Abstract
Nasopalatine duct cysts (NPDCs) are among the most common nonodontogenic cysts, typically located in the midline of anterior maxillary hard palate. They usually arise from the embryonic epithelial vestiges of the nasopalatine duct. NPDCs predominantly affect adult males, generally during their fourth decade of life. Clinically, they present as asymptomatic or occasionally painful, fluctuant or discharging swellings involving the hard palate. Radiographically, NPDCs are characterized by a well-defined, fairly corticated, inverted pear-shaped or heart-shaped radiolucency situated between the roots of the maxillary incisors. Histopathologically, NPDCs exhibit a wide spectrum of findings. The lining may be comprised of stratified squamous, pseudostratified ciliated columnar, columnar, or cuboidal epithelium, or a combination and transition of these types. The cystic capsule is fibrocollagenous and can exhibit certain unique features, such as neurovascular bundles, mucous glands, and cartilaginous rests. NPDCs are typically managed through surgical enucleation, and recurrences are rare. Herein, we present two cases of NPDCs, along with a brief overview of their origin, relevant diagnostic features, and management.
Keywords: Cyst, enucleation, incisive canal, nasopalatine duct, palate
INTRODUCTION
The nasopalatine duct cyst (NPDC) is the most common non-odontogenic cyst located in the midline of the anterior maxilla. It comprises approximately 4% of all jaw cysts. It is believed to arise from the embryonic remnants of the nasopalatine duct, located within the incisive canalicular space. Meyer first described the entity in 1914,[1] initially characterizing it as a supernumerary midline paranasal sinus and later as a median maxillary anterior cyst in 1931. The phrase NPDC was included in the WHO classification due to its association with the nasopalatine duct. NPDC is also occasionally termed as the incisive canal cyst, as it is found in close proximity to the incisive canal.[2,3]
The entity is most commonly observed in adults, primarily during the fourth decade of life, with a higher prevalence in males. NPDCs are typically located in the midline of maxillary hard palate, posterior to the central incisor teeth. The most common presenting symptom is an asymptomatic swelling, which may be fluctuant and located in the upper anterior hard palate. Occasionally, the swelling may be painful and associated with purulent discharge and/or displacement and divergence of adjacent tooth roots.[2,4]
Radiographically, NPDCs appear as well-defined and fairly corticated radiolucencies, which can be round, ovoid, inverted pear-shaped, or heart-shaped. These radiolucencies are located in the midline of the anterior hard palate, originating within the incisive canal. They are generally evident between and apical to the roots of the upper central incisors. The lamina dura and periodontal ligament space remain intact.[2,5]
Histopathologically, the NPDCs exhibit a variable spectrum. The cyst is usually lined by either pseudostratified columnar epithelium, stratified squamous epithelium, or a combination of both. Goblet cells may be present in the lining, and columnar or cuboidal epithelium can occasionally be observed. The cystic capsule is comprised of a fibro-collagenous component and may include large nerves, blood vessels, or cartilaginous rests. Mucous glands are often evident in many instances, and focal and patchy inflammatory infiltrate may be noted.[2,4,6]
NPDCs are managed through surgical enucleation, and recurrences are rare.[2]
Herein, we report two unique and interesting cases of patients with NPDC, along with their relevant follow-up. Both patients exhibit distinct clinico-radiological features and histopathological hallmarks, including prominent neurovascular bundles, which are not commonly observed in all cases.
CASE HISTORY
Case 1
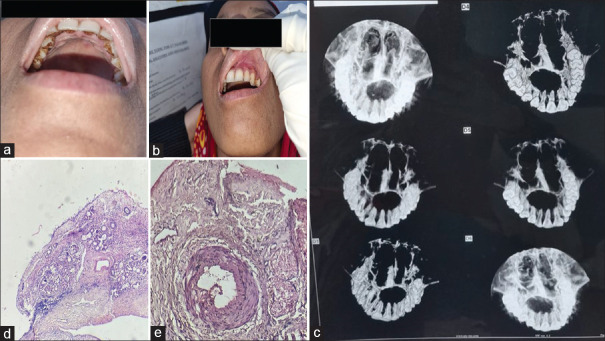
A 28-year-old female patient presented to the Oral Pathology Department with a complaint of discomfort associated with a swelling in the upper anterior jaw. The patient had no deleterious oral habits, and her medical and family histories were noncontributory. The haematological assays of the patient, including total count, differential count, bleeding time, clotting time, erythrocyte sedimentation rate, platelet count, international normalized ratio, haemoglobin (Hb %), fasting and post prandial blood glucose levels, were within normal limits. Intraoral examination revealed the presence of a slightly fluctuant soft tissue swelling in the anterior hard palatal region, extending from the 11 to 24 region, present for the past five months [Figure 1a and b]. The adjacent teeth were vital. Cone beam computed tomography (CBCT) of the maxilla revealed a slightly ovoid, unilocular, and well-defined fairly corticated radiolucency extending from the 12 to 25 regions [Figure 1c]. After obtaining relevant informed consent, surgical enucleation was performed on the cystic lesion, and the enucleated tissue was subjected to histopathological evaluation. Haematoxylin and eosin-stained sections showed a partially fragmented pseudostratified ciliated cystic epithelial lining, supported by a fibrocollagenous connective tissue wall of the cyst. The cystic capsule contained cross-sections of prominent nerve bundles, thick muscular arteries, and numerous coalescing foci of mucous glands within the depth of the fibrous capsule. Additionally, a moderately patchy inflammatory infiltrate was evident within the fibrous wall of the cyst. The overall histopathological features were highly suggestive of NPDC [Figure 1d and e]. The patient was followed up after three months, and the healing of the surgically enucleated area was satisfactory without any postoperative complications.
