Abstract
Background:
Measures such as the Patient Acceptable Symptom State and minimum clinically important difference have been used to contextualize patient-reported outcomes (PROs). Assessment of patients’ perception of being “completely better” (CB) after hip arthroscopy has not been studied.
Purposes:
To (1) determine the prevalence and characteristics of patients who report being CB at 2 years after hip arthroscopy; (2) determine whether PROs measuring function, pain, and mental health are associated with CB status; and (3) determine threshold values for PROs predictive of achieving CB status.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
Patients undergoing hip arthroscopy at a single institution from October 2015 to January 2020 were administered electronic surveys assessing sociodemographic variables and PROs at baseline and 2 years postoperatively. The CB anchor question was “Is the condition for which you underwent surgery completely better now?” Threshold values for PROs associated with achieving CB status at 2 years postoperatively were identified with 90% specificity. Variables with an area under the curve of >0.80 on a receiver operating characteristic curve were selected for multivariate analysis.
Results:
Overall, 29 of 62 patients (47%) achieved CB status. There were no differences in age, sex, body mass index, race, prior hip surgery, preoperative opioid use, smoking status, or preoperative expectations between the CB and no-CB groups. The CB group had better 2-year postoperative and pre- to postoperative change values on all PROs (P < .05 for all) except for the Patient-Reported Outcomes Measurement Information System (PROMIS)–Depression and the Numeric Pain Scale (NPS) for whole-body pain. Two-year postoperative PRO thresholds for achieving CB status were determined as PROMIS–Physical Function (PF) ≥51.3 or increase in PROMIS–PF ≥12 points, PROMIS–Pain Interference ≤46.6 or decrease in PROMIS–Pain Interference ≥12.2 points, NPS for operative hip pain of ≤1.0, Musculoskeletal Outcomes Data Evaluation and Management System–expectations met ≥95.0, and Surgical Satisfaction Questionnaire (SSQ-8) ≥87.5. Multivariate analysis demonstrated that higher SSQ-8 score and greater improvement on the PROMIS–PF were independent predictors of achieving CB status.
Conclusion:
Almost half of the study patients perceived being CB at 2 years after hip arthroscopy. Multiple postoperative PROs scores were associated with achieving CB status.
Keywords: hip arthroscopy, femoroacetabular impingement, hip/pelvis/thigh, clinical assessment/grading scale, patient-reported outcomes
The prevalence of hip arthroscopy has grown in recent years as a result of increased understanding of hip pathologies and improvements in operative techniques and training. Femoroacetabular impingement (FAI) syndrome has become the primary indication for hip arthroscopy, as it causes hip pain and functional deficits and can potentially lead to osteoarthritis.8,10,21 Hip arthroscopy is also indicated as both a diagnostic and therapeutic tool for a variety of pathologies including labral tears, loose bodies, and microinstability, among many other conditions.17,31 Hip arthroscopy has shown improved outcomes compared with nonoperative measures and provides a lesser risk of complications compared with open procedures without compromising postoperative results.11,19,28,29,38
As hip arthroscopy indications and surgical techniques evolve, it is important to remain focused on measuring the benefits to patients. Patient-reported outcomes (PROs) are a powerful way to interpret surgical outcomes, focusing on specific factors such as quality of life, pain, and function. PROs in isolation do not aid in clinical decision-making and must be interpreted to be used in clinical practice. Therefore, contextualizing PROs can help to differentiate meaningful clinical outcomes. Minimal clinically important difference (MCID), Patient Acceptable Symptom State (PASS), and substantial clinical benefit (SCB) are anchor-based methods of determining thresholds for meaningful improvements,13,37 but the ultimate patient-centered outcome measure may be the patient's perception of resolution of the symptoms or condition for which he or she is being treated. Recently, a patient-perceived “completely better” (CB) status has been used to contextualize PROs to differentiate clinically meaningful outcomes after anterior cruciate ligament surgery. 34 Assessment of patients’ perception of being CB after hip arthroscopy has not been studied and may be of particular value for this rapidly growing field.
The purpose of this study was to (1) determine the prevalence and characteristics of patients who report being CB at 2 years after hip arthroscopy; (2) determine whether PROs measuring function, pain, and mental health are associated with achieving CB status; and (3) determine threshold values for PROs predictive of achieving CB status. We hypothesized that PRO thresholds could be established to predict CB status with approximately 90% specificity.
Methods
This was a level 3 case-control study of patients who underwent hip arthroscopy at a single institution between October 2015 and January 2020. Patients were identified in preoperative or clinic sites and enrolled into an institutional review board–approved, prospective, web-based registry. 15 All surgeries were performed by 2 board-certified sports medicine fellowship–trained orthopaedic surgeons (including S.J.M.), both of whom routinely performed hip arthroscopy. Similar postoperative rehabilitation protocols were used by both surgeons. Current Procedural Terminology (CPT) codes were used to identify patients who underwent hip arthroscopy. Patients with a primary CPT code of 29914, 29915, 29916, or 29862 were included. Excluded were (1) patients <12 years of age, (2) non-English speakers, (3) incarcerated patients, and (4) patients lacking a working email address. Survey data were collected within 1 week of surgery and 2 years postoperatively using Research Electronic Data Capture (REDCap). 14
Of the 92 eligible patients who filled out baseline questionnaires, 62 patients (67%) were included in the analysis. At the postoperative evaluation, these patients were asked the CB anchor question “Is the condition for which you underwent surgery completely better now?” Of these patients, 29 (47%) responded yes (CB group) and 33 (53%) responded no (no-CB group) (Figure 1).
Figure 1.
