Abstract
In addition to the viral envelope (Env) proteins, host cell-derived proteins have been reported to be present in human immunodeficiency virus and simian immunodeficiency virus (SIV) envelopes, and it has been postulated that they may play a role in infection. We investigated whether the incorporation of host cell proteins is affected by the structure and level of incorporation of viral Env proteins. To compare the cellular components incorporated into SIV particles and how this is influenced by the structure of the cytoplasmic domain, we compared SIV virions with full-length and truncated Env proteins. The levels of HLA-I and HLA-II molecules were found to be significantly (15- to 25-fold) higher in virions with full-length Env than in those with a truncated Env. Virions with a truncated Env were also found to be less susceptible to neutralization by specific antibodies against HLA-I or HLA-II proteins. We also compared the level of incorporation into SIV virions of a coexpressed heterologous viral glycoprotein, the influenza virus hemagglutinin (HA) protein. We found that SIV infection of cells expressing influenza virus HA resulted in the production of phenotypically mixed SIV virions containing influenza virus HA as well as SIV envelope proteins. The HA proteins were more effectively incorporated into virions with full-length Env than in virions with truncated Env. The phenotypically mixed particles with full-length Env, containing higher levels of HA, were sensitive to neutralization with anti-HA antibody, whereas virions with truncated Env proteins and containing lower levels of HA were more resistant to neutralization by anti-HA antibody. In contrast, SIV virions with truncated Env proteins were found to be highly sensitive to neutralization by antisera to SIV, whereas virions with full-length Env proteins were relatively resistant to neutralization. These results indicate that the cytoplasmic domain of SIV Env affects the incorporation of cellular as well as heterologous viral membrane proteins into the SIV envelope and may be an important determinant of the sensitivity of the virus to neutralizing antibodies.
A critical step during human or simian immunodeficiency virus (HIV or SIV) assembly is the incorporation of viral Env proteins into mature virions. In addition to the viral Env proteins, host cell-derived molecules have been demonstrated to be present on the viral surface (1, 2, 26), and it has been postulated that these proteins may play a role in viral infection (4, 7, 17, 31). Incorporation of HLA molecules by SIV also has significant immunologic effects. Macaques immunized with uninfected human cells were protected against challenge with SIV grown in human cells (33). It has been suggested that the selective incorporation of cellular antigens within retrovirus envelopes may affect host range and influence the course of the disease (22, 23). Incorporation of the intercellular adhesion molecule ICAM-1 into HIV type 1 (HIV-1) has been reported to increase the avidity of virus-cell attachment and enhance virus entry (30). However, it is still controversial whether the incorporation of cellular membrane proteins by retroviruses is selective or not (1, 5, 22–24, 30). Evidence indicates that during replication or release of human T-cell leukemia virus, the virions become preferentially associated with the Tac antigen (21). Other findings indicated that feline leukemia virus specifically incorporated host-derived FLA antigens (23). Evidence has been obtained for a selective incorporation of HLA-DR over other HLA proteins into HIV-1 virions (2). However, others have reported that uptake of cellular proteins by the viral envelope is nonselective and depends on the type of cells and level of expression of host and Nef proteins (1, 7).
SIVmac239 is pathogenic molecular clone of SIV that encodes a TM (transmembrane) protein of 41 kDa with a cytoplasmic domain of 164 amino acids. SIVmac239 efficiently infects macaque peripheral blood lymphocytes, but infection of the human T-cell line HUT78 results in low levels of virus production. Continued passage of this virus in HUT78 cells resulted in the appearance of a virus encoding a 28-kDa TM protein with a truncated cytoplasmic domain of 18 amino acids (20). Similar truncations have been observed in other SIV isolates that were passaged in human cell lines (9, 14, 19, 20). Truncation of the cytoplasmic domain of the SIV Env glycoprotein was found to increase Env incorporation into virus particles (16, 35, 36) and also to enhance the cell fusion activity of the Env protein (32).
Because of the reported differences in density and conformation of Env glycoproteins on surfaces of particles with truncated versus full-length Env proteins, we have investigated whether the incorporation of host cell proteins could also be affected by the structure and level of incorporation of Env proteins. To compare the cellular components incorporated into SIV particles and how this is influenced by the structure of the Env cytoplasmic tail, we used SIV virions with full-length or truncated Env proteins. We have also investigated the sensitivity of these virions to neutralization by antibodies to viral or cellular antigens.
MATERIALS AND METHODS
Cell culture, viruses, and plasmids.
The recombinant monkey cell line sMAGI was provided by the AIDS Research and Reference Reagent Program, Division of AIDS, National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIAID, NIH) (Rockville, Md.). sMAGI cells were maintained in Dulbecco's minimal essential medium (DMEM) supplemented with 10% fetal calf serum. Human cell line HUT78 was maintained in RPMI 1640 medium supplemented with 10% fetal calf serum. p239SpSp5′ and p239SpE3′ were provided by the AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH. The SIVmac239 provirus was regenerated by SphI digestion of p239SpSp5′ and p239SpE3′ (18, 29) and religation of a mixture of the two plasmids. SIVmac1A11 virus, which was produced by continued passage of infected HUT78 cells, was kindly provided by C. Miller. For preparation of virus stocks, virus-infected cell supernatants were precleared by low-speed centrifugation, filtered through a 0.45-μm-pore-size filter (Nalge Company), and used as stock, or they were pelleted by centrifugation for 2 h at 20,000 rpm in an SW28 tube, resuspended, frozen in aliquots at −80°C, and used as concentrated stock. The titer of the virus stock was quantitated by performing an endpoint dilution assay in a 96-well plate, using the HUT78 cells and testing by reverse transcriptase (RT) assay (11) or by sMAGI assay (8). Vesicular stomatitis virus (VSV) (Indiana strain) was grown in BHK-21 cells and titered by procedures previously described (25). Plasmid pCMV/H1 expressing the hemagglutinin (HA) protein from A/PR/8/34 (H1N1) influenza virus was kindly provided by Harriet Robinson (12).
