Abstract
Conservative laparoscopic torsioning with or without cystectomy or oophoropexy has emerged as a promising approach for the management of ovarian torsion, particularly in pediatric populations. We sought to understand the efficacy of this approach. We comprehensively reviewed the relevant literature. We formulated a search strategy by combining keywords related to laparoscopic surgery, conservative management, and ovarian torsion in pediatric and adolescent populations. Data were retrieved from Web of Science, PubMed, Medline, Cochrane Library, and ClinicalTrials. The Gov and Scopus databases. Eligible articles met the following criteria: Involved pediatric or adolescent populations with ovarian or adnexal torsion and evaluating the use of any method of laparoscopic torsioning surgery. We included the following outcomes; recurrence, conversion to laparotomy, need for oophorectomy, mean time to the onset of symptoms, abdominal pain at the time of presentation, fever, and evidence of ovarian function on postoperative ultrasound. In our meta-analysis, conducted using OpenMeta[Analyst], we analyzed both continuous and dichotomous data with mean difference and risk ratio, respectively, along with 95% confidence intervals (CI). First, the incidence of recurrence was reported in five studies, where 17 cases experienced recurrence out of 391 cases experienced recurrence. Additionally, instances requiring open surgery were documented in five studies, with 22 out of 360 cases requiring this conversion to open surgery, resulting in a combined ratio of 0.051 [95% CI (0.018, 0.083), p=0.02]. Moreover, six studies provided data on cases necessitating oophorectomy, with 27 out of 437 cases requiring the procedure. Furthermore, the mean time from symptom onset to surgery was 51.9 h. Abdominal pain was prevalent at presentation, affecting 264 out of 324 patients. Fever was less frequently reported, with 19 out of 324 patients experiencing it. Finally, a high percentage of patients showed evidence of ovarian function on postoperative ultrasound, with a pooled proportion of 0.69. Our analysis performed the conservative management of ovarian torsion in young women. Recurrence occurred in 17 out of 391, and 22 out of 360 required conversion to open surgery. Furthermore, oophorectomy was necessary in 27 of 437 patients, and the mean time from symptom onset to surgery was 51.9 h. Abdominal pain was the most common symptom, affecting 264 out of 324 cases, whereas fever was less common.
Keywords: Torsion, pediatrics, conservative management, laparoscopy
Öz
Sistektomi veya ooforopeksi ile birlikte veya bunlar olmaksızın konservatif laparoskopik detorsiyon, özellikle pediatrik popülasyonlarda over torsiyonunun tedavisinde umut verici bir yaklaşım olarak ortaya çıkmıştır. Veriler Web of Science, PubMed, Medline, Cochrane Library, ClinicalTrials.Gov ve SCOPUS veri tabanlarından elde edildi. İlk olarak, toplam 391 olgudan 17’sinde nüks görüldüğü beş çalışmada nüks insidansı bildirilmiştir. Ek olarak, açık cerrahi gerektiren olgular 5 çalışmada belgelenmiştir. Üç yüz altmış olgudan 22’sinde açık cerrahiye geçilmesi gerekmiştir ve bu da 0,051’lik bir birleşik oranla sonuçlanmıştır [%95 güven aralığı (0,018-0,083), p=0,02]. Ayrıca, 6 çalışma ooferektomi gerektiren vakalar hakkında veri sağlamıştır ve 437 olgudan 27’sinde bu prosedür gerekmiştir. Ayrıca, semptomların başlangıcından ameliyata kadar geçen ortalama süre 51,9 saat olarak bildirilmiştir. Başvuru sırasında karın ağrısı sık olarak bildirilmiştir ve 324 olgunun 264’ünü etkilemiştir. Ateş daha az sıklıkla rapor edilmiş olup 324 olgunun 19’unda görülmüştür. Son olarak, genel olarak, ameliyat sonrası ultrasonda yumurtalık fonksiyonuna dair kanıt bulunan hastaların oranı yüksek olup, havuzlanmış oran 0,69’dur. Analizimiz genç kadınlarda over torsiyonunun konservatif tedavisini değerlendirdi. Rekürrens 391 olgunun 17’sinde görüldü ve 360 olgunun 22’sinde açık cerrahiye geçilmesi gerekti. Ayrıca, 437 olgunun 27’sinde ooferektomi gerekti ve semptom başlangıcından ameliyata kadar geçen ortalama süre 51,9 saatti. Karın ağrısı 324 olgunun 264’ünü etkileyen baskın bir semptomken, ateş daha az görüldü.
