Abstract
Background:
Anterior shoulder instability is a common pathology seen especially in young men and highly active patient populations. Subluxation is a commonly encountered clinical issue, yet little is known about the effects of first-time subluxation compared with dislocation on shoulder stability and clinical outcomes after surgical stabilization.
Purpose:
To compare revision and redislocation rates as well as patient-reported outcomes (PROs) between subluxators and dislocators after a first-time anterior shoulder instability event.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Included were patients who underwent operative intervention for a first-time anterior instability event between 2013 and 2020 at a single institution. Exclusion criteria were posterior/multidirectional instability, revision surgery, and recurrent instability. The main outcomes of interest were the rates of redislocation and revision. Demographics and surgical details were retrospectively collected. Instability was categorized as subluxation (no documentation of formal shoulder reduction) or dislocation (documented formal shoulder reduction). Labral tear location and size were determined from preoperative magnetic resonance imaging scans. PROs and return-to-sport, redislocation, and revision rates were collected from prospective survey data.
Results:
A total of 256 patients (141 subluxators and 115 dislocators) were available for analysis. There were no significant differences in baseline demographics or preoperative physical examination findings. Rates of bony Bankart lesions were comparable, but Hill-Sachs lesions were more commonly present in dislocators compared with subluxators (88.7% vs 53.9%; P < .01). There were no group differences in labral tear size, incidence of concomitant posterior or superior labrum anterior-posterior tears, or number of anchors used. Rates of remplissage were comparable between groups. Prospectively collected survey data of 60 patients (35 subluxators, 25 dislocators) were collected at 6.4 and 7.1 years of follow-up, respectively. Rates of recurrent dislocation (11.8% vs 20.0%) and revision (8.8% vs 16.0%) were comparable between subluxators and dislocators, respectively. All PROs and return-to-sport rates were comparable between groups.
Conclusion:
Subluxators and dislocators may present with comparable rates of redislocation and revision surgery even at midterm follow-up. Both cohorts may further present with comparable injury characteristics and PROs. Given the findings, future prospective studies comparing outcomes of first-time instability events are needed.
Keywords: subluxation, dislocation, shoulder, outcomes, anterior shoulder instability
Anterior shoulder instability is a common pathology seen especially in young men, athletes, and other highly active patient populations,11,24,40 with the incidence of subluxations and dislocations reported to be approximately 15% and 85% of all the shoulder instability events in the military population, respectively. 24 Among the pathologies of anterior shoulder instability, traumatic dislocation receives a disproportionately large amount of attention within the literature, likely given the consequences on athlete in-season participation, return to sport/activity, and the likelihood of requiring operative stabilization to prevent recurrent dislocation.5,9,31,37,42
Glenohumeral joint subluxation, traditionally defined as a transient loss of articulation between the glenoid and humerus with spontaneous reduction, has been shown to occur more frequently than dislocation in athletes. 24 While these subluxation events account for 20% of all shoulder injuries in contact athletes,17,19 there is a scarcity of literature characterizing their clinical features, extent of injury, and long-term outcomes. Furthermore, previous studies investigating glenohumeral subluxation have been limited by low sample size and a lack of differentiation between subluxation and dislocation events, increasing the risk for bias and subsequently a lack of predictive, generalizable results.4,12,25,29,39
Given the frequency of young, active individuals affected by glenohumeral subluxation, it is essential to further understand at-risk patients, the extent of injury after subluxation, and how these patients compare to those with dislocation events. Therefore, the purpose of this study was to assess the revision and redislocation rates as well as the patient-reported outcomes (PROs) in subluxators and dislocators at a minimum 2-year follow-up after a first-time anterior shoulder instability event. We hypothesized that subluxators would have lower revision and redislocation rates postoperatively. Secondarily, we hypothesized that subluxators would have a milder clinical presentation and superior postoperative outcomes in comparison with dislocators.
Methods
This study received approval from our institutional review board and included patients >14 years of age who underwent operative intervention for a first-time anterior instability event between 2013 and 2020 at a single institution. The surgeries were performed by fellowship-trained orthopaedic surgeons. There were no absolute indications for surgery for either subluxations or dislocations, but patient counseling and ultimate decisions to proceed with surgery were based on known risk factors for recurrence after first-time instability events, including younger age, contact sports, and male sex. All patients were counseled regardless of instability status (subluxation vs dislocation) based on these risk factors for recurrence without surgery. Surgical techniques included both arthroscopic and open Bankart approach with or without bony Bankart repair, as well as the addition of remplissage. The decision to proceed with an arthroscopic versus open approach was largely based on surgeon preference, yet open approaches were largely reserved for patients with larger amounts of glenoid bone loss, particularly between 10% and 20%. Exclusion criteria were multidirectional instability, recurrent instability, prior ipsilateral shoulder surgery, and incomplete data. Additionally, any patient without preoperative magnetic resonance imaging (MRI) scans was excluded. While the amount of bone loss was not an exclusion criterion, no patients who underwent a bony stabilization procedure (ie, Latarjet and use of distal tibia allograft) were included, as they all had recurrent instability.
