Abstract
Purpose
Therapies for treatment of rheumatoid arthritis (RA) have shown significant improvement since the introduction of biological agents (BIO) in 2003 and Janus kinase inhibitors (JAKi) in 2013 in Japan. The rate of orthopedic surgery, including total hip arthroplasties (THA), may reflect trends in disease severity, management, and health outcomes.
Materials and Methods
An analysis of data on THAs performed at our institutes for treatment of RA with BIO or non-BIO therapy from 2004 to 2021 was conducted.
Results
A total of 40,328 orthopedic surgeries, including 5,938 primary THAs and 204 RA-THAs, were performed between 2004 and 2021. An increase in the annual rate of THA performed for patients undergoing orthopedic surgery was observed. The rates of THA decreased annually for patients with RA when compared to the total number of orthopedic surgeries and primary THAs performed.
Conclusion
The number of THAs performed for patients with RA may show an annual decrease resulting from early and aggressive drug therapy for management of RA in the era of BIO and JAKi. However, patients with RA undergoing THA have several unmet needs, including secondary osteoarthritis, dislocation, periprosthetic joint infection, and periprosthetic fracture with osteoporosis.
Keywords: Total hip arthroplasties, Rheumatoid arthritis, Biological agents, Janus kinase inhibitors
INTRODUCTION
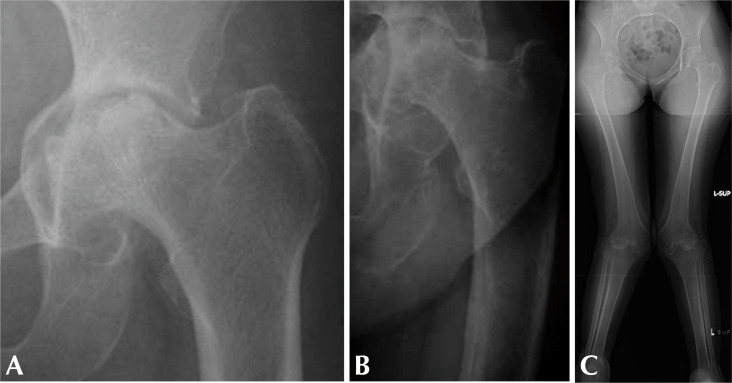
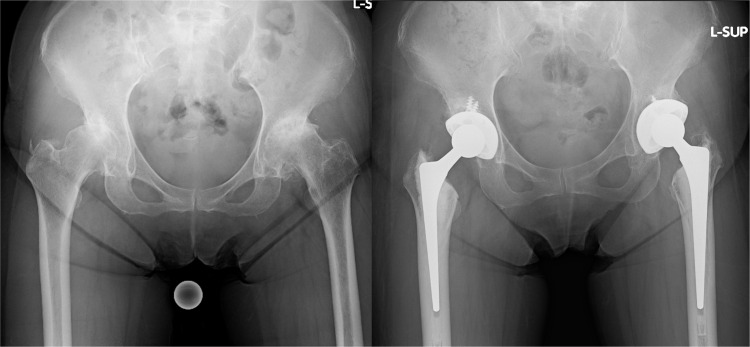
Rheumatoid arthritis (RA), an inflammatory disease, is associated with joint destruction. Joint destruction has been reported in small joints including the hand or foot, as well as in large joints, including the hip and knee1,2). In cases of hip joint damage caused by RA-associated inflammation, the ability to stand and walk is diminished, thus, activities of daily living and quality of life tend to show a rapid decrease in patients with RA2-5). Before the era of the biological agents (BIO) and Janus kinase inhibitors (JAKi), joint arthroplasty performed within 10 years after the onset of RA was associated with a high level of disease activity and mortality6,7). In addition, an Otto pelvis or protrusio acetabuli with a Dorr type C8) femoral canal, indicating the elongation of the femoral medullary cavity, was observed as part of the typical hip destruction observed in patients with severe RA9,10) (Fig. 1A, B). In many patients with severe RA, examination of the entire leg showed valgus deformity of the lower legs with flexion contracture of the knee (Fig. 1C) before the era of BIO and JAKi.
