Abstract
Healthcare systems and providers have increasingly acknowledged the role and impact of social determinants in overall health. However, gender-diverse individuals face persistent health disparities due to their identities. There is limited research on the impact of clinical and sociodemographic characteristics on mood and quality of life (QoL) for transgender (TG) individuals. Our study aims to understand and better elucidate social and clinical characteristics of transmasculine (TM) and transfeminine (TF) individuals and their impact on quality of life and depressive symptoms. In this cross-sectional study, 298 TF and TM individuals on gender-affirming hormone therapy (GAHT) were surveyed about their demographic characteristics (age, gender identity, body mass index (BMI), and education), social needs, mood, and quality of life. Multivariable regression modelling was performed to assess the effect of each variable listed above on three domains of QoL (psychological, environmental, and physical) as well as depressive symptoms. We find that QoL scores are similar between TM and TF individuals, with scores in the psychological domain particularly low in both cohorts. TM individuals report higher rates of stress and restroom avoidance than TF individuals. In particular, psychological well-being (measured by the psychological domain of QoL and depressive symptoms) is significantly associated with increased BMI, financial instability, and stress in TM individuals while for TF individuals, psychological well-being is associated with stress and social integration. These data suggest that social circumstances are key drivers of QoL and psychological well-being among gender-diverse individuals receiving GAHT with specific differences between TF and TM individuals. This information may be utilized by healthcare providers and policymakers to address and improve clinical care and social policies to improve health equity for gender-diverse individuals.
Keywords: Transgender medicine, Social determinants of health, Quality of life, Gender-affirming hormone therapy
1. Introduction
Individuals who are transgender (TG) typically have an incongruence between their biologic sex assigned at birth and their gender identity. Gender identities include male and female, as well as other expansive categories including gender-fluid, gender-queer, and non-binary. Some TG individuals may elect medical interventions such as hormone therapy, surgeries, and/or other modifications that align their outward physical appearance to match their gender identity. However, not all TG individuals choose to undergo medical interventions (Cicero et al., 2019).
TG individuals face a number of disparities and disadvantages including higher rates of homelessness, sexual and physical assaults and trauma, unemployment, discrimination, and increased morbidity and mortality (Cicero et al., 2019; Fredriksen Goldsen et al., 2022; Grant et al., 2010). Prior work has reported that only 30–40 percent of TG individuals utilize the healthcare system regularly (Feldman et al., 2021; Grant et al., 2010). Of these individuals, at least one-quarter report suboptimal care due to unsafe public and healthcare spaces, lack of knowledgeable clinicians (Grant et al., 2010), decreased trust in the healthcare system (Baguso et al., 2022), and restricted health insurance benefits that limit access to gender affirming health care services (Andermann, 2018; Hobster and McLuskey, 2020; Safer et al., 2016). Additionally, there is also concern that sexual orientation and gender identity information (SOGI) is not adequately collected from providers or documented in the electronic health record despite recent recommendations from the National Academy of Medicine and the Joint Commission to better document SOGI information (Deutsch et al., 2013; Deutsch and Buchholz, 2015; The Health of Lesbian, Gay, Bisexual, and Transgender People, 2011). As a result, LGBTQ + individuals may not be getting identified and their specific health needs may not be getting appropriately addressed (Cahill and Makadon, 2014; Wolfe et al., 2021).
Although there has been an increased awareness in healthcare of the impact of social needs on overall health status and outcomes, unmet social needs remain a persistent barrier in providing high-quality, evidence-based clinical care (O’Gurek and Henke, 2018). Additionally, mounting evidence across a spectrum of health issues has demonstrated that low income, lower educational attainment, and decreased social status/support are associated with worse health outcomes, notably increased morbidity and premature mortality (Andermann, 2018; Gama e Colombo, 2010).
While screening for social determinants of health in a clinical setting in the general population has been increasing, there is limited research utilizing these screening tools in TG patients. A cross-sectional study assessing food and housing insecurity in TG and cisgender adults in the United States, using the Behavioral Risk Factor Surveillance System Survey (BRFSS), found that TG individuals have higher odds of experiencing food-related stress and underemployment (Henderson et al., 2019). In terms of QoL, a systematic review and meta-analysis suggested that TG individuals have lower QoL than the general population (Nobili et al., 2018), with some evidence supporting that QoL improves within 6–12 months of commencing gender-affirming hormone therapy (GAHT) (Foster Skewis et al., 2021; Manieri et al., 2014).
There are a small number of studies using the World Health Organization Quality of Life Survey (WHO-QoL) in TG individuals. A study used and validated the brief version of this instrument (WHOQOL-BREF) in a cohort of TF individuals (Thompson et al., 2015). Two other cross-sectional studies utilized this survey in TM and TF individuals undergoing GAHT or surgical therapy and concluded that physical characteristics (such as body hair and breast size), family support, and employment are associated with higher QoL scores (Gómez-Gil et al., 2014; Silva et al., 2021).
Our work builds upon the Minority Stress Model which was developed to better understand how diverse minority groups experience stress and its effect on mental and physical health (Meyer, 2003). Specifically, the Transgender Resilience Intervention Model focuses on developing resilience-based interventions that can buffer some of this stress in TG individuals to improve psychological well-being (Matsuno and Israel, 2018). Knowing that these resilience factors mitigate excess stressors creates more of an impetus to focus work on further identifying and measuring these stressors and their impact on QoL and health.
Our study uses a comprehensive survey of TF and TM individuals to evaluate multiple social needs including restroom access, financial stability, social interactions, stress, and transportation availability. The goal of this research is to understand the influence of social needs on multiple QoL domains and symptoms of depression in TM and TF persons receiving GAHT.
2. Materials and methods
2.1. Participants and recruitment
The participants in this study were recruited as part of a broad project known as “sex Hormones and Lower Urinary Tract Symptoms” (H-LUTS). In the H-LUTS project we are studying a comprehensive set of biologic, behavioral, psychological and socioeconomic variables in cohorts of TM and TF subjects receiving GAHT therapy for at least 12 months. One of the aims of the study is understanding the interplay of these variables with lower urinary tract symptoms (LUTS). Following approval by the MetroHealth System Institutional Review Board (IRB), initial survey participant screening and identification was conducted using the EPIC electronic health record (EHR). Study data were collected and managed using REDCap electronic data capture tools hosted at Case Western Reserve University. All eligible survey participants received care at the MetroHealth System, in Northeast Ohio, and were identified with permission of their respective treating health care provider. Inclusion criteria included the following: at least 18 years old, able to read English, able to complete a survey, individuals assigned male sex at birth or female sex at birth who had been receiving exogenous estrogens or testosterone, respectively, for gender dysphoria for at least 12 months. Individuals with a documented history of chronic kidney disease (CKD) stage 5, congenital urinary tract malformations, and pregnancy at time of survey were excluded from the study, due to the potential role of these conditions on LUTS. Eligible individuals were invited to complete the study survey either on paper, online via REDCap, or via a telephone interview. A total of 310 individuals consented to participate, of whom 298 completed all questionnaires and are included in the analysis.
2.2. Survey instrument
We administered a comprehensive survey that included the following: whether participants considered themselves to be TG/gender nonconforming, sex assigned at birth, gender identity (male, female, other including non-binary or gender-diverse), sex hormone therapy and duration, history of genital surgery (bottom surgery) for gender-affirming care (i.e. surgery on penis/testicle vs. surgery on vagina/uterus/ovaries), QoL, depression, lower urinary tract symptoms (LUTS), race/ethnicity, height, weight, social needs, smoking status, alcohol intake, and substance use. We also included a novel question on whether bathroom facilities were avoided due to safety concerns: ‘Over the last month or so, did you have to hold your urine, and avoid going to the bathroom, because you felt that the bathroom facilities were not adequate, friendly, or safe for transgender persons?. A complete version of survey items is included (Supplemental Materials; Fig. S1). This survey was administered between July 5, 2019, and March 9, 2020.
Study participants were asked their current gender identity and were given three options: ‘male’, ‘female’, and ‘other’, which is referring to individuals who identify as non-binary or gender-diverse. The ‘other’ group only contained twenty participants, thus was not large enough to perform comparable statistical analyses. As a result, we operationally categorized the study sample into individuals using feminizing hormone therapy as TF and masculinizing hormone therapy as TM. For all analyses, we refer to our populations as TM and TF.
The WHO QoL-BREF instrument consists of 26 items: two global items and 24 additional items assessing four domains: psychological, environmental, social, and physical. Domain scores were transformed and scaled from zero to 100 according to instrument guidelines to allow for comparisons between domains (The WHOQOL Group, 1998). Cronbach’s alpha was used to analyze internal consistency of the domains. Values close to and greater than 0.70 indicated acceptable internal consistency (Supplemental Data; Table S1). The social domain of the WHO QoL-BREF was omitted from our analysis of outcomes; after review of the individual items, we found considerable overlap between the wording of the QoL measure and the social integration social determinants of health indicators.
