Abstract
From January 2001 through June 2002, 128 consecutive patients undergoing lung resection for various diseases were evaluated preoperatively by a cardiologist at our institution in order to predict postoperative cardiac complications in pulmonary surgery. Our assessment algorithm consisted of the following: Smoking, hypertension, hyperlipidemia, advanced age, diabetes mellitus, and history of cardiac disease or angina pectoris were considered as risk factors. A stress test was performed when at least 2 of the first 3 risk factors or at least 1 of the last 3 risk factors was present. Coronary angiography was performed in the case of a positive stress test. Patients were classified as low-risk when there was no need for a stress test. Patients were considered as intermediate-risk when a stress test revealed no ischemia or if there was a history of congestive heart failure or valvular disease. Patients in whom coronary artery disease was detected on angiography were classified as high-risk. Ninety-five of our patients were in the low-risk group, and 29 were in the intermediate-risk group.
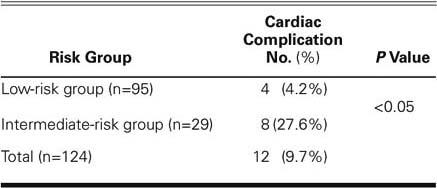
After lung resection, cardiac complications developed in 4 patients in the low-risk group (atrial fibrillation) and in 8 patients in the intermediate-risk group (5 atrial fibrillation and 3 paroxysmal atrial tachycardia). The overall cardiac complication rate was 9.7%. No death occurred due to cardiac events. The difference in the incidence of arrhythmias between the low- and the intermediate-risk groups was significant (P <0.05). We present this simple algorithm for preoperative cardiac evaluation in patients scheduled to undergo lung resection, and we suggest that it may be possible to predict postoperative cardiac complications with this method.
Key words: Arrhythmia, heart diseases/classification/complications/history, prospective studies, postoperative complications, prognosis, pulmonary resection, risk factors, thoracic surgery
Preoperative cardiac evaluation of patients undergoing lung resection is of great importance, because cardiac problems are the 2nd-most-common postoperative complication in thoracic surgery.1 Supraventricular arrhythmias constitute most of the cardiac complications and are well documented, but their published incidence varies widely.2 The commonly used cardiac risk indices for noncardiac surgery have been introduced by Goldman,3 Detsky,4 Larsen,5 and their associates. The value of these indices has been confirmed in large prospective series, but mostly in general surgical patients.3–5 In an effort to predict postoperative cardiac complications, we used a new algorithm to prospectively evaluate patients undergoing pulmonary resection from January 2001 through June 2002.
Patients and Methods
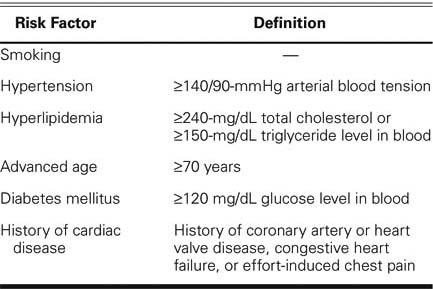
At the thoracic surgery clinic of our institution, 128 consecutive patients undergoing elective pulmonary resection for various diseases were enrolled in the study. Types of resection included segmentectomy, lobectomy, bilobectomy, and pneumonectomy. Routine preoperative examinations included a thorough cardiac history, physical examination, laboratory tests, chest radiography, and electrocardiography. All findings were evaluated preoperatively by one consulting cardiologist. In accordance with our proposed algorithm, smoking history, hypertension, hyperlipidemia, advanced age, diabetes mellitus, and history of cardiac disease (coronary artery disease, heart valve disease, or congestive heart failure) or angina pectoris were considered as risk factor determinants. Arterial blood tension greater than 140/90 mmHg was accepted as hypertension, and a total cholesterol level of 240 mg/dL or a blood triglyceride level of 150 mg/dL was considered a borderline limit for hyperlipidemia (Table I). A stress test was performed when at least 2 of the first 3 risk factors or at least 1 of the last 3 risk factors was present. Echocardiography was performed when indicated. Coronary angiography was performed when the stress test was positive for ischemia. Patients were classified as low-risk when there were no risk factors or in the presence of a negative stress test with risk factors, and as intermediate-risk when coronary artery disease was present without ischemia on stress test or when there was a history of congestive heart failure or valvular disease. Coronary angiography was performed in the case of a positive stress test. Patients in whom angiography showed coronary artery disease and documented ischemia were classified as high-risk. We classified patients as intermediate-risk even when stress test or coronary angiography results were negative, because the need for these further studies implied some risk for the planned operation.
TABLE I. Preoperative Cardiac Risk Determinants
Patients in the low-risk group underwent surgery without any further testing. All patients in the intermediate-risk group received nitrate therapy and β-blockers unless there were contraindications such as a heart rate less than 60 beat/min, blood pressure less than 90/60 mmHg, or severe bronchoconstriction. Statin therapy was given if indicated. Aspirin was discontinued 10 days before the operation.
