Abstract
Vascular Leiomyoma of the oral cavity is an uncommon benign soft tissue neoplasia arising from the tunica media of the smooth muscle cells. We reported a rare case of Vascular Leiomyoma involving the retromolar trigone area of a young man. A 24-year-old male presented with a slowly growing mass in the retromolar area, which was associated with pain and difficulty in opening of mouth and eating and drinking. A punch biopsy was taken and sent for histopathological examination which revealed a benign angiomatous lesion. The mass was excised, and the adjoining area was curetted. Histopathological examination confirmed the diagnosis of Vascular Leiomyoma. The immunohistochemistry of cells shows: alpha-smooth muscle (+); vimentin (+), Desmin, actin (+), and S100 (−). Angioleiomyomas are benign lesions, but malignant transformation is a possibility so careful histologic inspection is necessary to distinguish these lesions from their malignant counterpart.
Keywords: Benign neoplasm, thick smooth muscle cells, vascular leiomyoma
INTRODUCTION
Leiomyoma is a common neoplasm of the uterus and gastrointestinal tract, mostly occurring in solid variants. It was first described by Virchow in 1854 and first reported by Blanc in 1884. Leiomyoma, a benign smooth muscle neoplasm, is classified by the World Health Organization based on histopathology into three types: 1) solid, 2) vascular (angiomyxoma, angioleiomyoma), and 3) epithelioid. In the head and neck region, leiomyoma is rare, and in the oral cavity, it accounts for only 0.4% of all soft tissue neoplasms and 0.06% of all leiomyomas. Oral leiomyoma mostly presents as an angioleiomyoma variant, accounting for 64–66.2% of all reported cases. It has a wide range of age presentations and no definite gender predilection. The most common sites of occurrence in the oral cavity are the lip, tongue, cheek, and palate. Less commonly, it can involve the gingiva, mandible, and other mucosal sites. Usually, it presents as a slow-growing, asymptomatic, firm nodular mass and is occasionally painful.[1] We report a rare case of large mandibular-retromolar trigone area Vascular Leiomyoma of the oral cavity (VLOC). Clinically, connective tissue tumours e.g. fibromas and lipomas, may present with similar findings to leiomyoma; hence a differential diagnosis must be established. Histological findings play a key role in the final diagnosis of leiomyoma. Moreover, the differential diagnosis must also include the malignant form.
CASE REPORT
A 24-year-old male patient was referred to the Out Patient Department with the chief complaint of a slowly growing mass in the posterior region of the lower jaw. The patient was alright 1 month back, when he noticed a growth in the retromolar trigone area which was initially small but gradually progressed to attain the present size of approx. 6 × 3 cm. He also experienced pain in the same region for 15 days, described as dull, aching, and intermittent. For the past 15 days, he has had difficulty with mastication and eating. He had a history of tobacco chewing for a year. His medical history was otherwise insignificant, and he was not taking any medications.
Clinical examination
A multilobulated, reddish-pink colour mass, approximately six-by-three cm in size, arising from the retromolar trigone area, with surface indentations seen. It was pedunculated and not attached to adjacent tissues. The mass appears to originate from the retromolar area on the right lower jaw, occupying the palate and dorsal surface of the tongue [Figure 1]. It was not fixed to either the palate or the tongue. On palpation, the mass was tender to touch and firm in consistency. Mass was non-reducible, non-compressible, and non-pulsatile. No lymphadenopathy was noted.
Figure 1.

An intraoral photograph shows an ulcerated, expansive swelling in the retromolar trigone region
Computed tomography of the neck revealed an ill-defined, hypodense soft tissue-attenuating lesion approximately 6.0 cm × 2.9 cm in size, seen in the right buccal space, involving the buccal mucosa at the level of the 2nd premolar and molar tooth. The lesion extends up to the gingival surface, reaching posteriorly to the retromolar region and involving the same, possibly indicating neoplastic growth [Figure 2].
Figure 2.