The Alcohol Use Disorders Identification Test (AUDIT-C) instrument consists of three items evaluating the frequency of drinking, the amount of alcohol consumed, and the number of binging events. Each question is scored from zero to four and summed for a possible score of zero to 12 (Bush et al., 1998). AUDIT scores greater than eight were re-coded to eight since few participants scored higher than eight.
The Center of Epidemiological Studies Depression Scale-8 (CESD-8) is an instrument for the screening of depression. The CESD-8 consists of eight questions to measure the presence of symptoms such as depressed mood, feelings of guilt and worthlessness, loss of appetite, and sleep disturbance. Responses were summed for a possible score of zero to eight (Van de Velde et al., 2009).
Additional social determinants of health questions were included in this survey to evaluate financial strain (Kahn and Pearlin, 2006; Puterman et al., 2012), stress (Elo et al., 2003), social isolation (Berkman and Syme, 1979; Ford et al., 2006; Pantell et al., 2013), and transportation accessibility (De Marchis et al., 2020). These questions have been utilized, scored, and validated in prior studies in the general population (Chagin et al., 2021).
Individual social isolation questions are demonstrated in the univariable analysis. However, for use in the bivariable and multivariable analyses, they were summed and used as a continuous variable. The scoring for these questions has been described elsewhere (Pantell et al., 2013).
Survey participants were asked whether they had been on GAHT for at least 12 months and their hormone therapy start date. The difference between self-reported hormonal therapy start date and survey completion date was calculated, with the assumption that therapy had been continuous throughout this period.
2.3. Statistical analysis
Patient characteristics were described using median with interquartile range (IQR) for continuous variables, and percentages for categorical data. Wilcoxon rank sum, chi-squared, and ANOVA tests were used where appropriate. Four models were created to understand the effect of multiple predictors on overall well-being (measured by three QoL domains: physical, environmental, and psychological, and CESD-8 scores).
While we presented each Likert scaled variable as categorical variables in the univariable analysis, due to their relatively normal distribution and large sample size, we treated these variables as continuous in the bivariable and multivariable analyses. Spearman ranked correlation coefficients were further used for bivariable analyses to account for interval responses of the Likert variables.
To assess the importance of social and clinical demographic information on the different domains of QoL and depressive symptoms, multiple linear regression models were created for TM and TF groups. Other covariates in the models included BMI, education attainment level, whether bathroom facilities were avoided due to safety or other concerns, financial insecurity, stress levels, social integration, transportation accessibility, exercise frequency, current/past smoking status, AUDIT score, time on hormone therapy, and age.
To estimate the variability of each coefficient, a bootstrapping procedure was employed. Ten thousand resamples were generated from the original sample population, and each model was run through the resampled populations to create a mean of the standardized regression coefficients. The distribution of these bootstrapped means was used to construct a 95% confidence interval. The sample standardized regression coefficients, the bootstrapped 95% confidence intervals, and the bootstrapped coefficient of determination are reported to determine model fit.
This study was approved by the MetroHealth Institutional Review Board (IRB). All analyses were conducted using R version 4.2.1, Vienna, Austria.
3. Results
3.1. Demographics and descriptive characteristics
The demographic characteristics of our study sample are displayed in Table 1. A total of 298 participants completed the survey. Screened participants had a median age of 28 years. The majority of participants were white (78%), unmarried (54%), 36% attended some college, and 42% reported some degree of higher education (i.e. Associate’s, Bachelor’s, graduate degree). Our study sample was almost equally distributed between TM (51%) and TF (49%) individuals. The TM group was younger (median, IQR; 26 years; (20–31)) than the TF cohort (31 years (25–44), p < 0.001; Table 1A). A minimal percentage of our sample population had a BMI <18.5 (1.7%). The rest of the population distributed approximately evenly between a BMI of 18.5–24.9 (33%), 25–29.9 (30%), and >30 (34.7%).
Table 1.
A Subject characteristics and demographics.
| Characteristic | Overall, N = 2981 | Transmasculine, N = 1521 | Transfeminine, N = 1461 |
|---|---|---|---|
| Race/Ethnicity | |||
| White | 231 (78%) | 116 (76%) | 115 (79%) |
| Black | 33 (11%) | 17 (11%) | 16 (11%) |
| Other/Mixed | 23 (7.7%) | 13 (8.6%) | 10 (6.8%) |
| Unknown | 11 (3.7%) | 6 (3.9%) | 5 (3.4%) |
| Highest Level of Education | |||
| Some Grade School | 20 (6.7%) | 12 (7.9%) | 8 (5.5%) |
| High School Graduate/GED | 46 (15%) | 18 (12%) | 28 (19%) |
| Some College, No Degree | 107 (36%) | 56 (37%) | 51 (35%) |
| Associate’s/Bachelor’s | 95 (32%) | 50 (33%) | 45 (31%) |
| Graduate Degree (i.e. MA, MD, PhD) | 30 (10%) | 16 (11%) | 14 (9.6%) |
| Marital Status | |||
| Never Married | 161 (54%) | 87 (57%) | 74 (51%) |
| Married | 39 (13%) | 20 (13%) | 19 (13%) |
| Living with a partner | 71 (24%) | 35 (23%) | 36 (25%) |
| Widowed | 2 (0.7%) | 1 (0.7%) | 1 (0.7%) |
| Separated | 25 (8.4%) | 9 (5.9%) | 16 (11%) |
| BMI (kg/m 2 ) | |||
| < 18.5 | 5 (1.7%) | 1 (0.7%) | 4 (2.7%) |
| 18.5–24.9 | 98 (33%) | 51 (34%) | 47 (32%) |
| 25–29.9 | 90 (30%) | 40 (26%) | 50 (34%) |
| > 30 | 105 (35%) | 60 (39%) | 45 (31%) |
| Age (Years) 2 | 28 (22, 36) | 26 (20, 31) | 31 (25, 44) |
n (%); Median (IQR).
p < 0.001 by t-test.
Median time on hormone therapy was 2.9 years (IQR 1.7–5.1), and 16.1% of participants reported having undergone gender-affirming genital surgeries, with no significant differences between TF and TM individuals (Table 1B).
Table 1B.
Gender-affirming therapy characteristics.
| Characteristic | Overall, N = 2981 | Transmasculine, N = 1521 | Transfeminine, N = 1461 |
|---|---|---|---|
| Gender-Affirming Genital Surgery | |||
| Feminizing Surgery | 26 (8.7%) | 0 (0%) | 26 (18%) |
| Masculinizing Surgery | 22 (7.4%) | 22 (14%) | 0 (0%) |
| None | 250 (84%) | 130 (86%) | 120 (82%) |
| Time on Gender-Affirming Hormone Therapy (Years) | 2.9 (1.7, 5.1) | 2.9 (1.8, 4.9) | 3.1 (1.7, 5.7) |
n (%); Median (IQR).
A large percentage (61%) of surveyed participants reported having three or more depressive symptoms, as measured by the CESD-8. 35% of participants reported previously smoking cigarettes, while 13% of individuals reported currently smoking. Most of our sample population reported never having used recreational drugs (64%) or misused prescription drugs (90%). These numbers were similar between TM and TF groups.
The Center for Disease Control (CDC) recommendations for physical activity include a mix of moderate and high intensity aerobic activity on two or more days a week. 73% of the TM and 64% of the TF individuals reportedly met these recommendations (Table 1C).
Table 1C.
Clinical characteristics and health behaviors.
| Characteristic | Overall, N = 2981 | Transmasculine, N = 1521 | Transfeminine, N = 1461 |
|---|---|---|---|
| AUDIT-C | |||
| Scored 0–2 | 193 (65%) | 95 (62%) | 98 (67%) |
| Scored 3 | 33 (11%) | 16 (11%) | 17 (12%) |
| Scored 4 or more | 72 (24%) | 41 (27%) | 31 (21%) |
| Screening AUDIT | |||
| Positive | 105 (35%) | 57 (38%) | 48 (33%) |
| Negative | 193 (65%) | 95 (62%) | 98 (67%) |
| Moderate to Strenuous Exercise (Days per week) | |||
| 0–1 day(s) per week | 94 (32%) | 41 (27%) | 53 (36%) |
| 2–4 days per week | 133 (45%) | 72 (47%) | 61 (42%) |
| 5 or more days per week | 71 (24%) | 39 (26%) | 32 (22%) |
| Social Isolation | |||
| Most socially isolated (Scored 0–1) | 194 (65%) | 99 (65%) | 95 (65%) |
| Less socially isolated (Scored 2–3) | 102 (34%) | 53 (35%) | 49 (34%) |
| Least socially isolated (Scored 4) | 2 (0.7%) | 0 (0%) | 2 (1.4%) |
| CESD-8 Score | |||
| 0–2 depressive symptoms | 115 (39%) | 52 (34%) | 63 (43%) |
| 3–5 depressive symptoms | 84 (28%) | 41 (27%) | 43 (29%) |
| 6–8 depressive symptoms | 99 (33%) | 59 (39%) | 40 (27%) |
| Has Smoked at least 100 Cigarettes within Lifetime | 105 (35%) | 53 (35%) | 52 (36%) |
| Currently Smokes | 38 (13%) | 22 (14%) | 16 (11%) |
| Recreational Drugs | |||
| Never | 190 (64%) | 91 (60%) | 99 (68%) |
| Less than monthly | 37 (12%) | 15 (9.9%) | 22 (15%) |
| Monthly | 24 (8.1%) | 13 (8.6%) | 11 (7.5%) |
| Weekly | 18 (6.0%) | 13 (8.6%) | 5 (3.4%) |
| Daily or almost daily | 29 (9.7%) | 20 (13%) | 9 (6.2%) |
| MisusedPrescription Drugs | |||
| Never | 268 (90%) | 135 (89%) | 133 (91%) |
| Less than monthly | 16 (5.4%) | 12 (7.9%) | 4 (2.7%) |
| Monthly | 4 (1.3%) | 2 (1.3%) | 2 (1.4%) |
| Weekly | 5 (1.7%) | 3 (2.0%) | 2 (1.4%) |
| Daily or almost daily | 5 (1.7%) | 0 (0%) | 5 (3.4%) |
n (%).
