Abstract
Background:
Ample research has documented the potential of both negative and positive impacts secondary to the COVID-19 pandemic on global mental health in adults and families, but less work has focused on mothers who experience economic marginalization. This longitudinal study aims to assess the impact of positive changes from the pandemic on the association between COVID-related stressors and psychopathology before and after the start of the pandemic.
Methods:
Seventy-five mothers from low income, economically marginalized backgrounds (mean age=30 years, 80 % Black) completed a pre-pandemic visit (T1;2015–2019) and an online survey (T2;2020–2021) mid-pandemic. The study assessed mother’s depressive and posttraumatic stress symptoms and lifetime adversity, COVID-19 related stressors, and positive changes associated with the pandemic.
Results:
Controlling for pre-pandemic psychopathology symptoms, lifetime adversity and educational attainment, there was a significant, positive association between exposure to COVID-19 related stressors and risk for T2 psychopathology. Positive life changes buffered this association, however, such that exposure to COVID-19 related stressors and psychopathology were unrelated for mothers who reported a moderate to high level of positive changes associated with the pandemic.
Limitations:
The sample was small and generalizability of results is limited.
Conclusions:
The pandemic was associated with an increase in mental health problems and unique stressors, especially among caregivers who are low-income. These findings shine light on how both material and psychological access to positive experiences (e.g., more time with family) can buffer the impact of stressors on mental health symptoms.
Keywords: Covid-19 pandemic, Depressive symptoms, Post-traumatic stress symptoms, Mothers, Low-income
1. Introduction
Families of color have been disproportionately impacted by the COVID-19 pandemic and associated social disruptions, including housing instability, increased domestic violence, and job loss (Loades et al., 2020; Brooks et al., 2020; Racine et al., 2022; Whaley and Pfefferbaum, 2023). The global lockdown also resulted in a set of novel stressors such as social isolation, school closures, remote working/schooling, physical distancing, and masking (Clair et al., 2021). These stressors may be more manageable for the socioeconomically advantaged, as access to physical and mental resources may help mitigate their impact (e.g., consistent at-home Wi-Fi and technology, opportunity for remote work, availability of caregivers for at-home schooling, access to personal protective equipment). And, while death of a loved one and risk of infections affected all Americans, those with less economic resources experienced greater frequency of COVID-19 related deaths and infection rates (Parenteau et al., 2022). Moreover, people of color experienced higher rates of hospitalization and mortality during the pandemic than their White counterparts (Wortham et al., 2020; Hooper et al., 2020). The resulting disproportionate impact stems from a backdrop of historical and racial trauma and systemic inequities in healthcare and socioeconomic position for families of color (Walton et al., 2021).
Meta-analytic and scoping reviews also have documented the unique challenges faced by caregivers, specifically mothers, during the pandemic (Racine et al., 2022; Whaley and Pfefferbaum, 2023). School and childcare closures, decreased access to social support, and reduction in household income all disrupted family routines, deteriorated parental mental health, and negatively impacted children’s psychosocial functioning (Racine et al., 2022). These challenges are compounding, rather than additive, such that school and childcare closures were particularly straining for caregivers without the opportunity to work from home and with low levels of social support (Usmani et al., 2021; Kinser et al., 2021; Iob et al., 2020).
Research has documented an increase in depressive and post-traumatic stress symptoms globally among caregivers after the start of the pandemic (Cooke et al., 2020). Further, Racine et al. (2022) concluded that approximately one in four mothers of young children experienced clinically significant levels of depression during the pandemic. Many expected the disproportionate impacts of COVID-19 stressors among marginalized communities (e.g., people of color who are low-income economically marginalized in the US; APA, 2019) to result in disproportionate increases in mental health problems, however, meta-analytic comparative findings are mixed (Park et al., 2020; Racine et al., 2022; Whaley and Pfefferbaum, 2023). According to Whaley & Pfefferbaum (2023), demographic variables such as race, age, and socioeconomic status moderated the impact of these stressors on mothers’ mental health, such that higher SES, lower age, and being White buffered the association between stress and mental health in the family domain. In Racine et al. (2022) meta-analytic review, studies with people of color showed lower levels of clinically significant depression, counter to other research studies that people of color have faced disproportionately negative outcomes as a result of the pandemic (Hooper et al., 2020; Brown et al., 2020; Cameron et al., 2020). One possible explanation is that mothers of color faced COVID-19 related stressors with developed, adaptive coping skills that buffered against the negative impact of stressors related to racism, systemic inequities and oppression (Racine et al., 2021; Zimmerman, 2013). Specifically, prior research focused on Black mothers has shown that methods of coping through optimism and strong social support are associated with lower levels of depression and anxiety symptoms, despite harsh environmental conditions or chronic stress exposure (Hassoun Ayoub et al., 2023; Taylor et al., 2010). An additional explanation may be that biased or culturally insensitive assessment methods are normed in predominantly White samples and may obscure accurate levels of depression in mothers of color (Perez et al., 2023). More research is needed to specifically address protective variables that may moderate stress and mental health for mothers of color from low-income, economically marginalized backgrounds who have experienced previous life adversity.
1.1. Unintended positive changes from COVID-19
While the impact of the pandemic has been equated with poor mental health, emergent research has detailed the unintended positive impacts of the COVID-19 pandemic across the world (Williams et al., 2021; Cornell et al., 2022; Tamiolaki and Kalaitzaki, 2020; Stallard et al., 2021). In a study with caregivers from Portugal and the United Kingdom, Stallard et al. (2021) asked participants to identify “positives” that may have come out of the pandemic in an open-ended question. Themes emerged including improved family relationships, new appreciation for life, and adoption of a healthier lifestyle. Results showed associations between high frequency of self-reported “positives” and fewer anxiety symptoms and improved well-being for these mothers. This sample consisted of predominantly middle class, Portuguese and British caregivers who had the opportunity to work from home during the pandemic. In a national longitudinal survey in Australia, Cornell et al. (2022) identified three major themes in self-reported positive changes: increased family time, work flexibility, and a calmer life. Further, they found that cis-women, individuals who lived with a partner, and access to paid remote work were separately, positively associated with more self-reported positive changes because of the pandemic. Alternatively, individuals who lived alone, worked outside of the home, or were unemployed reported fewer positive effects. These findings align with the social patterning of change highlighted in a study in Scotland which found that women who lived with a partner and were employed reported increased quality time with family and better sleep and physical health since the pandemic’s onset (Williams et al., 2021). These trends show that although families face many new challenges because of the pandemic, they also have the opportunity to enjoy more quality time. Further, these international findings suggest that access to flexible remote work seems to be correlated with more time with family members within the household. However, national variability in responses to the COVID-19 pandemic offered widely variable supports to families and workers, as well as in COVID-19′s impacts, may limit the generalizability of these findings to the United States.