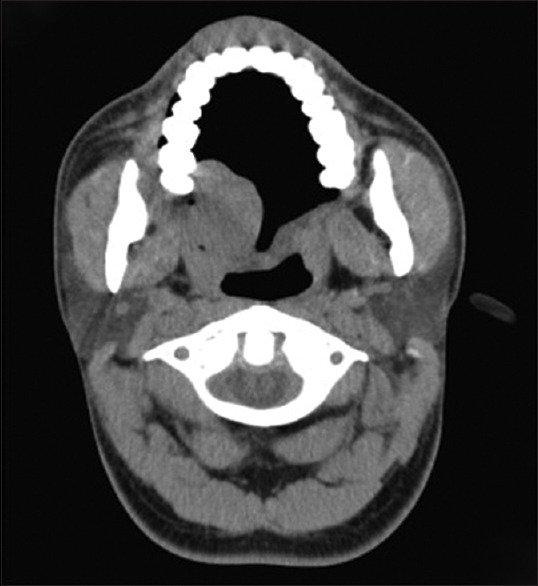
Computed tomography axial image illustrating a 6.0 cm lesion with the largest diameter, which is ill-defined, destructive, expansive, heterogeneous, and hypodense lesion, involving the right buccal mucosa
A punch biopsy was taken and sent for histopathological evaluation, which revealed a benign angiomatous lesion. This tumor was completely excised, and the adjacent area was curetted and cauterized. The tumour was well-circumscribed with a thin fibrous capsule, and a sample obtained was a firm, well-circumscribed, pinkish-white ovoidal nodule (3 cm × 6 cm in dimension). The postoperative period was uneventful.
Histopathology
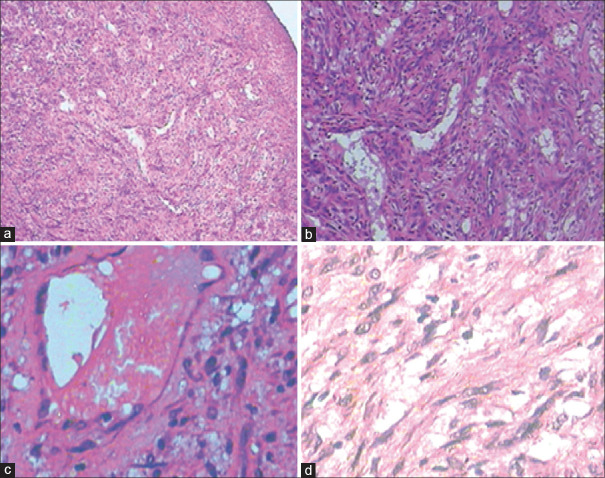
The tumour was well-circumscribed, and the haematoxylin and eosin-stained section showed the presence and abundance of multiple small to large dilated vascular channels, some of which had thick vascular walls. Inter-vascular areas showed spindle cells with eosinophilic cytoplasm and elongated, blunt-ended, cigar-shaped nuclei.
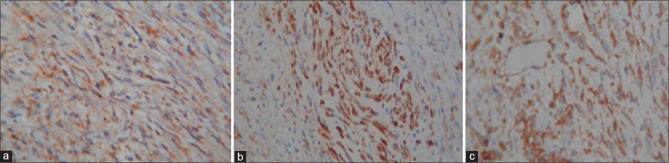
Higher magnification revealed that the tumour consisted of brightly eosinophilic, spindle-shaped cells with copious amounts of cytoplasm but indistinct cytoplasmic membranes. The nuclei were small and round to elongated with blunt ends. No cellular or nuclear atypia was seen. No mitotic activity was noted. The tumour cells were arranged in concentric rings around endothelium-lined vascular channels, which appeared compressed. Interstitial areas between these concentric whorls of cells were occupied by loose fascicles of similarly bright eosinophilic spindle cells [Figure 3]. Smooth muscle differentiation was confirmed by the expression of three myogenic markers. The tumour cells were diffusely and uniformly, strongly reactive to Desmin, Actin, and Vimentin [Figure 4]. The strong cytoplasmic markers reactivity extended to both the cells arranged in whorls around the vascular channels and those arranged in short fascicles [Figure 3]. Based on the histopathological and immunohistochemical findings, a diagnosis of angioleiomyoma (vascular leiomyoma) was given.
Figure 3.
(a) Scanner view. (b) Scanner view. (c) Low power view.(d) High field view
Figure 4.