3.2. Transmasculine individuals delay urination at higher rates due to decreased availability of adequate facilities and report higher levels of stress
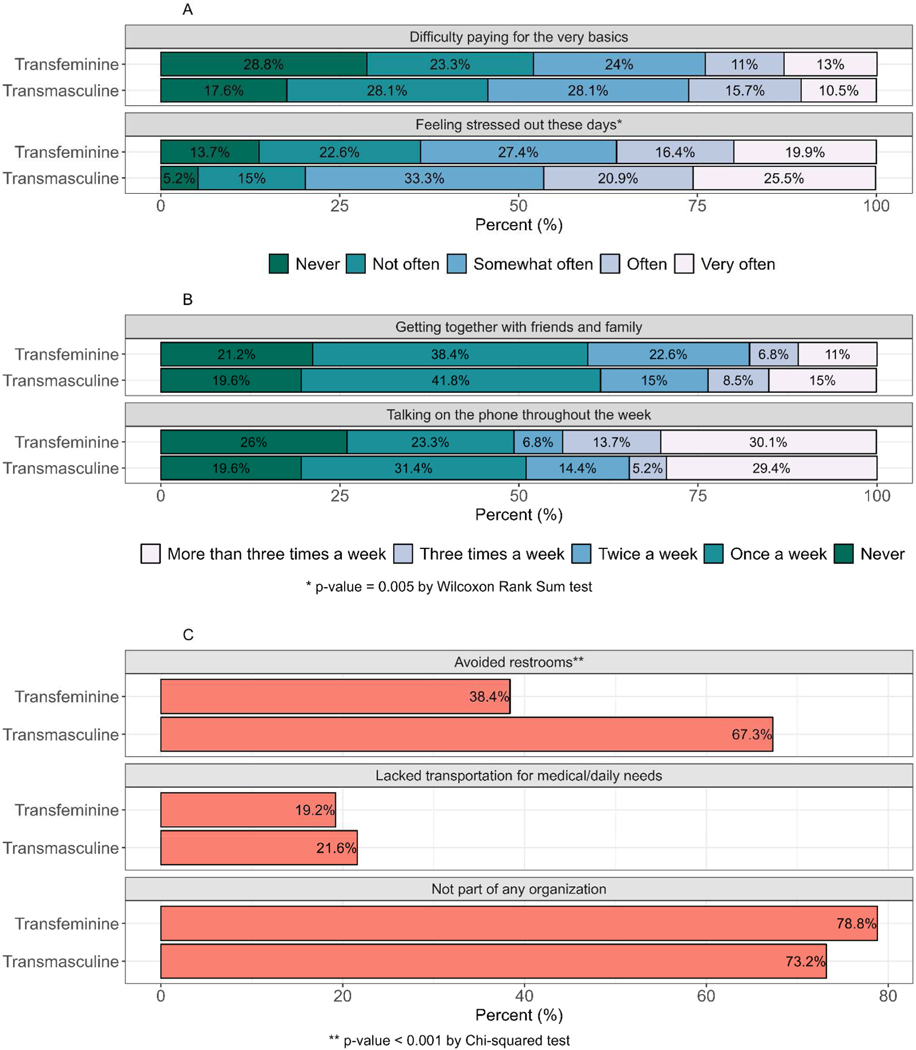
When asked about stress levels, 46.8% of TM individuals reported high levels of stress (often or very often) compared to 36.3% of our TF individuals (Fig. 1A, p = 0.005). A minority of our cohort reported getting together with friends and family often or very often (20.8%) and talking on the phone throughout the week often or very often (39%; Fig. 1B). A striking and significantly higher percentage of the TM individuals (67.8%) reported avoiding restroom facilities, as compared to TF individuals (38.4%; Fig. 1C; p < 0.001). TM and TF cohorts had similar percentages for all other social needs.
Fig. 1. Social needs in transmasculine and transfeminine individuals.
Stacked bar graphs demonstrating social needs assessed on a five-point scale. From top to bottom the following were assessed: A) difficulty affording the basics, stress levels; B) getting together with friends and family, talking on the phone throughout the week; C) avoidance of restroom facilities, transportation inaccessibility, and not part of any organization. Lowest values were shown on the left and highest values were shown on the right.
3.3. Psychological domain QoL scores were lower compared to other domains in both transmasculine and transfeminine cohorts
QoL scores were broken into four main domains: physical, psychological, social, and environmental (Table 2). Overall, psychological satisfaction scores (median, IQR; 54.2, 37.5–66.7) were lower than that of physical (median, IQR; 67.9, 53.6–78.6), social (median, IQR; 66.7, 50.0–75.0), and environmental (median, IQR; 65.6, 53.1–78.1) in both TM and TF cohorts.
Table 2.
Quality of life domain scores by gender.
| Characteristic | Overall, N = 298a | Transmasculine, N = 152a | Transfeminine, N = 146a |
|---|---|---|---|
| Physical Satisfaction | 67.9 (53.6, 78.6) | 67.9 (53.6, 78.6) | 67.9 (50.0, 82.1) |
| Psychological Satisfaction b | 54.2 (37.5, 66.7) | 50.0 (37.5, 63.5) | 54.2 (41.7, 70.8) |
| Social Satisfaction | 66.7 (50.0, 75.0) | 66.7 (50.0, 75.0) | 66.7 (41.7, 75.0) |
| Environmental Satisfaction | 65.6 (53.1, 78.1) | 67.2 (53.1, 78.1) | 65.6 (53.9, 78.1) |
Median (IQR).
p < 0.001 by ANOVA for all groups.
Variables that showed an association with other independent variables in the bivariate analyses are presented in Supplemental Materials (Fig. S2). Of note, there appears to be a positive correlation between an inability to afford the basics with stress and depressive symptoms. Other social needs correlate with different QoL domains and were included in the multivariable models.
In order to assess the effects of multiple factors such as demographic data, GAHT data, health behaviors, and social needs on QoL and depressive symptoms, multiple linear regressions were performed (Table 3). A separate multivariable model was created with each of the following as a separate outcome measure: psychological domain, physical domain, environmental domain, and CESD-8 scores for the TM (Table 3A) and TF (Table 3B) cohorts.
Table 3A.
Clinical and sociodemographic predictors in transmasculine individuals.