Keywords: Torsiyon, pediatri, konservatif tedavi, laparoskopi
Introduction
Ovarian and adnexal torsion are rare but critical gynecologic emergencies. The prevalence among women aged 18 years was approximately 4.9 per 100,000 individual(1). Approximately 3% of acute abdominal pain cases in children where urgent surgical intervention is required(2). This syndrome describes torsion of the ovary and vascular pedicle, thereby interrupting blood flow. Consequently, Ischemia and necrosis may occur if not promptly treated. In children, this condition can also present with non-specific symptoms such as severe abdominal pain, nausea, and vomiting(3, 4). Several factors might be implicated in the ovarian torsion of children, ranging from anatomical abnormalities to unusual presentation of ovarian masses, or even hormonal variations(5). Timely diagnosis is vital to avoid complications and to preserve the function of the ovaries. Unfortunately, many times the diagnosis remains undetermined due to the condition’s inconsistent presentation and the potential overlap with other intra-abdominal pathologies in children. Imaging techniques, including ultrasound (US) and magnetic resonance imaging, have an undoubtedly significant role in making a diagnosis; however, clinical awareness and suspicion are also critically important components to accurate diagnosis(6, 7). Despite advancements in diagnostic methods and treatment approaches, challenges persist in the diagnosis of ovarian torsion in children. Thus, a collaborative, multidisciplinary approach involving pediatricians, gynecologists, and radiologists is crucial to improve outcomes and mitigate complications effectively(8). The conventional treatment for ovarian torsion has typically favored oophorectomy over detorsion because of concerns about post-detorsion thromboembolic events, as well as the risks of peritonitis or infection from the presence of a necrotic ovary in the abdomen. However, there is a growing trend toward conservative, ovary-sparing management, which recognizes its advantages over oophorectomy. In the USA, the rates of conservative management have increased from approximately 20% of all surgically managed ovarian torsion cases in 2001 to just over 25% in 2015(8). Conservative procedures typically involve accessing the abdominal cavity via laparoscopy and performing detorsion to restore normal vascular supply to the ovaries, and may include oophoropexy or cystectomy(9). In our analysis, we aimed to investigate the efficacy and perioperative complications of laparoscopic procedures to conserve the ovaries in pediatric or adolescent patients and to analyze recent population-based patterns in the surgical treatment of ovarian torsion.
Methodology
Our study adhered to the PRISMA guidelines and recommendations(10). We formulated a search strategy by combining keywords related to laparoscopic surgery, conservative management, and ovarian torsion in pediatric and adolescent populations. We included all studies that considered themselves to be inclusive of a population that was described to be “child/(ren),” “young,” “pediatric” or “adolescent” and excluded any studies that included at least one participant that was referenced as being an “adult” or included participants that were shown by the data to be greater than 18 years of age at time of study inclusion. Data were retrieved from Web of Science, PubMed, Medline, Cochrane Library, and ClinicalTrials. The Gov and Scopus databases.
Study Selection
The titles and abstracts were initially screened, followed by full-text screening. Eligible articles met the following criteria. First, we only included studies involving pediatric and adolescent females with ovarian or adnexal torsion in which the investigators evaluated management with laparoscopic torsioning or oophorectomy. We only included studies that reported on at least one of our preselected outcomes, which included recurrence rates, conversion to laparotomy rates, the need for oophorectomy, mean time to the onset of symptoms, abdominal pain at the time of presentation, fever, and follicular changes in postmenarche females. We chose to include randomized control trials (RCTs) and observational studies, excluding reviews, surveys, abstracts, and meta-analyses. Ultimately, no RCTs have been found on this topic. We did not restrict study selection by language or country of origin.
Quality Assessment
The NHLB quality assessment tools were used to assess the quality of the observational studies. Each study’s risk of bias was categorized as low, high, or unclear(11).
Data Extraction
Data were extracted into three categories: patient demographics and baseline data, outcomes including recurrence, conversion to laparotomy, need for oophorectomy, mean time to the onset of symptoms, abdominal pain at the time of presentation, fever, evidence of ovarian function on a postoperative US, and data related to the quality assessment. Microsoft Excel was used to facilitate data collection.
Statistical Analysis
OpenMeta[Analyst](12) was used for the meta-analysis. Continuous data were analyzed using the mean difference and risk ratio for dichotomous outcomes, with a 95% confidence interval (CI). The fixed-effects and random-effects models were applied to the homogeneous and heterogeneous data, respectively. Heterogeneity was determined using the I2 and chi-square tests. Heterogeneity was indicated by p<0.1 or I2>50%.
Results
Results of our literature search
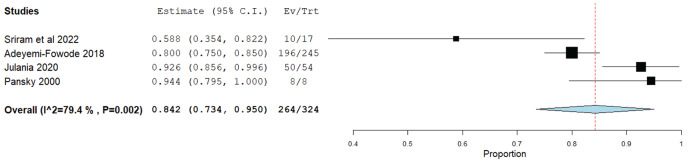
Our review of the literature is depicted in Figure 1 using a PRISMA diagram. We identified seven articles(13, 14, 15, 16, 17, 18, 19) that satisfied our inclusion criteria and were from diverse databases. These studies focused on young females who experienced ovarian torsion and were managed through conservative laparoscopic detorsion. In total, 456 cases were included, including 157 on the right side, 137 on the left side, and 25 bilateral cases. Among these cases, 233 women were postmenarche. The average age of the participants was 12.3 years, with a standard deviation of 3.5. The complete demographics of the study are presented in Table 1.