Fig. 1.
A typical X-ray of hip destruction in patients with rheumatoid arthritis shows Otto pelvis, protrusio acetabuli (A), and a Dorr type C femoral canal (elongation of the medullary cavity) (B) before the era of BIO and JAKi. (C) Valgus deformity of the lower legs with flexion contracture of the knee. BIO: biological agents, JAKi: Janus kinase inhibitors.
Since 2000, knowledge regarding treatment strategies that can be applied in clinical practice along with the availability of newer disease-modifying anti-rheumatic drugs, including BIO and JAKi, has led to a paradigm shift in the treatment of RA.
In Japan, methotrexate (MTX) up to 8 mg per week was approved as an RA drug in 1999, and the first BIO was approved in 2003. The allowable dose of MTX was then increased to 16 mg/week in 2011. The first JAKi was approved in 201310-12). The rate of orthopedic surgery and total hip arthroplasty (THA) may reflect trends in disease severity, management, and health outcomes in the era of BIO and JAKi, based on the rapid advancement of RA treatment since 20039,13,14).
The objective of this study is to determine the number and rate of orthopedic surgeries and THAs performed between 2004 and 2021 among patients with RA from our orthopedic surgery and total joint arthroplasty registry.
MATERIALS AND METHODS
1. Study Design
The number and rate of orthopedic surgeries and THAs performed between 2004 and 2021 on patients with RA who were admitted to our institutes (Yamagata University Hospital and Yamagata Saisei Hospital) was determined using our orthopedic surgery and total joint arthroplasty registry10). Cemented THAs were performed in all cases from 2004 to 2016. Hybrid THAs (cementless cup and cemented stem) have also been performed since 2017. In 2021, hybrid THAs were performed in 72% of primary THAs, including patients with RA. Composite beam stems (YU stem; Kyocera) were used from 2004 to 2014. However, we began use of loaded taper stems in 2015 (Exeter [Stryker], CPT stem [Zimmer], C-stem [Depuy], or DTP stem [Kyocera]).
Data on patients who underwent THA including the use of diagnostic procedure combination systems and complications of THA were collected from medical records, surgical records, and shipment documents for orthopedic implants. All THAs were performed using the posterior approach from 2004 to 2021. Patients who presented with many dislocations were counted as one case in this study.
The study protocol, which adheres to the principles of the 2013 Declaration of Helsinki, was approved by the Ethics Committee of Yamagata University (No. 2008-102, H27-163). The written informed consent was waived by the Ethics Committee due to the retrospective nature of the study.
2. Statistical Analysis
Univariable regression analyses were performed using the Mann–Whitney U test and Spearman’s correlation analysis was performed using IBM SPSS Statistics software (ver. 25; IBM Corp.) for comparison of data. Values of P<0.05 were considered statistically significant.
