Abstract
This report presents the long-term (over 15 years) results of four Japanese patients who underwent total joint replacement for thumb carpometacarpal (CMC) joint arthritis. Four patients (mean age 60.5 years) underwent prosthesis replacement for thumb CMC joint arthritis with AVANTA(TM) (Small Bone Innovations, Morrisville, PA, USA) implants between 2001 and 2004, with a mean follow-up of 20 years and seven months. One patient was classified as Eaton stage 2 and three patients were classified as Eaton stage 3 prior to surgery. Although radiographs at the last follow-up showed loosening of the trapezium-side implant in all cases, three of the patients were excellent and only one was good according to Eaton's clinical criteria, and none of them reported severe pain or significant problems. Despite radiographic evidence of implant loosening and subsidence, long-term results were positive with minimal clinical symptoms. The results suggest that thumb CMC joint arthroplasty can provide satisfactory long-term results. However, the use of thumb CMC joint prostheses is currently limited in Japan, and alternative surgical methods such as suspension arthroplasty are more common. We believe that the thumb CMC joint prosthesis is as effective as any other surgical method based on the good results we have seen.
Keywords: arthroplasty, implant, long-term outcomes, prosthesis, thumb carpometacarpal joint arthritis
Introduction
Thumb carpometacarpal (CMC) joint arthritis is one of the most frequently encountered hand diseases in outpatient clinics, with a prevalence of 50.2% in Japan [1] because the CMC joint is loaded 12 times more than the phalanges during thumb pinch and is susceptible to osteoarthritis [2]. Thumb CMC joint arthritis is more common in postmenopausal women [3], who present with pain and swelling at the base of the thumb that interferes with activities of daily living, including household tasks. When the joint is refractory to orthotics or other conservative treatments, surgery is performed to relieve pain, restore a stable, mobile, and strong thumb, and achieve long-term stability [4,5]. Numerous surgical procedures are performed, including suspension arthroplasty, arthrodesis, and prosthesis [5]. The choice of surgical procedures varies widely from region to region. Especially in North America, suspension arthroplasty is mainly performed due to its good results. In contrast, the results of prostheses are reported to be poor, and the survey results show that the frequency of suspension arthroplasty is increasing every year [6]. However, prostheses are preferred as an effective treatment in Europe because of their good postoperative results [7]. The thumb CMC joint has the specific shape of a plyometric joint and is classified as a biaxial joint. AVANTA(TM) (Small Bone Innovations, Morrisville, PA, USA) implants are a resurfacing prosthesis that can reproduce a structure very close to the shape of the thumb CMC joint and can preserve the trapezium, which is subject to axial pressure [8] and were the implants used in the surgery we performed.
To the best of our knowledge, no literature on the long-term results of thumb CMC joint prostheses in Japanese patients has been published in English. We report the long-term results of four Japanese patients with thumb CMC joint prostheses over 15 years.
Case presentation
The details of the four patients who underwent surgery between 2001 and 2004 and were followed up for more than 15 years are shown in Table 1. The mean age at surgery was 60.5 years, and the mean follow-up period was 20 years and seven months. AVANTA(TM) (Small Bone Innovations, Morrisville, PA, USA) implants were used in all cases.
Table 1. Patient details.
E, Excellent; G, Good.