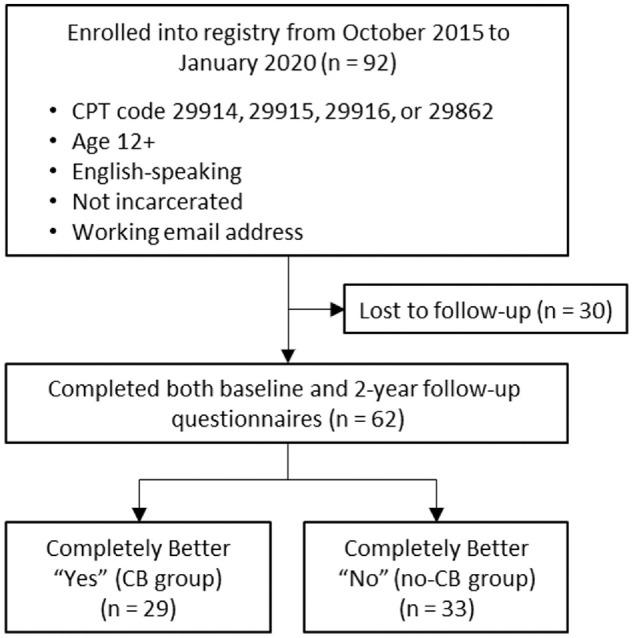
CONSORT (Consolidated Standards of Reporting Trials) flowchart illustrating the patient inclusion process. CB, completely better; CPT, Current Procedural Terminology.
Data Collection
Participant sociodemographic information was self-reported preoperatively through an electronic survey system. Operative and medical history information were gathered through a review of the patients’ electronic medical records. PROs were administered preoperatively and at 2 years postoperatively and included the Patient-Reported Outcomes Measurement Information System (PROMIS) 6 in 6 domains (Physical Function [PF], Pain Interference [PI], Social Satisfaction [SS], Fatigue, Anxiety, and Depression); the Numeric Pain Scale (NPS)9,18 for both the entire body and the operative hip; the Marx activity rating scale; 24 the Tegner activity scale; 3 and the Musculoskeletal Outcomes Data Evaluation and Management System (MODEMS) expectations domain. 33 Patient satisfaction was assessed at 2 years postoperatively with the Surgical Satisfaction Questionnaire (SSQ-8). 12 These measures comprise the standard set of outcomes assessed in the institutional registry and were selected to provide a comprehensive assessment of PROs and satisfaction with surgical treatment across a diverse set of patients. 15
PROMIS utilizes computer-adaptive testing, a validated method to decrease survey burden and administration time by adjusting questions asked based on the previous question's answer. 4 All PROMIS domains are scored on a 100-point scale, in which 50 represents the mean for the population. Higher numeric scores indicate better outcomes on the PF and SS domains and worse outcomes on the Fatigue, PI, Anxiety, and Depression domains. The Marx scale assesses the greatest level of patient physical activity over the past year, and the Tegner scale determines activity level before and after an injury.3,24 The raw Marx score was converted to a 100-point scale, with 100 indicating the highest activity level. The MODEMS and SSQ-8 were utilized to assess expectations before and after surgery and satisfaction after surgery, respectively.12,33
Statistical Analysis
Responses to the CB anchor question (yes or no) were analyzed with respect to patient characteristics to identify potential confounders. Associations with PROs were assessed with bivariate analysis. PRO score thresholds for responding yes to the CB anchor question were calculated via a receiver operating characteristic (ROC) curve, with values chosen as thresholds at approximately 90% specificity. ROC curves were tested for reliability through an area under the curve (AUC) analysis, with AUCs of 0.7 and 0.8 deemed acceptable and excellent, respectively. 22
Continuous data were reported as mean and standard deviation while categorical data were reported as frequency and percentage. A goodness-of-fit test was run assessing for normality among both preoperative and postoperative PROs, and a majority did not fit normal distributions, justifying nonparametric analyses. Continuous and categorical data were analyzed via the Wilcoxon rank-sum test or Pearson chi-square test, respectively. The Fisher exact test was utilized for categorical variables with cell counts of <5. Associations between 2 continuous variables were analyzed through the Spearman correlation coefficient. Backward stepwise elimination regression for maximal validation R2 was applied to identify independent predictors of CB status. Variables were selected a posteriori for inclusion into the multivariate based on an AUC of >0.80. Statistical significance was determined when P < .05, with all tests being 2-sided. All statistical analyses were performed using JMP Pro (Version 13; SAS Institute).
Results
The median time to follow-up was 25.2 months (IQR, 24-28 months). When stratifying patient characteristics by CB status, significantly more patients with single marital status were seen in the CB group than the no-CB group (P = .04). There were no other significant differences observed between groups, including age, sex, body mass index (BMI), race, prior ipsilateral hip surgery, preoperative opioid use, or smoking status (Table 1). Additionally, there was no difference in the proportion of patients who achieved CB status based on primary CPT code (P = .26).
Table 1.
