continued until January 2021. Data collection ended in October 2021, corresponding to the sixth week postpartum for the last participant.
Use of the PANDA app during subsequent ANCs
The use of the PANDA app was not uniform across the health centres in the intervention group. For the first ANC, it was confirmed that the woman was offered an ANC with the PANDA application; however, the health workers did not use the PANDA App systematically for subsequent ANCs. Thus, the use of the PANDA application increased from 72.5% for ANC2 to 78.1% for ANC3 and declined to 66.0% for ANC6. Table 1 shows the disparities in using the PANDA application for subsequent ANC by the intervention group health centre.
Table 1.
Use of the PANDA application during subsequent ANCs 2 to 7.
| PANDA app use during the antenatal care* | ||||||
|---|---|---|---|---|---|---|
| Health centre name | ANC 2 | ANC 3 | ANC 4 | ANC 5 | ANC 6 | N |
| Kalwêga | 84.4 | 96.0 | 97.1 | 77.3 | 75.0 | 59 |
| Zaogo | 41.0 | 50.0 | 25.6 | 38.7 | 30.0 | 53 |
| Dialgaye | 96.0 | 87.5 | 93.6 | 95.5 | 100.0 | 66 |
| Sampongho | 84.6 | 82.9 | 84.6 | 77.3 | 88.9 | 64 |
| Gounghin | 78.7 | 82.9 | 68.1 | 88.5 | 66.7 | 64 |
| Zéguédéga | 39.5 | 54.5 | 51.3 | 47.8 | 42.9 | 55 |
| Total | 72.5 | 78.1 | 69.5 | 69.2 | 66.0 | 319 |
*The PANDA app was used for all women during the first antenatal care.
Pregnancy and Newborn Diagnostic Assessment; ANC: antenatal care.
Characteristics of women at inclusion
Regarding sociodemographic characteristics at inclusion, women were evenly distributed between the two groups for all other socio-demographic characteristics (Table 2).
Table 2.
Socio-demographic characteristics of women at inclusion.
| Group | |||||
|---|---|---|---|---|---|
| intervention | Comparison | p | |||
| N = 319 | % | N = 272 | % | ||
| Age of the woman (in years) | .343 | ||||
| 13–17 | 10 | 3.1 | 5 | 1.8 | |
| 18–24 | 137 | 42.9 | 121 | 44.5 | |
| 25–34 | 133 | 41.7 | 102 | 37.5 | |
| 35 and over | 39 | 12.2 | 44 | 16.2 | |
| Marital status | .166 | ||||
| Married | 245 | 76.8 | 225 | 82.7 | |
| Common-law | 70 | 21.9 | 43 | 15.8 | |
| Single | 4 | 1.3 | 4 | 1.5 | |
| Highest level of education achieved | .068 | ||||
| None | 223 | 69.9 | 169 | 62.1 | |
| Primary | 50 | 15.7 | 45 | 16.5 | |
| Secondary/higher | 46 | 14.4 | 58 | 21.3 | |
| Current occupation | .303 | ||||
| Pupil/student | 14 | 4.4 | 14 | 5.1 | |
| Housewife/farmer | 271 | 85.0 | 220 | 80.9 | |
| Tradeswomen | 34 | 10.7 | 38 | 13.9 | |
| Total number of pregnancies including the pregnancy used for inclusion | .754 | ||||
| 1 | 78 | 24.5 | 60 | 22.1 | |
| 2–3 | 186 | 58.3 | 161 | 59.2 | |
| 4 and over | 55 | 17.2 | 51 | 18.8 | |
| Number of living (biological) children | .169 | ||||
| None | 89 | 27.9 | 72 | 26.5 | |
| 1–4 | 205 | 64.3 | 166 | 61.0 | |
| 5–9 | 25 | 7.8 | 34 | 12.5 | |
Regarding the clinical characteristics of the women, 27.3% and 32.4% of the women in the intervention and comparison groups, respectively, reported having planned the pregnancy used for inclusion (p = .001). A comparison of the other variables showed no significant difference between the intervention and comparison groups. These results are summarised in Table 3.
Table 3.