Preoperative data on patient characteristics (sex, body mass index, and dominant hand), sport played when the injury occurred, range of motion, and strength were collected. Episodes of first-time anterior instability events were then recorded, and patients were divided into 2 groups based on whether the instability event did not require manual reduction (subluxation) 25 or did require a formal reduction (dislocation).
Imaging Analysis and Measurement of Bipolar Bone Loss
Imaging findings, including Bankart lesions, bony Bankart lesions, Hill-Sachs lesions, rotator cuff tears, and superior labrum anterior-posterior (SLAP) tears on radiographs and MRI scans, were recorded. Additionally, labral tear location and size were determined using the clockface method on MRI, where labral tear size was determined by assigning 1 point unit to each hour around the clockface, for a maximum total value of 12 (Figure 1). 15 Glenoid bone loss and length of Hill-Sachs lesions were measured as previously described, 3 with glenoid bone loss measured on sagittal plane MRI 14 and the Hill-Sachs interval (HSI) measured on axial plane imaging. 13 The glenoid track (GT) was calculated based on the method described by Yamamoto et al. 43 Lastly, distance to dislocation (DTD) was calculated according to Li et al, 21 where on-track Hill-Sachs lesions have a DTD >0 mm, off-track lesions have a DTD ≤0 mm, and near-track lesions are defined as 0 mm < DTD ≤ 10 mm. Bipolar bone loss measurements evaluated on MRI are summarized in Table 1.
Figure 1.
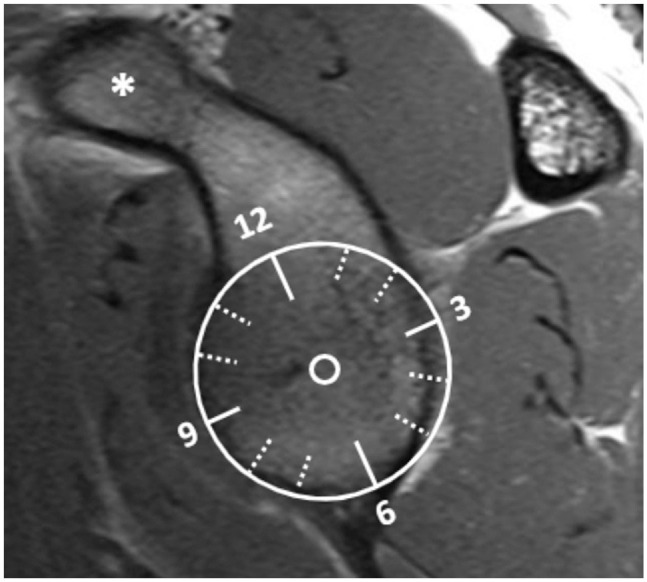
Example of the clockface method 15 utilized on preoperative magnetic resonance imaging to localize location and extent of Bankart lesion. Here, the glenoid face is isolated on sagittal imaging with a superimposed clock face. For consistency with laterality, 3 faces are posterior and 9 faces are anterior. Using this orientation, we can determine the labral tear location and extent. *Coracoid process, providing orientation to the anterior shoulder.
Table 1.
Measurements of Bipolar Bone Loss on MRI a
| Metric | Method of Measurement |
|---|---|
| Glenoid bone loss 14 | Best-fit-circle method: D−d, where D is the diameter of glenoid on sagittal MRI and d is the maximum anterior glenoid bone loss |
| Hill-Sachs interval (HSI) 13 | Distance between medial-most edge of the Hill-Sachs lesion and insertion of infraspinatus tendon on axial MRI |
| Glenoid track (GT) 43 | GT = 0.83 (D − d) |
| Distance to dislocation (DTD) 21 |
GT−HSI On-track: DTD > 0 mm Off-track: DTD ≤ 0 mm Near-track: 0 mm < DTD ≤ 0 mm |
MRI, magnetic resonance imaging.
Inter- and intrarater reliabilities of the MRI measurements were calculated using the intraclass correlation coefficient (ICC), shown to have good (ICC, 0.71) and excellent (ICC, 0.82) inter- and intrarater reliability, respectively, in previous studies.2,3,21 New or missing MRI data were collected by a separate reviewer only after a subset of 30 measurements were made to confirm appropriate interrater reliability and 2 weeks later to confirm interrater reliability.
Intraoperative surgical characteristics of the 2 cohorts were then collected. This included type of surgery (ie, open, arthroscopic, or remplissage) and whether anterior and posterior labral repair or SLAP repair occurred. Additionally, the number of anterior labral anchors was recorded for each patient.
In addition to retrospectively collected data, patients were contacted via survey to collect PROs, including the Subjective Shoulder Value (SSV), Western Ontario Shoulder Instability Index (WOSI) score, Brophy score, and the American Shoulder and Elbow Surgeons (ASES) functional component score, and a return-to-sport questionnaire. Minimal clinically important differences (MCIDs) in the WOSI and ASES scores were assessed based on previous literature.26,27 Lastly, patients were queried regarding both redislocation (requiring formal reduction) and revision (ie, revision instability surgery). Follow-up was defined as the time from index surgery to the time of survey completion. The primary outcome of interest was redislocation and revision rates, while return-to-sport and PRO scores were secondary outcomes of interest.