| Case No. | Age at surgery | Preoperative X-ray evaluation based on Eaton's classification | Surgical side | Follow-up term (Y: years, M: months) | X-ray evaluation at the final observation | Final pinch power (kg) (surgical side/contralateral side) | Eaton’s clinical criteria | |
| Implant loosening | Implant subsidence | |||||||
| 1 | 59 | 3 | L | 19Y2M | + | - | 4.0/3.0 | E |
| 2 | 60 | 3 | L | 21Y0M | + | - | 3.5/2.5 | E |
| 3 | 61 | 2 | R | 21Y9M | + | + | 4.0/1.0 | E |
| 4 | 62 | 3 | L | 20Y3M | + | + | 4.5/5.0 | G |
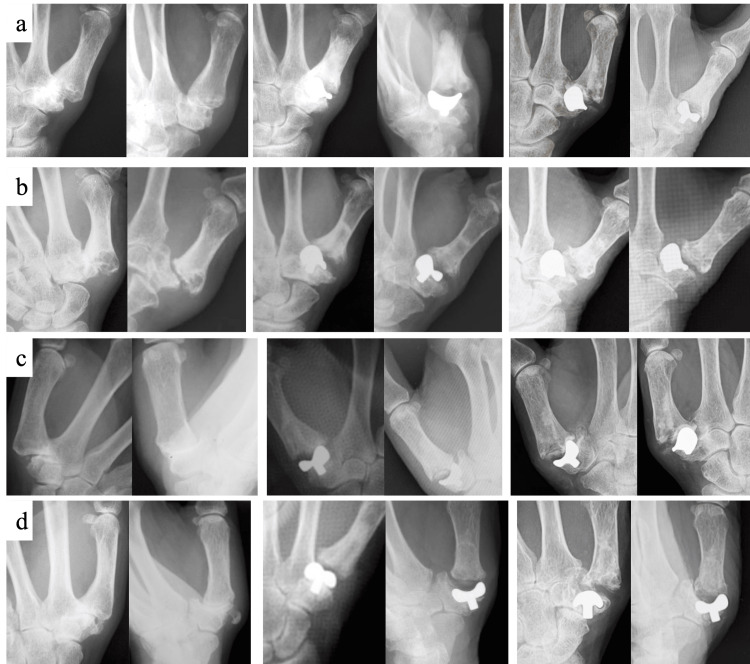
Two hand surgeons evaluated the patients’ radiographic findings. In disagreements regarding radiographic findings between the two surgeons, the final assessment was determined after discussion. According to Eaton’s classification in 1984 [4], preoperative radiographic evaluation revealed one case with stage 2 and three cases with stage 3. Radiographs taken immediately postoperatively and at the last follow-up are shown in Figure 1.
Figure 1. Postoperative radiographs (a: case 1, b: case 2, c: case 3, d: case 4): (left) preoperative, (middle) immediate postoperative, and (right) last observation (frontal and oblique views, respectively).
Although two cases showed implant subsidence on the trapezium side and all cases showed implant loosening on the final radiograph, none of the patients complained of pain or other complicated symptoms. The clinical evaluation at the final observation was based on Eaton’s clinical criteria (Table 2) [4], which was excellent in three cases and good in one case.
Table 2. Eaton’s clinical criteria [4].
Failures were not improved from preoperative status.
| Eaton's clinical criteria in 1984; results were classified as excellent, good, fair, or failure | |
| Excellent | No pain, pinch strength more than 90% of the contralateral thumb, and no instability |
| Good | Occasional pain after prolonged activity, pinch strength greater than 70% of the contralateral thumb, and minimum laxity |
| Fair | Frequent pain with average use, strength less than 70% of the contralateral thumb, or mild joint laxity but were better than preoperatively |
Our four cases are presented here. Case 1 was a 59-year-old woman who underwent surgery. Based on preoperative radiographs, the patient was diagnosed with stage 3 Eaton’s classification. Radiographs of the surgical site at 19 years and two months postoperatively showed some subsidence of the implant on the trapezium side and mild dislocation or subluxation of the joint. The tip pinch force was comparable to the contralateral side, and the outcome based on Eaton’s clinical criteria was excellent. Case 2 was a 59-year-old woman. Based on preoperative radiographs, the patient was diagnosed with stage 3 Eaton’s classification. Radiographs of the surgical site at 21 years postoperatively showed some subsidence of the implant on the trapezium side. The tip pinch force was comparable to the contralateral side, and the outcome based on Eaton’s clinical criteria was excellent. Case 3 was a 61-year-old woman. Based on preoperative radiographs, the patient was diagnosed with stage 2 Eaton’s classification. Radiographs of the surgical site at 21 years and nine months postoperatively showed some loosening and subsidence of the implant on the trapezium side. The tip pinch force of the operative side was much higher than the contralateral side because the nonoperative side of the CMC joint of the thumb was painful due to osteoarthritis and the pinch force of the nonoperative side was low. Case 4 was a 62-year-old woman. The patient complained of CMC joint pain and was diagnosed with stage 3 Eaton’s classification based on preoperative radiographs. Radiographs of the surgical site 20 years and three months postoperatively showed significant subsidence and loosening of the implant on the trapezium side and mild dislocation or subluxation of the joint. The tip pinch force was comparable to the contralateral side, and the outcome according to Eaton’s clinical criteria was good.