Monoclonal antibodies, antisera, and plasma samples.
SIV-specific plasma samples from rhesus monkeys infected with SIVmac239, SIVmac239/17E, or SIVsmm9 were kindly provided by S. O'Neil; samples from monkeys infected with SIVmac251 were provided by P. Marx. Monoclonal antibodies against SIVmac p27 and SIVmac251 gp41 (KK15) were provided by the NIAID AIDS Research and Reference Reagent Program; antibodies against cellular proteins HLA-ABC and HLA-DR were obtained from Immunotech, and HLA-DR antibody (L-243) was obtained from the American Type Culture Collection. Rabbit anti-VSV and anti-influenza virus polyclonal antibodies were previously described (25). Mouse anti-A/PR/8/34 (H1N1) influenza virus was provided by Zhiyi Sha. Goat anti-rabbit and anti-mouse sera were obtained from Southern Biotechnology Associates, Inc., Birmingham, Ala.
DNA transfection and virus infection.
Infectious SIVmac239 DNA was transfected into HUT78 cells by a DEAE-dextran procedure (27); during a 1-month period of virus growth, we passaged the virus twice. For SIVmac1A11 infection, 107 cells were pelleted and diluted in 3 ml of complete RPMI 1640 medium containing approximately 104 infectious particles. After overnight incubation, the medium was replaced by fresh complete RPMI 1640. Virus replication was analyzed by measurement of RT activity in the culture supernatant (11). At appropriate times, the cell-free culture supernatant was used for purification of virus particles. During infection, fresh medium and 5 × 106 cells per 175-cm T flask were added to infected cells once per week. In some experiments we also used SIVmac239(t), which also was obtained initially by DNA transfection, then passaged five or nine times, and found to have a truncated Env TM protein. For transfection of cells with pCMV/H1, we used FuGENE 6 (Boehringer Mannheim) or Lipofectin (GibcoBRL) according to the protocol provided by the manufacturer or the calcium phosphate precipitation method (10). Plasmid pCMV/H1 (6 μg) was used to transfect 6 × 106 HUT78 cells. For 3-day infections, we used SIV at a multiplicity of infection (MOI) of 0.001 inoculated with DEAE-dextran at a final concentration of 15 μg/ml; after 2 h, an additional volume of complete DMEM was added.
Purification of virus particles.
For purification of virus particles, we used linear sucrose gradients (15 to 40% and 20 to 60%) in SW41 polyallomer tubes. Sucrose solutions were prepared in 10 mM Tris-HCl (pH 7.4)–0.1 mM phenylmethylsulfonyl fluoride. For removal of cell debris and vesicles from the samples, the culture medium was harvested, clarified by centrifugation at 3,500 for 20 min (HS-4 Sorvall), and then filtered through a 0.45-μm-pore-size filter (Nalge). The supernatant was pelleted by centrifugation for 2 h at 20,000 in an SW28 tube. Such pellets contained SIV proteins but also vesicles and debris. To further separate the virus particles, the pellet was suspended in 100 μl of phosphate-buffered saline (PBS), loaded on a 15 to 40% sucrose gradient, and then centrifuged for 50 min at 12,900 in an SW41 tube. The gradient was collected in three fractions: top (1 ml), middle (3.5 ml), and bottom (7 ml). The middle fraction containing virus particles (35) was diluted with PBS and pelleted for 1 h at 29,000 in an SW41 rotor. The pellet was suspended in 100 μl of PBS, loaded on a 20 to 60% sucrose gradient, and centrifuged for 18 h at 24,000 in an SW41 rotor. Four fractions were collected: top (3.5 ml), middle (2 ml), lower (3 ml), and bottom (3 ml). The bottom fraction was discarded. The lower fraction was diluted in PBS, pelleted by centrifugation for 1 h at 29,000 in an SW41 rotor, and analyzed.
Western blotting and radioimmunoprecipitation (RIP) analysis.
For Western blotting proteins of purified virus particles were separated on a 10% polyacrylamide gel, and transferred to a nitrocellulose filter (Bio-Rad). Filters were blocked for 16 h at 4°C with 5% nonfat dry milk and 10% bovine serum (HyClone) in PBS and incubated with an SIV-specific antiserum from an infected rhesus monkey as described above. After three washes with PBS-Tween 20 (0.05%), the filters were incubated with an anti-monkey immunoglobulin G (IgG)-peroxidase conjugate (Sigma) in PBS-Tween 20-milk. After three washes, bound peroxidase activity was revealed using an ECL (enhanced chemiluminescence) kit (Amersham Life Science).
For RIP analysis, SIVmac239- or SIVmac1A11-infected cells were radiolabeled with 50 μCi of [35S]cysteine/methionine per ml for 22 h; after labeling for 4 h, 4% dialyzed serum was added. Supernatants from samples were collected, and virus particles were purified. The samples were lysed in RIP buffer (0.15 M NaCl, 1% NP-40, 0.5% deoxycholate, 0.1% sodium dodecyl sulfate [SDS], 20 mM EDTA) with 1 mM phenylmethylsulfonyl fluoride and immunoprecipitated for 16 h with SIV-specific antisera from an infected rhesus monkey and protein A-agarose. The agarose beads were then washed, and the proteins were characterized by SDS-polyacrylamide gel electrophoresis (PAGE) (21).
Surface iodination.