In a longitudinal study of families in the US, Bleil et al. (2021) found that adults who experienced childhood neighborhood disadvantage reported higher levels of positive changes during the pandemic relative to adults who did not, suggesting that adults who have experienced prior hardship or adversity in early life may perceive a higher frequency of positive changes. This study was majority White (79 %) and 45 % of parents had a college degree or more, so it remains unclear if these patterns apply to communities of color or communities that are economically marginalized. Indeed, research on positive changes associated with the COVID-19 pandemic has been limited to Western European or White samples with middle class backgrounds, and the role of positive changes among mothers of color who are low-income, economically marginalized during the pandemic remains underrepresented. In an aging sample of Black and White, Non-Hispanic adults, Willey et al. (2022) found that Black participants experienced greater post-traumatic growth than their White, Non-Hispanic counterparts, possibly secondary to coping skills such as positive reframing and religion.
In a mixed-methods study on Black mothers specifically, Hassoun Ayoub and authors (2023), explored Black mothers’ experiences during the shelter-in-place lockdown in the US. Black mothers reported both positive ways of coping (e.g., prayer, meaning making, engaging in routines and eating healthy) and experiences of stress and conflict (e.g., domestic violence in the home, social isolation, barriers to healthcare). Taken together, existing research suggests that mothers of color from low-income, economically marginalized backgrounds with previous lifetime adversity may be disproportionately exposed to COVID-19 related stressors and increases in mental health problems, but also may have strong social support systems and positive meaning-making strategies to buffer these impacts.
Positive life changes from the pandemic are generally associated with greater levels of well-being for adults, and levels of reported positive changes seem to be dependent on situational and societal contexts. Given the highly context-dependent nature of the impact of COVID-19 in physical, emotional, and social domains, and lack of research focus on mothers of color from low-income, economically marginalized backgrounds, attention to this specific group is warranted. This study aims to explore the relationship between positive COVID-19 related changes on maternal psychopathology in a sample with elevated, multifaceted exposure to lifetime adversity through both structural and interpersonal mechanisms.
2. Hypotheses
COVID-19 related stressors will be positively associated with an increase in depressive and post-traumatic stress symptoms from pre-pandemic to mid pandemic.
Controlling for prior psychopathology symptoms and stress exposure, self-reported positive changes during the pandemic will buffer the association between exposure to COVID-19 related stressors and depressive and post-traumatic stress symptoms.
3. Current study
The current study was a secondary analysis of data collected as part of a longitudinal study examining stress and coping among mother-child dyads. Data collection occurred at two timepoints (T1 and T2). At T1, between September 2015 to February 2019, participants included 158 mothers (Mean age= 29.89 years, SD = 5.42; 100 % female) and their preschool-aged children (Mean age= 51.45 months, SD= 8.97; 51.3 % female). Most mothers self-identified as Black or African American (82.9 %) and non-Hispanic (72.8 %), had at least a high school education (88.5 %) and were employed at least part-time (59.5 %). All participating families were low income and at or near the federal poverty level (≤185 % federal poverty guidelines). Families were excluded from participation if the mothers were unable to complete study measures in English; if children had a previous diagnosis of global developmental delay per parental report; or if caregivers were not biological mothers, due to heritability of biological outcomes of interest in the parent study.
T2 data was collected during the COVID-19 pandemic through self-report surveys between October 2020-April 2021. Fifty-eight percent (N = 91) of mothers from T1 had current contact information and consented to participate at T2, of whom 75 provided data on previous lifetime adversity, COVID-19 related stressors, depressive symptoms and post-traumatic stress symptoms. Eighty percent self-identified as Black or African American, 13.3 % White, 2.7 % Asian American and/or Pacific Islander, and 4 % reported Other. Participants reported varying levels of educational attainment (9.5 % college degree, 34.8 % 1–3 years of college, 28.5 % high school diploma or equivalent degree), and mean age was 30.15 years, (SD=5.75). Given links between educational attainment and self-reported positive changes (both high and low levels; see Henson et al., 2021), educational attainment was included as an ordinal covariate a priori in subsequent analyses. One participant did not report their education level and was not included in moderation analyses.
4. Methods
4.1. Data collection procedures
Procedures were approved by a university Social-Behavioral Institutional Review Board. At T1, screenings took place at Head Start programs and clinics in New Orleans, Louisiana. As part of the aims of the larger study, mothers were oversampled for exposure to family violence and interpersonal trauma using the Life Events Checklist (Gray et al., 2004). Participation in T1 consisted of two visits with mother and child; each visit was approximately two hours and took place either in the family’s home or at our office, according to mothers’ preference. Mothers who completed both visits at T1 were invited to participate in a remote follow up survey at T2. The average length of time between T1 and T2 was 3.59 years (mode= 3.49, range= 1.95 to 5.09 years). Mothers were compensated with a $50 gift card for each visit and survey, and children received a book and small toys at the visits.
4.2. Self-report measures
4.2.1. Sociodemographic information
At T1 (pre-pandemic; see Table 1), mothers self-reported demographics including age, race, ethnicity, and educational attainment. Age was calculated at T2 (October 2020-February 2021; mid-pandemic). Race was measured at T1 with the question, “Which group below most accurately describes your race?”. Response choices included American Indian/Alaska Native, Asian, Black or African American, Native Hawaiian or other Pacific Islander, White or Other with an option to describe their race. Ethnicity was measured at T1 with a binary choice option (Hispanic/Non-Hispanic).
Table 1.
Descriptive & correlations for study variables.