A post hoc subgroup comparison was made between patients with Hill-Sachs lesions in the subluxator and dislocator cohorts. This was done to address the possibility that there were patients in our first-time subluxator cohort who may have had undisclosed index dislocation events (with Hill-Sachs lesions) before their instability episode that led to treatment and evaluation by the senior surgeon of this study.28,34
Power Analysis
An a priori power analysis was conducted utilizing previously published data on recurrent instability and revision rates after arthroscopic stabilization after subluxation and dislocation in an athletic population. 22 Based on the rates of revision and recurrent instability in individuals with subluxation and dislocation events in the study, 108 dislocators and 135 subluxators were required in the present study to achieve a power of 0.8 (alpha = .05, beta = .2).
Statistical Analyses
Univariate statistical analyses were performed on all included variables. Group comparisons of continuous variables were analyzed by using a Mann-Whitney U test. Categorical variables were compared between groups (subluxators vs dislocators) with the chi-square or Fisher exact test depending on the number of samples in a group. All significance tests were 2-sided, and significance was set at P < .05 for all statistical comparisons (Prism Version 9.3.0; GraphPad).
Results
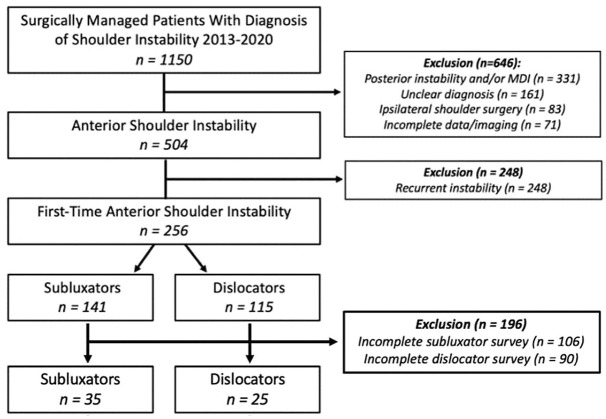
A total of 1150 consecutive patients with a diagnosis of shoulder instability undergoing operative intervention were identified during the study period (Figure 2). After applying exclusion criteria (ie, recurrent anterior instability, posterior and/or multidirectional instability, ipsilateral shoulder surgery, or incomplete data/imaging), 256 first-time anterior instability patients (141 subluxators and 115 dislocators) with a mean age of 23.1 years were available for analysis (Table 2).
Figure 2.
Recurrent instability includes multiple dislocation episodes, acute-on-chronic dislocators, and multiple subluxation events. MDI, multidirectional instability.
Table 2.
Baseline Characteristics of Patients With Glenohumeral Subluxation Versus Dislocations a
| Variable | Subluxator (n = 141) | Dislocator (n = 115) | P |
|---|---|---|---|
| Age, y | 23.4 ± 8.3 | 22.7 ± 6.8 | .52 |
| Male sex | 100 (70.9) | 81 (70.4) | .89 |
| Body mass index | 24.4 [22.2-27.6] | 25.1 [22.7-27.9] | .24 |
| Dominant hand, yes | 60 (42.6) | 51 (44.3) | .78 |
| Bony Bankart, yes | 23 (16.3) | 15 (13.0) | .49 |
| Hill-Sachs lesion, yes | 76 (53.9) | 102 (88.7) | <.01 |
| Rotator cuff tear, yes | 9 (6.4) | 15 (13.0) | .09 |
| SLAP tear, yes | 38 (27.0) | 32 (27.8) | .89 |
| Glenoid bone loss, % | 3.6% [0.0-7.8] | 3.6% [0-7.5] | .98 |
| Hill-Sachs interval, mm | 11.4 ± 6.1 | 7.6 ± 5.6 | <.01 |
| Glenoid track, mm | 21.4 [19.5-23.1] | 21.6 [19.9-23.1] | .96 |
| Distance to dislocation, mm | 13.7 ± 6.6 | 10.2 ± 7.0 | <.01 |
| Labral tear size, mm | 3.0 [2.5-5.0] | 3.0 [2.0-4.0] | .13 |
| Preoperative FF, deg | 170.0 [160.0-170.0] | 170.0 [160.0-180.0] | .63 |
| Preoperative ER, deg | 55.0 [45.0-70.0] | 60.0 [50.0-67.5] | .66 |
| Preoperative Ssp strength grade | .45 | ||
| 1/5 | 1 (0.9) | 0 (0.0) | |
| 4/5 | 21 (18.4) | 12 (13.8) | |
| 5/5 | 92 (80.7) | 75 (86.2) | |
| Preoperative ER strength grade | .44 | ||
| 1/5 | 1 (0.9) | 0 (0.0) | |
| 4/5 | 19 (16.2) | 10 (11.6) | |
| 5/5 | 97 (82.9) | 76 (88.4) | |
| Preoperative IR strength grade | .52 | ||
| 1/5 | 1 (1.0) | 0 (0.0) | |
| 3/5 | 0 (0.0) | 1 (1.2) | |
| 4/5 | 11 (10.8) | 7 (8.6) | |
| 5/5 | 90 (88.2) | 73 (90.1) |
Data are presented as mean ± SD, n (%), or median [IQR]. ER, external rotation; FF, forward flexion; IR, internal rotation; SLAP, superior labrum anterior-posterior; Ssp, supraspinatus. Bolded values denote a significant difference between groups (P < .05).