Purified virus particles were iodinated by the Bolton-Hunter method as described by Thompson et al. (34), with modification. To 2 μl of a 0.2-mg/ml stock solution of sulfosuccinimidyl-3[4-hydroxyphenyl] propionate (sulfo-SHPP; Pierce), the following reagents were added sequentially: 2 μl of 125I (100 mCi/ml; Amersham), 10 μl of chloramine T (5-mg/ml stock solution in 0.5 M sodium phosphate [pH 7.5]), 100 μl of hydroxyphenylacetic (1 mg/ml in water), and 10 μl of sodium metabisulfate (12 mg/ml in 0.05 M sodium phosphate [pH 7.5]). This mixture was added to 500 μl of ice-cold purified virus in PBS, mixed, and incubated for 30 min at 4°C. The reaction was terminated by adding 5 μl of lysine (100 mg/ml in PBS). Samples were transferred to another tube containing 2× RIP lysis buffer including protease inhibitors (see above). The samples were immunoprecipitated with specific antibodies, and the proteins were characterized by SDS-PAGE and autoradiography.
Virus-binding ELISA.
A virus-binding enzyme-linked immunosorbent assay (ELISA) modified from that of Orentas and Hildreth (28) was used to quantitate the capture of SIV by anti-HA antibodies. Briefly, 96-well plates were coated overnight at 4°C with 0.75 μg of goat anti-rabbit IgG (Fc fragment specific) or rabbit anti-mouse IgG (Fc fragment specific) (Jackson Laboratory, West Grove, Pa.) per well in carbonate buffer (15 mM Na2CO3, 35 mM NaHCO3, 3 mM NaN3 [pH 9.6]). The plates were blocked for 1 h at 37°C with 200 μl of 3% BSA in PBS per well; then murine or rabbit antibodies against HA were added at a 1:50 dilution, murine antibodies against gp41 were added at a 1:20 dilution, and murine anti-HLA antibodies were added at 2 μg/well in DMEM containing 5% heat-inactivated newborn calf serum and 0.02% NaN3 (Sigma), and the mixture was incubated for 2.5 h at 37°C. This was followed by the addition of 100 μl (2 or 35 ng of p27) of purified virus in PBS. The virus was allowed to bind to the anti-HA antibodies overnight at 4°C. After six washes with RPMI 1640 to remove unbound virus, the bound virus was lysed with 250 μl of 1% Triton X-100 (Sigma) per well for 1 h at room temperature, and p27 was quantitated by ELISA (Immunotech) according to the protocol provided by the manufacturer. All experiments were run in duplicate. The results for the experimental groups were compared to the results for controls in which virus was exposed to secondary rabbit anti-mouse IgG or goat anti-rabbit IgG in the absence of anti-gp41, anti-HA, or anti-HLA antibody.
Neutralization assays.
Neutralization assays were performed on sMAGI cells (8). Briefly, sMAGI cells were added to a 96-well plate 24 h prior to infection. Antibody samples were diluted in complete DMEM to a final volume of 25 μl and added to an equal volume of virus stocks diluted in complete DMEM to 100 infectious particles per 25 μl. The virus-antibody mixture was incubated at 37°C for 1 h and then added to sMAGI cells with DEAE-dextran to a final concentration of 15 μg/ml. After 2 h of incubation, an additional 200 μl of complete DMEM was added. After 24 and 48 h, medium was replaced by complete DMEM containing 5 μM zidovudine (Sigma). Three days after infection, the medium was removed and the cells were fixed and stained as described by Chackerian et al. (8). Neutralization was scored by comparing the average ratio of the number of blue cells in infected wells without treatment with antibodies to the number in wells where virus was preincubated with antibodies.
Surface immunofluorescence.
To check cell surface expression of SIV Env or HA proteins, cells were washed two times with 3% BSA (Sigma) and incubated for 30 min at 4°C with anti-SIV or anti-HA (rabbit) antibody. After the cells were again washed with 3% bovine serum albumin (BSA), samples were incubated with anti-rabbit Ig-Texas red (Amersham) or anti-monkey IgG-fluorescein isothiocyanate conjugate (Sigma) for 30 min 4°C. After incubation, the cells were fixed by 3% paraformaldehyde and examined using a Nikon microscope.
Electron microscopy.
HUT78 cells infected with SIVmac239 or SIVmac1A11 were fixed with 1% glutaraldehyde in PBS, postfixed with osmium tetroxide, stained with tannic acid, and embedded for electron microscopy as described previously (35).
RESULTS
Incorporation of full-length and truncated Env into SIV particles.
We have compared the incorporation of Env proteins into SIVmac239 virions which contain a full-length TM protein and SIVmac1A11 virions which possess a truncated Env protein. SIVmac1A11 virions were found to be produced by HUT78 cells at a level about 30-fold higher than that of SIVmac239. Comparison of the distribution of SIVmac239 and SIVmac1A11 proteins showed that for both viruses, Gag was broadly distributed in sucrose gradients (Fig. 1). However, the amount of SIVmac1A11 Gag in the top fraction was about 14-fold higher than the amount of SIVmac239 Gag (Fig. 1, lanes 3 and 6). Env proteins were found in only the lower fractions (Fig. 1, lanes 1 and 4). We did not observe a significant difference in the levels of Env incorporation into SIVmac1A11 or SIVmac239 virions (Fig. 1, lanes 1 and 4), as indicated by the Env/Gag ratio. Therefore, both truncated Env and full-length Env were incorporated with high efficiency into SIV particles.
FIG. 1.