Clinical characteristics of women at inclusion.
| Group | |||||
|---|---|---|---|---|---|
| intervention | Comparison | p | |||
| N = 319 | % | N = 272 | % | ||
| Time elapsed between the end of the last pregnancy and the start of the pregnancy used for inclusion | .638 | ||||
| <6 months | 6 | 1.9 | 4 | 1.5 | |
| 6–11 months | 6 | 1.9 | 5 | 1.8 | |
| 12–23 months | 34 | 10.7 | 39 | 14.3 | |
| 24–35 months | 93 | 29.2 | 88 | 32.4 | |
| At least 36 months | 102 | 32.0 | 76 | 27.9 | |
| First pregnancy | 78 | 24.5 | 60 | 22.1 | |
| Current planned pregnancy | .001 | ||||
| No | 40 | 12.5 | 63 | 23.2 | |
| Yes | 279 | 87.5 | 209 | 76.8 | |
| Contraception use in the year before becoming pregnant | .178 | ||||
| No | 232 | 72.7 | 184 | 67.6 | |
| Yes | 87 | 27.3 | 88 | 32.4 | |
| Number of abortions | .342 | ||||
| No | 273 | 85.6 | 240 | 88.2 | |
| Yes | 46 | 14.4 | 32 | 11.8 | |
| Does the woman always go for a consultation on her own? | .703 | ||||
| No | 247 | 77.4 | 207 | 76.1 | |
| Yes | 72 | 22.6 | 65 | 23.9 | |
Quality of ANC
Intent-to-treat analysis showed that 50 women out of 319 (15.67%; 95% CI [12.07–20.10]) in the intervention group had at least 75% of the total ANC quality score, compared with 17 women out of 272 (6.25%; 95% CI [3.91–9.84]) in the comparison group.
In univariate analysis, we found that women in the intervention group were 2.51 (95% CI [1.48–4.25]) times more likely to have an excellent total ANC quality score than women in the comparison group (p = .001). In multivariate analysis, the difference was still in favour of the intervention group (RR = 2.71; 95% CI [1.60–4.60]; p < .001). The results were adjusted for the number of ANCs performed, the highest level of education achieved, knowledge of the childbirth preparation and obstetric emergencies card, the number of biological children, and pregnancy planning at inclusion. These variables were not equally distributed between the two study groups.
ANC quality by dimension
The analyses showed a significant difference between the two study groups in favour of the intervention group only for the dimensions relating to advice. No differences were noted between the study groups for the dimensions relating to welcoming the woman (not significant), history-taking and dietary lifestyle (not significant), and obstetrical examination (not significant). However, the differences were significant for physical examination and preventive care but in favour of the control group. Table 4 presents the results of the study.
Table 4.
Effects of the PANDA system on ANC quality dimensions.
| Intervention n (%) | Control n (%) | RR (95% CI) | p | |
|---|---|---|---|---|
| Women having 75% of the score for welcoming the woman | 257 (80.6) | 218 (80.1) | 1.00 (0.92–1.08) | .948 |
| Women having 75% of the score for history-taking and dietary history | 157 (49.2) | 120 (44.1) | 1.12 (0.95–1.32) | .181 |
| Women having 75% of the score for the physical examination | 285 (89.3) | 260 (95.6) | 0.94 (0.89–0.98) | .006 |
| Women having 75% of the score for the obstetrical examination | 152 (47.6) | 120 (44.1) | 1.11 (0.93–1.33) | .262 |
| Women having 75% of the score for preventive care | 1 (0.3) | 20 (7.4) | 0.04 (0.01–0.3) | .002 |
| Women having 75% of the score for advice | 112 (35.1) | 62 (22.8) | 1.68 (1.29–2.17) | <.001 |
Pregnancy and Newborn Diagnostic Assessment; ANC: antenatal care.