Figure 1.
(a) Presence of slightly fluctuant soft tissue swelling involving anterior hard palatal region and (b) labial vestibular aspect of the same subject. (c) CBCT of maxilla revealed slightly ovoid, unilocular, well defined fairly corticated radiolucency extending from 12 to 25 region. (d) (4x microscopic view) H & E stained sections revealed fragmented pseudostratified cliated cystic epithelial lining, being backed by fibrocollagenous connective tissue wall with numerous dispersed mucous glands and patchy inflammatory infiltrate and (e) (10x) shows fibrocollagenous capsule of cyst showing two prominent nerve bundles along with a thick muscular blood vessel
Case 2
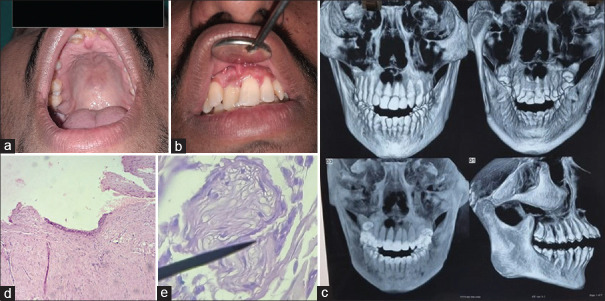
A 23-year-old male patient presented to the Oral Pathology Department with a complaint of discomfort and aesthetic concerns due to an enlargement in the upper anterior jaw. The patient had no deleterious oral habits, and both his medical and family histories were non-contributory. Haematological assays of the patient were within normal limits. Intraoral examination revealed the presence of a fluctuant and slightly compressible swelling in the anterior midline of the hard palate, extending from the 12 to 21 regions, with an enlarged incisive papilla and displaced 11 and 21 teeth [Figure 2a and b]. CBCT revealed the presence of a unilocular, well-defined, corticated radiolucency present between and apical to the roots of 12, 11, and 21 regions [Figure 2c]. After obtaining relevant informed consent, surgical enucleation was performed on the cystic lesion, and the enucleated tissue was subjected to histopathological evaluation. Sections stained with haematoxylin and eosin revealed the presence of a cystic lining composed of pseudostratified ciliated epithelium and stratified squamous epithelium, supported by a fibrocollagenous connective tissue capsule containing bundles of collagen fibres, a focal area with prominent cross-sections of nerve bundles, and patchy inflammatory infiltrate. The histopathological features were suggestive of NPDC [Figure 2d and e]. The patient was followed up for three months, and healing of the surgically enucleated area was satisfactory without any postoperative complications.
Figure 2.