RESULTS
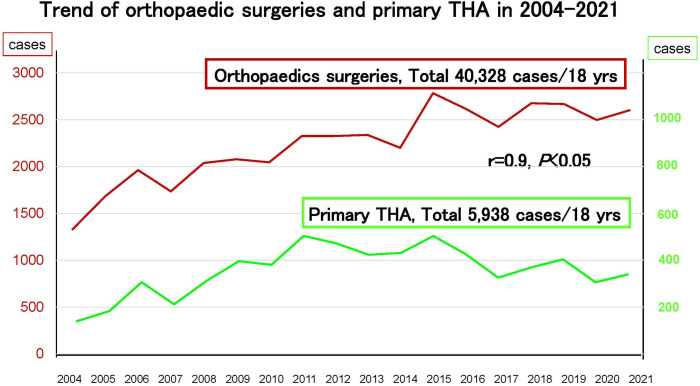
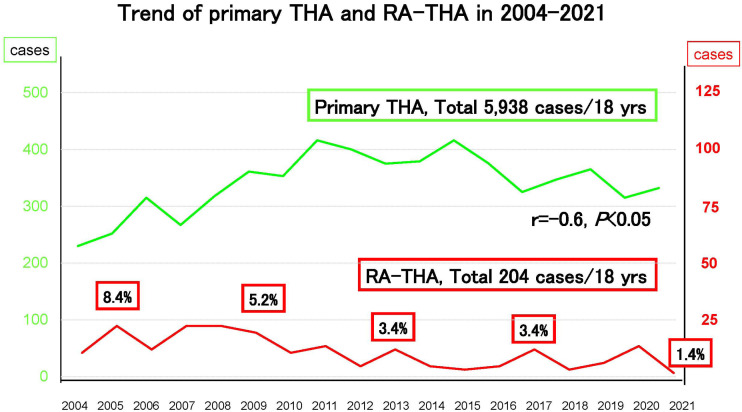
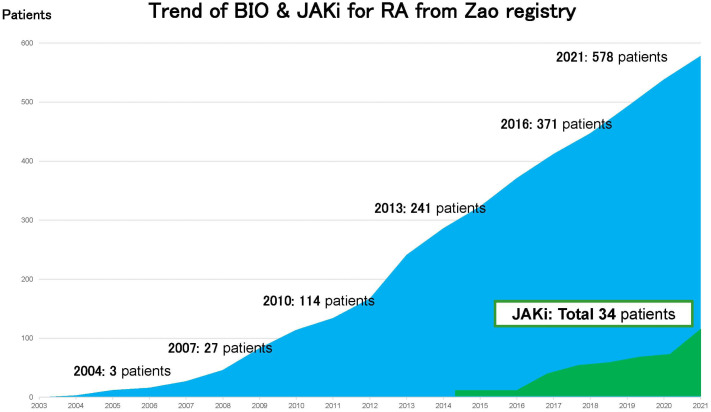
A total of 40,328 orthopedic surgeries were performed from 2004 to 2021 in our institutes. A total of 5,938 primary THAs and 204 RA-THAs were performed or supervised by 12 senior hip surgeons over 18 years. Of 40,328 orthopedic surgeries, 5,938 primary THAs were performed from 2004 to 2021 in our institutes (Fig. 2). The rate of primary THA showed a direct increase along with orthopedic surgeries (r=0.9, P<0.05). Of these, 204 RA-THAs were performed from 2004 to 2021. The rate of RA-THA showed a slight negative correlation with the rate of primary THA (r=–0.6, P<0.05; Fig. 3)10). The rate of THA performed on patients with RA per annual primary THA showed a decline, in particular, by 4.0% (13/329) in 2020 and by 1.4% (5/352) in 2021, which may have been related to the impact of the coronavirus disease 2019 (COVID-19) pandemic in 2020 and 2021. The total number of orthopedic surgeries and primary THAs performed during 2013-2021 increased and was higher than during 2004-2012; however, the number of RA-THAs decreased by half (Table 1). According to our Zao registry, usage of BIO and JAKi has shown an annual increase (Fig. 4)10).
Fig. 2.
Trend of orthopedic surgeries with primary THA in our institutes. A total of 40,328 orthopedic surgeries, including 5,938 primary THA, were performed from 2004 to 2021. THA: total hip arthroplasty.
Fig. 3.
Trend of orthopedic surgeries with primary THA with RA-THA in our institutes. A total of 204 RA-THAs were performed from 2004 to 2021. The rate of RA-THA showed a slight negative correlation with primary THA. THA: total hip arthroplasty, RA: rheumatoid arthritis.
Table 1.
Trends of Orthopedic Surgeries and RA-THA
| 2004-2012 | 2013-2021 | 2013-2021/2004-2012 | Total (2004-2021) | |
|---|---|---|---|---|
| Orthopedic surgeries | 17,524 | 22,804 | (1.3 times) | 40,328 |
| Primary THA | 2,673 | 3,265 | (1.2 times) | 5,938 |
| RA-THA | 128 | 76 | (0.6 times) | 204 |
Values are presented as number only or times only.
RA: rheumatoid arthritis, THA: total hip arthroplasty.