Comparison of Patient Characteristics and Medical Background by CB Status a
| Variable | Overall (N = 62) | CB (n = 29) | No CB (n = 33) | P | Variable | Overall (N = 62) | CB (n = 29) | No CB (n = 33) | P |
|---|---|---|---|---|---|---|---|---|---|
| Age | 39.6 ± 12.4 | 39 ± 10.8 | 40.2 ± 13.8 | .79 | Surgical history | ||||
| BMI | 27.4 ± 5.4 | 27 ± 4.9 | 27.8 ± 5.8 | .55 | Prior ipsilateral hip surgery | 0.1 ± 0.4 | 0.2 ± 0.5 | 0.1 ± 0.3 | .60 |
| Sex | .23 | Orthopaedic procedures | 1.3 ± 2.6 | 0.9 ± 1.1 | 1.7 ± 3.4 | .93 | |||
| Male | 13 (21) | 4 (13.8) | 9 (27.3) | Any surgery | 3.2 ± 3.7 | 3.1 ± 3.1 | 3.3 ± 4.3 | .80 | |
| Female | 49 (79) | 25 (86.2) | 24 (72.7) | Prior ipsilateral hip surgery | .70 | ||||
| Race | .15 | No | 53 (85.5) | 25 (86.2) | 28 (84.8) | ||||
| Asian | 2 (3.2) | 1 (3.4) | 1 (3.0) | Yes | 7 (11.3) | 4 (13.8) | 3 (9.1) | ||
| Black | 4 (6.5) | 0 (0.0) | 4 (12.1) | Charlson Comorbidity Index | 0.8 ± 1.1 | 0.8 ± 1.1 | 0.8 ± 1.0 | .81 | |
| White | 56 (90.3) | 28 (96.6) | 28 (84.8) | History of depression/anxiety | .68 | ||||
| Other | 0 (0.0) | 0 (0.0) | 0 (0.0) | No | 34 (54.8) | 18 (62.1) | 16 (48.5) | ||
| Ethnicity | ≥.99 | Yes | 13 (20.9) | 6 (20.7) | 7 (21.2) | ||||
| Hispanic/Latino | 2 (3.2) | 1 (3.4) | 1 (3.0) | ASA physical status score | .57 | ||||
| Not Hispanic/Latino | 59 (95.2) | 28 (96.6) | 31 (93.9) | I | 23 (37.1) | 12 (41.4) | 11 (34.3) | ||
| Education level | .46 | II | 37 (59.7) | 17 (58.6) | 20 (60.6) | ||||
| College education | 47 (75.8) | 23 (79.3) | 24 (72.7) | III | 1 (1.6) | 0 (0.0) | 1 (3.0) | ||
| High school graduate | 4 (6.5) | 2 (6.9) | 2 (6.1) | Preoperative opioid use | .74 | ||||
| Less than high school | 5 (8.1) | 1 (3.4) | 4 (12.1) | No | 51 (82.3) | 23 (79.3) | 28 (84.8) | ||
| Marital status | .04 | Yes | 11 (17.7) | 6 (20.7) | 5 (15.2) | ||||
| Single | 30 (48.4) | 18 (62.1) | 12 (36.4) | Smoking status | .39 | ||||
| Married or domestic | 27 (43.5) | 9 (30.1) | 18 (54.5) | Daily | 5 (8.1) | 1 (3.4) | 4 (12.1) | ||
| Live with caretaker | .34 | Never | 45 (72.6) | 22 (75.9) | 23 (69.7) | ||||
| No | 4 (6.5) | 3 (10.3) | 1 (3.0) | Quit | 5 (8.1) | 3 (10.3) | 2 (6.1) | ||
| Yes | 53 (85.5) | 24 (82.8) | 29 (87.9) | Alcohol intake | .12 | ||||
| Employment status | .29 | ≤4 times/month | 26 (41.9) | 9 (31.0) | 17 (51.5) | ||||
| Employed/Retired | 41 (66.1) | 20 (73.4) | 21 (63.4) | >4 times/month | 20 (32.3) | 13 (44.8) | 7 (21.2) | ||
| Student | 9 (14.5) | 3 (10.3) | 6 (18.2) | Never | 10 (16.1) | 5 (17.2) | 5 (15.2) | ||
| Unable to work | 1 (1.6) | 0 (0.0) | 1 (3.0) | Recreational drug use | ≥.99 | ||||
| Unemployed | 5 (8.1) | 4 (13.8) | 1 (3.0) | No | 55 (88.7) | 26 (89.7) | 29 (87.9) | ||
| Annual income | .46 | Yes | 2 (3.2) | 1 (3.4) | 1 (3.0) | ||||
| >$70,000 | 32 (51.6) | 15 (51.7) | 17 (51.5) | Legal claim filed? | .49 | ||||
| <$70,000 | 21 (33.9) | 12 (41.4) | 9 (27.3) | No | 55 (88.7) | 27 (93.1) | 28 (84.8) | ||
| Insurance | .92 | Yes | 2 (3.2) | 0 (0.0) | 2 (6.1) | ||||
| Government | 11 (17.7) | 5 (17.2) | 6 (18.2) | ||||||
| Private | 51 (82.3) | 24 (82.8) | 27 (81.8) |
Data are presented as mean ± SD or n (%). Boldface P value indicates statistically significant difference between the CB and no-CB groups (P < .05). ASA, American Society of Anesthesiologists; BMI, body mass index; CB, completely better.
Patient-Reported Outcomes
Patients in both the CB and no-CB groups saw pre- to postoperative improvement on all PROs with the exception of NPS–whole body and PROMIS-Depression (Table 2). Additionally, patients in the no-CB group saw no pre- to postoperative improvement on the Marx and Tegner scores. There were no differences in preoperative PROs or MODEMS–preoperative expectations between the CB and no-CB groups (Table 2).
Table 2.