Of the 256 patients included for final analysis, 127 (49.6%) were contact athletes. Additionally, most (178; 69.5%) were overhead athletes. There were no significant differences between the subluxators (n = 141) and dislocators (n = 115) in baseline patient characteristics including age, sex, body mass index, hand dominance, range of motion, and strength, or in the presence of concomitant bony Bankart lesions, rotator cuff injuries, or SLAP tears (Table 2). Although the HSI was significantly greater for subluxators (11.4 ± 6.1 mm) compared with dislocators (7.6 ± 5.6 mm; P < .01), the GT was similar between subluxators and dislocators (median [IQR], 21.4 mm [19.5-23.1 mm] vs 21.6 mm [19.9-23.1 mm], respectively; P = .96). The DTD was significantly greater for subluxators (13.7 ± 6.6 mm) compared with dislocators (10.2 ± 7.0; P < .01), and Hill-Sachs lesions were less commonly found in subluxators compared with dislocators (54% vs 89%; P < .01).
The majority of both subluxators and dislocators underwent arthroscopic stabilization surgery (86.5% and 78.3%, respectively; P > .05), and there was no difference in the rate of remplissage between the 2 groups. Additionally, the proportion of patients undergoing anterior and posterior labral repair, as well as the median number of anchors anteriorly and posteriorly, were comparable between groups. Rates of SLAP repair and anchors utilized were comparable between groups. At follow-up before administration of the postoperative surveys, revision rates were comparable between groups (subluxators, 15.6%; dislocators, 15.7%; P > .99) (Table 3).
Table 3.
Treatment Characteristics of Patients With Glenohumeral Subluxation Versus Dislocations a
| Variable | Subluxator (n = 141) | Dislocator (n = 115) | P |
|---|---|---|---|
| Type of surgery | .10 | ||
| Arthroscopic | 122 (86.5) | 90 (78.3) | |
| Open | 19 (13.5) | 25 (21.7) | |
| Remplissage b | 19 (14.4) | 9 (8.1) | .16 |
| Anterior labral repair | 125 (88.7) | 103 (89.6) | .84 |
| Anterior anchors | |||
| Median [IQR] | 4 [3-4] | 4 [3-4] | .35 |
| Mean ± SD | 3.1 ± 1.4 | 3.3 ± 1.3 | |
| Posterior labral repair | 42 (29.8) | 32 (27.8) | .96 |
| Posterior anchors | |||
| Median [IQR] | 2 [1-3] | 2 [1-3] | .24 |
| Mean ± SD | 0.7 ± 1.3 | 0.6 ± 1.1 | |
| SLAP repair | 28 (19.9) | 25 (21.7) | .76 |
| SLAP anchors | |||
| Median [IQR] | 2 [1-2] | 1 [1-2] | .26 |
| Mean ± SD | 1.8 ± 1.0 | 1.6 ± 0.7 | |
| Total anchors | |||
| Median [IQR] | 4 [3-5] | 4 [3-5] | .35 |
| Mean ± SD | 4.2 ± 2.2 | 4.0 ± 2.0 | |
| Revisions | 22 (15.6) | 18 (15.7) | >.99 |
Data are presented as n (%) unless otherwise indicated. SLAP, superior labrum anterior-posterior.
No. of subluxators (%)/No. of dislocators (%) of the total remplissage sample: 132 (93.6)/111 (96.5).
A total of 60 patients (35 subluxators, 25 dislocators) completed the outcome surveys at a mean follow-up of 6.8 years (6.4 years for subluxators, 7.1 years for dislocators; P = .25). There were no significant differences between cohorts on any PRO (Table 4). Furthermore, the group differences in the WOSI and ASES scores were 75 points (subluxators, 233; dislocators, 308) and 3.2 points (subluxators, 46.3; dislocators, 43.1), respectively, neither of which reached the MCID based on the available literature.26,27 Both groups had comparable rates of return to sport, although in both groups, only about 50% of the patients reported returning to sport without restrictions. Lastly, the rates of recurrent dislocation (11.8% vs 20.0%; P = .47) and revision surgery (8.8% vs 16.0%; P = .44) were comparable between subluxators and dislocators, respectively (Table 4).
Table 4.
Patient-Reported Outcomes of Patients With Glenohumeral Subluxation Versus Dislocations a
| Patient-Reported Outcome | Subluxator (n = 35) | Dislocator (n = 25) | P |
|---|---|---|---|
| Follow-up, y | 6.4 ± 2.3 | 7.1 ± 1.9 | .25 |
| ASES score | 46.3 ± 4.2 | 43.1 ± 8.3 | .052 |
| WOSI score | 233 [138-427] | 308 [126-878] | .46 |
| Brophy score | 11.8 ± 4.6 | 12.6 ± 4.7 | .55 |
| SSV | 80.8 ± 19.9 | 83.0 ± 16.7 | .64 |
| Return-to-sport questionnaire | |||
| Have you returned to your normal sports or recreational activities? | .71 | ||
| Yes, without restrictions | 17 (48.6) | 13 (52.0) | |
| Yes, modified intensity | 8 (22.9) | 8 (32.0) | |
| No, not returned to sport | 6 (17.1) | 2 (8.0) | |
| Not applicable | 3 (8.6) | 2 (8.0) | |
| Type of sports participation? | .89 | ||
| Contact | 18 (51.4) | 12 (48.0) | |
| Overhead | 21 (60.0) | 16 (64.0) | |
| None | 4 (11.4) | 2 (8.0) | |
| Shoulder redislocation | 4 (11.8) | 5 (20.0) | .47 |
| Further surgery on affected shoulder | 3 (8.6) | 4 (16.0) | .44 |
Data are presented as mean ± SD, n (%), or median [IQR]. ASES, American Shoulder and Elbow Surgeons; SSV, Subjective Shoulder Value; WOSI, Western Ontario Shoulder Instability Index.