Discussion
The thumb CMC joint is potentially unstable, which is one of the reasons for its susceptibility to osteoarthritis [9]. The current mainstream prostheses for thumb CMC joint arthritis in Europe are “double-mobile” types with mobility on both the metacarpal bone and trapezium sides [10]. Although one of the main complications of thumb CMC joint prostheses is loosening of the trapezium implant and not the metacarpal implant, “double-mobile” implants have the advantage of improving joint laxity and placing less mechanical stress on the trapezium compared to simple prostheses (arthroplasty of the trapezium side only, or surface replacement of both the metacarpal bone and the trapezium), resulting in less loosening and better long-term results. In our study, there were no revision cases, even though our implants were only surface replacements for both metacarpal and trapezium sides, and not double-mobile types. This may be due to the ingenuity of the surgical procedure, particularly the improvement in joint stability with soft tissue reconstruction in addition to the prosthesis. Instability of the thumb CMC joint is mainly due to traction from the abductor pollicis longus (APL) [11]. Therefore, we used the dorsal approach in all cases, and after replacing the articular surfaces with prostheses, to achieve joint stability, the APL tendons are detached and reattached to the metacarpal base in an advanced position after implant placement in our surgical procedure.
According to a worldwide survey of 1138 hand surgeons, there were significant differences in the number of implant prostheses between the United States and Europe, with European hand surgeons reporting far higher numbers [12]. The long-term outcome of a thumb CMC joint prosthesis is generally considered to be poor [13,14]; therefore, the number of prostheses for thumb CMC joint arthritis has decreased, especially in North America, and non-implant arthroplasty, especially suspension arthroplasty, is now a major surgical procedure [15]. In contrast, several reports have compared prostheses with suspension arthroplasty for thumb CMC joint arthritis and found no difference in clinical outcomes and complications between the two [16,17]. A Norwegian registry study reported good results with thumb CMC joint prosthesis, with an overall 10-year survival rate of 90% [18]. Furthermore, according to a systematic review [17,19], the poor long-term outcome of thumb CMC joint prostheses was due to technical errors, such as implant malpositioning or poor indication with respect to the shape or bone quality of the trapezium.
In our four cases, the radiographic change at the last observation showed that the implants on the trapezium side had loosened in all patients, and two of them had sunk; however, only one patient complained of symptoms at the last observation, and it was mild. In addition, the final pinch force of the surgical side was more than 70% of that of the contralateral side in all cases. Since the previous reports of implant arthroplasty for thumb CMC joint arthritis showed a low correlation between radiographic and clinical symptoms [20], which is similar to our results, implant loosening or subsidence may not contribute to the long-term outcome. Unfortunately, at the time of writing this manuscript, implants for the thumb CMC joint have been commercially discontinued in Japan, only a few custom-made joint prostheses have been invented and used by some surgeons, and performing implant arthroplasty for the thumb CMC joint is now unrealistic for Japanese hand surgeons. Although osteotomy, arthrodesis, and non-implant arthroplasty are performed depending on the condition of each case, the optimal technique has not yet been determined. We believe that the results of this study may help to provide evidence that implant arthroplasty for thumb CMC joint arthritis is as good as other surgical methods.