Analysis of proteins of released SIV particles. HUT78 cells were infected with SIVmac1A11 (lanes 1 to 3) or transfected with SIVmac239 proviral DNA (lanes 4 to 6), and released virus was purified in a 20 to 60% sucrose gradient as described in Materials and Methods. Three fractions, lower (lanes 1 and 4), middle (lanes 2 and 5), and top (lanes 3 and 6), were analyzed by SDS-PAGE and Western blotting using a polyclonal SIV antiserum. The amounts of proteins were quantitated by densitometer analysis (NIH Image version 1.54). SU, surface protein; TM(t), truncated TM protein.
To compare the morphologies of SIVmac239 and SIV-mac1A11 virions, we used electron microscopy. A more prominent layer of spikes was identified on SIVmac1A11 particles containing truncated Env (Fig. 2A) than on SIVmac239 particles containing full-length Env (Fig. 2B). These results are similar to those previously obtained for virus-like particles (VLPs) having truncated or full-length Env proteins (35). We suggest that this morphological difference may be due to changes in the conformation of the Env proteins.
FIG. 2.
Thin section of SIV particles. HUT78 cells producing SIVmac1A11 (A) or SIVmac239 (B) virions were fixed and embedded, and thin sections were stained with tannic acid to visualize envelope spikes. Original magnification, ×105,000.
Incorporation of cellular proteins into SIV particles.
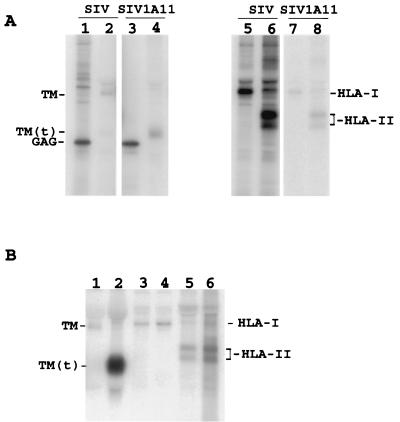
We compared the incorporation of HLA-I and HLA-II molecules in SIV virions by surface labeling with 125I. SIVmac1A11 or SIVmac239 virions with full-length or truncated Env proteins were purified, and similar amounts of particles (as estimated by core antigen ELISA) were labeled either by the membrane-permeable reagent SHPP-125I to analyze Gag proteins or by the surface-labeling reagent sulfo-SHPP-125I to analyze proteins on the viral surface (Fig. 3A). We observed labeling of the full-length TM protein in SIVmac239 (Fig. 3A, lane 2) and truncated TM in SIVmac1A11 (Fig. 3A, lane 4). The levels of TM proteins in the two samples were similar. We observed that much higher levels of HLA-I and HLA-II proteins were incorporated into SIVmac239: about a 25-fold-higher level of HLA proteins was observed in SIVmac239 (Fig. 3A, lane 5) compared with SIVmac1A11 (Fig. 3A, lane 7), and about a 15-fold-higher level of HLA-II proteins was found in SIVmac239 (Fig. 3A, lane 6) compared with SIVmac1A11 (Fig. 3A, lane 8).
FIG. 3.
Incorporation of HLA-I or HLA-II into SIV particles. HUT78 cells were infected with SIVmac239 (A, lanes 1, 2, 5, and 6; B, lanes 1, 3, and 5) or with SIVmac1A11 (A, lanes 3, 4, 7, and 8; B, lanes 2, 4, and 6). The culture medium was collected after 1 week of new passage, and viruses were purified in 20 to 60% (A) or 15 to 40% and 20 to 60% (B) sucrose gradients. The levels of p27 were estimated by core antigen ELISA (Immunotech); equivalent amounts of virions were used in all samples in panel A; the same amount of medium from equal amounts of cells was used for all samples in panel B. The proteins present were analyzed by SHPP-125I (A, lanes 1 and 3). The proteins present on the viral surface were labeled by sulfo-SHPP-125I (A, lanes 2, 4, and 5 to 8; B, all lanes) and immunoprecipitated with the following monoclonal antibodies: anti-p27 (A, lanes 1 and 3) anti-gp41 (A, lanes 2 and 4; B, lanes 1 and 2), anti-HLA-I (A, lanes 5 and 7; B, lanes 3 and 4), and anti-HLA-II (L-243) (A, lanes 6 and 8; B, lanes 5 and 6). The proteins were analyzed by SDS-PAGE (12% gel) and quantitated by densitometer analysis (NIH Image, version 1.54). TM(t), truncated TM protein.
When we used equal amounts of cells to prepare virus samples (Fig. 3B), the levels of Gag proteins determined by ELISA were found to be about 30-fold higher in the case of SIVmac1A11 compared to SIVmac239 (data not shown). The ratio of TM in SIVmac239 to TM in SIVmac1A11 was also about 1:30 (Fig. 3B, lanes 1 and 2). However, we observed that levels of HLA-I and HLA-II proteins in both of these samples were similar (Fig. 3B, lanes 3 to 6). Taken together, these results show that HLA-I and HLA-II proteins are present at about 15- to 25-fold-higher concentrations in SIVmac239 particles compared to SIVmac1A11 particles which have truncated Env proteins.
The determination of a physical association between cellular proteins and retrovirus particles can be complicated by the presence of cellular debris containing host proteins (6, 13). To control for such possible contamination, we carried out several experiments. First, we carried out virus purification using medium after culture of SIVmac239-transfected HUT78 cells for 3 or 11 weeks. Released virus as detected by RT assay was present only in the 11-week sample. SIV as well as host (HLA-I and HLA-II) proteins were found only in the samples obtained after 11 weeks, and were not detected after 3 weeks, providing evidence that cellular HLA proteins are not released in cellular components which cosediment with virions (not shown). In the second experiment, VSV particles were purified from VSV-infected HUT78 cells. We observed only VSV-specific proteins in these particles, which indicated that HLA proteins were not incorporated in detectable amounts into VSV virions and that such virions were not contaminated by cellular vesicles (not shown). As an additional experiment we used virus-binding ELISA to determine the profile of HLA molecules on the viral envelope. When we used equal amounts of virus particles with full-length or truncated Env, according to the estimated level of Gag proteins, similar amounts of intact virions were captured by anti-gp41 antibodies (not shown). HLA-II molecules were about threefold more abundant than HLA-I proteins in both SIVmac239 and SIVmac1A11 virions. These data are consistent with our observation that higher levels of HLA molecules are incorporated into SIVmac239 than SIVmac1A11.