Figure 1.
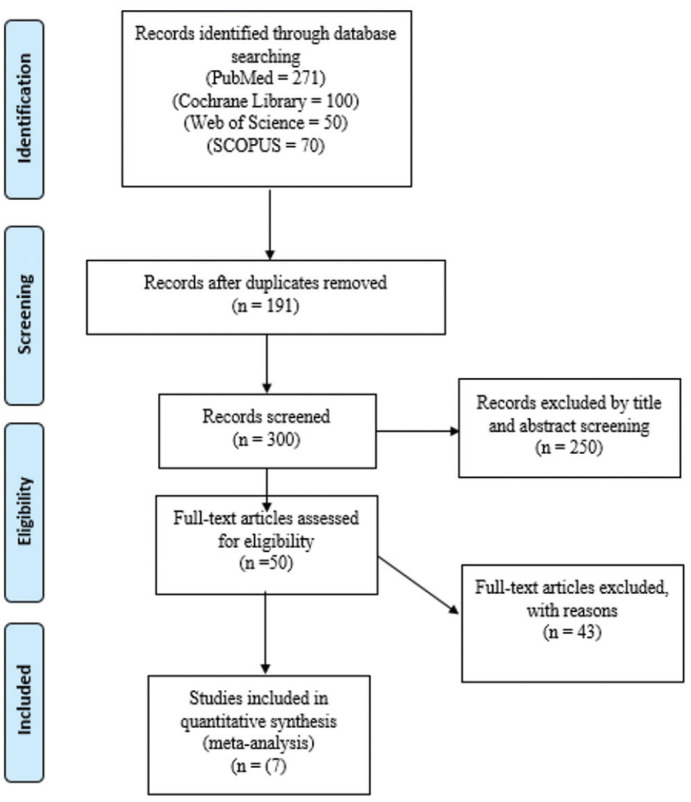
PRISMA flow diagram describing our literature search
Table 1. Demographic and clinical characteristics of the participants.
|
Country |
Study design |
Sample size |
Age > years, (mean, SD/IQR) |
Menarche (%) |
The type of mass causing ovarian torsion |
Side affected |
Follow-up period: 1 month |
||||||
|
Immature teratoma |
Follicular cyst |
Dermoid cyst |
Adenoma |
Adeno-carcinoma |
Right |
Left |
Bilateral |
NR |
|||||
|
India |
Retrospective study |
10 |
11 [6-17] |
5 (50) |
NR |
1 |
NR |
NR |
NR |
7 |
3 |
0 |
8.4 |
|
USA |
Retrospective study |
245 |
12.4 3.29 |
170 (60) |
2 (0.8) |
12 (4.8%) |
35 (14%) |
10 (4) |
1 (0.4) |
134 |
109 |
1 |
8.8 |
|
India |
Retrospective study |
46 |
14.3 [1-18] |
- |
NR |
36 (80) |
7 (15.2) |
NR |
NR |
NR |
NR |
18 |
4-5 years |
|
Australia |
Retrospective study |
54 |
9.80±3.95 |
14 (25.9) |
NR |
12 (21) |
10 (18.51) |
2 (3.70) |
NR |
16 |
21 |
2 |
NR |
|
USA |
Retrospective study |
50 |
13.9±2.6 |
44 (88) |
NR |
16 |
NR |
NR |
NR |
NR |
NR |
NR |
|
|
Canada |
Retrospective review of medical records |
8 |
NR |
NR |
NR |
4 |
1 |
NR |
NR |
NR |
4 |
4 |
32.2 |
|
USA |
Retrospective series |
43 |
8.3 [4.1, 13.6] |
NR |
NR |
10 |
5 |
3 |
NR |
NR |
NR |
NR |
NR |
SD: Standard devation, IQR: Interquartile range
Results of risk of bias assessment
The mean score of the observational studies was 10.7 out of 14. Table 2 provides a detailed illustration of the quality assessment of the observational studies.
Table 2. Quality assessment of the included studies.