All pulmonary resections were performed through a standard posterolateral thoracotomy incision. After the operation, patients were extubated in the operating room, and they were observed in the intensive care unit by cardiac and respiratory monitoring. Electrocardiograms were obtained at 0, 12, 24, and 48 hours postoperatively and examined by the cardiologist. In the case of a cardiac problem, appropriate medication was given. Patients were closely observed during the perioperative and postoperative courses. The high-risk group patients were not evaluated postoperatively in this study.
Statistical Analysis.
Data are presented as mean ± standard deviation. The 2-tailed Fisher's exact test was used for comparison of the groups. A P value of less than 0.05 was considered statistically significant.
Results
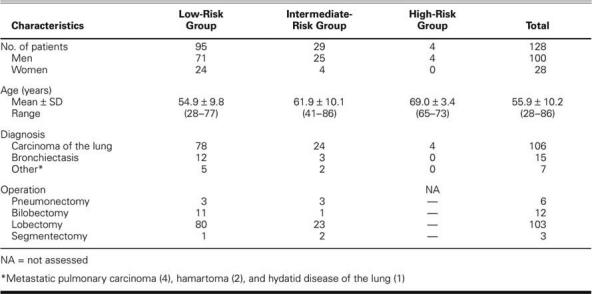
The study comprised 128 consecutive patients, 100 men and 28 women, whose ages ranged from 28 to 86 years (mean, 55.9 ± 10.2 years). Ninety-five of the patients were in the low-risk group, and 29 patients were in the intermediate-risk group. Postoperative results in the 4 high-risk patients were not recorded for the purposes of this study. Of the 124 recorded procedures, 6 were pneumonectomies; 12, bilobectomies; 103, lobectomies; and 3, segmentectomies. The general characteristics of the patients are summarized in Table II.
TABLE II. General Features of the Patients
Four patients (4.2%) in the low-risk group and 8 (27.6%) in the intermediate-risk group developed cardiac complications postoperatively (P <0.05) (Table III). The type of cardiac abnormality was atrial fibrillation in all of the patients in the low-risk group. In the intermediate-risk group, 5 patients developed atrial fibrillation and 3 developed paroxysmal atrial tachycardia. Sinus tachycardia, mainly due to intravascular fluid depletion or postoperative pain, was not considered as a postoperative cardiac complication. No problem related to myocardial ischemia was detected. There was no death related to a cardiac complication.
TABLE III. Cardiac Complications Detected in Low- and Intermediate-Risk Groups
Surgery was postponed in 1 of the 4 patients in the high-risk group. The other 3 patients had ischemia in the left anterior descending coronary artery (LAD) territory and underwent concomitant cardiac and pulmonary operations. Two of the patients underwent coronary artery bypass grafting (CABG) on a beating heart. In 1 of these patients, a left internal mammary artery (LIMA)–LAD anastomosis and left lower lobectomy were performed through 2 different incisions (median sternotomy and posterolateral thoracotomy). In the second of these patients, a right upper lobe apical segmentectomy and a LIMA–LAD anastomosis were performed through a median sternotomy. The 3rd patient had CABG (LIMA–LAD and saphenous vein graft–right coronary artery anastomoses) and right upper lobe anterior segmentectomy under cardiopulmonary bypass.
Discussion
The most common complication seen after lung resection is supraventricular tachycardia; its incidence varies from 10% to 28%.6 In a study of 121 patients reported by Oka and Ozawa,7 the incidence of supraventricular arrhythmia was 22.3%. In another study in which 298 patients were evaluated, the incidence of postoperative atrial fibrillation was 8.4% and was seen in 24% of patients after pneumonectomy.8 In a similar study consisting of 136 patients undergoing pneumonectomy, Harpole and coworkers9 found that 24% of the patients developed supraventricular arrhythmias, and the incidence increased with extrapleural pneumonectomy and right-sided procedures. Curtis and colleagues10 reported that pulmonary resection was frequently followed by atrial fibrillation and that its development seemed to be associated with pneumonectomy but not with the magnitude of pulmonary resection.
In our study of 124 patients in low- and intermediate-risk groups, the incidence of arrhythmia was 9.7%. This is lower than the incidence reported in the English-language medical literature. This might be explained by the limited number of patients and the large percentage of lobectomy operations in the study. However, we believe that preoperative cardiac evaluation, measures taken accordingly, and the exclusion of high-risk patients who underwent revascularization procedures along with lung resection may have played a role. Another limitation of the study is that the relationship between postoperative arrhythmias and the magnitude of lung resection was not evaluated. Since the types of resection were similar in both groups, it can be speculated that the magnitude of resection had no effect on arrhythmia development.