(a) Desmin positive. (b) Actin positive. (c) Vimentin positive
DISCUSSION
Leiomyoma is described by the World Health Organization as a tumour of soft tissue that arises from smooth muscle. It can be found in sites rich in smooth muscles, such as the gastrointestinal tract, the myometrium, and the skin. Leiomyoma originating from smooth muscle cells in vessels located in deep soft tissue is rare. Due to the lack of smooth muscle in the oral cavity, leiomyoma is relatively rare or uncommon. Possible sources of smooth muscle in the oral cavity include blood vessels, circumvallate papillae, and heterotopic smooth muscle.[1,2,3]
The highest prevalence of head and neck leiomyoma is observed in the 4th and 5th decade of life, with a peak prevalence occurring between 40 and 49 years of age.[4]
Several histological types of leiomyomata have been reported in the literature: solid, vascular (angiomyxoma or angioleiomyoma), and epithelioid. The vascular variant is the most frequent in the oral cavity. Our case involves the vascular type. Smooth muscle is scarce in the oral cavity; however, this region is rich in blood vessels. Therefore, it has been proposed that the media layer of blood vessels may be the origin of oral cavity vascular leiomyoma.[5]
In general, non-cutaneous head and neck leiomyomas are rare lesions. Only two leiomyomas were found by Fu and Perzine in a series review of 256 non-epithelial neoplasms of the sinonasal tract and nasopharynx. Barnes reviewed 257 leiomyomas of the head and neck and he found that 92 of them were associated with the cervical oesophagus, 58 with the skin of the head and neck, 52 with the oral cavity, 22 with the larynx, 12 with orbit, 6 with the nasal cavity, and the remaining were associated with the trachea, salivary glands, paranasal sinuses, thyroid gland, and intraosseous sites associated with the maxilla and mandible.[4]
In the head and neck, angioleiomyoma are found more frequently in the nasal cavity, paranasal sinuses, and oral cavity. In a study of 562 cases of angioleiomyomas. It is observed that 68% of the angiomyxomas occurred in the lower extremities, 22% in the upper extremities, and only 9% occurred in the head and neck.[4] Barnes reviewed 69 angioleiomyomas of the head and neck and reported that 31 cases were found in the oral cavity, most often in the lips (13), soft palate (8), tongue (5), buccal mucosa (3), gingiva (1) and uvula (1).[4]
To the best of our knowledge, this is the first case reported case of a Vascular Leiomyoma of the oral cavity occurring in the retromolar trigone region of a young male patient. This unique case contributes valuable insights into the clinical presentation and management of Vascular Leiomyoma in atypical locations and demographic groups. This tumour can be diagnosed across a wide age range, from 14 to 79 years. However, most tumours are seen from the 4th to the 6th decades of life.[1,3,6] Small tumours are asymptomatic. Large tumours produce mass effects, such as difficulty in closing the mouth, chewing, and swallowing. Tumours may occasionally become traumatized and ulcerated during oral function, which can result in discomfort and pain.[1,3,6] A tongue lesion has also been reported to occasionally cause numbness.[3]
The vascular leiomyoma is characterized by a well-defined proliferation of mesenchymal tapered cells with eosinophilic cytoplasm and elongated basophilic nuclei that show tapered endings (cigar-like shape nuclei). The vascular spaces, which are lined by a single layer of endothelial cells[6,7] are a constant feature of vascular leiomyoma.
Scientific literature on the immunohistochemical characteristics of leiomyoma is scarce.[7] Assessing their immune characteristics is important for differential diagnosis, specifically to rule out other neoplasia of soft tissue, mostly mesenchymal lesions with a predominance of fusiform cells. Smooth muscle actin corresponds to the alpha fraction of the actin chain; it is a specific immunomarker for smooth muscle, although it can also exhibit an immunoreaction in skeletal muscle. In all our cases, the neoplastic cells showed a positive immunoreaction to actin. Vimentin is a structural protein of the cytoplasm filaments of mesenchymal cells.[7] Its expression in our VLOC cases was observed in the cytoplasm of the neoplastic cell population.