|
Study ID |
Sriram et al.(19) |
Adeyemi-Fowode et al.(18) |
Agarwal et al.(17) |
Julania et al. (13) |
Fang et al.(15) |
Pansky et al.(14) |
Walker et al.(16) |
|
1. Was the research question or objective clearly stated in this paper? |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
|
2. Was the study population clearly defined? |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
|
3. Was the participation rate of eligible persons at least 50%? |
1 |
1 |
1 |
1 |
0 |
1 |
1 |
|
4. Were all subjects selected or recruited from the same or similar populations (including the same time period)? Were the inclusion and exclusion criteria prespecified and applied uniformly to all participants? |
0 |
1 |
1 |
1 |
1 |
1 |
1 |
|
5. A sample size justification, power description, or variance and effect estimates |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
6. For the analyses in this paper, were the exposure(s) of interest measured before the outcome(s) was measured? |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
|
7. Was the timeframe sufficient to reasonably expect an association between exposure and outcome if it existed? |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
|
8. For exposures that can vary in amount or level, did the study examine different levels of exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
|
9. Are the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all participants? |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
|
10. Was the exposure(s) assessed more than once? |
0 |
0 |
1 |
0 |
0 |
0 |
0 |
|
11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all participants? |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
|
12. Were the outcome assessors blinded to the exposure status of the participants? |
* |
* |
* |
* |
* |
* |
* |
|
13. Did loss to follow-up after a baseline of 20% or less? |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
|
14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? |
1 |
0 |
1 |
1 |
1 |
1 |
1 |
|
Total score (out of 14) |
10/14 |
10/14 |
12/14 |
11/14 |
10/14 |
11/14 |
11/14 |
Key: 1= Yes, 0= No, *: Not reported, N/A: Not applicable
Outcomes
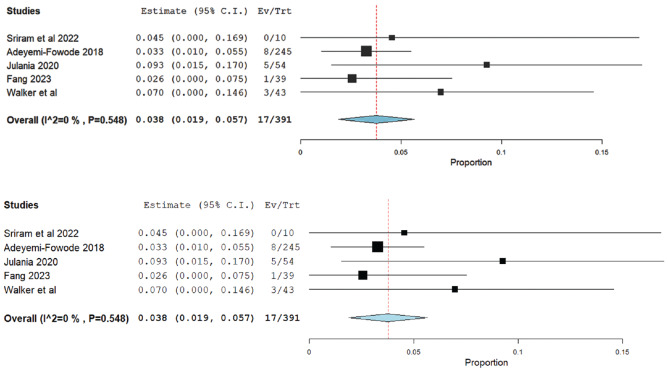
1. Recurrence
Recurrence was difficult to define among the studies, as there was an inconsistent definition regarding whether recurrence referred to the recurrence of acute ovarian torsion, the recurrence of the benign or malignant process that led to the acute torsion, or if both were required to meet the definition. Ultimately, we accepted each included study’s definition of “recurrence” of each included study for data synthesis. Accordingly, the incidence of recurrence was reported in five studies. Seventeen cases experienced recurrence from a total number of 391. The pooled ratio was 0.038 with a [95% CI (0.019, 0.057), p=0.01]. The pooled analysis was homogeneous (I2=0%, p=0.54), as shown in Figure 2.
Figure 2.
Meta-analysis of the incidence of recurrence
CI: Confidence interval
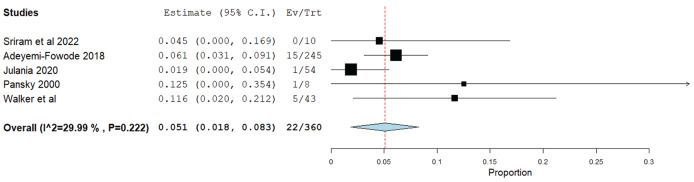
2. Required laparotomy
In five of the studies, we analyzed documented instances where laparoscopic surgery needed to be converted to laparotomy to complete the procedure. Among the 360 cases across these studies, 22 required this conversion. The combined ratio of cases requiring conversion to open surgery was calculated to be 0.051, with a [95% CI (0.018, 0.083), p=0.02]. The p-value associated with this analysis was 0.02. The pooled analysis was homogeneous (I2=29%, p=0.22), as shown in Figure 3.
Figure 3.
Meta-analysis of the incidence of conversion to laparotomy
CI: Confidence interval
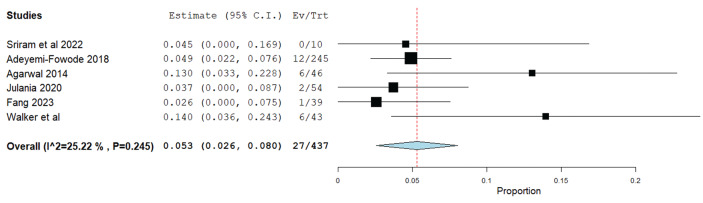
3. Required oophorectomy
The six studies included in our analysis provided data on cases in which conversion to oophorectomy (removal of the ovary) was considered necessary by the attending surgeon. Among the 437 patients who underwent laparoscopic detorsion, 27 required conversion to oophorectomy. The pooled ratio was 0.053 with a [95% CI (0.026, 0.080), p=0.01]. The pooled analysis was homogeneous (I2=25%, p=0.24), as shown in Figure 4.
Figure 4.