Discussion
The most important finding of this study was that in comparison with dislocation events, operatively treated shoulder subluxations resulted in comparable extents of injury to soft tissue and bony structures of the glenohumeral joint complex. Additionally, regardless of whether patients presented with first-time subluxation or dislocation, comparable operative management strategies for bony and soft tissue stabilization were used. Finally, postoperative outcomes and revision rates were comparable between the 2 cohorts, even at a follow-up of nearly 7 years. Given the comparable injury characteristics, revision rates, and outcomes seen in this investigation, further studies evaluating subluxation in the first-time setting and its comparison with dislocation events are warranted.
A 2010 prospective evaluation of first-time anterior shoulder instability demonstrated that glenohumeral subluxation resulted in comparable to dislocation events. 25 In these cases where the humeral head did not lock into a fully dislocated position, a “transient luxation event,” patients shared pathoanatomic findings with patients experiencing dislocation events. These pathological intra-articular findings are supported by other literature reporting labral pathology arthroscopically identified in the majority of cases after both dislocation and subluxation. 35 The current study reinforces this notion of shared pathoanatomy and mechanism of injury between dislocation and subluxation events in the first-time anterior instability event setting, as rates of SLAP tears, overall median labral tear size, and subsequent rates of anterior, posterior, and superior labral repair were similar between the subluxator and dislocator cohorts.
Additionally, this study builds on the more recent body of literature looking at bipolar bone loss and further shows a shared pathoanatomy at initial presentation, as subluxators and dislocators were found to have similar percentages of glenoid bone loss and GT calculations. While the DTD was greater for subluxators compared with dislocators, likely driven by the greater HSI observed in the subluxator cohort, both groups had a mean DTD >10 mm, a threshold value below which recurrent instability after arthroscopic Bankart repair has been shown to increase exponentially. 2 Overall, these similarities in presentation and treatment between the 2 cohorts expound on the findings of recent studies and further support the concept of anterior shoulder instability existing on a continuum rather than there being a black-and-white definition of “subluxation” versus “dislocation.”
Previous research evaluating glenohumeral subluxation demonstrated Hill-Sachs lesions in 50% of patients ultimately requiring shoulder stabilization. 39 Similarly, 53.9% of the patients with subluxation events in the present study presented with Hill-Sachs lesions. While the rate of Hill-Sachs lesions was significantly lower in subluxators, it approached the estimated range of Hill-Sachs lesions observed after first-time dislocations (58%-93%) defined in recent literature. 30 This modest rate within the subluxation cohort, in addition to the finding of a greater HSI in the subluxator cohort, demonstrates that humeral head lesions may play an important role in both subluxation and dislocation events and provide an indication for surgical stabilization regardless of first-time anterior instability event status.
Another finding seen in this study was a high rate of SLAP tears (27.0% vs 27.8% for subluxators and dislocators, respectively). These tears have been described as contributors to anterior shoulder instability and may be present either before the instability event (in the case of overhead athletes) or as a part of a high-energy traumatic instability event.10,32,38 Similarly, posterior labral repairs (29.8% and 27.8% for subluxators and dislocators, respectively) in patients who were evaluated with anterior shoulder instability may have been present before the instability event; however, we did not account for possible anteroinferior labral extension to the posterior glenoid, a finding that should be evaluated in future studies to further develop the algorithm of treatments of first-time instability events.
While previous literature has looked at functional outcomes in patients with recurrent anterior shoulder subluxation and dislocation after stabilization surgery and found no differences in any functional outcomes, 33 a paucity of data exist for first-time anterior shoulder instability events. In this study, PROs from a variety of validated survey instruments, including ASES, WOSI, Brophy, and SSV scores, were collected at a mean follow-up of 6.7 years with no significant differences between cohorts. Additionally, based on previous literature reporting MCID values of ASES and WOSI for 1-year postoperative outcomes after first-time anterior shoulder instability events,26,27 neither cohort met the MCID for either metric. Future studies dedicated to determining MCIDs at midterm follow-up should be performed to determine if this conclusion of similarity still holds at longer follow-up periods.