| Characteristic | Psychological |
Physical |
Environmental |
CESD-8 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta | 95% CI1 | p-value | Beta | 95% CI1 | p-value | Beta | 95% CI1 | p-value | Beta | 95% CI1 | p-value | |
| Intercept | 0.12 | −0.12, 0.36 | <0.001 | 0.03 | −0.19, 0.24 | <0.001 | 0.33 | 0.10, 0.56 | <0.001 | 0.02 | −0.25, 0.30 | 0.2 |
| BMI | −0.16 | −0.29, −0.03 | 0.013 | −0.13 | −0.25, −0.02 | 0.024 | −0.08 | −0.21, 0.04 | 0.2 | 0.14 | −0.01, 0.28 | 0.063 |
| Education | 0.10 | −0.04, 0.23 | 0.2 | 0.13 | 0.01, 0.26 | 0.040 | −0.07 | −0.20, 0.06 | 0.3 | −0.03 | −0.19, 0.12 | 0.7 |
| Avoided Bathroom Facilities | 0.2 | >0.9 | 0.052 | 0.8 | ||||||||
| No | – | – | – | – | – | – | – | – | ||||
| Yes | −0.16 | −0.43, 0.11 | 0.00 | −0.24, 0.25 | −0.25 | −0.50, 0.00 | −0.03 | −0.33, 0.27 | ||||
| Difficulty Affording the Basics | −0.21 | −0.34, −0.08 | 0.002 | −0.40 | −0.52, −0.28 | <0.001 | −0.52 | −0.64, −0.39 | <0.001 | 0.27 | 0.12, 0.43 | <0.001 |
| Stress | −0.44 | −0.58, −0.30 | <0.001 | −0.31 | −0.44, −0.19 | <0.001 | −0.13 | −0.27, 0.00 | 0.047 | 0.33 | 0.17, 0.49 | <0.001 |
| Social Integration | 0.15 | 0.02, 0.27 | 0.022 | −0.02 | −0.13, 0.10 | 0.8 | 0.07 | −0.05, 0.19 | 0.2 | −0.01 | −0.15, 0.13 | 0.9 |
| Lack of Transportation | >0.9 | 0.011 | <0.001 | >0.9 | ||||||||
| No | – | – | – | – | – | – | – | – | ||||
| Yes | 0.01 | −0.30, 0.32 | −0.37 | −0.65, −0.09 | −0.59 | −0.89, −0.29 | 0.02 | −0.34, 0.37 | ||||
| Exercise | 0.16 | 0.04, 0.28 | 0.011 | 0.21 | 0.09, 0.32 | <0.001 | −0.01 | −0.13, 0.10 | 0.8 | −0.14 | −0.28, 0.00 | 0.051 |
| Current Smoker | 0.043 | 0.015 | 0.053 | 0.8 | ||||||||
| No | – | – | – | – | – | – | – | – | ||||
| Yes | −0.44 | −0.87, −0.02 | −0.49 | −0.88, −0.09 | −0.40 | −0.81, 0.00 | 0.06 | −0.43, 0.55 | ||||
| Past Smoker | 0.4 | 0.019 | 0.6 | 0.8 | ||||||||
| No | – | – | – | – | – | – | – | – | ||||
| Yes | 0.14 | −0.17, 0.46 | 0.35 | 0.06, 0.64 | 0.07 | −0.23, 0.38 | −0.05 | −0.41, 0.31 | ||||
| Alcohol Screening Score | 0.02 | −0.12, 0.15 | 0.8 | 0.08 | −0.04, 0.20 | 0.2 | 0.11 | −0.02, 0.24 | 0.083 | 0.13 | −0.03, 0.28 | 0.11 |
| Time on Hormone Therapy | −0.01 | −0.19, 0.17 | >0.9 | 0.08 | −0.09, −0.24 | 0.4 | 0.07 | −0.10, 0.25 | 0.4 | −0.08 | −0.29, 0.12 | 0.4 |
| Age | 0.07 | −0.12, 0.27 | 0.5 | −0.37 | −0.54, −0.19 | <0.001 | −0.08 0.625 | −0.26, 0.11 | 0.4 | 0.09 | −0.13, 0.31 | 0.4 |
| R2 | 0.545 | 0.625 | 0.625 | |||||||||
CI = Confidence Interval (Bootstrapped).
Table 3B.
Clinical and sociodemographic predictors in transfeminine individuals.
| Characteristic | Psychological |
Physical |
Environmental |
CESD-8 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta | 95% CI1 | p-value | Beta | 95% CI1 | p-value | Beta | 95% CI1 | p-value | Beta | 95% CI1 | p-value | |
| Intercept | −0.02 | −0.22, 0.17 | <0.001 | 0.04 | −0.17, 0.25 | <0.001 | 0.19 | −0.02, 0.39 | <0.001 | −0.03 | −0.24, 0.17 | >0.9 |
| BMI | −0.05 | −0.18, 0.08 | 0.5 | −0.14 | −0.28, −0.01 | 0.042 | −0.05 | −0.18, 0.09 | 0.5 | 0.03 | −0.10, 0.17 | 0.6 |
| Education | 0.04 | −0.09, 0.17 | 0.6 | 0.06 | −0.08, 0.20 | 0.4 | 0.04 | −0.10, 0.18 | 0.6 | −0.13 | −0.27, 0.00 | 0.053 |
| Avoided Bathroom Facilities | 0.7 | 0.7 | 0.4 | 0.14 | ||||||||
| No | – | – | – | – | – | – | – | – | ||||
| Yes | 0.05 | −0.22, 0.32 | 0.06 | −0.23, 0.34 | −0.13 | −0.41, 0.15 | 0.21 | −0.07, 0.50 | ||||
| Difficulty Affording the Basics | −0.07 | −0.20, 0.07 | 0.3 | −0.23 | −0.38, −0.09 | 0.002 | −0.37 | −0.52, −0.23 | <0.001 | 0.09 | −0.05, 0.24 | 0.2 |
| Stress | −0.56 | −0.70, −0.42 | <0.001 | −0.39 | −0.54, −0.24 | <0.001 | −0.26 | −0.41, −0.12 | <0.001 | 0.57 | 0.43, 0.72 | <0.001 |
| Social Integration Score | 0.25 | 0.12, 0.39 | <0.001 | 0.07 | −0.08, 0.21 | 0.3 | 0.23 | 0.09, 0.37 | 0.002 | −0.17 | −0.31, −0.02 | 0.024 |
| Lack of Transportation | 0.4 | 0.11 | 0.090 | 0.7 | ||||||||
| No | – | – | – | – | – | – | – | – | ||||
| Yes | 0.15 | −0.20, 0.49 | −0.30 | −0.66, 0.07 | −0.31 | −0.67, 0.05 | −0.07 | −0.43, 0.30 | ||||
| Exercise | 0.02 | −0.11, 0.16 | 0.7 | 0.13 | −0.02, 0.27 | 0.086 | −0.06 | −0.20, 0.08 | 0.4 | −0.01 | −0.15, 0.13 | 0.9 |
| Current Smoker | 0.4 | 0.6 | >0.9 | 0.6 | ||||||||
| No | – | – | – | – | – | – | – | – | ||||
| Yes | 0.18 | −0.27, 0.63 | −0.14 | −0.62, 0.33 | −0.02 | −0.48, 0.45 | 0.13 | −0.34, 0.60 | ||||
| Past Smoker | 0.4 | 0.8 | 0.2 | 0.4 | ||||||||
| No | – | – | – | – | – | – | – | – | ||||
| Yes | −0.13 | −0.43, 0.16 | 0.04 | −0.28, 0.35 | −0.21 | −0.51, 0.10 | −0.14 | −0.44, 0.17 | ||||
| Alcohol Screening Score | 0.19 | 0.06, 0.32 | 0.005 | 0.09 | −0.05, 0.23 | 0.2 | 0.06 | −0.08, 0.20 | 0.4 | 0.02 | −0.12, 0.16 | 0.8 |
| Time on Hormone Therapy | 0.07 | −0.08, 0.22 | 0.4 | −0.04 | −0.20, 0.12 | 0.6 | −0.05 | −0.21, 0.10 | 0.5 | −0.06 | −0.22, 0.09 | 0.4 |
| Age | 0.07 | −0.10, 0.23 | 0.4 | 0.04 | −0.13, 0.21 | 0.7 | 0.04 | −0.13, 0.21 | 0.6 | 0.10 | −0.07, 0.27 | 0.2 |
| R2 | 0.570 | 0.516 | 0.516 | 0.515 | ||||||||
CI = Confidence Interval (Bootstrapped).
For the psychological domain in our TM cohort, BMI (β: −0.16; −0.29, −0.03), difficulty to afford the basics (β: −0.21; −0.34, −0.08), stress levels (β: −0.44; −0.58, −0.30), social integration score (β: 0.15; 0.02, 0.27), exercise frequency (β: 0.16; 0.04, 0.28), and current smoking status (β: −0.44; −0.87, −0.02) were significantly associated with psychological QoL. For our TF cohort, stress levels (β: −0.56, −0.70, −0.42), social integration score (β: 0.25, 0.12, 0.39), and AUDIT-C scores (β: 0.19; 0.06, 0.32) were significantly associated with psychological QoL.
For the physical domain in our TM cohort, BMI (β: −0.13; −0.25, −0.02), education (β: 0.13; 0.01, 0.26), difficulty to afford the basics (β: −0.40; −0.52, −0.28), stress levels (β: −0.31; −0.44, −0.19), lack of transportation (β: −0.37; −0.65, −0.09), exercise (β: 0.21; 0.09, 0.32), past smoking status (β: 0.35; 0.06, 0.64), and age (β: −0.37; −0.54, −0.19) were significantly associated with physical QoL. For our TF cohort, BMI (β: −0.14; −0.28, −0.01), difficulty affording the basics (β: −0.23; −0.38, −0.09), and stress levels (β: −0.39; −0.54, −0.24) were significantly associated with physical QoL.
For the environmental domain in our TM cohort, an inability to afford the basics (β: −0.52; −0.64, −0.39), stress (β: −0.13; −0.27, 0.00), and lack of transportation (β: −0.59; −0.89, −0.29) were significantly associated with QoL while avoiding bathroom facilities (β: −0.25; −0.50, 0.00; p = 0.052) trended towards significance. In our TF cohort, difficulty affording the basics (β: −0.37; −0.52, −0.23), stress levels (β: −0.26; −0.41, −0.12), and social integration scores (β: 0.23; 0.09, 0.37) were significantly associated with environmental QoL.