Differential diagnosis of VLOC should include soft tissue neoplasia characterized by fusiform cells.[1] The solitary myofibroma of the oral cavity is a benign neoplasm characterized by the proliferation of fibroblasts and myofibroblasts.[7] It is most commonly observed between the 1st and 2nd decades of life, in contrast to leiomyomas, which are more frequent in the adult population. Histologically, solitary myofibromas are well-defined lesions with a cellular component of fusiform cells with tapered nucleus and undefined cytoplasm borders. The solitary myofibroma has an important vascular component; therefore, this neoplasm could show an angiopericytoma-like aspect with a peripheral desmoplastic reaction. The typical immunophenotype of myofibroma is very similar to that of leiomyoma, showing positive immunoreactivity against actin and vimentin. However, VLOC is desmin-positive, while myofibroma is desmin-negative.[7] Another differential diagnosis of VLOC is oral cavity myopericytoma.[8] Oral cavity myopericytoma shares clinical and histological characteristics with VLOC. The myopericytoma belongs to the myoid and pericytoid neoplasms. Histological characteristics include a tapered cellular population with elongated nucleus with round endings (cigar-shape), similar to those observed in vascular leiomyoma.[7] The intravascular variant of myopericytoma is a rare from characterized by an intravascular mass similar in appearance to a vascular leiomyoma.[3] On the other hand, the oral inflammatory myofibroblast tumour is a controversial lesion characterized by fusiform cells arranged in whorls.[6,8] The immunophenotype of oral inflammatory myofibroblast tumours shares some characteristics with vascular leiomyoma. Both lesions are vimentin-positive, but while leiomyomas are desmin-positive, oral inflammatory myofibroblast tumours show variable immunoreactivity against desmin.[6,8]
Leiomyomas must be carefully distinguished from their malignant counterpart, leiomyosarcoma, as both can present with a similar clinical picture. Although leiomyosarcoma presents with histologic features as leiomyoma, atypia, cellularity, pleomorphism, and necrosis may indicate of malignant disease. Mitotic activity represents the most reliable criterion for malignant behaviour.[9] Kumar and Cotran[10] stated that histological features indicative of smooth muscle malignancy includes more than 10 mitoses per 10 highpower fields (HPF), with or without cellular atypia, and 5–10 mitoses/10 HPF with atypia. Tumours with 1–4 mitoses are best considered as potentially malignant, especially if they are large and exhibit areas of necrosis and significant nuclear atypia.
Surgical excision is the treatment of choice for VLOC and should lead to the minimization of recurrences, offering an excellent prognosis. Despite the vascular origin of these lesions, excessive bleeding after excision is rare.
In conclusion, VLOC is the most common histologic type of oral leiomyoma, which is among the rarest of oral benign neoplasms. Histological and immunohistochemical examinations are fundamental for confirming the diagnosis and differentiating this entity from other benign lesions as well as malignant lesions like leiomyosarcoma. However, the classification of histologic subtype does not affect clinical manifestations or prognosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ranjan S, Singh KT. Gingival angioleiomyoma-infrequent lesion of oral cavity at a rare site. J Oral Maxillofac Pathol. 2014;18:107–10. doi: 10.4103/0973-029X.131928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fletcher C.D.M., Unni K. K., Mertens F., editors. WHO, Pathology and Genetics of Tumours of Soft Tissue and Bone. IARC Press; Geneva: 2002. [Google Scholar]
- 3.De Araújo GR, Costa SFDS, Mesquita RA, Gomez RS, Dos Santos JN, Pontes HAR, et al. Leiomyoma and leiomyosarcoma (primary and metastatic) of the oral and maxillofacial region: A clinicopathological and immunohistochemical study of 27 cases. Head Neck Pathol. 2022;16:294–303. doi: 10.1007/s12105-021-01336-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brooks JK, Nikitakis NG, Goodman NJ, Levy BA. Clinicopathologic characterization of oral angioleiomyomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:221–7. doi: 10.1067/moe.2002.125276. [DOI] [PubMed] [Google Scholar]
- 5.Barnes L. Tumors and tumor like lesions of soft tissue. In: Barnes L, editor. Surgical Pathology of Head and Neck. 2nd ed. New York: Marcel Dekker; 2001. pp. 912–5. [Google Scholar]
- 6.Tsuji T, Satoh K, Nakano H, Kogo M. Clinical characteristics of angioleiomyoma of the hard palate: Report of a case and an analysis of the reported cases. J Oral Maxillofac Surg. 2014;72:920–6. doi: 10.1016/j.joms.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 7.Gaitan Cepeda LA, Quezada Rivera D, Tenorio Rocha F, Leyva Huerta ER, Mendez Sánchez ER. Vascular leiomyoma of the oral cavity. Clinical, histopathological and immunohistochemical characteristics. Presentation of five cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2008;13:E483–8. [PubMed] [Google Scholar]
- 8.Veeresh M, Sudhakara M, Girish G, Naik C. Leiomyoma: A rare tumor in the head and neck and oral cavity: Report of 3 cases with review. J Oral Maxillofac Pathol. 2013;17:281–7. doi: 10.4103/0973-029X.119770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barrios-Sánchez GM, Dean-Ferrer A, Alamillos-Granados FJ, Ruiz-Masera JJ, Zafra-Camacho FM, García de Marcos JA, et al. Inflammatory pseudotumor of the parotid gland. Med Oral Patol Oral Cir Bucal. 2005;10:371–5. [PubMed] [Google Scholar]
- 10.Kumar V, Cotran RI. 7th ed. Philadelphia: Elsevier; 2004. Robbin's Basic Pathology; p. 1090. [Google Scholar]