Return-to-sport rates in patients with anterior shoulder instability after shoulder stabilization have ranged from 37% to 100%.8,9,22 A variety of factors have been examined in return-to-play studies, including age,16,20 sport type, 44 level of play, 7 and type of shoulder stabilization procedure.6,18,23,36 However, return-to-play rates between subluxators and dislocators are infrequently studied in the literature. One 2014 study evaluating return-to-play rates in elite-level athletes with anterior shoulder instability showed that patients with subluxation events were >5 times more likely to return to play than their dislocation counterparts. However, football players made up the majority of athletes (although there was no report of how many football players were in each cohort), and even then the incidence of recurrent instability events remained equivalent between subluxator and dislocator groups. 8 Additionally, there was no report of how many football players were in each cohort, an important distinction that may be a confounding variable. The current study demonstrated comparable return-to-sport rates (subluxators, 71%; dislocators, 84%) at a final follow-up period of nearly 7 years, and overall included a more balanced cohort of contact versus noncontact athletes (subluxators, 51.4% contact athletes; dislocators, 48% contact athletes). However, it is important to note that only about 50% of all participants reported a full return to sport without restrictions, thus warranting further investigation with higher-level studies.
Revision rates after first-time anterior instability event stabilization have been previously reported to range from 5% to 15%. 41 Furthermore, while the general recurrence rate of instability after arthroscopic Bankart repair has been reported to be 14.5%, recurrence rates for high-risk patients (ie, younger, overhead athletes; those with shoulder hyperlaxity; etc) have been shown to approach up to 70%. 1 While many studies have reported on postoperative revision and recurrent instability rates, few studies differentiate between subluxators and dislocators. In the current study, failure rates were comparable between subluxators and dislocators at short-term follow-up (15.6% vs 15.7%, respectively). However, even at longer-term follow-up, albeit with lower response rates, both revision and redislocation rates were comparable between the subluxator and dislocator cohorts. These data suggest that even after shoulder stabilization, both subluxation and dislocation first-time anterior instability events portend a comparable risk of revision and redislocation. For both athletes and surgeons, the findings of this study provide important information on the gravity of these anterior shoulder instability events and suggest that both subluxation and dislocation events should be treated with equal importance when considering treatment options. However, larger and higher-level investigations are needed to further determine demographic and anatomic predictive risk factors influencing outcomes between these 2 populations.
Limitations
There are several limitations to this study. First, given the retrospective nature of this study, the results are subject to selection bias and absence of data available for analysis. Although we included survey data for increased follow-up, a response bias is noted, as only a quarter of initial patients provided responses. Although every attempt was made to obtain responses, the reality is that it was challenging given the young transient population (ie, many patients move after college, often live in different cities for schools/jobs, etc), and therefore this must be considered as a limitation. Additionally, although the definitions of subluxation and dislocation are in line with those used in previous studies, 25 the categorization of primary versus recurrent subluxation depends on accounts from patients, given that there was no manual reduction performed. This is noteworthy, as it may result in an overestimation of primary subluxation events reported in this cohort, especially in those who self-reduce soon after the instability event before muscle spasm has set in. Additionally, even though there were no differences in variables, such as rate of Hill-Sachs lesions, labral tear size, rotator cuff tear size, rate of remplissage, recurrent dislocation, or revision surgery between the groups, it is possible that a difference would have been found in the setting of a larger patient cohort. Furthermore, no data were available on recurrence of those treated nonoperatively, including subluxators, which may have shown a possible bias toward surgery in subluxators with higher risk factors, as well as preoperative examination findings. Lastly, while the current study included a follow-up of nearly 7 years, the results of the a priori power analysis indicated it was underpowered, necessitating larger studies to further evaluate whether subluxation and dislocation events carry equal weight in the surgical treatment algorithm for a first-time anterior instability event.
Conclusion
Subluxators and dislocators may present with comparable rates of redislocation and revision surgery even at midterm follow-up. Both cohorts may further present with comparable injury characteristics and PROs. Given our findings, future prospective studies comparing outcomes of first-time instability events are needed.
Footnotes
Final revision submitted May 1, 2024; accepted May 20, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: I.D.E. has received grant support from Arthrex, education payments from Arthrex and Smith & Nephew, and hospitality payments from Stryker. C.M.G. has received education payments from Mid-Atlantic Surgical Systems. J.J.G. has received grant support from Arthrex, education payments from Arthrex and Smith & Nephew, and hospitality payments from Stryker. J.D.H. has received grant support from Arthrex; education payments from Mid-Atlantic Surgical Systems, Smith & Nephew, and Medical Device Business Services; and hospitality payments from SI-Bone. B.P.L. has received education payments from Mid-Atlantic Surgical Systems. A.L. has received education payments from Arthrex; nonconsulting fees from Arthrex; consulting fees from Arthrex, Stryker, and Wright Medical Technology; and honoraria from Wright Medical Technology. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Pittsburgh Medical Center (reference No. STUDY22100149).