(a) Intraoral examination revealed the presence of a fluctuant and slightly compressible swelling involving anterior midline of hard palate, tracing posteriorly, extending from 12 to 21 regions, with enlarged incisive papilla, and (b) displaced 11 and 21. (c) CBCT revealed the presence of a unilocular, well defined, corticated, radiolucency present in between and apical to roots of 12,11,21 region. (d) (4x magnification) H & E stained sections showed a combination of pseudostratified ciliated cystic lining along with parts of stratified squamous lining being backed by cystic capsule showing collagen fibre bundles and scanty inflammation and (e) (40x) showed fibrocollagenous connective tissue stroma showing a nerve bundle (indicated by black arrow)
DISCUSSION
NPDCs are infrequent, benign non-odontogenic cysts of the anterior maxilla, affecting approximately 1% of the population. They typically involve the anterior midline of hard palatal mucosa, located behind the incisors.[7] The present designation of the term nasopapaltine duct cyst or NPDC was adopted in the WHO classification of 1971 due to the cyst’s association with the nasopalatine duct.[2,3]
NPDCs are thought to originate from vestiges of the nasopalatine ductal, an embryonic developmental component that communicates between the oral and nasal apertures through the incisive canal. Due to this reason, NPDCs are sometimes referred to as incisive canal cysts. There are several theories regarding their origin- 1) According to one hypothesis, NPDCs arise from the spontaneous proliferation of nasopalatine duct remnants within the incisive canal. Bodin et al. (1986)[8] observed that approximately 50% of incisive canals contained remnants of nasopalatine ducts. Even in adulthood, stimuli such as trauma, infection, and inflammation may trigger this proliferation. 2) According to this theory, NPDCs originate from the entrapment of epithelial remnants during the embryonic fusion between the nasal cavity and anterior maxilla. 3) The presence of mucous glands near the nasopalatine ducts, and occasionally within the fibrous capsule of NPDCs, have led certain researchers to speculate that NPDCs might represent mucous extravasation or retention cysts.[2,4,5,9]
In general, NPDCs are thought to arise from the cystic degeneration of naso palatine ductal epithelial residues.
NPDCs commonly affect adults over a broad age range, ranging from 7 to 90 years. It is most commonly observed between 30 and 55 years of age, peaking during the fourth decade of life, as observed by Swanson et al., in a case series. It is quite rare in children and adolescents. Males are more frequently affected than females. In our case, the patients were a 28-year-old female and 23-year-old male, respectively.[2,10]
NPDCs most commonly affect the central portion of the hard palate, located behind the maxillary central incisors and in close proximity to the incisive papilla. Many cases present as an asymptomatic swelling of the anterior hard palate, often detected on routine radiographs, such as a maxillary occlusal radiograph. Other common presentations may include pain and purulent or mucoid discharge. Displacement of the regional incisor teeth may also occur. Similar findings were noted in the second patient, who showed displacement of the 11 and 21 teeth. However, there was no pain and discharge in either patients.[2,4,9]
Radiographs generally exhibit a well-circumscribed, fairly sclerotic radiolucency involving the anterior maxillary midline, situated between and above the roots of the central incisor teeth, or sometimes superimposed over the tooth roots. The radiolucency may appear inverted pear-shaped due to the resistance provided by the adjacent tooth roots. Occasionally, a heart-shaped radiolucency may be observed, resulting from the superimposition of the nasal spine. Displacement of the roots of the regional incisor teeth may also be evident, although root resorption is rare. In both of our patients, CBCT showed well-defined, fairly corticated radiolucencies in the anterior maxillary hard palatal regions, with tooth divergence noted in second patient.[5]
On gross and macroscopic analyses, the NPDCs may present with cystic and fibrous areas. The cystic lumen typically contains brownish fluid, with intermittent mucus or pus components.[2,4]
On histopathological examination, NPDCs exhibit a widely variable spectrum. It is characteristic to find more than one type of cystic epithelial lining, along with the presence of neurovascular bundles and glandular elements within the cystic wall. NPDCs may be composed of different types of cystic lining—stratified squamous epithelium, pseudostratified columnar epithelium, simple columnar, cuboidal epithelium, or a combination and transition between these types. The stratified squamous epithelial lining is the most commonly observed epithelium, which is usually thin, regular, and nonkeratinized, followed by pseudostratified columnar lining that resembles respiratory lining, often containing goblet or mucus cells and cilia. Cuboidal or columnar lining is less frequently seen and typically consists of 2–5 cell layers.[2,5,6,9]
In our first case, the cystic lining was of pseudostratified ciliated type, whereas in the second instance, the lining showed an amalgation between stratified squamous and pseudostratified ciliated lining.
The nature of the cystic lining in NPDCs is influenced by the vertical location of the cyst within incisive canal. Cysts that are in proximity to the oral cavity are usually lined stratified squamous epithelium, while those nearer to the nasal floor are comprised of pseudostratified columar cliated type epithelium, similar to respiratory lining.[5,6]
Swanson et al.[10] observed that 71.8% NPDCs are lined by squamous, columnar, cuboidal, or a combination of these epitheliums, but no respiratory epithelium. The epithelia may also exhibit metaplastic changes at times.