Comparison of Patient-Reported Outcome Scores by CB Status and Time Point a
| Outcome Measure | Overall (N = 62) | CB (n = 29) | No CB (n = 33) | P (CB vs No-CB) |
|---|---|---|---|---|
| PROMIS-PF | ||||
| Preop | 40.7 ± 5.3 | 39.7 ± 6.4 | 41.6 ± 4.0 | .29 |
| Postop | 50.7 ± 9.0 | 56.3 ± 8.5 | 45.7 ± 6.1 | <.0001 |
| Δ(postop-preop) | 9.9 ± 10.2 | 16.6 ± 9.9 | 4.1 ± 5.9 | <.0001 |
| P (preop vs postop) | — | <.0001 | <.0001 | |
| PROMIS-PI | ||||
| Preop | 61.0 ± 6.1 | 62.1 ± 6.5 | 60.0 ± 5.6 | .2 |
| Postop | 50.7 ± 8.8 | 44.8 ± 7.2 | 55.9 ± 6.7 | <.0001 |
| Δ(postop-preop) | −10.4 ± 10.8 | −17.2 ± 10.8 | −4.2 ± 6.2 | <.0001 |
| P (preop vs postop) | — | <.0001 | <.0001 | |
| PROMIS-Fatigue | ||||
| Preop | 53.3 ± 9.6 | 53.2 ± 10.1 | 53.3 ± 9.3 | .99 |
| Postop | 46.7 ± 9.6 | 42.6 ± 9.3 | 50.3 ± 8.4 | .001 |
| Δ(postop-preop) | −6.9 ± 9.3 | −11.0 ± 9.5 | −3.3 ± 7.6 | .002 |
| P (preop vs postop) | — | .0002 | .002 | |
| PROMIS-SS | ||||
| Preop | 42.1 ± 6.8 | 42.4 ± 7.0 | 41.9 ± 6.7 | .95 |
| Postop | 52.4 ± 11.2 | 57.9 ± 11.0 | 47.5 ± 8.9 | <.0001 |
| Δ(postop-preop) | 10.3 ± 12.3 | 15.5 ± 13.1 | 5.8 ± 9.7 | .002 |
| P (preop vs postop) | — | <.0001 | .001 | |
| PROMIS-Anxiety | ||||
| Preop | 55.5 ± 9.0 | 55.3 ± 9.2 | 55.6 ± 9.2 | .94 |
| Postop | 50.5 ± 9.7 | 47.2 ± 10.5 | 53.4 ± 8.0 | .01 |
| Δ(postop-preop) | 5.3 ± 10.0 | −8.7 ± 9.3 | −2.3 ± 9.6 | .009 |
| P (preop vs postop) | — | .002 | .009 | |
| PROMIS-Depression | ||||
| Preop | 50.6 ± 8.3 | 50.4 ± 8.5 | 50.9 ± 8.2 | .87 |
| Postop | 48.5 ± 9.5 | 46.5 ± 9.7 | 50.2 ± 9.1 | .1 |
| Δ(postop-preop) | −2.3 ± 8.4 | −3.8 ± 8.1 | −1.0 ± 8.5 | .25 |
| P (preop vs postop) | — | .13 | .25 | |
| NPS–operative hip | ||||
| Preop | 4.8 ± 2.5 | 4.4 ± 2.7 | 5.1 ± 2.3 | .34 |
| Postop | 2.7 ± 2.6 | 1.1 ± 1.6 | 4.1 ± 2.4 | <.0001 |
| Δ(postop-preop) | −1.9 ± 3.6 | −3.3 ± 8.1 | −0.9 ± 3.5 | .01 |
| P (preop vs postop) | — | <.0001 | .01 | |
| NPS–whole body | ||||
| Preop | 1.6 ± 2.0 | 1.5 ± 1.9 | 1.6 ± 2.2 | .89 |
| Postop | 2.4 ± 2.3 | 1.8 ± 1.5 | 3.0 ± 2.7 | .17 |
| Δ(postop-preop) | 0.9 ± 2.1 | 0.3 ± 2.3 | 1.3 ± 1.9 | .21 |
| P (preop vs postop) | — | .25 | .20 | |
| Marx score | ||||
| Preop | 42.4 ± 37.8 | 40.0 ± 36.3 | 44.5 ± 39.4 | .77 |
| Postop | 36.6 ± 31.0 | 44.4 ± 27.2 | 29.5 ± 32.8 | .02 |
| Tegner score | ||||
| Preop | 4.9 ± 2.6 | 4.2 ± 2.5 | 5.5 ± 2.6 | .11 |
| Postop | 4.3 ± 2.5 | 5.1 ± 2.3 | 3.6 ± 2.5 | .02 |
| MODEMS–preoperative expectations | 89.8 ± 13.8 | 90.1 ± 12.3 | 89.5 ± 15.2 | .79 |
| MODEMS–expectations met | 70.6 ± 27.5 | 87.6 ± 17.2 | 54.8 ± 25.9 | <.0001 |
| SSQ-8 | 76.8 ± 20.8 | 88.6 ± 15.3 | 66.5 ± 19.5 | <.0001 |
Data are presented as mean ± SD. Dashes indicate areas not applicable. Boldface P values indicate statistically significant difference between groups as indicated (P < .05). CB, completely better; PROMIS, Patient-Reported Outcomes Measurement Information System; MODEMS, Musculoskeletal Outcomes Data Evaluation and Management System; NPS, Numeric Pain Scale; PF, Physical Function; PI, Pain Interference; Postop, postoperative; Preop, preoperative; SS, Social Satisfaction; SSQ-8, Surgical Satisfaction Questionnaire.
Two-year postoperative PRO scores and pre- to postoperative change (Δ) in PRO scores were significantly better in the CB group for all PROs with the exception of the PROMIS-Depression and NPS–whole body (Table 2).