ORCID iDs: Ian D. Engler  https://orcid.org/0000-0002-2951-4991
https://orcid.org/0000-0002-2951-4991
Janina Kaarre  https://orcid.org/0000-0003-2559-8283
https://orcid.org/0000-0003-2559-8283
Robert T. Tisherman  https://orcid.org/0000-0002-9710-808X
https://orcid.org/0000-0002-9710-808X
Christopher M. Gibbs  https://orcid.org/0000-0003-4116-3845
https://orcid.org/0000-0003-4116-3845
Justin J. Greiner  https://orcid.org/0000-0001-6189-6101
https://orcid.org/0000-0001-6189-6101
Jonathan D. Hughes  https://orcid.org/0000-0002-1298-7514
https://orcid.org/0000-0002-1298-7514
References
- 1. Balg F, Boileau P. The Instability Severity Index Score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89(11):1470-1477. [DOI] [PubMed] [Google Scholar]
- 2. Barrow AE, Charles SJ, Issa M, et al. Distance to dislocation and recurrent shoulder dislocation after arthroscopic Bankart repair: rethinking the glenoid track concept. Am J Sports Med. 2022;50(14):3875-3880. [DOI] [PubMed] [Google Scholar]
- 3. Boden SA, Charles S, Hughes JD, et al. Recurrent instability after arthroscopic Bankart repair in patients with hyperlaxity and near-track lesions. Orthop J Sports Med. 2023;11(9):23259671231200231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Burkhead WZ, Jr, Rockwood CA., Jr. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am. 1992;74(6):890-896. [PubMed] [Google Scholar]
- 5. Buss DD, Lynch GP, Meyer CP, Huber SM, Freehill MQ. Nonoperative management for in-season athletes with anterior shoulder instability. Am J Sports Med. 2004;32(6):1430-1433. [DOI] [PubMed] [Google Scholar]
- 6. Ciccotti MC, Syed U, Hoffman R, Abboud JA, Ciccotti MG, Freedman KB. Return to play criteria following surgical stabilization for traumatic anterior shoulder instability: a systematic review. Arthroscopy. 2018;34(3):903-913. [DOI] [PubMed] [Google Scholar]
- 7. Dekker TJ, Goldenberg B, Lacheta L, P., Horan M, Millett PJ. Anterior shoulder instability in the professional athlete: return to competition, time to return, and career length. Orthop J Sports Med. 2020;8(11):2325967120959728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dickens JF, Owens BD, Cameron KL, et al. Return to play and recurrent instability after in-season anterior shoulder instability: a prospective multicenter study. Am J Sports Med. 2014;42(12):2842-2850. [DOI] [PubMed] [Google Scholar]
- 9. Dickens JF, Rue JP, Cameron KL, et al. Successful return to sport after arthroscopic shoulder stabilization versus nonoperative management in contact athletes with anterior shoulder instability: a prospective multicenter study. Am J Sports Med. 2017;45(11):2540-2546. [DOI] [PubMed] [Google Scholar]
- 10. Durban CM, Kim JK, Kim SH, Oh JH. Anterior shoulder instability with concomitant superior labrum from anterior to posterior (SLAP) lesion compared to anterior instability without SLAP lesion. Clin Orthop Surg. 2016;8(2):168-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Galvin JW, Ernat JJ, Waterman BR, Stadecker MJ, Parada SA. The epidemiology and natural history of anterior shoulder instability. Curr Rev Musculoskelet Med. 2017;10(4):411-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Garth WP, Jr, Allman FL, Jr, Armstrong WS. Occult anterior subluxations of the shoulder in noncontact sports. Am J Sports Med. 1987;15(6):579-585. [DOI] [PubMed] [Google Scholar]
- 13. Gyftopoulos S, Beltran LS, Bookman J, Rokito A. MRI Evaluation of bipolar bone loss using the on-track off-track method: a feasibility study. AJR Am J Roentgenol. 2015;205(4):848-852. [DOI] [PubMed] [Google Scholar]
- 14. Gyftopoulos S, Beltran LS, Yemin A, et al. Use of 3D MR reconstructions in the evaluation of glenoid bone loss: a clinical study. Skeletal Radiol. 2014;43(2):213-218. [DOI] [PubMed] [Google Scholar]
- 15. Hansen CH, Asturias AM, Pennock AT, Edmonds EW. Adolescent posterior-superior glenoid labral pathology: does involvement of the biceps anchor make a difference? Am J Sports Med. 2020;48(4):959-965. [DOI] [PubMed] [Google Scholar]
- 16. Harada Y, Iwahori Y, Kajita Y, et al. Return to sports after arthroscopic Bankart repair in teenage athletes: a retrospective cohort study. BMC Musculoskelet Disord. 2023;24(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hudson RA, Baker RT, Nasypany A, Reordan D. Treatment of anterior shoulder subluxation using the Mulligan concept and reflex neuromuscular stabilization: a case report. Int J Sports Phys Ther. 2017;12(1):155-162. [PMC free article] [PubMed] [Google Scholar]
- 18. Hurley ET, Montgomery C, Jamal MS, et al. Return to play after the Latarjet procedure for anterior shoulder instability: a systematic review. Am J Sports Med. 2019;47(12):3002-3008. [DOI] [PubMed] [Google Scholar]
- 19. Kaplan LD, Flanigan DC, Norwig J, Jost P, Bradley J. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med. 2005;33(8):1142-1146. [DOI] [PubMed] [Google Scholar]