Meta-analysis of the incidence of required oophorectomy
CI: Confidence interval
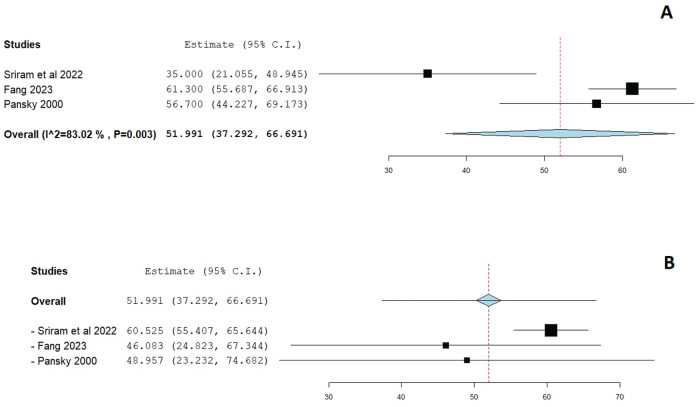
4. Mean time from diagnosis to surgical intervention (in hours)
Three studies reported the time elapsed from the diagnosis of ovarian torsion to surgical intervention. The pooled estimate was 51.9 hours with a [95% CI (37.2, 66.6), p=0.01]. The pooled analysis was heterogeneous (I2=83.017%, p=0.03), as shown in Figure 5A. We performed a leave-one-out meta-analysis to display the effect size after excluding each study. Excluding Sriram et al.(19) seemed to have the largest influence on reducing the heterogeneity, producing an estimate of 60.25 with a [95% CI (55.4, 65.6), p=0.01], as seen in Figure 5B.
Figure 5.
A) Meta-analysis of the mean time from diagnosis to surgical intervention, B) Meta-analysis of the mean time from diagnosis to surgical intervention after excluding Sriram et al.(19) in an attempt to solve heterogeneity
CI: Confidence interval
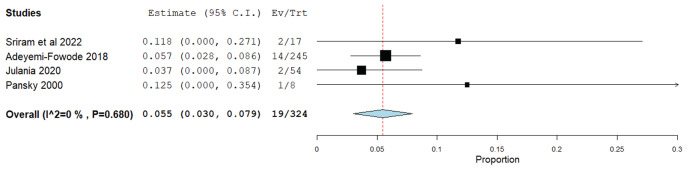
5. Abdominal pain at presentation
Abdominal pain was among the most commonly experienced symptoms at the time of the presentation. A total of 264 out of 324 patients suffered from abdominal pain. The pooled ratio was 0.842 with a [95% CI (0.734, 0.950), p=0.01]. The pooled analysis was heterogeneous (I2=79.4%, p=0.02), as shown in Figure 6.
Figure 6.
Meta-analysis of the presence of abdominal pain on initial presentation
CI: Confidence interval
6. Fever as a symptom at presentation
Fever at presentation was reported in 19 out of 324 patients. The pooled proportion was 0.055, with a [95% CI (0.030, 0.079), p=0.01]. The pooled analysis was homogeneous (I2=0%, p=0.6), as shown in Figure 7.
Figure 7.
Meta-analysis of the presence of fever on initial presentation
CI: Confidence interval
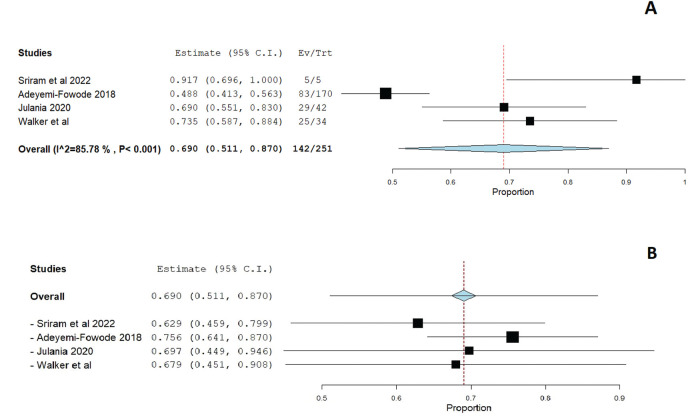
7. Evidence of ovarian function in postoperative US
Almost all studies included assessments of ovarian function in the postoperative period. Studies varied on what was acceptable criteria for evidence of function, and some included the presence of follicles, normal results on Doppler flow studies, or simply a radiologist’s interpretation of a normal appearing ovary for the patient’s age. Studies also varied in the postoperative time frame, but all were within 8 weeks of surgery. The pooled proportion was 0.69 with a [95% CI (0.511, 0.87), p=0.01]. The pooled analysis was heterogeneous (I2=85.7%, p=0.01), as shown in Figure 8.
Figure 8.
Meta-analysis of the presence of evidence of ovarian function on post-operative ultrasound
CI: Confidence interval
Discussion
In our analysis, several key outcomes related to ovarian torsion were evaluated. First, the incidence of recurrence was reported in five studies, where 17 cases experienced recurrence out of 391 cases experienced recurrence. Additionally, instances requiring open surgery were documented in five studies, with 22 out of 360 cases requiring this conversion to open surgery, resulting in a combined ratio of 0.051 [95% CI (0.018, 0.083), p=0.02]. Moreover, six studies provided data on cases requiring oophorectomy, with 27 out of 437 cases requiring this conversion. The mean time from diagnosis to surgery was 51.9 hours. Abdominal pain was very prevalent at presentation, affecting 264 out of 324 patients. Fever was less frequently reported, with only 19 out of 324 cases experiencing it. Finally, most conservative surgeries seemed to be successful, with postoperative evidence of ovarian function showing a pooled proportion of 0.69. These findings shed light on the various aspects of ovarian torsion presentation, management, and associated outcomes, thereby providing a deeper understanding of this condition.