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Covariates and Predictor Variables | |||||||||
| 1. | Education Levela | – | – | – | – | – | – | – | – |
| 2. | Depressive Symptoms T1c | .070 | – | – | – | – | – | – | – |
| 3. | Post-Traumatic Stress Symptoms T1 | .063 | .871** | – | – | – | – | – | – |
| 4. | PTEb Exposure T2 | .323** | .204 | .272* | – | – | – | – | – |
| 5. | COVID-19 Related Stressors | .207 | .215 | .296** | .386** | – | – | – | – |
| 6. | Positive Change Outcomes Outcome Variables | −0.049 | −0.264* | −0.324** | −0.038 | −0.012 | – | – | – |
| 7. | Depressive Symptoms T2 | .122 | .544** | .576** | .227 | .409** | −0.228* | – | – |
| 8. | Post-Traumatic Stress Symptoms T2 | .148 | .409** | .495** | .194 | .476** | −0.061 | .775** | – |
|
| |||||||||
| Descriptive Statistics | |||||||||
| N | 74 | 75 | 75 | 75 | 75 | 75 | 75 | 75 | |
| M | – | 10.47 | 14.87 | 5.59 | 16.04 | 3.95 | 17.71 | 15.79 | |
| SD | - | 12.48 | 15.15 | 4.88 | 9.49 | 2.09 | 17.44 | 15.31 | |
Maternal education coded as 0 = 8th grade or less, 1 = 1–3 years of high school, 2=HS diploma/GED, 3=vocational school/other non-college, 4 = 1–3 years of college, 5=associate’s degree, 6=college degree, 7=master’s degree, 8=professional degree.
PTE = Potentially Traumatic Experience.
T1 = Time 1, data collected pre-COVID-19 (2015–2019), T2 = Time 2, data collected mid-COVID-19 (2020–2021).
P < .05,.
P < .001.
4.2.2. Potentially traumatic life events
Mothers reported on their exposure to potentially traumatic life events at T2 (mid-pandemic) via a modified version of the Life Events Checklist (LEC; Gray et al., 2004), a 20-item measure capturing both direct and indirect PTE (potentially traumatic experience) exposure (e.g., natural disaster, community violence) across their lifetime, either happening to them or witnessed exposure. Each item has a response of “yes” or “no”, and sum scores were created for PTE exposure. The LEC is intended to capture total lifetime events but does not include exposure to COVID-19related stressors.
4.2.3. The epidemic-pandemic impacts inventory (EPII; Grasso et al., 2020)
The EPII is an inventory of pandemic-related experiences across several life domains: Work Life, Home Life, Social Activities and Isolation, Emotional/Physical Health and Infection, and Positive Change. A shortened version of the EPII was used in consultation with the authors of the measure. All domains except for the Positive Change domain index negative or adverse experiences. Each item has a response set of “Yes, Me”, “Yes, Person in Home”, “No”, and “Not Applicable”, except for items 42, 43, and 65, which pertain to the household more globally. For the purposes of this paper, the two “Yes” responses were collapsed, as were the “No” and “N/A” responses, which resulted in dichotomous indicator; this yielded a 43-item COVID-19 stressor exposure scale score (M = 16.04, SD=9.49). The 6 Positive Change items were also summed to yield a Positive Change scale score (M = 3.95, SD=2.09). The EPII is a newly developed measure, therefore research is limited on its scoring and psychometric properties, especially for the Positive Change subscale. Alpha internal consistency reliability for the Positive Change subscale was high (0.80).
4.2.4. Depressive symptoms
Mothers self-reported on their T1 and T2 depressive symptoms using the Center for Epidemiologic Studies Depression Scale – Revised (CESD-R; Eaton et al., 2004), a widely-used 20-item scale assessing depressed mood, disturbances with appetite or sleep, difficulty concentrating, fatigue, feelings of worthlessness, psychomotor agitation, and suicidal ideation throughout the past month using a 4-point Likert scale (not at all to a lot). Sum scores were created for depressive symptoms at T1 and T2. Alpha internal consistency reliability was high at time 1 (0.94) and time 2 (0.95).
4.2.5. Post-traumatic stress symptoms
Mothers self-reported on their T1 and T2 post-traumatic stress symptoms using the PTSD Checklist for DSM-5 (PCL-5; Blevins et al., 2015). The 20-item PCL-5 measured the degree to which mothers experienced symptoms of post-traumatic stress such as hypervigilance, intrusive thoughts, and avoidance throughout the past month on a 5-point Likert scale (not at all to extremely). Sum scores were created for post-traumatic stress symptoms at T1 and T2. Alpha internal consistency reliability was high at time 1 (0.94) and time 2 (0.95).
5. Results
5.1. Preliminary analyses and descriptive statistics
Data was examined for missing items and normality assumptions. T-tests revealed no significant differences between participants who completed the T2 survey data (N = 75) and those who did not (N = 78) on their reports of T1 post-traumatic stress symptoms, T1 depressive symptoms, educational attainment. There was one outlier case removed for a final N = 74. Preliminary analyses examined descriptive statistics and correlations among study variables and demographic characteristics (see Table 1). For post-traumatic stress symptoms, 14.7 % of mothers reported post-traumatic stress symptoms above the clinical threshold at T1 and T2. At T1, 21.3 % of mothers reported depressive symptoms above the clinical threshold, and T2, 41.3 % of mothers reported depressive symptoms above the clinical threshold. While mean depressive symptoms were sub-clinical prior to the pandemic, during the pandemic, mean depressive symptoms were above the clinical cut off of 16 or above (Roth et al., 2008; see Table 1). The frequencies of endorsements of items by response option for positive changes are reported in Table 2.
Table 2.
Base Rates of EPII COVID-19 Positive Changes.
| Positive Changes Subscale | N endorsed | % of subjects |
|---|---|---|
| 1.More appreciative of things usually taken for granted | 64 | 85.3 % |
| 2.More quality time with family or friends in person or from a distance (e.g., on the phone, Email, social media, video conferencing, online gaming). | 56 | 75 % |
| 3.Developed new hobbies or interest or spent more time doing hobbies or other interests | 42 | 56. % |
| 4.Improved relationships with family or friends. | 41 | 54.7 % |
| 5.Donated time/things or volunteered to help people in need. | 39 | 52.0 % |
| 6.New connections made with supportive people | 34 | 45.3 % |
| 7.Increase in exercise or physical activity | 20 | 26.7 % |
Note. N = 75.
5.2. Moderation analysis
To test our primary hypotheses – that positive changes during the pandemic would moderate the association between COVID-19 stress exposure and mothers’ psychopathology– we ran two bootstrapped, generalized linear models. These analyses were conducted separately for T2 depressive symptoms and T2 post-traumatic stress symptoms using the PROCESS macro, an observed variable OLS and logistic regression path analysis modeling tool that uses a bootstrapping method of resampling with replacement to adjust for non-normality (Hayes, 2017). Statistically significant interactions were interpreted using simple slopes analyses. For each model, conditional effects of COVID-19 stress exposure on maternal psychopathology (e.g., depressive or post-traumatic stress symptoms) at different values of the moderator (−1 SD, mean and +1 SD positive changes scores) were calculated and visualized. Additionally, the PROCESS macro estimates regions of significance using the Johnson-Neyman technique. Using this technique, we examined the moderating effects of positive changes (w = positive changes due to COVID) on the pathway between the predictor (x = COVID-19 stress exposure) and the outcome (y = mothers’ depressive or post-traumatic stress symptoms).