Algorithms that predict cardiac complications after noncardiac operations have been proposed. In a clinical risk index that was generated by Goldman and associates3 in 1977 and modified by Detsky and coworkers4 in 1986, 4 risk categories were established on the basis of clinical and laboratory variables. Larsen and colleagues,5 in a study consisting of 2,609 patients undergoing noncardiac surgery, found congestive heart failure, ischemic heart disease, diabetes mellitus, a serum creatinine level above 0.13 mmol/L, emergency surgery, and the type of operation to be the 6 perioperative predictors of postoperative cardiac risk. In their model, the type of operation was evaluated in 2 categories: aortic and all other surgeries. Although age over 70 years was considered as a risk factor by Goldman,3 Detsky,4 and their associates, it was not taken into consideration by Larsen and colleagues.5 Another cardiopulmonary risk index was proposed by Epstein and coworkers11 for preoperative evaluation of thoracic surgery patients; however, Melendez and Carlon12 stated that this index was inadequate to predict complications after thoracic surgery.
In developing our algorithm for the preoperative evaluation of patients undergoing lung resections, we took into consideration the risk assessments mentioned above. Smoking, hypertension, hyperlipidemia, advanced age, diabetes mellitus, and history of cardiac disease or angina pectoris were designated as risk factors. In designing such algorithms, another consideration is the extent to which cardiac evaluation should be performed in a patient undergoing pulmonary resection. The extent of resection and the patient's individual characteristics are very important in planning cardiac evaluation. Such an evaluation can lower costs, and unneeded tests can be avoided. Therefore, we believe that the presented algorithm takes the major details into consideration, is effective, and is simple to use in the daily clinical practice of thoracic surgery.
Footnotes
Address for reprints: Ufuk Cagirici, MD, Ege Universitesi Tip Fakultesi, Gogus Kalp Damar Cerrahisi Anabilim Dali, Bornova - Izmir 35100, Turkey. E-mail: cagirici@med.ege.edu.tr
References
- 1.Alexander JC Jr, Anderson RW. Preoperative cardiac evaluation of the thoracic surgical patient and management of perioperative cardiac events. In: Shields TW, LoCicero J, Ponn RB, editors. General thoracic surgery. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2000. p. 305–13.
- 2.Asamura H, Naruke T, Tsuchiya R, Goya T, Kondo H, Suemasu K. What are the risk factors for arrhythmias after thoracic operations? A retrospective multivariate analysis of 267 consecutive thoracic operations. J Thorac Cardiovasc Surg 1993;106:1104–10. [PubMed]
- 3.Goldman L, Caldera DL, Nussbaum SR, Southwick FS, Krogstad D, Murray B, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977; 297:845–50. [DOI] [PubMed]
- 4.Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery. A multifactorial clinical risk index. Arch Intern Med 1986;146:2131–4. [PubMed]
- 5.Larsen SF, Olesen KH, Jacobsen E, Nielsen H, Nielsen AL, Pietersen A, et al. Prediction of cardiac risk in non-cardiac surgery. Eur Heart J 1987;8:179–85. [DOI] [PubMed]
- 6.von Knorring J, Lepantalo M, Lindgren L, Lindfors O. Cardiac arrhythmias and myocardial ischemia after thoracotomy for lung cancer. Ann Thorac Surg 1992;53:642–7. [DOI] [PubMed]
- 7.Oka T, Ozawa Y. Correlation between intraoperative hemodynamic variability and postoperative arrhythmias in patients with pulmonary surgery [in Spanish]. Masui 1999; 48:118–23. [PubMed]
- 8.Dyszkiewicz W, Skrzypczak M. Atrial fibrillation after surgery of the lung: clinical analysis of risk factors. Eur J Cardiothorac Surg 1998;13:625–8. [DOI] [PubMed]
- 9.Harpole DH, Liptay MJ, DeCamp MM Jr, Mentzer SJ, Swanson SJ, Sugarbaker DJ. Prospective analysis of pneumonectomy: risk factors for major morbidity and cardiac dysrhythmias. Ann Thorac Surg 1996;61:977–82. [DOI] [PubMed]
- 10.Curtis JJ, Parker BM, McKenney CA, Wagner-Mann CC, Walls JT, Demmy TL, Schmaltz RA. Incidence and predictors of supraventricular dysrhythmias after pulmonary resection. Ann Thorac Surg 1998;66:1766–71. [DOI] [PubMed]
- 11.Epstein SK, Faling LJ, Daly BD, Celli BR. Predicting complication after pulmonary resection. Preoperative exercise testing vs a multifactorial cardiopulmonary index. Chest 1993;104:694–700. [DOI] [PubMed]
- 12.Melendez JA, Carlon VA. Cardiopulmonary risk index does not predict complications after thoracic surgery. Chest 1998; 114:69–75. [DOI] [PubMed]