In contrast to ovarian torsion in adults, pediatric cases rarely involve malignant masses, with a prevalence ranging from 0.4% to 1.4%(20). Therefore, a higher rate of ovarian salvage may be possible in this population than in oophorectomy. The majority of ovarian masses in this age group are benign, with only a small percentage being malignant. Studies by Prieto et al.(21) and Ashwal et al.(22) indicated that benign masses or cysts are present in a significant proportion of pediatric ovarian torsion cases and that these were almost universally benign and usually related to hormonal influences. Additionally, ovarian neoplasms >5 cm in diameter are associated with a higher risk of torsion, albeit with lower rates of malignancy in cases involving both mass and torsion. The biggest negative of oophorectomy is the decrease in fertility through its side effects. It simply means that women who have had oophorectomy twice in their lives face difficulties conceiving naturally and also speed up the appearance of menopause. Before puberty, when both ovaries are removed there is abnormal sexual development, primary amenorrhea, and development of infertility(23). Consequently, the interference with fertility should be considered before performing the first oophorectomy and should be avoided as long as it is possible too. Other than that, women with only one ovary also experience different levels of fertility impairment because of diminished ovarian reserve, as shown by the higher basal serum follicle stimulating hormone levels, lower anti-müllerian hormone levels, and poorer response to stimulation. Additionally, they are prone to teenage menopause and a shortened reproductive age span(24). These features led to the variation in conservative care of ovarian twists within different age groups and children who are under 15 years were 40% conservatively treated, compared to women who are under 35 years at 20% and those who are over 50 years at 5%(9).
The growing adoption of conservative management for ovarian torsion is largely attributable to the increasing recognition of its safety and the notably high rates of ovarian viability following detorsion. Numerous studies have explored the outcomes of universally applied conservative treatment, yielding promising findings. For instance, in a medical center where all pediatric cases of ovarian torsion were conservatively managed, 92% of ovaries demonstrated good vascularity and follicular development on follow-up ultrasonography, despite initial presentation with darkened or necrotic appearance(25). Another study by Moiety(26) detailed conservative management in 48 cases of ovarian torsion, all of which resulted in preserved ovarian tissue, as confirmed by various follow-up assessments, including Doppler ultrasonography and laparoscopy. Moreover, analysis of a large database comprising over 150,000 women treated for ovarian torsion, a quarter of whom underwent conservative management, revealed no increased risk of complications such as venous thromboembolism or sepsis(9). These findings collectively suggest that a strategy of universally opting for conservative management of ovarian torsion could lead to high rates of ovarian function preservation with minimal complications. As supported by numerous literature studies, the ovaries that have been salvaged from torsion are reported to show a rate of follicle development that is comparable to normal ovaries. An experiment was conducted that showed within 12 weeks following detorsion of 42 torsed ovaries without follicles all specimens maintained full normal anatomy and the resumption of folliculogenesis. Different research surveyed showed that 74% of pediatric patients had visible follicles 18.7 weeks post detorsion, with a low oophorectomy rate of 2%(16, 27). The other important finding is that the anatomical appearance (sonographic morphology) of the involved ovary does not appear to be altered with or without the cystectomy at the time of detorsion(28).
Rousseau et al.(29) examined 40 cases of ovarian and adnexal torsion in children aged 16 years, excluding neonates, to analyze their clinical and therapeutic characteristics. Abdominal or pelvic pain was the primary symptom, with some children experiencing pain for several months before surgery and most presenting with associated vomiting. US diagnosed various ovarian lesions, including mature teratomas, cystadenoma, functional cysts, and malignant neoplasms. Conservative management was successful in 19 cases, but detorsion with incomplete tumor removal resulted in tumor enlargement and re-torsion in some cases. Bilateral ovarian pathology necessitated unilateral ovariectomy in some cases, whereas others underwent conservative treatment. The findings of the study advocate conservative treatment to preserve ovarian function whenever possible. Oskaylı et al.(30) investigated the diagnosis and treatment of ovarian torsion in children, focusing on conservative approaches and their long-term outcomes. The study involved 41 patients with 42 affected ovaries, most of whom presented with abdominal pain. Conservative detorsion was employed in 62% of the cases. Over time, there has been a shift toward conservative management. Follow-up for conservatively treated patients revealed mostly normal US results although some ovaries were smaller than their counterparts, yet with present ovarian follicles.
Study Limitations
This single-arm meta-analysis of retrospective studies has several limitations that warrant consideration. First, inherent biases are prevalent in retrospective studies due to the reliance on previously collected data, leading to potential selection bias and confounding variables that may not be adequately controlled for. Second, the nature of a single-arm analysis precludes a control or comparison group, which, by its nature, can invite selection bias and limit the interpretation of results. Although single-arm meta-analyses of retrospective studies can provide valuable insights into associations and trends, cautious interpretation is essential because of these inherent limitations. Our study was also limited by heterogeneity among the included studies, which most likely stemmed from the variability in surgical practices across studies. However, in most cases, we were able to solve the heterogeneity problem using accepted techniques. Lastly, we were disappointed that we were unable to find any RCTs on this topic and were forced to utilize only observational studies to complete our analysis. The existence of RCTs on this topic would provide higher quality data and allow more insight into the details of the surgical treatment of ovarian torsion.