The 2-year postoperative and pre- to postoperative change score thresholds for predicting CB status with approximately 90% specificity were calculated for multiple PROs (Table 3). The postoperative and change score thresholds for PROMIS-PF and PROMIS-PI, as well as the postoperative NPS–operative hip score, MODEMS–expectations met, and SSQ-8, had excellent predictive value (AUCs: PROMIS-PF postoperative = 0.87, PROMIS-PF Δ = 0.86; PROMIS-PI postoperative = 0.85, PROMIS-PI Δ = 0.85; NPS–operative hip postoperative = 0.88; MODEMS–expectations met = 0.87; SSQ-8 = 0.86).
Table 3.
Patient-Reported Outcome Thresholds Predictive of Achieving CB Status at 2 Years Postoperatively a
| Measure | Threshold b | Sensitivity | Specificity | AUC |
|---|---|---|---|---|
| PROMIS-PF | ||||
| Postop | ≥51.3 | 0.69 | 0.91 | 0.87 |
| Δ(postop-preop) | ≥12.0 | 0.69 | 0.91 | 0.86 |
| PROMIS-PI | ||||
| Postop | ≤46.6 | 0.62 | 0.91 | 0.85 |
| Δ(postop-preop) | ≤–12.2 | 0.76 | 0.91 | 0.85 |
| PROMIS-Fatigue | ||||
| Postop | ≤37.8 | 0.31 | 0.91 | 0.74 |
| Δ(postop-preop) | ≤–13.1 | 0.43 | 0.91 | 0.73 |
| PROMIS-SS | ||||
| Postop | ≥60.0 | 0.48 | 0.91 | 0.79 |
| Δ(postop-preop) | ≥17.8 | 0.46 | 0.91 | 0.74 |
| PROMIS-Anxiety | ||||
| Postop | ≤40.9 | 0.31 | 0.91 | 0.69 |
| Δ(postop-preop) | ≤–16.1 | 0.25 | 0.91 | 0.79 |
| NPS–operative hip | ||||
| Postop | ≤1.0 | 0.79 | 0.84 | 0.88 |
| Marx | ||||
| Postop | ≥80.0 | 0.11 | 0.90 | 0.67 |
| Tegner | ||||
| Postop | ≥8.0 | 0.14 | 0.90 | 0.68 |
| MODEMS–expectations met | ≥95.0 | 0.62 | 0.90 | 0.87 |
| SSQ-8 | ≥87.5 | 0.66 | 0.91 | 0.86 |
Boldface values indicate an AUC of >0.80. AUC, area under the curve; CB, completely better; PF, Physical Function; PI, Pain Interference; Postop, postoperative; Preop, preoperative; PROMIS, Patient-Reported Outcomes Measurement Information System; MODEMS, Musculoskeletal Outcomes Data Evaluation and Management System; NPS, Numeric Pain Scale; SS, Social Satisfaction; SSQ-8, Surgical Satisfaction Questionnaire.
All threshold values were chosen with approximately 90% specificity.
Outcome score thresholds with excellent predictive value (ie, thresholds with AUC >0.80 in Table 3) were used in a multivariate analysis for predicting CB status. On logistic regression analysis, higher SSQ-8 scores and greater improvement from baseline in PROMIS PF scores were independent predictors of achieving CB status at 2 years postoperatively (Table 4).
Table 4.
Logistic Regression Model for Achieving CB Status at 2 Years Postoperatively a
| Estimate b | SE | P | |
|---|---|---|---|
| SSQ-8 | 0.08 | 0.029 | .004 |
| PROMIS-PF Δ(postop-preop) | 0.19 | 0.057 | .001 |
Boldface P values indicate statistical significance (P < .05). CB, completely better; PROMIS-PF, Patient-Reported Outcomes Measurement Information System–Physical Function; SSQ-8, Surgical Satisfaction Questionnaire.
Log odds of “yes” compared with “no” for CB status.
Discussion
To the best of our knowledge, this is the first study to evaluate patient-perceived CB status after hip arthroscopy. In this study, 47% of patients responded yes to the CB anchor question at 2 years after hip arthroscopy. There were no differences in patient characteristics, including age, sex, BMI, race, prior ipsilateral hip surgery, preoperative opioid use, or smoking status, between the CB and no-CB groups. Multiple PROs were shown to be significantly better in the CB group than the no-CB group, and threshold values for these PROs predictive of achieving CB status were identified. Multivariate analysis revealed that higher SSQ-8 score and greater pre-to postoperative improvement on the PROMIS–PF were independent predictors of CB status.
Measuring PROs has become the new standard for determining surgical quality and treatment efficacy, and as a result, multiple measures have been developed to allow for clinical interpretation of PROs.5,36 In other hip arthroscopy studies with MCID methodology, worse preoperative scores were associated with a higher likelihood of achieving MCID, but this may not equate to a satisfactory result for the patient.28,30 PASS has been shown to have a positive correlation with preoperative scores and patient factors.16,30,35 However, it is plausible that a patient who already has a higher level of function or less severe symptoms preoperatively will also feel better than other patients postoperatively, without achieving the desired improvement in function, decrease in symptoms, or outcome. There may be a difference between the acceptable symptom level and the symptoms or lack thereof when achieving CB status. For this reason, measuring CB status may be the ultimate patient-centered outcome for a younger, more active population. In this study, no preoperative PROs were predictive of achieving CB status. This may be due to variations in patients’ perception of feeling CB. One patient with lower preoperative PROs may see greater improvement postoperatively, which one considers to be CB, while at the same time, another patient with higher PROs may start off closer to complete resolution of the symptoms that one achieves postoperatively. Additionally, preoperative expectations did not predict CB status.