On CESD-8 scores, in our TM cohort difficulty affording the basics (β: 0.27; 0.12, 0.43) and stress levels (β: 0.33; 0.17, 0.49) were significantly associated with depressive symptoms, while exercise (β: −0.14; −0.28, 0.00; p = 0.051) trended towards significance. In our TF cohort, stress levels (β: 0.57; 0.43, 0.72) and social integration (β: −0.17; −0.31, −0.02) were significantly associated with depressive symptoms, while education (β: −0.13, −0.27, 0.00; p = 0.053) trended towards significance.
4. Discussion
This study investigates social needs and QoL in TG individuals on GAHT within the MetroHealth system. In this study, QoL scores were similar in TF and TM cohorts receiving GAHT with highest physical satisfaction scores followed by social and environmental satisfaction, and lowest psychological satisfaction scores. This differs from previous reports which have shown social satisfaction to be highest in a cohort of TG patients taking GAHT (Silva et al., 2021) and psychological satisfaction to be highest in a cohort of TF individuals (Thompson et al., 2015). A cross-sectional study of healthy adults in the United States showed scores of the WHOQoL-100 to range from 71.7 to 77.1 for each of the four domains (Bonomi et al., 2000). Median scores in both our TM and TF cohorts were substantially lower than these reported values. In order to understand what factors may be associated with each domain of QoL, we created multivariable regression models with clinical and sociodemographic characteristics.
BMI was a significant predictor for two models (psychological, physical) in our TM cohort compared to one model (physical) in our TF cohort. A prior study reported that 26% of the TG population meet the clinical cut-point for classification with obesity compared to 18% of the cisgender population, comparable to our data (Martinson et al., 2020). The impact of BMI on different domains of QoL in our TG population can be due to several reasons. One is that previous studies have demonstrated a link between decreased psychological QoL and obesity in the general population (Pétré et al., 2016), which can be attributed to reduced daily functioning, increased comorbidities, and increased stigma (Luppino et al., 2010; Papadopoulos and Brennan, 2015; Puhl and Heuer, 2010; Stephenson et al., 2021). TG individuals are also more likely to be obese compared to cisgender individuals due to disparities in access to healthy lifestyle behaviors, consistent medical care, and increased gender minority stress, all of which can contribute to weight gain. In addition, weight stigma, may reinforce high body weight or promote weight gain. Thus, there may be a combination of factors overlapping and contributing to a higher BMI (Brewis, 2014; Hemmingsson et al., 2023; Herbozo et al., 2023; Taormina and Iwamoto, 2023). Finally, GAHT can also impact BMI, however, there is mixed data on its effect. Studies show that BMI in TF individuals typically increases due to a loss of lean muscle and an increase in overall fat mass (Ford et al., 2022) while BMI in TM individuals on GAHT also seems to increase to a higher extent likely due to increased muscle mass due to anabolic effects of testosterone (Bartolucci et al., 2015; Velho et al., 2017).
Social integration was a significant negative predictor for one model (psychological) in TM individuals and three models (psychological, environmental, CESD-8) in TF individuals. Although this questionnaire has been validated previously, to our knowledge, it has not been used in a gender-diverse population. In a previous study performed at MetroHealth, 45% of the surveyed individuals were considered to be socially isolated (Chagin et al., 2021). In our cohort, surveyed before the declaration of the COVID-19 pandemic, this number was even higher at 65%. No prior study has examined social isolation in a clinical sample of gender-diverse persons, but it is well-known that social stigma has a clearly negative impact on overall health, highlighting the importance of social support (Hendricks and Testa, 2012; Meyer, 2003). Prior work has postulated that this association exists because social support influences an individual’s thinking and acting and may enhance their motivation to engage in health promotion (Maida, 1985; Weiss, 1969).
Lack of transportation access was a significant predictor of two QoL domains (physical and environmental) in our TM cohort. In our study, 19% of TF individuals and 21.6% of TM individuals had unmet medical/daily needs due to lack of transportation. There is currently no other published finding on how prevalent transportation inaccessibility is in the gender-diverse population. However, there is inadequate protection against discrimination in public spaces such as public transportation (Reisner et al., 2015) and one known barrier to healthcare is the lack of available transportation (Safer et al., 2016).
Current smoking was a significant negative predictor for psychological QoL in our TM cohort. Additionally, our univariable analysis showed differing results from the literature. 11% of TF individuals and 14% of TM individuals reported smoking currently. These numbers are lower than what has been reported in previous literature, which have been around 32.6% and 39.7% (Buchting et al., 2017; Wheldon and Wiseman, 2019), similar to past cigarette use in our population. Thirty-five percent of TM and 35% of TF individuals reported having smoked at least 100 cigarettes in their lifetime. We hypothesize this discrepancy is due to two reasons. One, TG patients who are receiving GAHT are more likely to follow-up with a health care provider, giving providers additional opportunities to address other comorbidities such as smoking habits. Second, while there is a paucity of data understanding the effects of smoking on GAHT, there is a large amount of literature evaluating the negative effects of smoking for cisgender post-menopausal women utilizing estrogen as hormone-replacement therapy. Some of these effects include decreasing the efficacy of estrogen (Mueck and Seeger, 2005), and higher risks of breast cancer, and stroke, and venous thromboembolism (VTE) (Henderson and Lobo, 2012; Mueck and Seeger, 2005). Of note, an increased risk for VTE in TF individuals in general has been found in some, but not all studies (Arrington-Sanders et al., 2022). Similar data is found in cisgender males, in whom testosterone therapy is associated with an increase in short-term risk for VTE (Walker et al., 2020). Still, it should be considered that testosterone use in TM individuals appears to have a very low risk for serious side effects (Wierckx et al., 2012). According to the published guidelines for primary and gender-affirming care for TG individuals developed by the Center of Excellence for Transgender Health, all TF individuals should be counseled on tobacco risks and cessation options at every visit given the established risks of estrogen use (Sun et al., 2023; UCSF Gender Affirming Health Program, 2016). Therefore, health care providers may be more emphatic in motivating patients to stop smoking before initiation or continuation of GAHT.
4.1. Application of the AUDIT-C questionnaire in gender-diverse individuals
Alcohol use was a significant positive predictor of psychological QoL in TF individuals. Although prior literature indicates that heavy drinking is correlated with higher rates of clinical depression, low/moderate alcohol consumption may be associated with positive mood, which may be captured by our data (Baum-Baicker, 1985). Alcohol use disorder is highly prevalent in TG individuals (James et al., 2016). The United States Preventative Task Force recommends that clinicians screen all adults for alcohol misuse and provide counseling to those who engage in risky/hazardous behavior. One such screening tool is the AUDIT-C questionnaire, which currently screens positive for men scoring four or above and women scoring three or above (Bradley et al., 2003, 2007; Bush et al., 1998). While this tool has several limitations, we present below an additional concern when utilizing these gender/sex-related differences in our gender-diverse population.
Traditionally, substance use disorders have been diagnosed more frequently in cisgender men, despite cisgender women having increasing rates of alcohol consumption and binge drinking (Wilsnack et al., 2000). In response, screening tools were modified to increase sensitivity for cisgender women (Tan et al., 2018). Sex-related differences in neurocircuitry (Logrip et al., 2018), hormone profiles (Sutker et al., 1983), fat and muscle composition (Kwo et al., 1998), body water content (Sutker et al., 1983), and gastric absorption (Thomasson, 1995) affect alcohol metabolism. Additionally, gender-related differences in drinking habits affect alcohol consumption (Gilbert et al., 2018). Little is known about the validity of this screening tool in a gender-diverse population, which is at higher risk of alcohol use disorder. To our knowledge, there are few studies that have assessed the validity and reliability of common alcohol use screening tools such as the AUDIT-C (Flentje et al., 2020), the CAGE questionnaire, and the Michigan Alcoholism Screening Test (MAST) in gender-diverse individuals (Gilbert et al., 2018; Smalley et al., 2016). Additionally, for our study, we utilize the AUDIT-C screening tool separately based on sex assigned at birth and gender (Supplemental Materials; Table S2). Depending on which characteristic was used for the AUDIT-C screening tool, a differing number of individuals screen positive (Table S2). Our data demonstrates and emphasizes the need for improved, more gender-diverse and inclusive definitions of sex and gender’s relationship to alcohol use, as well as further research validating established screening protocols and/or developing new screening protocols for gender-diverse groups.
Time on hormone therapy was not a significant predictor for any of the QoL domains in these cohorts. Prior literature demonstrates that GAHT reduces gender dysphoria, body dissatisfaction, and uneasiness, resulting in an overall improvement in psychological QoL (van Leerdam et al., 2021). Our current study is cross-sectional; further longitudinal data would allow us to examine QoL over time.