This study has several limitations. First, this study is retrospective and lacks a control group. Second, although we were able to summarize the cases that could be followed up long-term, we did not include cases that dropped out during the study (it is possible that the cases with poor outcomes were mixed in the dropped-out cases). Third, patients with good clinical outcomes in the early postoperative period were more likely to be followed for a long period, i.e., there may be a selection bias. Finally, since this was only a single-center study and only a limited number of surgeons were involved in all the cases, our results may not be generalizable to all cases of thumb CMC joint arthritis.
Conclusions
Our cases with implant arthroplasty for the thumb CMC joint arthritis have showen that loosening or subsidence on radiographic findings after surgery are not always symptomatic and do not require revision, and they may not have a significant impact on clinical outcomes. Therefore, based on our cases with good long-term results, we believe that implant arthroplasty for thumb CMC joint arthritis with appropriate procedures of surrounding soft tissues may be a good surgical option similar to other methods.
Disclosures
Human subjects: Consent for treatment and open access publication was obtained or waived by all participants in this study. The Ethics Committee of Toho University Ohashi Medical Center, and the Ethical Committee of International University of Health and Welfare (IUHW) issued approval H23126 (Toho University), and 20-Nr-014 (IUHW).
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Masanori Nakayama, Hiroyasu Ikegami
Acquisition, analysis, or interpretation of data: Masanori Nakayama, Takanori Shintaku, Hideaki Ishii, Mitsuru Yagi
Drafting of the manuscript: Masanori Nakayama, Takanori Shintaku
Critical review of the manuscript for important intellectual content: Masanori Nakayama, Hideaki Ishii, Mitsuru Yagi, Hiroyasu Ikegami
Supervision: Hiroyasu Ikegami
References
- 1.Prevalence of hand osteoarthritis and its relationship to hand pain and grip strength in Japan: the third survey of the ROAD study. Kodama R, Muraki S, Oka H, et al. Mod Rheumatol. 2016;26:767–773. doi: 10.3109/14397595.2015.1130673. [DOI] [PubMed] [Google Scholar]
- 2.Biomechanical analysis of static forces in the thumb during hand function. Cooney WP 3rd, Chao EY. https://journals.lww.com/jbjsjournal/pages/articleviewer.aspx?year=1977&issue=59010&article=00004&type=Abstract. J Bone Joint Surg Am. 1977;59:27–36. [PubMed] [Google Scholar]
- 3.Osteoarthritis of the trapeziometacarpal joint: the pathophysiology of articular cartilage degeneration. I. Anatomy and pathology of the aging joint. Pellegrini VD Jr. J Hand Surg Am. 1991;16:967–974. doi: 10.1016/s0363-5023(10)80054-1. [DOI] [PubMed] [Google Scholar]
- 4.Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. Eaton RG, Lane LB, Littler JW, Keyser JJ. J Hand Surg Am. 1984;9:692–699. doi: 10.1016/s0363-5023(84)80015-5. [DOI] [PubMed] [Google Scholar]
- 5.Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. Vermeulen GM, Slijper H, Feitz R, Hovius SE, Moojen TM, Selles RW. J Hand Surg Am. 2011;36:157–169. doi: 10.1016/j.jhsa.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 6.Evidence-Based Practice in the Surgical Treatment of Thumb Carpometacarpal Joint Arthritis. Yuan F, Aliu O, Chung KC, Mahmoudi E. J Hand Surg Am. 2017;42:104–112. doi: 10.1016/j.jhsa.2016.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Total joint replacement for osteoarthritis of the carpometacarpal joint of the thumb: why and how? Duerinckx J, Verstreken F. EFORT Open Rev. 2022;7:349–355. doi: 10.1530/EOR-22-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Total arthroplasty of the thumb trapeziometacarpal joint. Cooney WP, Linscheid RL, Askew LJ. https://journals.lww.com/corr/abstract/1987/07000/total_arthroplasty_of_the_thumb_trapeziometacarpal.6.aspx. Clin Orthop Relat Res. 1987;220:35–45. [PubMed] [Google Scholar]