Discussion
The use of the PANDA system significantly affected the quality of ANC. In other words, performing ANC using the PANDA system could increase the proportion of women receiving high-quality ANC from 6.25% to 15.67%, although this proportion still needs improvement. Our result on the low proportion of high-quality ANC is similar to those of the authors who used several components of ANC to assess its quality. Indeed, while Olorunsaiye et al., in a study carried out with secondary data from several countries in West and Central Africa, found that less than one woman in five received good quality ANC, 17 in Nigeria, only one woman in 20 received all nine components used to assess the quality of ANC, 43 in Ethiopia, one study found that almost one woman in five received good quality ANC 44 and another study showed that this proportion was 33%. 45 Other authors have also demonstrated that the quality of ANC is poor in developing countries, at 31.38% 46 and 41.2%. 47
The low proportions noted in our study could be linked to the fact that we constructed the ANC quality indicator by considering all aspects of an ANC (starting with the key elements to look for in the woman's history, the data from the physical examination, the preventive care offered to the woman, the paraclinical examinations, etc.). Except for a few items, all other items must be measured at each ANC. Thus, we obtained the total score for each woman from the first to the last ANC. In almost all the studies, some components were not considered when constructing the ANC quality indicator. Studies in which the number of components used was similar to that used in our research reported similar results.17,43 However, although most studies agree that the quality of ANC is poor in developing countries, it should be noted that some studies have shown results that differ from ours regarding the proportion of women receiving good-quality ANC. Indeed, Duysburgh et al., in a study conducted in three countries (Burkina Faso, Ghana, and Tanzania), showed that the overall quality of routine antenatal and obstetric care was satisfactory in the six districts of their study.48,49 Another study carried out in 2021 on the effectiveness of the REC-Maternity in Burkina Faso showed that the overall quality of health service provision was relatively high in both intervention and control groups (52% vs 51%). 22 However, the REC Maternity study used direct observation to measure the quality of care in health facilities. Although this data collection technique is the best recommended, it could introduce some bias as health workers could change their practice during the observation, as the sample size was only around five in each health centre (the sample size estimation took into account the assumption of at least five consultations in each of the 48 health centres), 22 contributing in the high overall quality of health service provision in both intervention and control groups.
However, ANC is an essential procedure and a critical intervention to help reduce maternal and neonatal mortality. Therefore, the WHO recommends eight ANC focal points because increasing the frequency of ANC in the health system for women and adolescents is associated with a reduced risk of stillbirths, as these consultations offer more opportunities to detect and manage potential problems. 50
Regarding the effect of the PANDA system on ANC quality, some authors found similar results. In Nigeria, McNabb et al. in 2015, tested a mobile application using health education audio clips to improve and standardise advice for pregnant women and concluded that introducing a low-cost mobile case management and decision support application could stimulate behavioural change and improve the quality of care provided to pregnant women by less skilled healthcare personnel. 27 Another study by Venkateswaran et al., in Palestine in 2017, showed that compared with the control group, the intervention led to greater adherence to guidelines in the intervention group for the screening and management of anaemia, hypertension, and gestational diabetes. 51 These results are consistent with some of our findings.
The results of this study showed that the difference between the intervention and control groups was statistically significant only for the physical examination, preventive care and counselling components. However, the score was significantly higher in the intervention group only for counselling/advice. Counselling includes advice on food hygiene, malaria prevention, use of insecticide-treated mosquito nets, pregnancy danger signs, newborn danger signs and signs of labour. Health workers’ characteristics may explain this difference in favour of the comparison group for the two components. Although we matched the health centres according to certain criteria, including the profiles of the health workers, there could still be some differences in skills and experience in providing ANC. Therefore, two people with the same profile could have different skills in providing ANC, unbalancing the difference in favour of the comparison group. The study on the REC-Maternity did not find a statistically significant difference in the overall quality score between the intervention and comparison districts. However, significant differences were observed between the two districts according to the sub-components of quality of care, 22 making these results similar to some of ours.
Our study also revealed that preventive care was not well explained to pregnant women. Only one woman had a high score on how to take malaria prophylaxis treatment, anaemia prevention, and deworming in the intervention group, compared to 20 women in the control group. This result is problematic because of the importance of these preventions, especially anaemia, which has many adverse effects on maternal and child health.52,53
Strengths and limitations of the study
These findings suggest that the PANDA system could serve as a model for expanding quality ANC in similar rural contexts, warranting further research and policy consideration for broader implementation. Each data collector had an intervention health centre and a comparison health centre. This presupposes standardised data collection in the two study groups. In addition, using tablets with the quality control system prevented errors and non-responses to the various questions. Supervision of data collection throughout the research also ensured that the data was of good quality. By opting for a randomised study, we can affirm that the results have a high level of evidence compared with the results already available in the literature, which for several studies were pilot or feasibility studies results with small sizes.
Regarding limitations, it should be noted that the implementation of the intervention (use of the PANDA system) was heterogeneous in the different health centres. In addition, within the same health centre, we noted a heterogeneity in implementation, depending on the health workers. Furthermore, although we used matching criteria for the health centres, we could not exclude the unequal skills of the care providers between the two study groups.