Finally, our data showed that 68% of TM individuals, and 39% of TF individuals have reportedly avoided using restrooms because they felt these facilities were inadequate, unsafe, or unfriendly. This is consistent with other studies that reported 49–61.9% of TG individuals made travel decisions based on safe restroom availability (Herman, 2013; Lerner, 2021; Seelman, 2016). We find that TM individuals also report higher rates of stress than their TF counterparts. Stress is a significant predictor for nearly all models in both TM and TF groups. Prior studies have found an association between increased suicidal ideation/attempt and anxiety as well as decreased resilience and QoL, with the ability to safely use public restrooms (Seelman, 2016; Weinhardt et al., 2017). Thus, safe bathroom access may be a likely contributor to overall stress. The minority stress model was established to understand the specific types of unique stressors that minority groups may face. These can be categorized as distal stressors, interactive proximal stressors, and internalized stressors (Hoy-Ellis, 2023). Our work has utilized survey data to identify specific stressors in each category. Distal stressors include financial insecurity, proximal stressors include physical appearance in the form of BMI and social integration, and internalized stressors include drinking behaviors in the form of AUDIT-C scores, exercise, and smoking behaviors. Given these elucidated stressors, the TG resilience intervention model provides critical context for advocating for community, group, and individual interventions at the state and national levels in order to buffer some of these stressors (Matsuno and Israel, 2018).
To date, and to the best of our knowledge, this is one of the largest studies examining a wide range of clinical and sociodemographic characteristics in TM and TF individuals on GAHT. Our analysis of these two separate groups allows us to understand the nuances in differences of how each predictor affects some aspect of well-being based on gender and hormone use. Our sample population is a group of individuals regularly engaging with the MetroHealth care system and receiving GAHT, limiting the generalizability of our results to the wider gender-diverse population. More large-scale prospective studies are needed to better understand the individual relationships uncovered in our regional sample population.
One limitation of this study is that there are several key pieces of data that are known to affect an individual’s well-being that were not captured in this study such as income, insurance status, and employment. Thus, our regression model did not adjust for these variables. Our survey also does not capture significant nuances in individual questions. For instance, we evaluate access to restroom facilities by asking about restroom adequacy, friendliness, and safety. There are multiple ways an individual may interpret this question such as access to gender-neutral bathrooms, the presence of legislation protecting restroom use related to gender identity, or overall public safety for gender-diverse individuals. Thus, there is a limitation on what conclusions we can extrapolate from these data. While we assessed cigarette smoking and marijuana use, we did not account for other methods of smoking such as vaping. Additionally, we did not evaluate individual satisfaction with their embodiment goals of gender transition. There is data that has demonstrated personal and social gender congruence to be associated with improved mental health. Specifically, visual conformity with affirmed gender, also known as ‘passing’, is associated with improved depression and anxiety, less distress, and less public violence, all of which may impact our results (Flynn and Smith, 2021; Peixoto et al., 2022; To et al., 2020). Future studies need to be done to understand these nuanced relationships. Finally, there is a limitation to how much we can generalize the results of this study to the entire TG population. Our inclusion criteria consisted of individuals on GAHT, which implies consistent healthcare and a certain level of access and financial security. Our population is also not widely representative of all racial and ethnic minority groups.
5. Conclusion
This study examines a variety of clinical and sociodemographic characteristics/factors as predictors for QoL in TM and TF groups. For both groups, we find that difficulty affording the basics, stress levels, and social integration are significant social need predictors in at least one model. These data suggest that social circumstances are powerfully associated with QoL and psychological well-being among gender-diverse individuals receiving gender-affirming hormone therapy, with relevant differences between TM and TF individuals.
These data are very relevant in the current political ecology and landscape where state and national legislation is being proposed and/or enacted that perpetuates discrimination against gender-diverse individuals, including increased barriers for adequate healthcare, sport participation, restroom access, and acquiring identification documents with preferred name and gender (Barbee et al., 2022). Previous data has also shown that legislation, such as employment protection for gender minority patients, positively impacts the type of health care TG patients seek out. For example, in states with legal protection, individuals were less likely to present with mood disorders compared to individuals who live in states without such policies (Blosnich et al., 2016). Data from this study may be utilized and leveraged by healthcare providers and policy makers to develop more tailored, acceptable, sensitive, and gender-diverse healthcare services and programming to enhance the overall well-being of TG persons.
Supplementary Material
Acknowledgements
We thank all the participants in the study, Kimberly Schach (study coordinator), Cynthia Newman, Brynna Baird-So, and Drs. Sarah E. Benuska, Jorge Calles-Escandón, Firouz Daneshgari, Mark A. McLoney, Laura J. Mintz, Thomas A. Murphy, Henry Ng, Rahul A. Patel, Erin N. Tomlinson, and Douglas P. Van Auken for their advice and support.
Funding statements
J. Sinopoli was supported by the Chester Summer Scholars Program. A.T. Perzynski was supported by a National institute on Aging award (NIA, 3R01AG055480–04S1). J.P. del Rincon was supported by a National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) K12 award (3R01DK089547–02S1) and by a MetroHealth Population Health Research Institute (PHRI) Pilot Grant.
Footnotes
CRediT authorship contribution statement
Saloni U. Lad: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Conceptualization. Jacob Sinopoli: Methodology. Brian Khong: Methodology. Britt Conroy: Writing – review & editing, Conceptualization. Adam T. Perzynski: Writing – review & editing, Supervision, Methodology, Formal analysis, Conceptualization. Juan P. del Rincon: Writing – review & editing, Supervision, Methodology, Investigation, Funding acquisition, Conceptualization.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2024.116734.
Data availability
The data that has been used is confidential.
References
- Andermann A, 2018. Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Publ. Health Rev. 39, 19. 10.1186/s40985-018-0094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrington-Sanders R, Connell NT, Coon D, Dowshen N, Goldman AL, Goldstein Z, Grimstad F, Javier NM, Kim E, Murphy M, Poteat T, Radix A, Schwartz A, St Amand C, Streed CG, Tangpricha V, Toribio M, Goldstein RH, 2022. Assessing and addressing the risk of venous thromboembolism across the spectrum of gender affirming care: a review. Endocr. Pract. 10.1016/j.eprac.2022.12.008. S1530891X22008989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baguso GN, Aguilar K, Sicro S, Mañacop M, Quintana J, Wilson EC, 2022. “Lost trust in the system”: system barriers to publicly available mental health and substance use services for transgender women in San Francisco. BMC Health Serv. Res. 22, 930. 10.1186/s12913-022-08315-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbee H, Deal C, Gonzales G, 2022. Anti-transgender legislation-A public health concern for transgender Youth. JAMA Pediatr. 176, 125–126. 10.1001/jamapediatrics.2021.4483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartolucci C, Gómez-Gil E, Salamero M, Esteva I, Guillamón A, Zubiaurre L, Molero F, Montejo AL, 2015. Sexual quality of life in gender-dysphoric adults before genital sex reassignment surgery. J. Sex. Med. 12, 180–188. 10.1111/jsm.12758. [DOI] [PubMed] [Google Scholar]
- Baum-Baicker C, 1985. The psychological benefits of moderate alcohol consumption: a review of the literature. Drug Alcohol Depend. 15, 305–322. 10.1016/0376-8716(85)90008-0. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Syme SL, 1979. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am. J. Epidemiol. 109, 186–204. 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- Blosnich JR, Marsiglio MC, Gao S, Gordon AJ, Shipherd JC, Kauth M, Brown GR, Fine MJ, 2016. Mental health of transgender Veterans in US states with and without discrimination and hate Crime legal protection. Am. J. Publ. Health 106, 534–540. 10.2105/AJPH.2015.302981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonomi AE, Patrick DL, Bushnell DM, Martin M, 2000. Validation of the United States’ version of the World health organization quality of life (WHOQOL) instrument. J. Clin. Epidemiol. 53, 1–12. 10.1016/s0895-4356(99)00123-7. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, Maynard C, Burman ML, Kivlahan DR, 2003. Two brief alcohol-screening tests from the alcohol use disorders identification test (AUDIT): validation in a female veterans affairs patient population. Arch. Intern. Med. 163, 821–829. 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR, 2007. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin. Exp. Res. 31, 1208–1217. 10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- Brewis AA, 2014. Stigma and the perpetuation of obesity. Soc. Sci. Med. 118, 152–158. 10.1016/j.socscimed.2014.08.003. [DOI] [PubMed] [Google Scholar]