Incorporation of heterologous viral glycoproteins into SIV particles.
To further test the hypothesis that the length of the cytoplasmic tail of the SIV Env protein can affect the incorporation of heterologous proteins into virus particles, HUT78 cells producing SIVmac239 or SIVmac1A11 virions were transfected with plasmid pCMV/H1 expressing the HA protein of A/PR/8/34 (H1N1) influenza virus. After 7 days, the medium from cells was collected, and phenotypically mixed SIV particles containing influenza virus HA proteins were purified and analyzed by surface iodination. We found the presence of the HA protein in samples of SIV particles with either full-length or truncated Env (not shown). To compare the incorporation of HA proteins into virions, we used a virus-binding ELISA. As shown in Fig. 4, SIVmac239 was captured efficiently by anti-HA (rabbit) and anti-HA (mouse) antibodies. The two antibodies had similar abilities to interact with virus. However, compared to SIVmac239 virus with full-length Env, SIVmac1A11 particles showed about a threefold reduction in binding to anti-HA antibody. No virus capture was observed in wells with no anti-HA (rabbit) or anti-HA (mouse) antibodies or in control wells containing vesicles or SIV prepared from cells not coexpressing HA proteins. These results show that mouse or rabbit antibody against HA proteins specifically recognized HA molecules associated with released SIVmac239 but were able to detect HA in SIVmac1A11 with much lower efficiency.
FIG. 4.
Capture of SIV virions in a virus-binding ELISA. The capture assay for phenotypically mixed SIV virions containing influenza virus HA proteins was performed as described in Materials and Methods. Antibody specificities, rabbit anti-HA [anti-HA(R)] and mouse anti-HA [anti-HA(M)]; controls, “omit” well coated with anti-mouse IgG or anti-rabbit IgG (only). Each well contained 35 ng of virus particles purified in a 20 to 60% sucrose gradient. For the virus-binding assay we used virus without HA with full-length Env and HA vesicles as negative controls. The assay was performed twice with similar results. Results are shown with the standard deviation (n = 3).
Sensitivity of SIV to neutralization by specific antibodies.
We initially examined whether the level of incorporation of HLA proteins into virions would influence the sensitivity of SIV to neutralization by anti-HLA antibodies. First, we found that anti-HLA-I and -II had a very limited neutralization effect. Only about 10% neutralization was observed after treating SIVmac239 virions with anti-HLA antibodies, and no neutralization by anti-HLA sera was detected with SIVmac1A11 (Fig. 5). We then determined whether treatment with secondary antibodies would enhance the neutralization effect. We found that secondary anti-mouse antibodies substantially increased the neutralization effect; when SIVmac239 virions were treated with anti-HLA-I plus anti-mouse serum, about 30% of the virus was neutralized, and 56% was neutralized after treatment with anti-HLA-II plus anti-mouse serum (Fig. 5). In contrast, with SIVmac1A11, no reduction in infectivity was observed after treatment with anti-HLA-I plus anti-mouse serum, and only about 10% reduction was found with anti-HLA-II plus anti-mouse serum (Fig. 5). We also used anti-VSV as an irrelevant antibody which did not have a neutralization effect on SIV virions. These results demonstrate that in contrast to SIV-mac239, SIVmac1A11 virions were almost completely resistant to the neutralization effect of anti-HLA antibodies.
FIG. 5.
Neutralization of SIV with anti-HLA. SIVmac239 with full-length Env ( ) or SIVmac1A11 with truncated Env (■) was incubated with anti-HLA-I or anti-HLA-II primary antibodies at 1:12 dilution and secondary anti-mouse antibodies (M) at 1:20 dilution before virus was added to sMAGI cells. Neutralization was scored by comparison of the number of blue cells in wells infected with antibody-treated virus to the number in wells infected with untreated virus. Results are shown with the standard deviation (n = 5).
) or SIVmac1A11 with truncated Env (■) was incubated with anti-HLA-I or anti-HLA-II primary antibodies at 1:12 dilution and secondary anti-mouse antibodies (M) at 1:20 dilution before virus was added to sMAGI cells. Neutralization was scored by comparison of the number of blue cells in wells infected with antibody-treated virus to the number in wells infected with untreated virus. Results are shown with the standard deviation (n = 5).
To extend these results, we also compared neutralization by anti-HA antibodies. In an attempt to increase incorporation of HA proteins into SIV particles and the sensitivity to neutralization, we infected HUT78 cells with SIVmac1A11 or SIV-mac239 at an MOI of 0.001; after a 2-h adsorption period, cells were transfected with plasmid pCMV/H1. Supernatants were collected after 3 days and used for neutralization assays. We observed that about 84% of SIVmac239 was neutralized after treatment with anti-HA serum (Fig. 6). In contrast, with SIVmac1A11, about 65% of infectivity was neutralized. Taken together, these results are consistent with the result that higher levels of cellular or heterologous viral proteins were incorporated into virus particles with full-length Env. Further, the HA protein is a more effective target for neutralization than the HLA proteins.
FIG. 6.