Barros et al.[11] evaluated the components of the fibrous cystic capsule in 30 NPDCs. Nerves in 15 (50%) NPDCs and minor mucous glands in 7 (23.3%) NPDCs were observed. The cyst wall is comprised of collagenous fibrous connective tissue with various distinguishing features. A valuable diagnostic feature is the presence of pronounced neurovascular bundles, including moderate to large nerve conglomerates within the capsule. Muscular arteries and numerous smaller veins are also observed in the wall of NPDCs. The presence of prominent neurovascular bundles can be attributed to the long sphenopalatine nerve and vessels that course through the incisive canals, which are removed during enucleation. Smaller mucous glandular foci or fibrosed glands have also been observed in the fibrous capsules of NPDC. Likewise, in our second case, the cyst capsule showed cross-sections of prominent nerve bundles, thick muscular arteries, and numerous coalescing foci of mucous glands at the depth of the fibrous capsule.[2,4,6,11]
The presence of inflammatory infiltrate within the fibrous capsule is variable, and it is usually focal or patchy and often associated with the presence of hyperplastic or proliferative squamous cystic epithelial linings. In our first case-, extremely focal patchy inflammation was noted, while in the second instance, a moderately patchy infiltrate was observed.[2,6]
Sometimes, epithelial remnants may be present in the capsule, representing cross-sectional fragments of small ducts, mucous glands, or remnants of nasopalatine duct. Rarely, rests of hyaline cartilage or adipose tissue might be observed in the cystic capsule of NPDCs.[4]
NPDCs should be differentiated from radicular cysts, lateral periodontal cysts, central haemangiomas and periapical granulomas, primordial cysts associated with mesiodens, and though rarely, chondrosarcomas arising from cartilaginous rests native to the incisive papilla or nasopalatine duct region.[5]
Although instances of malignant transformation of NPDC are extremely rare, there have been a few reported cases.[7]
NPDCs are managed surgically by total enucleation and curettage, with recurrences post-enucleation being infrequent.[7]
Timely diagnosis, with histopathological evaluation playing a gold standard role, and the institution of proper treatment through surgical enucleation, are crucial for achieving a favorable outcome for this rare entity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Key messages
NPDCs are relatively uncommon nonodontogenic cysts that typically present as asymptomatic or occasionally painful swellings. They generally involve the anterior hard palate and originates from the embryonic residues of the nasopalatine duct. The gold standard treatment is enucleation, followed by histopathological evaluation to rule out other common odontogenic entities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Meyer AW. A unique supernumerary paranasal sinus directly above the superior incisors. J Anat. 1914;48:118–29. [Google Scholar]
- 2.Speight PM. Shear's Cysts of the Oral and Maxillofacial Regions. 5th ed. Wiley Blackwell; 2022. Nasopalatine duct cyst; pp. 214–29. [Google Scholar]
- 3.Slootweg PJ, El-Naggar AK. World Health Organization 4th edition of head and neck tumor classification: Insight into the consequential modifications. Virchows Arch. 2018;472:311–3. doi: 10.1007/s00428-018-2320-6. [DOI] [PubMed] [Google Scholar]
- 4.Pathology outline--Martinez A. Nasopalatine duct cyst. Pathology Outlines.com website. [[Last accessed on 2023 Dec 08]]. Available from: https://www.pathologyoutlines.com/topic/mandiblemaxillanasopalatine.html .
- 5.Sun F, Dym H. Diagnosis and management of nasopalatine Duct Cyst: A report of two cases and literature review. N Y State J. 2023;89:28–32. [Google Scholar]
- 6.Chen IJ, Lai PT, Jin YT, Chiang CP. Nasopalatine duct cyst – Diagnosis from the content in the cystic wall. J Dent Sci. 2023;18:1449–51. doi: 10.1016/j.jds.2023.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lang MJ, Lee YP, Hwang MJ, Chiang CP. Nasopalatine duct cyst – Case report. J Dent Sci. 2021;16:1047–9. doi: 10.1016/j.jds.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bodin I, Issacsson G, Julin P. Cysts of the nasopalatine duct. Int J Oral Maxillofac Surg. 1986;15:696–706. doi: 10.1016/s0300-9785(86)80110-7. [DOI] [PubMed] [Google Scholar]
- 9.Neville BW, Damn DD, Allen CM, Chi AC. Oral and Maxillofacial Pathology. 4th ed. St Louis: Elsevier; 2016. Developmental defect of the oral &maxillofacial region; pp. 24–35. [Google Scholar]
- 10.Swanson KS, Kaugars GE, Gunsolley JC. Nasopalatine duct cyst: An analysis of 334 cases. J Oral Maxillofac Surg. 1991;49:268–71. doi: 10.1016/0278-2391(91)90217-a. [DOI] [PubMed] [Google Scholar]
- 11.Barros CCDS, Santos HBP, Cavalcante IL, Rolim LSA, Pinto LP, de Souza LB. Clinical and histopathological features of nasopalatine duct cyst: A 47-year retrospective study and review of current concepts. J Craniomaxillofac Surg. 2018;46:264–8. doi: 10.1016/j.jcms.2017.11.014. [DOI] [PubMed] [Google Scholar]