Conclusion
We found that recurrence occurred in 17 out of 391, with 22 out of 360 cases requiring conversion to open surgery. Furthermore, oophorectomy was necessary in 27 of 437 patients, and the mean time from symptom onset to surgery was 51.9 h. Abdominal pain was the predominant symptom, affecting 264 out of 324 cases, whereas fever was less prevalent, reported in only 19 cases. Additionally, evidence of retained ovarian function was frequently observed in postmenarche females, with a pooled proportion of 69%. These findings offer valuable insights into the presentation, management, and outcomes of ovarian torsion and contribute significantly to our understanding of this condition.
Acknowledgments
The Marchand Institute for Minimally Invasive Surgery would like to acknowledge the efforts of all the students, researchers, residents, and fellows at the institute who put their time and effort into these projects without compensation, only for the betterment of women’s health. We firmly assure them that the future of medicine belongs to them.
Footnotes
Authorship Contributions
Concept: G.J.M., A.M., M.D., H.U., Design: G.J.M., B.H., H.U., Data Collection or Processing: A.M., A.A., D.H.G., B.H., K.R., M.R., M.D., H.U., Analysis or Interpretation: A.A., K.R., H.U., Literature Search: A.M., A.A., D.H.G., B.H., K.R., M.R., M.D., H.U., Writing: G.J.M., A.M., M.D, H.U.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Guthrie BD, Adler MD, Powell EC. Incidence and trends of pediatric ovarian torsion hospitalizations in the United States, 2000–2006. Pediatrics. 2010;125(3):532–8. doi: 10.1542/peds.2009-1360. [DOI] [PubMed] [Google Scholar]
- 2.Breech LL, Hillard PJ. Adnexal torsion in pediatric and adolescent girls. Curr Opin Obstet Gynecol. 2005;17(5):483–9. doi: 10.1097/01.gco.0000179666.39548.78. [DOI] [PubMed] [Google Scholar]
- 3.Cohen A, Solomon N, Almog B, Cohen Y, Tsafrir Z, Rimon E. Adnexal torsion in postmenopausal women: Clinical presentation and risk of ovarian malignancy. J Minim Invasive Gynecol. 2017;24(1):94–7. doi: 10.1016/j.jmig.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell RE, Koyfman A, Long B. High-risk and low-prevalence diseases: Ovarian torsion. Am J Emerg Med. 2022;56:145–50. doi: 10.1016/j.ajem.2022.03.046. [DOI] [PubMed] [Google Scholar]
- 5.Varras M, Tsikini A, Polyzos D, Samara Ch, Hadjopoulos G, Akrivis Ch. Uterine adnexal torsion: pathological and gray-scale ultrasonographic findings. Exp Obstet Gynecol. 2004;31(1):34–8. [PubMed] [Google Scholar]
- 6.Mashiach R, Melamed N, Gilad N, Ben-Shitrit G, Meizner I. Sonographic diagnosis of ovarian torsion. J Ultrasound Med. 2011;30(9):1205–10. doi: 10.7863/jum.2011.30.9.1205. [DOI] [PubMed] [Google Scholar]
- 7.Singh T, Prabhakar N, Singla V, Bagga R, Khandelwal N. Magnetic resonance imaging findings in ovarian torsion. Polish J Radiol. 2018;83:564–75. doi: 10.5114/pjr.2018.81157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scheier E. Diagnosis and management of pediatric ovarian torsion in emergency departments: Current insights. Open Access Emerg Med. 2022;283-91. doi: 10.2147/OAEM.S342725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mandelbaum R, Smith M, Violette C, Matsuzaki S, Matsushima K, Klar M. Conservative surgery for ovarian torsion in young women: perioperative complications and national trends. BJOG An Int J Obstet Gynaecol. 2020;127(8):957–65. doi: 10.1111/1471-0528.16179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6. [PMC free article] [PubMed] [Google Scholar]
- 11.Robbins IM, Moore TM, Blaisdell CJ, Abman SH. National heart, lung, and blood institute workshop. Circulation. 2012;125(17):2165–70. doi: 10.1161/CIRCULATIONAHA.112.092924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end users: R as a computational back-end. J Stat Softw. 2012;49. [Google Scholar]
- 13.Julania S, Chown I, Gera S, Hunter T. Management of adnexal torsion in the pediatric and adolescent population of Western Australia’s single tertiary children’s hospital over the last 10 years: Retrospective study. J Minim Invasive Gynecol. 2021;28(6):1183–9. doi: 10.1016/j.jmig.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Pansky M, Abargil A, Dreazen E, Golan A, Bukovsky I, Herman A. Conservative management of adnexal torsion in premenarchal girls. J Am Assoc Gynecol Laparosc. 2000;7(1):121–4. doi: 10.1016/s1074-3804(00)80021-3. [DOI] [PubMed] [Google Scholar]