- 9.Metacarpophalangeal joint instability in trapeziometacarpal osteoarthritis: a systematic review. Degeorge B, Chiche L, Coulet B, Lazerges C, Chammas M. Hand Surg Rehabil. 2021;40S:0–34. doi: 10.1016/j.hansur.2020.05.013. [DOI] [PubMed] [Google Scholar]
- 10.ISIS trapeziometacarpal arthroplasty: what are the outcomes in male patients? Buffet A, Lucot-Royer L, Pichonnat M, Menu G, De Bie A, Obert L, Loisel F. Hand Surg Rehabil. 2022;41:463–469. doi: 10.1016/j.hansur.2022.04.007. [DOI] [PubMed] [Google Scholar]
- 11.Thumb carpometacarpal instability. Rabinovich RV, Polatsch DB, Shin SS, Beldner S. J Am Acad Orthop Surg. 2021;29:943–950. doi: 10.5435/JAAOS-D-21-00310. [DOI] [PubMed] [Google Scholar]
- 12.Geographical differences in carpometacarpal joint osteoarthritis treatment of the thumb: A survey of 1138 hand surgeons from the USA and Europe. Cerny MK, Aitzetmueller MM, Stecher L, Brett EA, Machens HG, Duscher D, Erne H. J Plast Reconstr Aesthet Surg. 2021;74:1854–1861. doi: 10.1016/j.bjps.2020.12.040. [DOI] [PubMed] [Google Scholar]
- 13.Ivory arthroplasty for trapeziometacarpal joint arthritis in men: analysis of clinical outcome and implant survival. Vanmierlo B, Buitenweg J, Vanmierlo T, Van Royen K, Bonte F, Goubau J. Hand (N Y) 2022;17:440–446. doi: 10.1177/1558944720930297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arpe total joint arthroplasty for trapeziometacarpal osteoarthritis: 80 thumbs in 63 patients with a minimum of 10 years follow-up. Dumartinet-Gibaud R, Bigorre N, Raimbeau G, Jeudy J, Saint Cast Y. J Hand Surg Eur Vol. 2020;45:465–469. doi: 10.1177/1753193420909198. [DOI] [PubMed] [Google Scholar]
- 15.Trapeziectomy with ligament reconstruction and tendon interposition versus trapeziometacarpal joint replacement for thumb carpometacarpal osteoarthritis: a systematic review and meta-analysis. Qureshi MK, Halim UA, Khaled AS, Roche SJ, Arshad MS. J Wrist Surg. 2022;11:272–278. doi: 10.1055/s-0041-1731818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Long term outcome of trapeziectomy with ligament reconstruction/tendon interposition versus thumb basal joint prosthesis. Vandenberghe L, Degreef I, Didden K, Fiews S, De Smet L. J Hand Surg Eur Vol. 2013;38:839–843. doi: 10.1177/1753193412469010. [DOI] [PubMed] [Google Scholar]
- 17.Trapeziometacarpal prosthesis: an updated systematic review. Remy S, Detrembleur C, Libouton X, Bonnelance M, Barbier O. Hand Surg Rehabil. 2020;39:492–501. doi: 10.1016/j.hansur.2020.08.005. [DOI] [PubMed] [Google Scholar]
- 18.The results of 479 thumb carpometacarpal joint replacements reported in the Norwegian Arthroplasty Register. Krukhaug Y, Lie SA, Havelin LI, Furnes O, Hove LM, Hallan G. J Hand Surg Eur Vol. 2014;39:819–825. doi: 10.1177/1753193413513988. [DOI] [PubMed] [Google Scholar]
- 19.Joint replacement for trapeziometacarpal osteoarthritis: implants and outcomes. Bæk Hansen T. J Hand Surg Eur Vol. 2021;46:115–119. doi: 10.1177/1753193420917582. [DOI] [PubMed] [Google Scholar]
- 20.Associations between radiographic features, clinical features and ultrasound of thumb-base osteoarthritis: A secondary analysis of the COMBO study. Shi Y, Fu K, Oo WM, et al. Int J Rheum Dis. 2022;25:38–46. doi: 10.1111/1756-185X.14248. [DOI] [PMC free article] [PubMed] [Google Scholar]