5.2.1. Model 1
Model 1 (see Table 3) examined T2 depressive symptoms, modeling main effects of COVID-19 positive and negative life events, a positive x negative interaction term, and covariates of education level, T1 depressive symptoms, and T2 potentially traumatic lifetime events. These predictors along with the positive changes x COVID-19 negative life events interaction term explained 45 % of the variance in mothers’ depressive symptoms. A significant interaction effect was observed between positive changes and COVID-19 negative life events (β = −0.201, 95 % CI [−0.387, −0.015]; R2 change for interaction = 0.04, F(1,73) = 4.63, p=.03).
Table 3.
Model 1: Moderation analysis of COVID-19 positive life changes on COVID-19 stress x depressive symptoms.
| Effect | β | SE | t | p | Lower CI | Upper CI |
|---|---|---|---|---|---|---|
| Constant | 10.876 | 4.272 | 2.545 | .013* | 2.354 | 19.398 |
| Maternal education level | −0.279 | 1.088 | −0.257 | .798 | −2.451 | 1.892 |
| Previous lifetime adversity | .199 | .378 | .541 | .590 | −0.535 | .933 |
| T1 depressive symptoms | .652 | .133 | 4.885 | .000** | .386 | .919 |
| COVID-19 stressful events (cneg) | .607 | .183 | 3.321 | .001** | .242 | .971 |
| COVID-19 positive life changes (cpos) | −1.100 | .788 | −1.414 | .162 | −2.653 | .452 |
| CNEG x CPOS interaction | −0.201 | .093 | −2.152 | .035* | −0.387 | −0.015 |
Note: n = 74,.
P < .05.
P < .01.
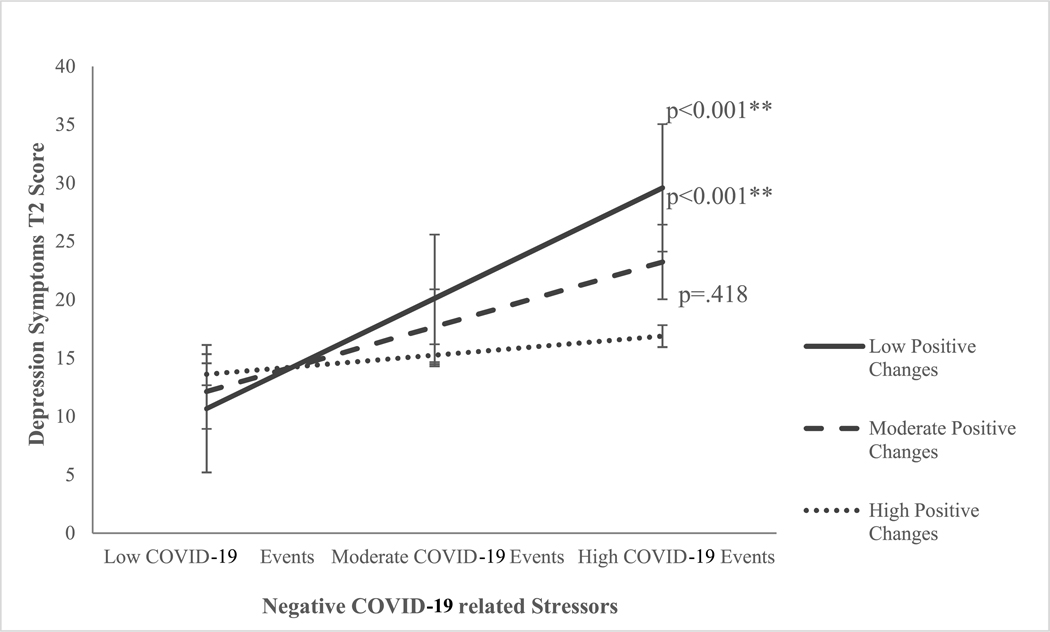
Conditional effects of COVID-19 negative life events on T2 depressive symptoms for low, moderate, and high frequency of positive changes were estimated (See Fig. 1). Analysis of conditional effects demonstrated that at low (−1 SD, 95 % CI [0.488, 1.569], p<.001) and moderate (mean = 3.95, 95 % CI [.242, 0.971], p<.001) reported positive changes, there was a significant, positive association between COVID-19 negative life events and T2 depressive symptoms. When parents reported approximately four or more positive changes, there was no significant association between COVID-19 negative life events and T2 depressive symptoms (see Fig. 1).
Fig. 1.
Positive changes moderate the effect of negative COVID-19 related stressors on T2 depressive symptoms.
Note. This figure demonstrates the moderating effect of low and moderate levels of positive changes on mid-pandemic depressive symptoms and negative COVID-19 related stressors, when controlling for lifetime adversity, pre-pandemic depressive symptoms, and educational attainment. Error bars represent the standard error. **p<.001
5.2.2. Model 2
Model 2 (See Table 4) was identical to Model 1 but tested T2 post-traumatic stress symptoms, controlling again for education level and T2 potentially traumatic lifetime events as well as T1 post-traumatic stress symptoms. For post-traumatic stress symptoms, covariates and main effects as well as the positive changes x COVID-19 negative life events interaction term explained 44 % of the variance in the model (R2 change = 0.44, F (1,73) = 8.68, p<.000). A significant interaction effect was observed between positive changes and COVID-19 negative life events (β = − 0.198, 95 % CI [−0.366, −0.029], p=.02).
Table 4.
Model 2: Moderation analysis of COVID-19 positive life changes on COVID-19 stress x post-traumatic stress symptoms.
| Effect | β | SE | t | p | Lower CI | Upper CI |
|---|---|---|---|---|---|---|
| Constant | 8.388 | 3.937 | 2.131 | .037* | .530 | 16.247 |
| Maternal education level | .316 | .993 | .319 | .751 | −1.666 | 2.298 |
| Previous lifetime adversity | −0.105 | .335 | −0.312 | .756 | −0.774 | .565 |
| T1 post-traumatic stress symptoms | .469 | .106 | 4.442 | .000** | .259 | .681 |
| COVID-19 stressful events (cneg) | .614 | .166 | 3.689 | .000** | .2819 | .946 |
| COVID-19 positive life changes (cpos) | .379 | .719 | .528 | .599 | −1.057 | 1.817 |
| CNEG x CPOS interaction | −0.198 | .084 | −2.343 | .022* | .366 | −0.029 |
Note: n = 74,.