This study demonstrated that multiple postoperative PROs were correlated with CB status. At 2 years postoperatively, the PROMIS PF, PI, Fatigue, SS, and Anxiety domains were associated with achieving CB status. PROMIS-Depression was not associated with achieving CB status. NPS–operative hip, SSQ-8, and MODEMS were also associated with achieving CB status at 2 years. This is reassuring, as it is expected that better quantifiable scores would correlate with a positive patient outcome as measured by a subjective anchor question. This is also a useful research tool, as this study identified threshold values for 2-year postoperative and pre- to postoperative changes in PRO scores that are predictive of CB status. The PROMIS-PF and PROMIS-PI, NPS, MODEMS, and SSQ-8 at 2 years postoperative all had excellent predictive capability (AUCs >0.80) with a sensitivity of about 90%. In addition, an increase in the PROMIS-PF of ≥12 points and decrease in PROMIS-PI of ≥12.2 points also had excellent predictive capability. This allows for interpretation of other studies measuring these domains in the context of outcomes that may be comparable with CB status.
Recent studies have reported PRO values associated with SCB,23,27 which included a patient response of “a good deal better” or “a great deal better,” as opposed to CB. Bodendorfer et al 2 defined SCB thresholds at 1 year after hip arthroscopy for FAI syndrome, and their thresholds for PROMIS-PI (51.9) and PROMIS-PF (49.9) were similar to the values reported in this study (≤46.6 and ≥51.3, respectively). In this study, 47% of patients reported feeling CB. This is slightly lower than the percentage of patients achieving SCB threshold for PROMIS-PI (51.6%) and PROMIS-PF (54.0%) in the study by Bodendorfer et al, which aligns with the theory that CB status is the highest mark of achievement in outcomes. This study did not utilize a legacy hip-specific measure, such as International Hip Outcome Tool, modified Harris Hip Score, or Hip Outcome Score. However, there is psychometric evidence to support that PROMIS measures are accurate and responsive in assessing outcomes after hip arthroscopy, and correlate well with legacy hip-specific measures.7,20,23,26 Additionally, this study showed that a traditional NPS in the operative hip of ≤1.0 is associated with CB status, which is similar to the visual analog scale for pain threshold for SCB (1.5) as demonstrated by Beck et al. 1 Although CB status is a novel measurement tool, a recent study by Schneider et al 34 showed that 70% of patients reported being CB at 2 years after anterior cruciate ligament reconstruction, which serves as a good point of reference for a widely successful surgery. Our finding that SSQ-8 at 2 years postoperative and change in PROMIS-PF over 2 years were independently predictive of CB status suggests that surgical satisfaction and improvement in PF may be the most important metrics to patients when undergoing hip arthroscopy.
Last, patient and clinical characteristics were very similar between the CB and no-CB groups, with self-reported marital status being the only observed significant difference. The CB group had a higher proportion of patients who reported being single compared with the no-CB group. This could be due to age differences between these subgroups, as single patients were on average 10 years younger than married patients. However, there was no overall association observed between age and CB status when examined directly. There were otherwise no differences in demographics of sex, BMI, race, prior ipsilateral hip surgery, preoperative opioid use, smoking status, or annual income between the CB and no-CB groups, indicating that patients may feel CB at 2 years after hip arthroscopy regardless of these factors. Contrary to many orthopaedic studies demonstrating differences, hip arthroscopy patients may have a similar opportunity to achieve feeling CB, regardless of demographics or socioeconomic background.25,32,35
Limitations
This study has several limitations. First, CB status is a global subjective measure, and there may be additional patient factors, such as specific type of sport participation or prior procedure, that influence a particular response that were not included in this study. Second, CB status is a novel assessment that limits direct comparison with prior literature. However, MCID, PASS, and SCB have been investigated and can provide some context for interpretation. Third, the data were limited to a small and relatively homogeneous sample from 2 surgeons operating at a single urban center, which may limit the generalizability to other populations. Some factors (ie, race, legal claim, alcohol intake) might be found to be significant with a larger study population. Surgical techniques are rapidly evolving with new technology, and this may affect results over the time period of the study and in the future. Additionally, the inclusion of both adolescents and adults for a variety of arthroscopic indications into a single cohort may further limit the generalizability. Fourth, 30 patients (33%) did not respond, and therefore, the true rate of achieving CB in our population could be as high as 64% (59 of 92 patients in the best case that all patients who did not respond actually were CB), or as low as 32% (29 of 92 patients in the worst case that all patients who did not respond were not CB). Further work is needed to reproduce these results in a larger sample and to compare the results with other legacy hip-specific outcome measures. Despite these limitations, this study provides a novel analysis of multiple PROs in a cohort of patients who underwent hip arthroscopy.
Conclusion
This is the first study to assess a subjective “completely better” status using PROs at 2 years after hip arthroscopy. The study findings indicated that 47% of patients perceived being CB after hip arthroscopy. Multiple postoperative PRO scores, but not preoperative PROs, were associated with CB status. Furthermore, PRO threshold criteria associated with achieving CB status were identified and demonstrated excellent predictive capability and high sensitivity.
Acknowledgments
The authors acknowledge J. Kathleen Tracy, PhD; Andrew G. Dubina, MD; Julio J. Jauregui, MD; Vidushan Nadarajah, MD; Patrick M.J. Sajak, MD: Tina Zhang, MD; Craig H. Bennett, MD; Cameran I. Burt; Shaun H. Medina; Keyan Shasti; Dominic J. Ventimiglia; Alexander J. Wahl; and Michael P. Smuda for their assistance with the data collection.