- 15.Fang ME, Crain C, Baquet E, Dietrich JE. Laparoscopic salvage procedures for adnexal torsion in pediatric and adolescent patients during the COVID-19 pandemic: a retrospective cohort study. Patient Saf Surg. 2023;17(1):1–7. doi: 10.1186/s13037-023-00376-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walker SK, Lal DR, Boyd KP, Sato TT. Pediatric ovarian torsion: evidence of follicular development after ovarian preservation. Surg (United States) 2018;163:547–52. doi: 10.1016/j.surg.2017.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Agarwal P, Agarwal P, Bagdi R, Balagopal S, Ramasundaram M, Paramaswamy B. Ovarian preservation for adnexal pathology in children, current trends in laparoscopic management and our experience. J Indian Assoc Pediatr Surg. 2014;19:65–9. doi: 10.4103/0971-9261.129594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adeyemi-Fowode O, Lin EG, Syed F, Sangi-Haghpeykar H, Zhu H, Dietrich JE. Adnexal torsion in children and adolescents: A retrospective review of 245 cases at a single institution. J Pediatr Adolesc Gynecol. 2019;32:64–9. doi: 10.1016/j.jpag.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 19.Sriram R, Zameer MM, Vinay C, Giridhar BS. Black Ovary: Experience with oophoropexy in pediatric ovarian torsion cases and review of relevant literature. J Indian Assoc Pediatr Surg. 2020;27:558. doi: 10.4103/jiaps.jiaps_207_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oltmann SC, Fischer A, Barber R, Huang R, Hicks B, Garcia N. Cannot exclude torsion—a 15-year review. J Pediatr Surg. 2009;44(6):1212–7. doi: 10.1016/j.jpedsurg.2009.02.028. [DOI] [PubMed] [Google Scholar]
- 21.Prieto JM, Kling KM, Ignacio RC, Bickler SW, Fairbanks TJ, Saenz NC. Premenarchal patients present differently: A twist in a typical patient presenting with ovarian torsion. J Pediatr Surg. 2019;54:2614–6. doi: 10.1016/j.jpedsurg.2019.08.020. [DOI] [PubMed] [Google Scholar]
- 22.Ashwal E, Hiersch L, Krissi H, Eitan R, Less S, Wiznitzer A. Characteristics and management of ovarian torsion in premenarchal compared With postmenarchal patients. Obstet Gynecol. 2015;126:514–20. doi: 10.1097/AOG.0000000000000995. [DOI] [PubMed] [Google Scholar]
- 23.Gold MA, Schmidt RR, Parks N, Traum RE. Bilateral ovaries and distal fallopian tubes. A case report. J Reprod Med. 1997;42(6):375–7. [PubMed] [Google Scholar]
- 24.Lass A. Fertility potential of women with a single ovary. Hum Reprod Update. 1999;5(5):546–50. doi: 10.1093/humupd/5.5.546. [DOI] [PubMed] [Google Scholar]
- 25.Parelkar SV, Mundada D, Sanghvi BV, Joshi PB, Oak SN, Kapadnis SP, al Should the ovary be preserved during torsion? A tertiary care institute experience. J Pediatr Surg. 2014;49:465–8. doi: 10.1016/j.jpedsurg.2013.11.055. [DOI] [PubMed] [Google Scholar]
- 26.Moiety FMS. Adnexal torsion: Management controversy: A case series. Middle East Fertil Soc J. 2017;22(2):156–9. doi: 10.1016/j.mefs.2017.01.006. [DOI] [Google Scholar]
- 27.Geimanaite L, Trainavicius K. Pediatric ovarian torsion: Follow-up after preservation of ovarian tissue. J Pediatr Surg. 2019;54:1453–6. doi: 10.1016/j.jpedsurg.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 28.Murphy NC, Elborno D, Kives S, Allen LM. Postoperative ovarian morphology on ultrasound after ovarian torsion—effect of immediate surgery: A retrospective cohort study. J Pediatr Adolesc Gynecol. 2022;35(3):353–8. doi: 10.1016/j.jpag.2021.10.013. [DOI] [PubMed] [Google Scholar]
- 29.Rousseau V, Massicot R, Darwish AA, Sauvat F, Emond S, Thibaud E. Emergency management and conservative surgery for ovarian torsion in children: A report of 40 cases. J Pediatr Adolesc Gynecol. 2008;21:201–6. doi: 10.1016/j.jpag.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 30.Oskaylı MÇ, Durakbaşa ÇU, Maşrabacı K, Mutuş HM, Zemheri IE, Okur H. Surgical approach to ovarian torsion in children. J Pediatr Adolesc Gynecol. 2015;28:343–7. doi: 10.1016/j.jpag.2014.10.001. [DOI] [PubMed] [Google Scholar]