P < .05.
P < .01.
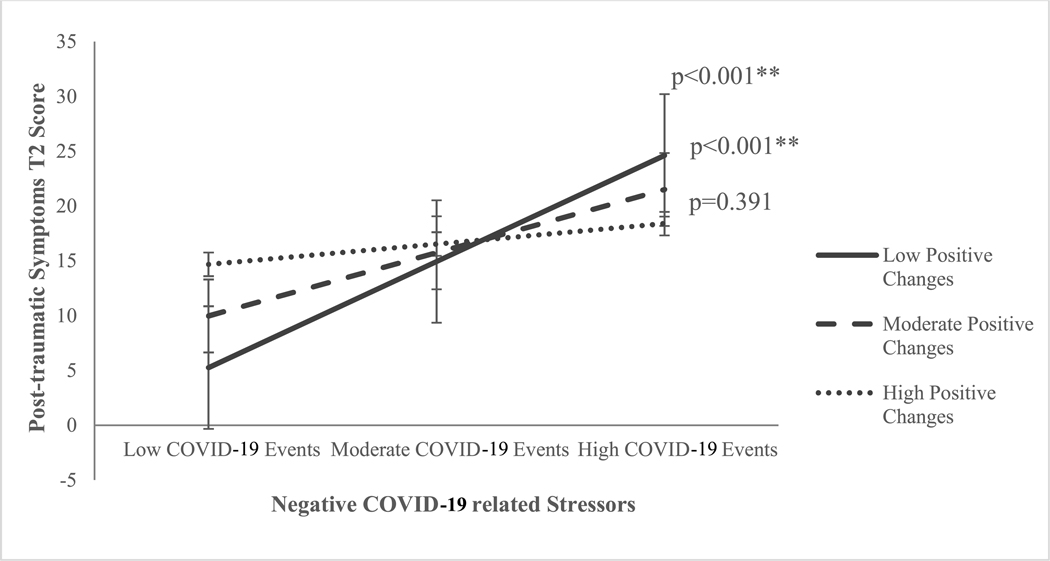
Conditional effects of COVID-19 negative life events on T2 post-traumatic stress symptoms for low, moderate, and high frequency of positive changes were estimated (See Fig. 2). Analysis of conditional effects demonstrated that at low (−1 SD, 95 % CI [0.543, 1.52], p<.001) and moderate (mean = 3.95, 95 % CI [0.282, 0.946, p<.001) reported positive changes, there was a significant, positive association between COVID-19 negative life events and T2 post-traumatic stress symptoms. In a trend similar to Model 1, for mothers who reported at least four or more positive changes there was no significant interaction between COVID-19 negative life events and T2 post-traumatic stress symptoms.
Fig. 2.
Positive changes moderate the effect of negative-COVID-19 related stressors on T2 post-traumatic stress symptoms.
Note. This figure demonstrates the moderating effect of low and moderate levels of positive changes on mid pandemic post-traumatic stress symptoms and negative COVID-19 related stressors, when controlling for lifetime adversity, pre-pandemic post-traumatic stress symptoms, and educational attainment. **p<.001
6. Discussion
These findings support and extend current research related to the impact of COVID-19 on mothers, particularly Black mothers from low-income, economically marginalized backgrounds. Firstly, consistent with previous work (Patrick et al., 2020; Racine et al., 2021), mothers’ depressive symptoms in this sample increased from pre- to mid-pandemic. A subset of mothers reported clinically significant levels of depressive (41.3 %) and post-traumatic stress symptoms (14.7 %) during the COVID data collection point. Mothers also reported higher levels of previously traumatic life events than other community samples (see Pugach et al., 2021) and higher rates of COVID-19 related stressors (See Grasso et al., 2021). These findings shed light on the pervasive health-wealth gradient in the US that is upheld by structural racism and socioeconomic inequality. However, some silver linings emerged. For mothers who reported at least four or more positive changes in their life, such as increased time with family, improved relationships, and increased feelings of gratitude, COVID-19 negative life events did not confer significant risk for depressive or post-traumatic stress symptoms.
These findings are also consistent with work on post-traumatic growth (PTG), which has demonstrated that potentially traumatic life events, such as the pandemic, may be catalysts for positive changes, including improved relationships, increased gratitude, spiritual and personal growth (Calhoun and Tedeschi, 2013; Ortega-Williams et al., 2021). After a traumatic event, the individual is theorized to challenge their own core beliefs and engage in some level of cognitive processing of the event (Calhoun and Tedeschi, 2013). According to Calhoun & Tedeschi (1998), PTG is a radical personal transformation with observable positive changes and not a culmination of positive life changes that may occur after an event. To this end, we can speculate that the positive changes in the current study may be evidence of PTG and coping within the pandemic. An additional interpretation is that exposure to opportunity for positive changes through both psychosocial and physical resources (e.g., social support, ability to work from home, access to healthy foods) may counterbalance the impacts of potentially traumatic life events and may be an important component of buffering negative impacts associated with exposure to adversity.
Individual differences in cognitive styles, especially attributional styles around processing stressful life events, may offer another interpretative lens for understanding the protective effects of positive changes. It is possible that the measure of positive changes used in this study, the Positive Changes subscale of the Epidemic-Pandemic Impacts Inventory (EPII; Grasso et al., 2020), is a proxy for a positive or “optimistic” attributional style. Optimism can be operationalized as an attributional style in which individuals perceive a negative event as 1) unstable, (the negative event will not continue forever), 2) external (I am not to blame for the event) and 3) specific (the event will not affect all aspects of my life) (Conversano et al., 2010). The optimistic individual consistently experiences better mental and physical health outcomes (Rasmussen et al., 2009; Rincon et al., 2022; Carver et al., 2014) because they believe they can prevent bad things from happening, which then translates into active coping (Peterson and De Avila, 1995). Optimistic individuals engage in more health-promoting activities when compared with their pessimistic counterparts (Peterson et al., 1993; Carver et al., 2010). In the context of this study, individuals who endorsed four or more positive changes on the EPII may be engaging in more active coping strategies for stress management (i.e., developing new hobbies, increasing physical activity), which may offset the adverse effects of exposure to COVID-19 related stressors. This is consistent with literature that for Black mothers exposed to adversity, higher levels of optimism are associated with fewer internalizing problems and increased ability to overcome challenges (Taylor et al., 2020).