Footnotes
Final revision submitted January 16, 2024; accepted February 13, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported in part by a grant from the James Lawrence Kernan Hospital Endowment Fund (BL 1941007WS) and from a US Department of Veterans Affairs Biomedical Laboratory Research and Development Service Career Development Award (IK2 BX004879). N.L.L. has received education payments from Supreme Orthopedic Systems. J.D.P. has received education payments from Supreme Orthopedic Systems. R.F.H. has received education payments from Supreme Orthopedic Systems. S.J.M. has received education payments from Arthrex and Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from University of Maryland Baltimore (ref No. HCR-HP-00062261-9).
References
- 1. Beck EC, Nwachukwu BU, Mehta N, et al. Defining meaningful functional improvement on the visual analog scale for satisfaction at 2 years after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2020;36(3):734-742.e2. doi: 10.1016/j.arthro.2019.09.028 [DOI] [PubMed] [Google Scholar]
- 2. Bodendorfer BM, DeFroda SF, Clapp IM, Newhouse A, Nwachukwu BU, Nho SJ. Defining clinically significant improvement on the Patient-Reported Outcomes Measurement Information System test at 1-year follow-up for patients undergoing hip arthroscopy for the treatment of femoroacetabular impingement syndrome. Am J Sports Med. 2021;49(9):2457-2465. doi: 10.1177/03635465211015687 [DOI] [PubMed] [Google Scholar]
- 3. Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890-897. doi: 10.1177/0363546508330143 [DOI] [PubMed] [Google Scholar]
- 4. Cella D, Gershon R, Lai JS, Choi S. The future of outcomes measurement: item banking, tailored short-forms, and computerized adaptive assessment. Qual Life Res. 2007;16(suppl 1):133-141. doi: 10.1007/s11136-007-9204-6 [DOI] [PubMed] [Google Scholar]
- 5. Cepeda NA, Polascik BA, Ling DI. A primer on clinically important outcome values: going beyond relying on P values alone. J Bone Joint Surg Am. 2020;102(3):262-268. doi: 10.2106/JBJS.19.00817 [DOI] [PubMed] [Google Scholar]
- 6. Cook KF, Jensen SE, Schalet BD, et al. PROMIS measures of pain, fatigue, negative affect, physical function, and social function demonstrated clinical validity across a range of chronic conditions. J Clin Epidemiol. 2016;73:89-102. doi: 10.1016/j.jclinepi.2015.08.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Day MA, Hancock KJ, Selley RS, et al. Patient-Reported Outcomes Measurement Information System Mobility computerized adaptive testing maintains high correlation and low test burden compared with legacy hip-specific instruments in patients undergoing hip arthroscopy for femoroacetabular impingement. Arthroscopy. 2022;38(11):3023-3029. doi: 10.1016/j.arthro.2022.03.038 [DOI] [PubMed] [Google Scholar]
- 8. Egger AC, Frangiamore S, Rosneck J. Femoroacetabular impingement: a review. Sports Med Arthrosc Rev. 2016;24(4):e53. doi: 10.1097/JSA.0000000000000126 [DOI] [PubMed] [Google Scholar]
- 9. Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149-158. doi: 10.1016/S0304-3959(01)00349-9 [DOI] [PubMed] [Google Scholar]
- 10. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120. doi: 10.1097/01.blo.0000096804.78689.c2 [DOI] [PubMed] [Google Scholar]
- 11. Griffin DR, Dickenson EJ, Wall PDH, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet. 2018;391(10136):2225-2235. doi: 10.1016/S0140-6736(18)31202-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Haff RE, Stoltzfus J, Lucente VR, Murphy M. The Surgical Satisfaction Questionnaire (SSQ-8): a validated tool for assessment of patient satisfaction following surgery to correct prolapse and/or incontinence. J Minim Invasive Gynecol. 2011;18(6):S49-S50. doi: 10.1016/j.jmig.2011.08.171 [DOI] [Google Scholar]
- 13. Harris JD, Brand JC, Cote M, Waterman B, Dhawan A. Guidelines for proper reporting of clinical significance, including minimal clinically important difference, patient acceptable symptomatic state, substantial clinical benefit, and maximal outcome improvement. Arthroscopy. 2023;39(2):145-150. doi: 10.1016/j.arthro.2022.08.020 [DOI] [PubMed] [Google Scholar]
- 14. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Henn RF, Dubina AG, Jauregui JJ, Smuda MP, Tracy JK. The Maryland Orthopaedic Registry (MOR): design and baseline characteristics of a prospective registry. J Clin Orthop Trauma. 2017;8(4):301-307. doi: 10.1016/j.jcot.2017.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ishøi L, Thorborg K, Ørum MG, Kemp JL, Reiman MP, Hölmich P. How many patients achieve an acceptable symptom state after hip arthroscopy for femoroacetabular impingement syndrome? A cross-sectional study including PASS cutoff values for the HAGOS and iHOT-33. Orthop J Sports Med. 2021;9(4):2325967121995267. doi: 10.1177/2325967121995267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jamil M, Dandachli W, Noordin S, Witt J. Hip arthroscopy: indications, outcomes and complications. Int J Surg. 2018;54:341-344. doi: 10.1016/j.ijsu.2017.08.557 [DOI] [PubMed] [Google Scholar]