- 20. Kasik CS, Rosen MR, Saper MG, Zondervan RL. High rate of return to sport in adolescent athletes following anterior shoulder stabilisation: a systematic review. J ISAKOS. 2019;4(1):33-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li RT, Kane G, Drummond M, et al. On-track lesions with a small distance to dislocation are associated with failure after arthroscopic anterior shoulder stabilization. J Bone Joint Surg Am. 2021;103(11):961-967. [DOI] [PubMed] [Google Scholar]
- 22. Lu Y, Okoroha KR, Patel BH, et al. Return to play and performance after shoulder instability in National Basketball Association athletes. J Shoulder Elbow Surg. 2020;29(1):50-57. [DOI] [PubMed] [Google Scholar]
- 23. Murphy AI, Hurley ET, Hurley DJ, Pauzenberger L, Mullett H. Long-term outcomes of the arthroscopic Bankart repair: a systematic review of studies at 10-year follow-up. J Shoulder Elbow Surg. 2019;28(11):2084-2089. [DOI] [PubMed] [Google Scholar]
- 24. Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35(7):1168-1173. [DOI] [PubMed] [Google Scholar]
- 25. Owens BD, Nelson BJ, Duffey ML, et al. Pathoanatomy of first-time, traumatic, anterior glenohumeral subluxation events. J Bone Joint Surg Am. 2010;92(7):1605-1611. [DOI] [PubMed] [Google Scholar]
- 26. Park I, Lee JH, Hyun HS, Lee TK, Shin SJ. Minimal clinically important differences in Rowe and Western Ontario Shoulder Instability Index scores after arthroscopic repair of anterior shoulder instability. J Shoulder Elbow Surg. 2018;27(4):579-584. [DOI] [PubMed] [Google Scholar]
- 27. Park I, Oh MJ, Shin SJ. Minimal clinically important differences and correlating factors for the Rowe score and the American Shoulder and Elbow Surgeons score after arthroscopic stabilization surgery for anterior shoulder instability. Arthroscopy. 2019;35(1):54-59. [DOI] [PubMed] [Google Scholar]
- 28. Provencher MT, Frank RM, Leclere LE, et al. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg. 2012;20(4):242-252. [DOI] [PubMed] [Google Scholar]
- 29. Rowe CR, Zarins B. Recurrent transient subluxation of the shoulder. J Bone Joint Surg Am. 1981;63(6):863-872. [PubMed] [Google Scholar]
- 30. Rutgers C, Verweij LPE, Priester-Vink S, et al. Recurrence in traumatic anterior shoulder dislocations increases the prevalence of Hill-Sachs and Bankart lesions: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30(6):2130-2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shanley E, Thigpen C, Brooks J, et al. Return to sport as an outcome measure for shoulder instability: surprising findings in nonoperative management in a high school athlete population. Am J Sports Med. 2019;47(5):1062-1067. [DOI] [PubMed] [Google Scholar]
- 32. Sheean AJ, Kibler WB, Conway J, Bradley JP. Posterior labral injury and glenohumeral instability in overhead athletes: current concepts for diagnosis and management. J Am Acad Orthop Surg. 2020;28(15):628-637. [DOI] [PubMed] [Google Scholar]
- 33. Shin SJ, Ko YW, Jeon YS, Lee J, Kim RG, Baek H. Comparison of intra-articular findings and clinical features between patients with symptomatic anterior instability after recurrent shoulder subluxation and dislocation. Arthroscopy. 2017;33(3):527-533. [DOI] [PubMed] [Google Scholar]
- 34. Taylor DC, Arciero RA. Pathologic changes associated with shoulder dislocations. Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. Am J Sports Med. 1997;25(3):306-311. [DOI] [PubMed] [Google Scholar]
- 35. Tischer T, Vogt S, Kreuz PC, Imhoff AB. Arthroscopic anatomy, variants, and pathologic findings in shoulder instability. Arthroscopy. 2011;27(10):1434-1443. [DOI] [PubMed] [Google Scholar]
- 36. Uhorchak JM, Arciero RA, Huggard D, Taylor DC. Recurrent shoulder instability after open reconstruction in athletes involved in collision and contact sports. Am J Sports Med. 2000;28(6):794-799. [DOI] [PubMed] [Google Scholar]
- 37. Vaswani R, Gasbarro G, Como C, et al. Labral morphology and number of preoperative dislocations are associated with recurrent instability after arthroscopic Bankart repair. Arthroscopy. 2020;36(4):993-999. [DOI] [PubMed] [Google Scholar]
- 38. Virk MS, Arciero RA. Superior labrum anterior to posterior tears and glenohumeral instability. Instr Course Lect. 2013;62:501-514. [PubMed] [Google Scholar]
- 39. Warren RF. Subluxation of the shoulder in athletes. Clin Sports Med. 1983;2(2):339-354. [PubMed] [Google Scholar]
- 40. Waterman B, Owens BD, Tokish JM. Anterior shoulder instability in the military athlete. Sports Health. 2016;8(6):514-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Waterman BR, Leroux T, Frank RM, Romeo AA. The evaluation and management of the failed primary arthroscopic Bankart repair. J Am Acad Orthop Surg. 2020;28(15):607-616. [DOI] [PubMed] [Google Scholar]
- 42. Watson S, Allen B, Grant JA. A clinical review of return-to-play considerations after anterior shoulder dislocation. Sports Health. 2016;8(4):336-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg. 2007;16(5):649-656. [DOI] [PubMed] [Google Scholar]
- 44. Yamamoto N, Kijima H, Nagamoto H, et al. Outcome of Bankart repair in contact versus non-contact athletes. Orthop Traumatol Surg Res. 2015;101(4):415-419. [DOI] [PubMed] [Google Scholar]