It is also important to note some limitations regarding our questionnaire and data collection techniques. Regarding the data collection techniques, some responses were obtained from women by direct interview and are therefore subject to bias. These biases may, on the one hand, be related to the fact that they are illiterate and may not have fully understood some questions about the receipt of the ANC components. On the other hand, these biases may be social desirability biases. For researchers to get a good picture of the quality of care provided to women by health workers, women may voluntarily under-report inadequacies in care. However, the opposite is also possible in this study: they may have falsely reported that components of ANC were not provided. All these limitations must be considered, not only when interpreting the proportion of women who received good quality ANC, but also when interpreting the effect of the PANDA application on the quality of ANC. Fortunately, not all components were collected by interviewing the woman, but only some, as detailed in the published protocol. 38 Most of the responses to the items were extracted from the women's health cards and health registers, as the health worker is required to record all care provided to the woman on the health card. The implication of extracting data from the registers is that care may have been provided but not recorded in the data collection instruments (maternity registers and health cards). Although these reporting biases may be balanced in the two study groups, some of our results should be interpreted cautiously.
Moreover, the difference was not significant for half (3/6) of the components. This may reflect sample size issues that make it difficult to detect small differences, as the original sample power was designed to detect a minimum difference of 15%. This may explain the findings at the granular level.
Finally, although we designed a cluster randomised controlled trial, due to the nature of the intervention, neither the study sites nor the participants are blinded to the study conditions. In addition, the participating sites are limited to one rural district of Burkina Faso, so the results may not be generalisable at the national level (no urban facilities are included in this study).
Conclusion
Although the proportion of women with good ANC quality was low, this study showed that the PANDA system significantly may improve the quality of ANC since its effect was higher for some components. These results are vital because Burkina Faso has decided to use these computerised clinical decision support systems in many areas, notably reproductive health (through the electronic consultation register for maternity-REC-Maternity) and child health (through the IeDA for the Integrated Management of Childhood Illnesses). The results on the quality dimensions of ANC call on the stakeholders to raise awareness and strengthen the skills of front-line staff in rural areas to advise pregnant women on the various prophylactics to be administered. As anaemia is a risk factor for many adverse pregnancy outcomes, its prevention in pregnant women must be scrupulously respected and in line with the current guidelines. Our results could guide countrywide policies for improving maternal and newborn health, highlighting the benefits of such an electronic decision support system for similar rural African areas where maternal and newborn morbidity and mortality rates are high.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076241298499 for Assessing the effectiveness of the Pregnancy And Newborn Diagnostic Assessment system on the quality of antenatal care in Burkina Faso: A cluster-randomised controlled trial by Abou Coulibaly, Armel Emmanuel Sogo, Nutsa Chikvaidze, Cecilia Capello, Tsion Kefene Gerbaba and Séni Kouanda in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241298499 for Assessing the effectiveness of the Pregnancy And Newborn Diagnostic Assessment system on the quality of antenatal care in Burkina Faso: A cluster-randomised controlled trial by Abou Coulibaly, Armel Emmanuel Sogo, Nutsa Chikvaidze, Cecilia Capello, Tsion Kefene Gerbaba and Séni Kouanda in DIGITAL HEALTH
Acknowledgements
We thank all those involved in the design of this study, mainly the Directorate of Health Information Systems, the Directorate of Family Health, and the members of the two non-governmental organisations Enfants Du Monde and the Private and Community Initiative for Health and the Response to HIV/AIDS in Burkina Faso. We also thank all the interviewers. Lastly, we thank Abdoul-Aziz Kinda for his assistance.
Footnotes
Access to data: The data are available to anyone who wishes to have them as soon as possible by formally requesting them from the research team or the sponsor.
Contributorship: Conceptualisation: Abou Coulibaly and Séni Kouanda; methodology: Abou Coulibaly and Séni Kouanda; supervision of data collection: Abou Coulibaly and Armel Emmanuel Sogo; validation: Abou Coulibaly and Armel Emmanuel Sogo; formal analysis: Abou Coulibaly and Seni Kouanda; writing-original draft preparation: Abou Coulibaly; writing-review and editing: Nutsa Chikvaidze, Mouna Al Amine, Cecilia Capello, Tsion Gerbaba, and Seni Kouanda; project administration: Mouna Al Amine, Cecilia Capello and Seni Kouanda. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The Burkina Faso Health Research Ethics Committee approved the research protocol for this trial under approval number 2020-3-051. The study was conducted in accordance with the principles of the Declaration of Helsinki. The scope, objectives, and advantages of the study were thoroughly communicated to those invited to participate. Adult participants (at least 18 years old) were included after obtaining their informed consent. Minor participants were included not only after obtaining their assent but also parental consent. The interviewers assigned to the various health centres were responsible for obtaining consent. This process was carefully monitored under the supervision of a field research team. The collected information was kept confidential and used solely for research purposes. None of the questionnaires in the database contained information that could be used to identify a woman formally.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Enfants du Monde Suisse, Rue de Varembé 1, 1202 Geneva, Switzerland.