Neutralization of SIV with anti-HA antibodies. HUT78 cells were infected by SIVmac239 or SIVmac1A11 at an MOI of 0.001 for each virus and transfected with plasmid pCMV/H1 expressing the influenza virus HA gene. After 3 days, the media were collected and virions were incubated with anti-HA (mouse) antibodies at 1:20 dilution before virus was added to sMAGI cells. Neutralization was scored by comparison of the number of blue cells in wells infected with antibody-treated virus to the number in wells infected with virus treated with normal mouse serum (w/o Ab). Results are shown with the standard deviation (n = 3).
We also compared the abilities of antisera to SIV to neutralize the three viruses: SIVmac239 virions, which possess a full-length TM protein; SIVmac1A11, with a truncated TM protein; and SIVmac239(t) (five passages), with similar amounts of truncated and full-length TM proteins. We found that antisera to SIVmac239 almost completely neutralized SIVmac1A11 and neutralized 66% of SIVmac239(t) and about 60% of SIVmac239 (Fig. 7). We also compared the abilities of different anti-SIV antisera and found that anti-SIVmac239/17E and anti-SIVmac251 antisera had neutralization effects similar to those observed above with anti-SIVmac239 sera: SIVmac1A11 was highly sensitive to anti-SIV antibody, SIVmac239 was relatively resistant, and SIVmac239(t) had intermediate sensitivity. Anti-SIVsmm9 serum neutralized 27% of SIVmac239, 56% of SIVmac239(t), and 86% of SIVmac1A11. These results indicate that SIV with a truncated Env is more sensitive to neutralization by polyclonal antisera to various SIV isolates, whereas SIV having a full-length Env protein is relatively resistant to neutralization.
FIG. 7.
Differences in sensitivity of virus to neutralization with anti-SIV antibodies. SIVmac239 with full-length ( ) or truncated (
) or truncated ( ) Env and SIVmac1A11 (■) were incubated with anti-SIV antisera as described in Materials and Methods at 1:12 dilution and assayed as described for Fig. 6. Results are shown with the standard deviation (n = 3).
) Env and SIVmac1A11 (■) were incubated with anti-SIV antisera as described in Materials and Methods at 1:12 dilution and assayed as described for Fig. 6. Results are shown with the standard deviation (n = 3).
DISCUSSION
One goal of this study was to determine whether the incorporation of cellular membrane proteins into SIV virions is affected by the cytoplasmic domain of the Env proteins. Our results using surface iodination clearly indicated that the levels of HLA-I and HLA-II molecules were significantly (15- to 25-fold) lower in virions with truncated Env proteins than in those with full-length Env proteins. We extended these results by analysis of the incorporation of expressed influenza virus HA proteins into SIV particles and found that HA incorporation was also much lower in SIVmac1A11 virions with truncated Env than in SIVmac239 virions with full-length Env. These results indicate that the incorporation of cellular as well as heterologous viral proteins into virions or VLPs depends on the structure and level of incorporation of the SIV Env proteins. SIV virions with truncated Env proteins exhibit more clearly defined spikes on the viral envelope, and we suggest that they may be packed into a more regular arrangement in the virion which results in more effective exclusion of heterologous membrane proteins.
Our previous observations with recombinant VLPs revealed that glycoproteins with full-length cytoplasmic tails were incorporated into such particles at a much lower density than Env proteins containing truncated cytoplasmic domains (35). In contrast to truncated Env, increasing the expression level of full-length Env did not enhance incorporation of these proteins into VLPs. In the present study using SIV virions, we found that both forms of Env proteins are incorporated into virions at similar levels. These results point to possible differences between the assembly of SIV proteins expressed by recombinant expression vectors and assembly of virions during virus infection. It is possible that the higher level of expression obtained with vaccinia virus recombinants results in a more rapid assembly process and that truncated Env proteins are more efficiently incorporated into recombinant VLPs under these conditions.
We found that SIVmac239 virions with full-length Env could be partially neutralized by specific antibodies against HLA-I or HLA-II proteins, but SIVmac1A11 particles were almost completely resistant to neutralization by HLA antibodies. Neutralization of SIVmac239 and SIVmac1A11 was more effective when anti-HLA-II antibodies were used. This may be due to higher levels of incorporation of HLA-II than HLA-I proteins into virions. Anti-HLA-I and anti-HLA-II antibodies themselves had a very low neutralization activity with SIVmac239, but the addition of a secondary antibody was found to increase this effect. The mechanism of virus neutralization under these conditions could be due to the ability of the secondary antibody to bind to the virus and form virus aggregates. Phenotypically mixed SIVmac239 virions containing influenza virus HA proteins were partially neutralized with anti-HA antibody (without secondary antibody), whereas virions with truncated Env proteins were more resistant to neutralization. Previous studies reported that HLA proteins are weaker immunogens than influenza virus HA proteins (3), and this may contribute to differences in neutralization.
We also compared the susceptibilities to neutralization of SIV with full-length or truncated Env proteins by specific SIV antibodies. While both SIVmac1A11 and SIVmac239(t) with truncated Env proteins were susceptible to neutralization, SIVmac239 with a full-length Env protein was found to be more resistant to neutralization by SIV-specific antibodies. The high susceptibility of virions with truncated Env proteins to neutralization by anti-SIV antisera clearly demonstrates that the lack of neutralization of such particles by antisera to heterologous proteins reflects the reduced level of incorporation of such proteins into virions rather than insensitivity of the virions to neutralization per se. The low-level HA proteins in SIV virions may be able to function as targets for neutralization for two reasons: high neutralization activity of antibodies to HA (3) and space between full-length Env subunits in the SIV envelope. The neutralization of SIV depends on the tertiary structure of the Env protein (15). Previous studies (32) provided evidence that truncation of the SIV Env cytoplasmic tail changes the conformation of the external domain. Our electron microscopy studies support this result, in that a more prominent layer of spikes was seen in virions with truncated Env than in those containing full-length Env. The finding that SIVmac239 virions with full-length Env and those with truncated Env show differences in susceptibility to neutralization indicates that these differences result from the differences in the cytoplasmic tails of the Env protein. It will be of interest to determine the mechanism by which such changes affect sensitivity to neutralizing antibody and whether such differences could play a role in the differences in the pathogenic potential of SIV isolates.