- Buchting FO, Emory KT, Scout null, Kim Y, Fagan P, Vera LE, Emery S, 2017. Transgender use of cigarettes, cigars, and E-cigarettes in a national study. Am. J. Prev. Med. 53, e1–e7 10.1016/j.amepre.2016.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA, for the Ambulatory Care Quality Improvement Project (ACQUIP), 1998. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch. Intern. Med. 158, 1789–1795. 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Cahill S, Makadon H, 2014. Sexual orientation and gender identity data collection in clinical settings and in electronic health records: a key to ending LGBT health disparities. LGBT Health 1, 34–41. 10.1089/lgbt.2013.0001. [DOI] [PubMed] [Google Scholar]
- Chagin K, Choate F, Cook K, Fuehrer S, Misak JE, Sehgal AR, 2021. A framework for evaluating social determinants of health screening and referrals for assistance. J Prim Care Community Health 12, 21501327211052204. 10.1177/21501327211052204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero EC, Reisner SL, Silva SG, Merwin EI, Humphreys JC, 2019. Healthcare experiences of transgender adults: an integrated mixed research literature review. ANS Adv Nurs Sci 42, 123–138. 10.1097/ANS.0000000000000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Marchis EH, Hessler D, Fichtenberg C, Fleegler EW, Huebschmann AG, Clark CR, Cohen AJ, Byhoff E, Ommerborn MJ, Adler N, Gottlieb LM, 2020. Assessment of social risk factors and interest in receiving health care–based social assistance among adult patients and adult caregivers of pediatric patients. JAMA Netw. Open 3, e2021201. 10.1001/jamanetworkopen.2020.21201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deutsch MB, Buchholz D, 2015. Electronic health records and transgender patients–practical recommendations for the collection of gender identity data. J. Gen. Intern. Med. 30, 843–847. 10.1007/s11606-014-3148-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deutsch MB, Green J, Keatley J, Mayer G, Hastings J, Hall AM, World Professional Association for Transgender Health EMR Working Group, 2013. Electronic medical records and the transgender patient: recommendations from the World professional association for transgender health EMR working group. J. Am. Med. Inf. Assoc. 20, 700–703. 10.1136/amiajnl-2012-001472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo A-L, Leppänen A, Jahkola A, 2003. Validity of a single-item measure of stress symptoms. Scand. J. Work. Environ. Health 29, 444–451. 10.5271/sjweh.752. [DOI] [PubMed] [Google Scholar]
- Feldman JL, Luhur WE, Herman JL, Poteat T, Meyer IH, 2021. Health and health care access in the U.S. Transgender population health (TransPop) survey. Andrology 9, 1707–1718. 10.1111/andr.13052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flentje A, Barger BT, Capriotti MR, Lubensky ME, Tierney M, Obedin-Maliver J, Lunn MR, 2020. Screening gender minority people for harmful alcohol use. PLoS One 15, e0231022. 10.1371/journal.pone.0231022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn S, Smith NG, 2021. Interactions between blending and identity concealment: effects on non-binary people’s distress and experiences of victimization. PLoS One 16, e0248970. 10.1371/journal.pone.0248970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ES, Loucks EB, Berkman LF, 2006. Social integration and concentrations of C-reactive protein among US adults. Ann. Epidemiol. 16, 78–84. 10.1016/j.annepidem.2005.08.005. [DOI] [PubMed] [Google Scholar]
- Ford K, Huggins E, Sheean P, 2022. Characterising body composition and bone health in transgender individuals receiving gender-affirming hormone therapy. J. Hum. Nutr. Diet. 35, 1105–1114. 10.1111/jhn.13027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster Skewis L, Bretherton I, Leemaqz SY, Zajac JD, Cheung AS, 2021. Short-term effects of gender-affirming hormone therapy on dysphoria and quality of life in transgender individuals: a prospective controlled study. Front. Endocrinol. 12, 717766 10.3389/fendo.2021.717766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen Goldsen KI, Romanelli M, Hoy-Ellis CP, Jung H, 2022. Health, economic and social disparities among transgender women, transgender men and transgender nonbinary adults: results from a population-based study. Prev. Med. 156, 106988 10.1016/j.ypmed.2022.106988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gama e Colombo D, 2010. Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. Rev. Direito Sanit. 10, 253. 10.11606/issn.2316-9044.v10i3p253-266. [DOI] [Google Scholar]
- Gilbert PA, Pass LE, Keuroghlian AS, Greenfield TK, Reisner SL, 2018. Alcohol research with transgender populations: a systematic review and recommendations to strengthen future studies. Drug Alcohol Depend. 186, 138–146. 10.1016/j.drugalcdep.2018.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Gil E, Zubiaurre-Elorza L, Esteva de Antonio I, Guillamon A, Salamero M, 2014. Determinants of quality of life in Spanish transsexuals attending a gender unit before genital sex reassignment surgery. Qual. Life Res. 23, 669–676. 10.1007/s11136-013-0497-3. [DOI] [PubMed] [Google Scholar]
- Grant JM, Mottet LA, Tanis JD, 2010. National transgender discrimination survey report on health and health care. Natl Cent Transgender Equal Natl Gay Lesbian Task Force 1, 1–23. [Google Scholar]
- Hemmingsson E, Nowicka P, Ulijaszek S, Sørensen TIA, 2023. The social origins of obesity within and across generations. Obes. Rev. 24, e13514 10.1111/obr.13514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson ER, Jabson J, Russomanno J, Paglisotti T, Blosnich JR, 2019. Housing and food stress among transgender adults in the United States. Ann. Epidemiol. 38, 42–47. 10.1016/j.annepidem.2019.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson VW, Lobo RA, 2012. Hormone therapy and the risk of stroke: perspectives ten years after the Women’s Health Initiative trials. Climacteric 15, 229–234. 10.3109/13697137.2012.656254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks ML, Testa RJ, 2012. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the Minority Stress Model. Prof. Psychol. Res. Pract. 43, 460–467. 10.1037/a0029597. [DOI] [Google Scholar]
- Herbozo S, Brown KL, Burke NL, LaRose JG, 2023. A call to reconceptualize obesity treatment in service of health equity: review of evidence and future directions. Curr Obes Rep 12, 24–35. 10.1007/s13679-023-00493-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman JL, 2013. Gendered restrooms and minority stress: the public regulation of gender and its impact on transgender people’s lives. Soc. Pol. 16. [Google Scholar]
- Hobster K, McLuskey J, 2020. Transgender patients’ experiences of health care. Br. J. Nurs. 29, 1348–1353. 10.12968/bjon.2020.29.22.1348. [DOI] [PubMed] [Google Scholar]
- Hoy-Ellis CP, 2023. Minority stress and mental health: a review of the literature. J. Homosex. 70, 806–830. 10.1080/00918369.2021.2004794. [DOI] [PubMed] [Google Scholar]
- James S, Herman J, Rankin S, 2016. The Report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality, Washington, DC. [Google Scholar]
- Kahn JR, Pearlin LI, 2006. Financial strain over the life course and health among older adults. J. Health Soc. Behav. 47, 17–31. 10.1177/002214650604700102. [DOI] [PubMed] [Google Scholar]
- Kwo PY, Ramchandani VA, O’Connor S, Amann D, Carr LG, Sandrasegaran K, Kopecky KK, Li TK, 1998. Gender differences in alcohol metabolism: relationship to liver volume and effect of adjusting for body mass. Gastroenterology 115, 1552–1557. 10.1016/s0016-5085(98)70035-6. [DOI] [PubMed] [Google Scholar]
- Lerner JE, 2021. Having to “hold it”: factors that influence the avoidance of using public bathrooms among transgender people. Health Soc. Work 46, 260–267. 10.1093/hsw/hlab027. [DOI] [PubMed] [Google Scholar]
- Logrip ML, Milivojevic V, Bertholomey ML, Torregrossa MM, 2018. Sexual dimorphism in the neural impact of stress and alcohol. Alcohol 72, 49–59. 10.1016/j.alcohol.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BWJH, Zitman FG, 2010. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch. Gen. Psychiatr. 67, 220–229. 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Maida CA, 1985. Social support and learning in preventive health care. Soc. Sci. Med. 21, 335–339. 10.1016/0277-9536(85)90110-8. [DOI] [PubMed] [Google Scholar]
- Manieri C, Castellano E, Crespi C, Di Bisceglie C, Dell’Aquila C, Gualerzi A, Molo M, 2014. Medical treatment of subjects with gender identity disorder: the experience in an Italian public health center. Int. J. Transgenderism 15, 53–65. 10.1080/15532739.2014.899174. [DOI] [Google Scholar]
- Martinson TG, Ramachandran S, Lindner R, Reisman T, Safer JD, 2020. High body mass index is A significant barrier to gender-confirmation surgery for transgender and gender-nonbinary individuals. Endocr. Pract. 26, 6–15. 10.4158/EP-2019-0345. [DOI] [PubMed] [Google Scholar]