Guarantor: Abou Coulibaly.
Trial registration: The trial was registered with the Pan-African Clinical Trials Registry under PACTR202009861550402 on 21/09/2020.
ORCID iD: Abou Coulibaly https://orcid.org/0000-0001-6015-3824
Supplemental material: Supplemental material for this article is available online.
References
- 1.Benova L, Tunçalp Ö, Moran AC, et al. Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries. BMJ Glob Health 2018; 3: e000779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arsenault C, Jordan K, Lee D, et al. Equity in antenatal care quality: an analysis of 91 national household surveys. Lancet Glob Health 2018; 6: e1186–e1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arroyave L, Saad GE, Victora CG, et al. Inequalities in antenatal care coverage and quality: an analysis from 63 low and middle-income countries using the ANCq content-qualified coverage indicator. Int J Equity Health 2021; 20: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institut national de la statistique et de la démographie, ICF TD. Burkina Faso Enquête Démographique et de Santé 2021. Ouagadougou, Burkina Faso, https://dhsprogram.com/publications/publication-FR378-DHS-Final-Reports.cfm (15 August 2023, accessed 2 September 2024).
- 5.UNICEF. Burkina Faso (BFA) - Demographics, health & infant mortality. UNICEF DATA, https://data.unicef.org/country/bfa/ (accessed 2 June 2022).
- 6.Nikiema L, Kameli Y, Capon G, et al. Quality of antenatal care and obstetrical coverage in rural Burkina Faso. J Health Popul Nutr 2010; 28: 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khatri RB, Mengistu TS, Assefa Y. Input, process, and output factors contributing to quality of antenatal care services: a scoping review of evidence. BMC Pregnancy Childbirth 2022; 22: 977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Conrad P, Schmid G, Tientrebeogo J, et al. Compliance with focused antenatal care services: do health workers in rural Burkina Faso, Uganda and Tanzania perform all ANC procedures? Trop Med Int Health 2012; 17: 300–307. [DOI] [PubMed] [Google Scholar]
- 9.Manithip C, Edin K, Sihavong A, et al. Poor quality of antenatal care services–is lack of competence and support the reason? An observational and interview study in rural areas of Lao PDR. Midwifery 2013; 29: 195–202. [DOI] [PubMed] [Google Scholar]
- 10.Phommachanh S, Essink DR, Wright EP, et al. Do health care providers give sufficient information and good counseling during ante-natal care in Lao PDR?: an observational study. BMC Health Serv Res 2019; 19: 449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tiembré I, Bi JVB, Aké-Tano O, et al. Evaluation of the quality of prenatal consultations in the health district of Grand Bassam, Côte d’Ivoire. Sante Publique 2010; 22: 221–228. [PubMed] [Google Scholar]
- 12.Ejigu T, Woldie M, Kifle Y. Quality of antenatal care services at public health facilities of Bahir-Dar special zone, Northwest Ethiopia. BMC Health Serv Res 2013; 13: 443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katemba BM, Bwembya P, Hamoonga TE, et al. Demand side factors associated with quality antenatal care services: a case study of Lusaka district, Zambia. Front Public Health 2018; 6: 285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leslie HH, Sun Z, Kruk ME. Association between infrastructure and observed quality of care in 4 healthcare services: a cross-sectional study of 4,300 facilities in 8 countries. PLoS Med 2017; 14: e1002464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jo Y, Alland K, Ali H, et al. Antenatal care in rural Bangladesh: current state of costs, content and recommendations for effective service delivery. BMC Health Serv Res 2019; 19: 861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Obsa AK, Tegene Y, Gebretsadik A. Iron and folic acid supplementation compliance and associated factors among pregnant women attending antenatal clinic in Shalla district, Southwest Ethiopia: a cross-sectional study. J Nutr Metab 2021; 2021: 6655027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olorunsaiye CZ, Brunner Huber LR, Laditka SB, et al. Individual and community socioeconomic factors related to the quality of antenatal care: a multilevel analysis of West and Central Africa. Women Health 2021; 61: 15–26. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization, 2016. [PubMed] [Google Scholar]
- 19.Al-Shorbaji N. The world health assembly resolutions on eHealth: eHealth in support of universal health coverage. Methods Inf Med 2013; 52: 463–466. [PubMed] [Google Scholar]
- 20.Labrique AB, Vasudevan L, Kochi E, et al. Mhealth innovations as health system strengthening tools: 12 common applications and a visual framework. Glob Health Sci Pract 2013; 1: 160–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Terre des hommes. IeDA – A digital solution to save children’s lives, https://www.tdh.org/en/projects/ieda (accessed 7 October 2024).