ACKNOWLEDGMENTS
This study was supported by NIH grants AI 28147 and AI 45883 from NIAID, NIH.
We thank Frank Novembre for assistance with RT assays and use of his laboratory facility, Lawrence Melsen for assistance in preparing the figures, Tanya Cassingham for assistance in preparing the manuscript, and Dahnide Taylor for technical assistance.
REFERENCES
- 1.Akari H, Goto Y, Shinjo T. Detection of the cellular membrane proteins on human T cell leukemia virus type 1. Arch Virol. 1995;140:375–382. doi: 10.1007/BF01309871. [DOI] [PubMed] [Google Scholar]
- 2.Arthur L O, Bess J W, Sowder R C, Benveniste R E, Mann D L, Chermann J-C, Henderson L E. Cellular proteins bound to immunodeficiency virus: implications for pathogenesis and vaccines. Science. 1992;258:135. doi: 10.1126/science.1470916. [DOI] [PubMed] [Google Scholar]
- 3.Atassi M Z, Webster R G. Localization, synthesis, and activity of an antigenic site on influenza virus hemagglutinin. Proc Natl Acad Sci USA. 1983;80:840–844. doi: 10.1073/pnas.80.3.840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baskar P, Narayan O, McClure H M, Hildreth J E K. Simian immunodeficiency virus SIVsmmPBj 1.9 induces multinucleated giant cell formation in human peripheral blood monocytes. AIDS Res Hum Retroviruses. 1994;10:73–80. doi: 10.1089/aid.1994.10.73. [DOI] [PubMed] [Google Scholar]
- 5.Bastiani L, Suman L, Kim M, Zolla-Pazner S. Host cell-dependent alterations in envelope components of HIV type 1 virions. J Virol. 1997;71:3444–3450. doi: 10.1128/jvi.71.5.3444-3450.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bess J W J, Gorelick R J, Bosche W J, Henderson L E, Arthur L O. Microvesicles are a source of contaminating cellular proteins found in purified HIV-1 preparations. Virology. 1997;230:134–144. doi: 10.1006/viro.1997.8499. [DOI] [PubMed] [Google Scholar]
- 7.Cantin R, Fortin J F, Tremblay M. The amount of host HLA-DR proteins acquired by HIV-1 is virus strain- and cell type-specific. Virology. 1996;218:372–381. doi: 10.1006/viro.1996.0206. [DOI] [PubMed] [Google Scholar]
- 8.Chackerian B, Haigwood N L, Overbaugh J. Characterization of a CD4-expressing macaque cell line that can detect virus after a single replication cycle and can be infected by diverse simian immunodeficiency virus isolates. Virology. 1995;213:386–394. doi: 10.1006/viro.1995.0011. [DOI] [PubMed] [Google Scholar]
- 9.Chakrabarti L, Emerman M, Tiollais P, Sonigo P. The cytoplasmic domain of simian immunodeficiency virus transmembrane protein modulates infectivity. J Virol. 1989;63:4395–4403. doi: 10.1128/jvi.63.10.4395-4403.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen C, Okayama H. High-efficiency transformation of mammalian cells by plasmid DNA Mol. Cell Biol. 1987;7:2745–2752. doi: 10.1128/mcb.7.8.2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daniel M D, Letvin N L, King N W, Kannagi M, Sehgal P K, Hunt R D, Kanki P J, Essex M, Desrosiers R C. Isolation of a T-cell tropic HTLV-III-like retrovirus from macaques. Science. 1985;228:1201–1204. doi: 10.1126/science.3159089. [DOI] [PubMed] [Google Scholar]
- 12.Fynan E F, Webster R G, Fuller D H, Haynes J R, Santoro J A C, Robinson H L. DNA vaccines: protective immunization by parenteral, mucosal and gene-gun inoculations. Proc Natl Acad Sci USA. 1993;90:478–482. doi: 10.1073/pnas.90.24.11478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gluschankof P, Mondor I, Gelderblom H R, Sattentau Q J. Cell membrane vesicles are a major contaminant of gradient-enriched human immunodeficiency virus type-1 preparations. Virology. 1997;230:125–133. doi: 10.1006/viro.1997.8453. [DOI] [PubMed] [Google Scholar]
- 14.Hirsch V M, Edmondson P, Murphey-Corb M, Arbeille B, Johnson P R, Mullins J L. SIV adaption to human cells. Nature. 1989;341:573–574. doi: 10.1038/341573a0. [DOI] [PubMed] [Google Scholar]
- 15.Javaherian K, Langlois A J, Schmidt S, Kaufmann M, Cates N, Langedijk J P M, Meloen R H, Desrosiers R C, Burns D P, Bolognesi D P. The principal neutralization determinant of simian immunodeficiency virus differs from that of human immunodeficiency virus type 1. Proc Natl Acad Sci USA. 1992;89:1418–1422. doi: 10.1073/pnas.89.4.1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnston P B, Dubay J W, Hunter E. Truncations of the simian immunodeficiency virus transmembrane protein confer expanded virus host range by removing a block to virus entry into cells. J Virol. 1993;67:3077–3086. doi: 10.1128/jvi.67.6.3077-3086.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kannagi M, Kiyotaki M, King N W, Lord C I, Letvin N. Simian immunodeficiency virus induces expression of class II major histocompatibility complex structures on infected target cells in vitro. J Virol. 1987;61:1421–1426. doi: 10.1128/jvi.61.5.1421-1426.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kestler H W I, Naidu Y N, Kodama T, King N W, Daniel M D, Li Y, Desrosiers R C. Use of infectious molecular clones of simian immunodeficiency virus for pathogenesis studies. J Med Primatol. 1989;18:305–309. [PubMed] [Google Scholar]