Mothers endorsing more positive changes may also experience more social support from family members and/or friends, which may also function to mitigate the negative impact of exposure to COVID-19 related stressors. Three items on the EPII positive changes subscale deal with increases to social support (i.e., more quality time with family or friends, improved relationships with family or friends, new connections made with supportive people). Social support is generally associated with better mental and physical health (Taylor, 2011; Callaghan and Morrissey, 1993; Uchino, 2006) and is protective against psychopathology (Racine et al., 2019; Collins et al., 1993; Prelow et al., 2010). Prior analyses with this particular study sample found that maternal social support buffered the association between maternal adverse childhood experiences (ACEs) and children’s externalizing behaviors (Hatch et al., 2020); these results underscore how social support acts as a context-specific and culturally relevant protective factor in a predominantly Black sample (Hassoun-Ayoub et al., 2023; Hall, 2007; Jarrett et al., 2010). The current study also finds evidence that social support (as measured in part on the EPII) may also be protective for mothers’ mental health.
The results of the current study also suggest that mothers who report fewer positive changes are at risk for heightened depressive and post-traumatic symptoms. For these mothers, there was a positive and statistically significant association between exposure to COVID-19 related stressors and psychopathology symptoms. This may be evidence of a more negative or “pessimistic” attributional style that is associated with hopelessness, a symptom of major depressive disorder (Haeffal and Vargas, 2011). Research suggests that an enhancing cognitive style or attribution of positive life events has been shown to decrease symptoms of depression (Needles and Abramson, 1990). The results of the current study underscore how negative attributional styles may be a risk factor for stress-induced psychopathology and a target for clinical intervention.
7. Limitations
The current study is limited in multiple domains. The sample is small, and confidence in these findings would increase with additional, larger longitudinal samples. Careful consideration should be given to the generalizability of these findings. The intended focus of this study was to explore risk and resilience with a vulnerable population of majority mothers of color from low-income, economically marginalized backgrounds. One major limitation of this study was the exclusion of racial discrimination measures as a predictor of stress and psychopathology in the context of the COVID-19 pandemic for mothers of color. Research has documented the pernicious effects of the “dual pandemic” or concurrent racism and the COVID-19 pandemic, on Black mothers’ mental well-being (Ibekewe-Okafor et al., 2023). Future studies should explore whether perceived positive changes from the pandemic can buffer the impact of both racial discrimination and COVID-19 stressors on mental health. Additionally, self-report measures of depressive and post-traumatic stress symptoms are better supplemented with clinical interviews to assess clinical prevalence of psychopathology. Our understanding of mechanisms underlying positive changes associated with the pandemic would be enhanced by measures that included qualitative assessment rather than with a simple frequency count. Furthermore, endorsement of positive changes may be attributed to specific cognitive styles or post-traumatic growth from previous life events, and these perceptions were not captured at T1. Lastly, quality and impact of a positive change may weigh more heavily than others, such as increased time with family (Cornell et al., 2022; Bleil et al., 2021), and these were not parsed out in the current analysis.
7.1. Future directions
Those at the intersection of multiple, oppressed social categories (e.g. gender, socioeconomic status, race, ethnicity) may be particularly vulnerable to traumatic stress and subsequently “optimal” for PTG. In a mixed-methods study of Black mothers from low-income, economically marginalized backgrounds following Hurricane Katrina, Manove et al. (2019) found that higher levels of self-reported PTG (personal strength, appreciation, new possibilities, spiritual growth) was associated with greater exposure to opportunities within post-Katrina communities such as better neighborhoods, new education and economic opportunity and increased racial diversity. These findings highlight the critical significance of opportunity following a traumatic event. Opportunities such as access to material and psychosocial resources such as social support, healthy foods, reliable employment and more fiscal resources are not equally distributed: access to them is more limited among socioeconomically disadvantaged and historically marginalized communities in the wake of a global disaster. While these findings provide burgeoning evidence that this population may possess adaptive strategies to cope with the pandemic, there is a critical need to consider how systems, policies and programs can provide material resources and de-emphasize the burden on individual resilience. These findings suggest that improving access to positive changes may support mental health in the face of adversity.
Acknowledgements
We, the authors, would like to express our gratitude to all the people who contributed their time and thoughtfulness to make this study a success. Thank you to all the mothers and families who participated in the Parent Child and Coping Study. Thank you to the undergraduate research assistant team and graduate student researchers in the Tulane Child and Family Lab who collected, cleaned, and prepared data for the Parent Child and Coping Study from 2015 to 2021.
Footnotes
CRediT authorship contribution statement
Allison Pequet: Writing – review & editing, Writing – original draft, Visualization, Formal analysis, Conceptualization. Anna Wilson: Writing – review & editing, Visualization. Hilary Skov: Writing – review & editing, Visualization, Data curation. Renee Lamoreau: Writing – review & editing, Visualization. Sarah A.O. Gray: Writing – review & editing, Validation, Supervision, Resources, Project administration, Investigation, Funding acquisition.