- 22.Maïga A, Ogyu A, Millogo RM, et al. Use of a digital job-aid in improving antenatal clinical protocols and quality of care in rural primary-level health facilities in Burkina Faso: a quasi-experimental evaluation. BMJ Open 2023; 13: e074770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarrassat S, Lewis JJ, Some AS, et al. An integrated eDiagnosis approach (IeDA) versus standard IMCI for assessing and managing childhood illness in Burkina Faso: a stepped-wedge cluster randomised trial. BMC Health Serv Res 2021; 21: 354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blanchet K, Lewis JJ, Pozo-Martin F, et al. A mixed methods protocol to evaluate the effect and cost-effectiveness of an Integrated electronic Diagnosis Approach (IeDA) for the management of childhood illnesses at primary health facilities in Burkina Faso. Implement Sci 2016; 11: 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lund S, Nielsen BB, Hemed M, et al. Mobile phones improve antenatal care attendance in Zanzibar: a cluster randomized controlled trial. BMC Pregnancy Childbirth 2014; 14: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health 2014; 14: 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McNabb M, Chukwu E, Ojo O, et al. Assessment of the quality of antenatal care services provided by health workers using a mobile phone decision support application in northern Nigeria: a pre/post-intervention study. PLOS ONE 2015; 10: e0123940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Atnafu A, Otto K, Herbst CH. The role of mHealth intervention on maternal and child health service delivery: findings from a randomized controlled field trial in rural Ethiopia. Mhealth 2017; 3, 39–39. Epub ahead of print 14 September 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feroz A, Perveen S, Aftab W. Role of mHealth applications for improving antenatal and postnatal care in low and middle income countries: a systematic review. BMC Health Serv Res 2017; 17: 704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oliveira-Ciabati L, Vieira CS, Franzon ACA, et al. PRENACEL – a mHealth messaging system to complement antenatal care: a cluster randomized trial. Reprod Health 2017; 14: 146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen H, Chai Y, Dong L, et al. Effectiveness and appropriateness of mHealth interventions for maternal and child health: systematic review. JMIR Mhealth Uhealth 2018; 6: e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haddad SM, Souza RT, Cecatti JG. Mobile technology in health (mHealth) and antenatal care–searching for apps and available solutions: a systematic review. Int J Med Inf 2019; 127: 1–8. [DOI] [PubMed] [Google Scholar]
- 33.PANDA. PANDA, https://pandatelemedicine.wordpress.com/ (accessed 29 September 2021).
- 34.Panda – Applications sur Google Play, https://play.google.com/store/apps/details?id=com.pandaproject&hl=fr&gl=BF (accessed 19 May 2021).
- 35.Benski AC, Stancanelli G, Scaringella S, et al. Usability and feasibility of a mobile health system to provide comprehensive antenatal care in low-income countries: PANDA mHealth pilot study in Madagascar. J Telemed Telecare 2017; 23: 536–543. [DOI] [PubMed] [Google Scholar]
- 36.Ouédraogo AM, Compaoré R, Somé A, et al. Acceptabilité et satisfaction de l’utilisation du système pregnancy and newborn diagnostic assessment (PANDA) pour les soins prénatals au Burkina Faso. Pan Afr Med J 2020; 3: 361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adepoju IOO, Albersen BJA, De Brouwere V, et al. mHealth for clinical decision-making in sub-Saharan Africa: a scoping review. JMIR Mhealth Uhealth 2017; 5: e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coulibaly A, Kouanda S. Effects of the pregnancy and newborn diagnostic assessment (PANDA) app on antenatal care quality in Burkina Faso: protocol for a cluster randomized controlled trial. JMIR Res Protoc 2023; 12: e37136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.QGIS Development Team. QGIS geographic information system, https://qgis.org/ (accessed 7 September 2024).