- Matsuno E, Israel T, 2018. Psychological interventions promoting resilience among transgender individuals: transgender resilience intervention model (TRIM). Counsel. Psychol. 46, 632–655. 10.1177/0011000018787261. [DOI] [Google Scholar]
- Meyer IH, 2003. Prejudice, social stress, and mental health in lesbian, Gay, and bisexual populations: conceptual issues and research evidence. Psychol. Bull. 129, 674–697. 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueck AO, Seeger H, 2005. Smoking, estradiol metabolism and hormone replacement therapy. Curr. Med. Chem. Cardiovasc. Hematol. Agents 3, 45–54. 10.2174/1568016052773270. [DOI] [PubMed] [Google Scholar]
- Nobili A, Glazebrook C, Arcelus J, 2018. Quality of life of treatment-seeking transgender adults: a systematic review and meta-analysis. Rev. Endocr. Metab. Disord. 19, 199–220. 10.1007/s11154-018-9459-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Gurek DT, Henke C, 2018. A practical approach to screening for social determinants of health. FPM 25, 7–12. [PubMed] [Google Scholar]
- Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N, 2013. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am. J. Publ. Health 103, 2056–2062. 10.2105/AJPH.2013.301261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papadopoulos S, Brennan L, 2015. Correlates of weight stigma in adults with overweight and obesity: a systematic literature review. Obesity 23, 1743–1760. 10.1002/oby.21187. [DOI] [PubMed] [Google Scholar]
- Peixoto EM, de Azevedo Oliveira Knupp VM, Soares JRT, Depret DG, de Oliveira Souza C, Messina MED, de Mello Andrade LM, de Melo LCS, de Figueiredo Bezerra D, de Castro CRV, da Silva LMT, Fernandes B, Jalil EM, Friedman RK, de Moura Silva C, Filho EJA, Grinsztejn BGJ, Moreira RI, de Mattos Russo Rafael R, de Souza Velasque L, 2022. Interpersonal violence and passing: results from a Brazilian trans-specific cross-sectional study. J. Interpers Violence 37, NP14397–NP14410. 10.1177/08862605211005152. [DOI] [PubMed] [Google Scholar]
- Pétré B, Scheen AJ, Ziegler O, Donneau A-F, Dardenne N, Husson E, Albert A, Guillaume M, 2016. Body image discrepancy and subjective norm as mediators and moderators of the relationship between body mass index and quality of life. Patient Prefer. Adherence 10, 2261–2270. 10.2147/PPA.S112639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA, 2010. Obesity stigma: important considerations for public health. Am. J. Publ. Health 100, 1019–1028. 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puterman E, Adler N, Matthews KA, Epel E, 2012. Financial strain and impaired fasting glucose: the moderating role of physical activity in the Coronary Artery Risk Development in Young Adults study. Psychosom. Med. 74, 187–192. 10.1097/PSY.0b013e3182448d74. [DOI] [PubMed] [Google Scholar]
- Reisner SL, Hughto JMW, Dunham EE, Heflin KJ, Begenyi JBG, Coffey-Esquivel J, Cahill S, 2015. Legal protections in public accommodations settings: a critical public health issue for transgender and gender-nonconforming people. Milbank Q. 93, 484–515. 10.1111/1468-0009.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safer JD, Coleman E, Feldman J, Garofalo R, Hembree W, Radix A, Sevelius J, 2016. Barriers to health care for transgender individuals. Curr. Opin. Endocrinol. Diabetes Obes. 23, 168–171. 10.1097/MED.0000000000000227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seelman KL, 2016. Transgender adults’ access to college bathrooms and housing and the relationship to suicidality. J. Homosex. 63, 1378–1399. 10.1080/00918369.2016.1157998. [DOI] [PubMed] [Google Scholar]
- Silva ED, Fighera TM, Allgayer RM, Lobato MIR, Spritzer PM, 2021. Physical and sociodemographic features associated with quality of life among transgender women and men using gender-affirming hormone therapy. Front. Psychiatr. 12, 621075 10.3389/fpsyt.2021.621075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smalley KB, Warren JC, Barefoot KN, 2016. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol. 35, 103–114. 10.1037/hea0000231. [DOI] [PubMed] [Google Scholar]
- Stephenson J, Smith CM, Kearns B, Haywood A, Bissell P, 2021. The association between obesity and quality of life: a retrospective analysis of a large-scale population-based cohort study. BMC Publ. Health 21, 1990. 10.1186/s12889-021-12009-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun CJ, Doran KM, Sevelius JM, Bailey SR, 2023. A qualitative examination of tobacco use and smoking cessation among gender minority adults. Ann. Behav. Med. 57, 530–540. 10.1093/abm/kaac072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutker PB, Tabakoff B, Goist KC, Randall CL, 1983. Acute alcohol intoxication, mood states and alcohol metabolism in women and men. Pharmacol. Biochem. Behav. 18 (Suppl. 1), 349–354. 10.1016/0091-3057(83)90198-3. [DOI] [PubMed] [Google Scholar]
- Tan CH, Hungerford DW, Denny CH, McKnight-Eily LR, 2018. Screening for alcohol misuse: practices among U.S. Primary care providers, DocStyles 2016. Am. J. Prev. Med. 54, 173–180. 10.1016/j.amepre.2017.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taormina JM, Iwamoto SJ, 2023. Filling a gap in care: addressing obesity in transgender and gender diverse patients. Int. J. Obes. 47, 761–763. 10.1038/s41366-023-01334-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding, 2011. National Academies Press, Washington, D.C. 10.17226/13128. [DOI] [PubMed] [Google Scholar]
- The WHOQOL Group, 1998. Development of the World health organization WHOQOL-BREF quality of life assessment. The WHOQOL group. Psychol. Med. 28, 551–558. 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- Thomasson HR, 1995. Gender differences in alcohol metabolism. Physiological responses to ethanol. Recent Dev. Alcohol 12, 163–179. 10.1007/0-306-47138-8_9. [DOI] [PubMed] [Google Scholar]
- Thompson HM, Reisner SL, VanKim N, Raymond HF, 2015. Quality-of-Life measurement: assessing the WHOQOL-BREF scale in a sample of high-HIV-risk transgender women in San Francisco, California. Int. J. Transgenderism 16, 36–48. 10.1080/15532739.2015.1039176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- To M, Zhang Q, Bradlyn A, Getahun D, Giammattei S, Nash R, Owen-Smith AA, Roblin D, Silverberg MJ, Tangpricha V, Vupputuri S, Goodman M, 2020. Visual conformity with affirmed gender or “passing”: its distribution and association with depression and anxiety in a cohort of transgender people. J. Sex. Med. 17, 2084–2092. 10.1016/j.jsxm.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UCSF Gender Affirming Health Program, 2016. Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People. [Google Scholar]
- Van de Velde S, Levecque K, Bracke P, 2009. Measurement equivalence of the CES-D 8 in the general population in Belgium: a gender perspective. Arch. Publ. Health 67, 15. 10.1186/0778-7367-67-1-15. [DOI] [Google Scholar]
- van Leerdam TR, Zajac JD, Cheung AS, 2021. The Effect of Gender-Affirming Hormones on Gender Dysphoria, Quality of Life, and Psychological Functioning in Transgender Individuals: A Systematic Review. Transgender Health. 10.1089/trgh.2020.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velho I, Fighera TM, Ziegelmann PK, Spritzer PM, 2017. Effects of testosterone therapy on BMI, blood pressure, and laboratory profile of transgender men: a systematic review. Andrology 5, 881–888. 10.1111/andr.12382. [DOI] [PubMed] [Google Scholar]
- Walker RF, Zakai NA, MacLehose RF, Cowan LT, Adam TJ, Alonso A, Lutsey PL, 2020. Association of testosterone therapy with risk of venous thromboembolism among men with and without hypogonadism. JAMA Intern. Med. 180, 190–197. 10.1001/jamainternmed.2019.5135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinhardt LS, Stevens P, Xie H, Wesp LM, John SA, Apchemengich I, Kioko D, Chavez-Korell S, Cochran KM, Watjen JM, Lambrou NH, 2017. Transgender and gender nonconforming youths’ public facilities use and psychological well-being: a mixed-method study. Transgend Health 2, 140–150. 10.1089/trgh.2017.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RS, 1969. The fund of sociability. Trans-action 6, 36–43. 10.1007/BF02819883. [DOI] [Google Scholar]
- Wheldon CW, Wiseman KP, 2019. Tobacco use among transgender and gender non-conforming adults in the United States. Tob. Use Insights 12. 10.1177/1179173X19849419, 1179173X19849419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wierckx K, Mueller S, Weyers S, Van Caenegem E, Roef G, Heylens G, T’Sjoen G, 2012. Long-term evaluation of cross-sex hormone treatment in transsexual persons. J. Sex. Med. 9, 2641–2651. 10.1111/j.1743-6109.2012.02876.x. [DOI] [PubMed] [Google Scholar]
- Wilsnack RW, Vogeltanz ND, Wilsnack SC, Harris TR, Ahlström S, Bondy S, Csémy L, Ferrence R, Ferris J, Fleming J, Graham K, Greenfield T, Guyon L, Haavio-Mannila E, Kellner F, Knibbe R, Kubicka L, Loukomskaia M, Mustonen H, Nadeau L, Narusk A, Neve R, Rahav G, Spak F, Teichman M, Trocki K, Webster I, Weiss S, 2000. Gender differences in alcohol consumption and adverse drinking consequences: cross-cultural patterns. Addiction 95, 251–265. 10.1046/j.1360-0443.2000.95225112.x. [DOI] [PubMed] [Google Scholar]
- Wolfe HL, Reisman JI, Yoon SS, Blosnich JR, Shipherd JC, Vimalananda VG, Rao SR, Hashemi L, Berlowitz D, Goodman M, Livingston NA, Reece SG, Jasuja GK, 2021. Validating data-driven methods for identifying transgender individuals in the veterans health administration of the US department of veterans affairs. Am. J. Epidemiol. 190, 1928–1934. 10.1093/aje/kwab102. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that has been used is confidential.