- 18. Johnson C. Measuring pain. Visual analog scale versus numeric pain scale: what is the difference? J Chiropr Med. 2005;4(1):43-44. doi: 10.1016/S0899-3467(07)60112-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kim CH, Moon JK, Yoon JY, et al. Arthroscopy versus nonoperative treatment of symptomatic femoroacetabular impingement syndrome. Medicine (Baltimore). 2020;99(49):e23247. doi: 10.1097/MD.0000000000023247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kollmorgen RC, Hutyra CA, Green C, Lewis B, Olson SA, Mather RC. Relationship between PROMIS computer adaptive tests and legacy hip measures among patients presenting to a tertiary care hip preservation center. Am J Sports Med. 2019;47(4):876-884. doi: 10.1177/0363546518825252 [DOI] [PubMed] [Google Scholar]
- 21. Lynch TS, Minkara A, Aoki S, et al. Best practice guidelines for hip arthroscopy in femoroacetabular impingement: results of a Delphi process. J Am Acad Orthop Surg. 2020;28(2):81-89. doi: 10.5435/JAAOS-D-18-00041 [DOI] [PubMed] [Google Scholar]
- 22. Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010;5(9):1315-1316. doi: 10.1097/JTO.0b013e3181ec173d [DOI] [PubMed] [Google Scholar]
- 23. Martin RL, Harris JD, Ellis T, Kollmorgen R. Comparison of the PROMIS and iHOT-12 in determining satisfaction levels after hip arthroscopy for FAIS. Orthop J Sports Med. 2023;11(5):23259671231168887. doi: 10.1177/23259671231168887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213-218. doi: 10.1177/03635465010290021601 [DOI] [PubMed] [Google Scholar]
- 25. McCurdy MA, Burt CI, Schneider MB, et al. Preoperative opioid use correlates with worse patient-reported outcomes two years after elective shoulder surgery. J Orthop. 2021;25:167-172. doi: 10.1016/j.jor.2021.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nwachukwu BU, Beck EC, Chapman R, Chahla J, Okoroha K, Nho SJ. Preoperative performance of the PROMIS in patients undergoing hip arthroscopic surgery for femoroacetabular impingement syndrome. Orthop J Sports Med. 2019;7(7):2325967119860079. doi: 10.1177/2325967119860079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nwachukwu BU, Beck EC, Kunze KN, Chahla J, Rasio J, Nho SJ. Defining the clinically meaningful outcomes for arthroscopic treatment of femoroacetabular impingement syndrome at minimum 5-year follow-up. Am J Sports Med. 2020;48(4):901-907. doi: 10.1177/0363546520902736 [DOI] [PubMed] [Google Scholar]
- 28. Nwachukwu BU, Rebolledo BJ, McCormick F, Rosas S, Harris JD, Kelly BT. Arthroscopic versus open treatment of femoroacetabular impingement: a systematic review of medium- to long-term outcomes. Am J Sports Med. 2016;44(4):1062-1068. doi: 10.1177/0363546515587719 [DOI] [PubMed] [Google Scholar]
- 29. Qiao HY, Zhang YH, Ren YM, Tian MQ. Arthroscopic versus open treatment for femoroacetabular impingement: a systematic review and meta-analyses. Medicine (Baltimore). 2020;99(47):e23364. doi: 10.1097/MD.0000000000023364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rosinsky PJ, Kyin C, Maldonado DR, et al. Determining clinically meaningful thresholds for the Nonarthritic Hip Score in patients undergoing arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2021;37(10):3113-3121. doi: 10.1016/j.arthro.2021.03.059 [DOI] [PubMed] [Google Scholar]
- 31. Ross JR, Larson CM, Bedi A. Indications for hip arthroscopy. Sports Health. 2017;9(5):402-413. doi: 10.1177/1941738117712675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Saks BR, Ouyang VW, Domb ES, et al. Equality in hip arthroscopy outcomes can be achieved regardless of patient socioeconomic status. Am J Sports Med. 2021;49(14):3915-3924. doi: 10.1177/03635465211046932 [DOI] [PubMed] [Google Scholar]
- 33. Saleh KJ, Bershadsky B, Cheng E, Kane R. Lessons learned from the hip and knee musculoskeletal outcomes data evaluation and management system. Clin Orthop Relat Res. 2004;(429):272-278. doi: 10.1097/01.blo.0000137589.23853.61 [DOI] [PubMed] [Google Scholar]
- 34. Schneider MB, Kung JE, Zhang T, et al. Patient perception of being “completely better” after anterior cruciate ligament reconstruction. Am J Sports Med. 2022;50(5):1215-1221. doi: 10.1177/03635465221074331 [DOI] [PubMed] [Google Scholar]
- 35. Stone AV, Beck EC, Malloy P, et al. Preoperative predictors of achieving clinically significant athletic functional status after hip arthroscopy for femoroacetabular impingement at minimum 2-year follow-up. Arthroscopy. 2019;35(11):3049-3056.e1. doi: 10.1016/j.arthro.2019.05.022 [DOI] [PubMed] [Google Scholar]
- 36. Tashjian R. Editorial Commentary: The Alphabet Soup of Understanding Clinical Shoulder Research: MCID (Minimal Clinically Important Difference), PASS (Patient Acceptable Symptomatic State), SCB (Substantial Clinical Benefit), and now … MOI (Maximal Outcome Improvement). Arthroscopy. 2020;36(7):1811-1812. doi: 10.1016/j.arthro.2020.04.004 [DOI] [PubMed] [Google Scholar]
- 37. Ueland TE, Disantis A, Carreira DS, Martin RL. Patient-reported outcome measures and clinically important outcome values in hip arthroscopy: a systematic review. JBJS Rev. 2021;9(1):e20.00084. doi: 10.2106/JBJS.RVW.20.00084 [DOI] [PubMed] [Google Scholar]
- 38. Zhang D, Chen L, Wang G. Hip arthroscopy versus open surgical dislocation for femoroacetabular impingement. Medicine (Baltimore). 2016;95(41):e5122. doi: 10.1097/MD.0000000000005122 [DOI] [PMC free article] [PubMed] [Google Scholar]