- 40.Ministère de la santé du Burkina. Protocoles de santé de la reproduction. Ouagadougou, Burkina Faso: Ministère de la santé, 2010. [Google Scholar]
- 41.Baafi JV, Adjei MR, Gladzah AN, et al. Determinants of quality antenatal care in a Peri-Urban Hospital, Ghana: an application of the content and timing of care in pregnancy (CTP) tool. Asian J Pharm Clin Res 2019; 2: 75–84. [Google Scholar]
- 42.StataCorp. Stata Statistical Software: Release 18, https://www.stata.com/products/, 2023.
- 43.Fagbamigbe OS, Olaseinde OS, Bello OO, et al. A multilevel Bayesian Markov Chain Monte Carlo Poisson modelling of factors associated with components of antenatal care offered to pregnant women in Nigeria. BMC Health Serv Res 2023; 23: 728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Negash WD, Fetene SM, Shewarega ES, et al. Multilevel analysis of quality of antenatal care and associated factors among pregnant women in Ethiopia: a community based cross-sectional study. BMJ Open 2022; 12: e063426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hailu GA, Weret ZS, Adasho ZA, et al. Quality of antenatal care and associated factors in public health centers in Addis Ababa, Ethiopia, a cross-sectional study. PLoS One 2022; 17: e0269710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tadesse Berehe T, Modibia LM. Assessment of quality of antenatal care services and its determinant factors in public health facilities of Hossana Town, Hadiya Zone, Southern Ethiopia: a longitudinal study. Adv Public Health 2020; 2020: e5436324. [Google Scholar]
- 47.Kare AP, Gujo AB, Yote NY. Quality of antenatal care and associated factors among pregnant women attending government hospitals in Sidama region, Southern Ethiopia. SAGE Open Med 2021; 9: 20503121211058055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Duysburgh E, Williams A, Williams J, et al. Quality of antenatal and childbirth care in northern Ghana. BJOG 2014; 121: 117–126. [DOI] [PubMed] [Google Scholar]
- 49.Duysburgh E, Temmerman M, Yé M, et al. Quality of antenatal and childbirth care in rural health facilities in Burkina Faso, Ghana and Tanzania: an intervention study. Trop Med Int Health 2016; 21: 70–83. [DOI] [PubMed] [Google Scholar]
- 50.OMS | Les femmes enceintes doivent pouvoir bénéficier de soins adaptés au bon moment. WHO, http://www.who.int/mediacentre/news/releases/2016/antenatal-care-guidelines/fr/ (accessed 23 January 2018).
- 51.Venkateswaran M, Ghanem B, Abbas E, et al. A digital health registry with clinical decision support for improving quality of antenatal care in Palestine (eRegQual): a pragmatic, cluster-randomised, controlled, superiority trial. Lancet Digital Health 2022; 4: e126–e136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rahman MM, Abe SK, Rahman MS, et al. Maternal anemia and risk of adverse birth and health outcomes in low- and middle-income countries: systematic review and meta-analysis. Am J Clin Nutr 2016; 103: 495–504. [DOI] [PubMed] [Google Scholar]
- 53.Karami M, Chaleshgar M, Salari N, et al. Global prevalence of anemia in pregnant women: a comprehensive systematic review and meta-analysis. Matern Child Health J 2022; 26: 1473–1487. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076241298499 for Assessing the effectiveness of the Pregnancy And Newborn Diagnostic Assessment system on the quality of antenatal care in Burkina Faso: A cluster-randomised controlled trial by Abou Coulibaly, Armel Emmanuel Sogo, Nutsa Chikvaidze, Cecilia Capello, Tsion Kefene Gerbaba and Séni Kouanda in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241298499 for Assessing the effectiveness of the Pregnancy And Newborn Diagnostic Assessment system on the quality of antenatal care in Burkina Faso: A cluster-randomised controlled trial by Abou Coulibaly, Armel Emmanuel Sogo, Nutsa Chikvaidze, Cecilia Capello, Tsion Kefene Gerbaba and Séni Kouanda in DIGITAL HEALTH