Declaration of competing interest
This research was supported by the National Institutes of Health (K23MH119047, SG), the Brain & Behavior Foundation NARSAD Young Investigator Program, and the Louisiana Board of Regents Research Competitiveness Subprogram. The content is solely the responsibility of the authors and does not represent the official views of the funding agencies. The authors have no other conflicts of interest to report. The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- American Psychological Association. (2019). Guidelines for psychological practice for people with low-income and economic marginalization. Retrieved from www.apa.org/about/policy/guidelines-lowincome.pdf. [DOI] [PubMed]
- Bleil ME, Appelhans BM, Thomas AS, Gregorich SE, Marquez N, Roisman GI, Crowder K, 2021. Early life predictors of positive change during the coronavirus disease pandemic. BMC. Psychol. 9 (1), 1–14. 10.1186/s40359-021-00586-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL, 2015. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J. Trauma Stress. 28 (6), 489–498. 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ, 2020. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 (10227), 912–920. 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SM, Doom JR, Lechuga-Pena S, Watamura SE, Koppels T, 2020. Stress and parenting during the global COVID-19 pandemic. Child Abuse Negl. 110, 104699 10.1016/j.chiabu.2020.104699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calhoun LG, Tedeschi RG, 2013. Posttraumatic Growth in Clinical Practice. Routledge. [Google Scholar]
- Callaghan P, Morrissey J, 1993. Social support and health: a review. J. Adv. Nurs. 18 (2), 203–210. 10.1046/j.1365-2648.1993.18020203.x. [DOI] [PubMed] [Google Scholar]
- Cameron EE, Joyce KM, Delaquis CP, Reynolds K, Protudjer JLP, Roos LE, 2020. Maternal psychological distress & mental health service use during the COVID-19 pandemic. J. Affect. Disord. 276, 765–774. 10.1016/j.jad.2020.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Segerstrom SC, 2010. Optimism. Clin. Psychol. Rev. 30 (7), 879–889. 10.1016/j.cpr.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, 2014. Dispositional optimism. Trends Cogn. Sci. (Regul. Ed.) 18 (6), 293–299. 10.1016/j.tics.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clair R, Gordon M, Kroon M, Reilly C, 2021. The effects of social isolation on well-being and life satisfaction during pandemic. Human. Social Sci. Commun. 8 (1) 10.1057/s41599-021-00710-3. [DOI] [Google Scholar]
- Collins NL, Dunkel-Schetter C, Lobel M, Scrimshaw SC, 1993. Social support in pregnancy: psychosocial correlates of birth outcomes and postpartum depression. J. Pers. Soc. Psychol. 65 (6), 1243. 10.1037/0022-3514.65.6.1243. [DOI] [PubMed] [Google Scholar]
- Conversano C, Rotondo A, Lensi E, Della Vista O, Arpone F, Reda MA, 2010. Optimism and its impact on mental and physical well-being. Clin. Pract. Epidemiol. Mental Health: CP & EMH 6, 25. 10.2174/1745017901006010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke JE, Eirich R, Racine N, Madigan S, 2020. Prevalence of posttraumatic and general psychological stress during COVID-19: a rapid review and meta-analysis. Psychiatr. Res. 292, 113347 10.1016/j.psychres.2020.113347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornell S, Nickel B, Cvejic E, Bonner C, McCaffery KJ, Ayre J, Dodd R, 2022. Positive outcomes associated with the COVID-19 pandemic in Australia. Health Promot. J. Aust. 33 (2), 311–319. 10.1002/hpja.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Muntaner C, Smith C, Tien A, Ybarra M, 2004. Center for epidemiological studies depression scale: review and revision. The use of psychological testing for treatment planning and outcomes assessment. Plos One. [Google Scholar]
- Grasso DJ, Briggs-Gowan MJ, Carter AS, Goldstein BL, Ford JD, 2021. Profiling COVID-related experiences in the United States with the epidemic-pandemic impacts inventory: linkages to psychosocial functioning. Brain Behav. 11 (8), e02197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasso DJ, Briggs-Gowan MJ, Ford JD, Carter AS, 2020. The Epidemic–Pandemic Impacts Inventory (EPII). University of Connecticut School of Medicine. [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW, 2004. Psychometric properties of the life events checklist. Assessment. 11 (4), 330–341. 10.1177/1073191104269. [DOI] [PubMed] [Google Scholar]
- Haeffel GJ, Vargas I, 2011. Resilience to depressive symptoms: the buffering effects of enhancing cognitive style and positive life events. J. Behav. Ther. Exp. Psychiatr. 42 (1), 13–18. 10.1016/j.jbtep.2010.09.003. [DOI] [PubMed] [Google Scholar]
- Hall C, 2007. Kinship ties: attachment relationships that promote resilience in African American adult children of alcoholics. Adv. Soc. Work 8 (1), 130–140. 10.18060/136. [DOI] [Google Scholar]
- Hassoun Ayoub L, Partridge T, Gómez JM, 2023. Two sides of the same coin: a mixed methods study of black mothers’ experiences with violence, stressors, parenting, and coping during the COVID-19 pandemic. J. Soc. Issues 79 (2), 667–693. 10.1111/josi.12526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatch V, Swerbenski H, Gray SA, 2020. Family social support buffers the intergenerational association of maternal adverse childhood experiences and preschoolers’ externalizing behavior. Am. J. Orthopsychiatr. 90 (4), 489. 10.1037/ort0000451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF, 2017. Introduction to Mediation, Moderation, and Conditional Process Analysis: A regression-Based Approach. Guilford publications. [Google Scholar]
- Hooper MW, Nápoles AM, Pérez-Stable EJ, 2020. COVID-19 and racial/ethnic disparities. J. Am. Med. Assoc. 323 (24), 2466–2467. 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henson C, Truchot D, Canevello A, 2021. What promotes post traumatic growth? A systematic review. Eur. J. Trauma Dissociation 5 (4), 100195. 10.1016/j.ejtd.2020.100195. [DOI] [Google Scholar]
- Ibekwe-Okafor N, Sims J, Curenton SM, 2023. Black motherhood and the dual pandemics: the protective role of stable income on mental wellbeing. J. Soc. Issues. [Google Scholar]
- Iob E, Frank P, Steptoe A, Fancourt D, 2020. Levels of severity of depressive symptoms among at-risk groups in the UK During the COVID-19 pandemic. J. Am. Med. Assoc. Netw. Open 3 (10), e2026064. 10.1001/jamanetworkopen.2020.26064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrett RL, Jefferson SR, Kelly JN, 2010. Finding community in family: neighborhood effects and African American kin networks. J. Comp. Fam. Stud. 41 (3), 299–328. 10.3138/jcfs.41.3.299. [DOI] [Google Scholar]