- 19.Kodama T, Burns D P W, Kestler H W, Daniel M D, Desrosiers R C. Molecular changes associated with replication of simian immunodeficiency virus in human cells. J Med Primatol. 1990;19:431–437. [PubMed] [Google Scholar]
- 20.Kodama T, Wooley D P, Naidu Y M, Kestler H W, Daniel M D, Li Y, Desrosiers R C. Significance of premature stop codons in env of simian immunodeficiency virus. J Virol. 1989;63:4709–4714. doi: 10.1128/jvi.63.11.4709-4714.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laemmli U K. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970;277:680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- 22.Lando Z, Sarin P, Megson M, Greene W C, Waldman T A, Gallo R C, Broder S. Association of human T-cell leukemia/lymphoma virus with the Tac antigen marker for human T-cell growth factor receptor. Nature. 1983;305:733–736. doi: 10.1038/305733a0. [DOI] [PubMed] [Google Scholar]
- 23.Lee T H, Essex M, De Noronha F, Azocar J. Neutralization of feline leukemia virus with feline antisera to leukocyte alloantigens. Cancer Res. 1982;42:3995. [PubMed] [Google Scholar]
- 24.Le Gall S, Prevost M C, Heard J M, Schwartz O. Human immunodeficiency virus type I Nef independently affects virion incorporation of major histocompatibility complex class I molecules and virus infectivity. Virology. 1997;229:295–301. doi: 10.1006/viro.1996.8417. [DOI] [PubMed] [Google Scholar]
- 25.Lydy S L, Basak S, Compans R W. Host cell-dependent lateral mobility of viral glycoproteins. Microb Pathog. 1990;9:375–386. doi: 10.1016/0882-4010(90)90056-v. [DOI] [PubMed] [Google Scholar]
- 26.Meerloo T, Sheikh M A, Bloem A C, de Ronde A, Schutten M, van Els C A C, Roholl P J M, Joling P, Goudsmit J, Schuurman H-J. Host cell membrane proteins on human immunodeficiency virus type 1 after in vitro infection of H9 cells and blood mononuclear cells. An immuno-electron microscopic study. J Gen Virol. 1993;74:129–135. doi: 10.1099/0022-1317-74-1-129. [DOI] [PubMed] [Google Scholar]
- 27.Naidu Y M, Kestler H W, Li Y, Butler C V, Silva D P, Schmidt D K, Troup C D, Sehgal P K, Sonigo P, Daniel M D, Desrosiers R C. Characterization of infectious molecular clones of simian immunodeficiency virus (SIVmac) and human immunodeficiency virus type 2: persistent infection of rhesus monkeys with molecularly cloned SIVmac. J Virol. 1988;62:4691–4696. doi: 10.1128/jvi.62.12.4691-4696.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Orentas R J, Hildreth J E K. Association of host cell surface adhesion receptors and other membrane proteins with HIV and SIV. AIDS Res Hum Retroviruses. 1993;9:1157–1165. doi: 10.1089/aid.1993.9.1157. [DOI] [PubMed] [Google Scholar]
- 29.Regier D A, Desrosiers R C. The complete nucleotide sequence of a pathogenic molecular clone of simian immunodeficiency virus. AIDS Res Hum Retroviruses. 1990;6:1221–1231. doi: 10.1089/aid.1990.6.1221. [DOI] [PubMed] [Google Scholar]
- 30.Rizzuto C D, Sodroski J G. Contribution of virion ICAM-1 to human immunodeficiency virus infectivity and sensitivity to neutralization. J Virol. 1997;71:4847–4851. doi: 10.1128/jvi.71.6.4847-4851.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saarloos M N, Sullivan B L, Czerniewski M A, Parameswar K D, Spear G T. Detection of HLA-DR associated with monocytotropic, primary, and plasma isolates of human immunodeficiency virus type 1. J Virol. 1997;71:1640–1643. doi: 10.1128/jvi.71.2.1640-1643.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spies C P, Ritter G D, Jr, Mulligan M J, Compans R W. Truncation of the cytoplasmic domain of the simian immunodeficiency virus envelope glycoprotein alters conformation of the external domain. J Virol. 1994;68:585–591. doi: 10.1128/jvi.68.2.585-591.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stott E J. Anti-cell antibody in macaques. Nature. 1992;355:393. doi: 10.1038/353393a0. [DOI] [PubMed] [Google Scholar]
- 34.Thompson J A, Lau A L, Cunningham D D. Selective radiolabeling of cell surface proteins to a high specific activity. Biochemistry. 1987;26:743–750. doi: 10.1021/bi00377a014. [DOI] [PubMed] [Google Scholar]
- 35.Vzorov A N, Compans R W. Assembly and release of SIV env proteins with full-length or truncated cytoplasmic domains. Virology. 1996;221:22–33. doi: 10.1006/viro.1996.0349. [DOI] [PubMed] [Google Scholar]
- 36.Zingler K, Littman D R. Truncation of the cytoplasmic domain of the simian immunodeficiency virus envelope glycoprotein increases Env incorporation into particles and fusogenicity and infectivity. J Virol. 1993;67:2824–2831. doi: 10.1128/jvi.67.5.2824-2831.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]