- Kinser PA, Jallo N, Amstadter AB, Thacker LR, Jones E, Moyer S, Salisbury AL, 2021. Depression, anxiety, resilience, and coping: the experience of pregnant and new mothers during the first few months of the COVID-19 pandemic. J. Womens Health 30 (5), 654–664. 10.1089/jwh.2020.8866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, Crawley E, 2020. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatr. 59 (11), 1218–1239. 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manove EE, Lowe SR, Bonumwezi J, Preston J, Waters MC, Rhodes JE, 2019. Posttraumatic growth in low-income black mothers who survived hurricane Katrina. Am. J. Orthopsychiatr. 89 (2), 144. 10.1037/ort0000398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Needles DJ, Abramson LY, 1990. Positive life events, attributional style, and hopefulness: testing a model of recovery from depression. J. Abnorm. Psychol. 99 (2), 156. 10.1037/0021-843X.99.2.156. [DOI] [PubMed] [Google Scholar]
- Ortega-Williams A, Beltrán R, Schultz K, Ru-Glo Henderson Z, Colón L, Teyra C, 2021. An integrated historical trauma and posttraumatic growth framework: a cross-cultural exploration. J. Trauma Dissociation 22 (2), 220–240. 10.1080/15299732.2020.1869106. [DOI] [PubMed] [Google Scholar]
- Parenteau AM, Boyer CJ, Campos LJ, Carranza AF, Deer LK, Hartman DT, Hostinar CE, 2022. A review of mental health disparities during COVID-19: evidence, mechanisms, and policy recommendations for promoting societal resilience. Dev. Psychopathol. 1–22. 10.1017/S0954579422000499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park AL, Velez CV, Kannan K, Chorpita BF, 2020. Stress, functioning, and coping during the COVID-19 pandemic: results from an online convenience sample. Behav. Ther. (N. Y. N. Y) 42 (6), 210–216. 10.31234/osf.io/jmctv. [DOI] [Google Scholar]
- Patrick SW, Henkhaus LE, Zickafoose JS, Lovell K, Halvorson A, Loch S, Letterie M, Davis MM, 2020. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 146 (4) 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- Peterson C, Maier SF, Seligman ME, 1993. Learned helplessness: A theory For the Age of Personal Control. Oxford University Press, USA. [Google Scholar]
- Peterson C, De Avila ME, 1995. Optimistic explanatory style and the perception of health problems. J. Clin. Psychol. 51 (1), 128–132. 10.1002/1097-4679(199501)51. :1≤128::AID-JCLP2270510120≥3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Perez NB, D’Eramo Melkus G, Wright F, Yu G, Vorderstrasse AA, Sun YV, Crusto CA, Taylor JY, 2023. Latent class analysis of depressive symptom phenotypes among black/African American mothers. Nurs. Res. 72 (2), 93. 10.1097/NNR.0000000000000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prelow HM, Weaver SR, Bowman MA, Swenson RR, 2010. Predictors of parenting among economically disadvantaged Latina mothers: mediating and moderating factors. J. Community Psychol. 38 (7), 858–873. 10.1002/jcop.20400. [DOI] [Google Scholar]
- Pugach CP, Nomamiukor FO, Gay NG, Wisco BE, 2021. Temporal stability of self-reported trauma exposure on the Life Events Checklist for DSM-5. J. Trauma Stress. 34 (1), 248–256. [DOI] [PubMed] [Google Scholar]
- Racine N, Eirich R, Cooke J, Zhu J, Pador P, Dunnewold N, Madigan S, 2022. When the bough breaks: a systematic review and meta-analysis of mental health symptoms in mothers of young children during the COVID-19 pandemic. Infant. Ment. Health J. 43 (1), 36–54. 10.1002/imhj.21959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N, McDonald S, Tough S, Madigan S, 2021. Mediating mechanisms for maternal mental health from pre-to during the COVID-19 pandemic: mediators of maternal mental illness during COVID-19. J. Affect. Disord. Rep. 6, 100287 10.1016/j.jadr.2021.100287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N, Plamondon A, Hentges R, Tough S, Madigan S, 2019. Dynamic and bidirectional associations between maternal stress, anxiety, and social support: the critical role of partner and family support. J. Affect. Disord. 252, 19–24. 10.1016/j.jad.2019.03.083. [DOI] [PubMed] [Google Scholar]
- Rasmussen HN, Scheier MF, Greenhouse JB, 2009. Optimism and physical health: a meta-analytic review. Annal. Behav. Med. 37 (3), 239–256. 10.1007/s12160-009-9111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rincon Uribe FA, Neira Espejo CA, Pedroso JDS, 2022. The role of optimism in adolescent mental health: a systematic review. J. Happiness. Stud. 23 (2), 815–845. 10.1007/s10902-021-00425-x. [DOI] [Google Scholar]
- Roth DL, Ackerman ML, Okonkwo OC, Burgio LD, 2008. The four-factor model of depressive symptoms in dementia caregivers: a structural equation model of ethnic differences. Psychol. Aging 23, 567–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stallard P, Pereira AI, Barros L, 2021. Post-traumatic growth during the COVID-19 pandemic in carers of children in Portugal and the UK: cross-sectional online survey. BJPsych. Open. 7 (1), e37. 10.1192/bjo.2021.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamiolaki A, Kalaitzaki AE, 2020. That which does not kill us, makes us stronger”: COVID-19 and posttraumatic growth. Psychiatr. Res. 289, 113044 10.1016/j.psychres.2020.113044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE, 2011. Social support: a review. Oxf. Handb. Health Psychol. 1, 189–214. [Google Scholar]
- Taylor ZE, Larsen-Rife D, Conger RD, Widaman KF, Cutrona CE, 2010. Life stress, maternal optimism, and adolescent competence in single mother, African American families. J. Fam. Psychol. 24 (4), 468–477. 10.1037/a0019870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino BN, 2006. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J. Behav. Med. 29, 377–387. 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Usmani S, Greca E, Javed S, Sharath M, Sarfraz Z, Sarfraz A, Ferrer G, 2021. Risk factors for postpartum depression during COVID-19 pandemic: a systematic literature review. J. Prim. Care Community Health 12, 21501327211059348. 10.1177/21501327211059348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton QL, Campbell RD, Blakey JM, 2021. Black women and COVID-19: the need for targeted mental health research and practice. Qual. Soc. Work 20 (1–2), 247–255. 10.1177/1473325020973349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whaley GL, Pfefferbaum B, 2023. Parental challenges during the COVID-19 pandemic: psychological outcomes and risk and protective factors. Curr. Psychiatr. Rep. 25 (4), 165–174. 10.1007/s11920-023-01412-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams L, Rollins L, Young D, Fleming L, Grealy M, Janssen X, Flowers P, 2021. What have we learned about positive changes experienced during COVID-19 lockdown? Evidence of the social patterning of change. PLoS. One 16 (1), e0244873. 10.1371/journal.pone.0244873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willey B, Mimmack K, Gagliardi G, Dossett ML, Wang S, Udeogu OJ, Vannini P, 2022. Racial and socioeconomic status differences in stress, posttraumatic growth, and mental health in an older adult cohort during the COVID-19 pandemic. EClinicalMedicine 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wortham JM, Lee JT, Althomsons S, 2020. Characteristics of persons who died with COVID-19 — United States, February 12–May 18, 2020. MMWR Morb. Mortality Wkly. Rep. 69, 923–929. 10.15585/mmwr.mm6928e. [DOI] [PubMed] [Google Scholar]
- Zimmerman MA, 2013. Resiliency theory: a strengths-based approach to research and practice for adolescent health. Health Educ. Behav. 40 (4), 381–383. 10.1177/1090198113493782. [DOI] [PMC free article] [PubMed] [Google Scholar]