Fig. 4.
The trend of BIO and JAKi for RA from our Zao registry10). The usage of BIO and JAKi has increased year by year. BIO: biological agents, JAKi: Janus kinase inhibitors, RA: rheumatoid arthritis.
The occurrence rate for dislocations of primary THA was 1.1% (65/5,938), including 2.9% (6/204) for patients with RA. The rate of dislocation for patients who underwent RA-THA was higher than that for all patients who underwent THA (P<0.05). The occurrence rate for periprosthetic fracture (PPF) was 0.3% (15/5,938) for primary THA, including 1.0% (2/204) for patients with RA (Table 2).
Table 2.
Dislocation and Periprosthetic Fracture Rate in Non–RA-THA and RA-THA in 2004-2021
| Non–RA-THA (n=5,734) | RA-THA (n=204) | Total (n=5,938) | |
|---|---|---|---|
| Dislocation | 59 (1.0)* | 6 (2.9)* | 65 (1.1)* |
| Periprosthetic fracture | 13 (0.2) | 2 (1.0) | 15 (0.3) |
Values are presented as number (%).
RA: rheumatoid arthritis, THA: total hip arthroplasty.
*P<0.05.
Revisions of THA were performed in 561 cases including 16 cases with RA from 2004 to 2021. Of these, aseptic loosening in 13 cases (81.3%), infection in two cases (12.5%), and frequent dislocation of the THA in one case were the reasons for THA revision in patients with RA (6.3%) (Table 3).
Table 3.
Cause of Revision THA in Patients with Non-RA or RA in 2004-2021
| Cause of revision THA | Non–RA-revision THA | RA-revision THA | Total |
|---|---|---|---|
| Aseptic loosening | 376 (69.0) | 13 (81.3) | 389 (69.3) |
| Infection | 77 (14.1) | 2 (12.5) | 79 (14.1) |
| Frequent dislocation | 69 (12.7) | 1 (6.3) | 70 (12.5) |
| Periprosthetic fracture | 18 (3.3) | 0 | 18 (3.2) |
| Breakage | 5 (0.9) | 0 | 5 (0.9) |
| Total | 545/561 (97.1) | 16/561 (2.9) | 561 |
Values are presented as number (%).
THA: total hip arthroplasty, RA: rheumatoid arthritis.
DISCUSSION
1. Trend of Hip Joint Destruction in Patients with RA in the BIO and JAKi Era
THA is regarded as an effective procedure for treating hip joint destruction in patients with musculoskeletal diseases including RA. However, the rate of orthopedic surgery including THA, decreased for patients with RA, reflecting trends in disease severity in the era of BIO and JAKi5,6,9,15-18).
According to data from the Finnish Coxa Hospital registry, total joint arthroplasties have decreased since 1990 compared to the period before approval of MTX and BIO15). According to the UK and Canada registry of THA, the frequency of RA-THAs performed in patients with RA has decreased in the BIO era in the United Kingdom of Great Britain and Northern Ireland (UK) and Canada19). In addition, according to the Japanese registry of RA surgeries, the Institute of Rheumatology, Rheumatoid Arthritis (IORRA) cohort, RA surgeries and RA-THAs have shown an annual decrease. However, the number of hand and foot surgeries for treatment of RA has increased in the IORRA cohort12).
2. Current Hip Joint Changes in Patients with RA in the BIO and JAKi Era
Several surgeons have reported that progression of joint destruction due to RA and osteoarthritis (OA) with osteoporosis continues, particularly in large joints with a Larsen grade II or higher severity, despite the potential for remission of RA20,21). In Japan, destruction due to RA-associated synovitis and OA change with mild acetabular dysplasia appears to be the characteristic feature of hip destruction in patients undergoing RA-THA (Fig. 5).
Fig. 5.
The characteristic feature of hip destruction in patients undergoing RA-THA appears to be a result of RA synovitis and OA change with mild acetabular dysplasia in the era of BIO and JAKi in Japan. RA: rheumatoid arthritis, THA: total hip arthroplasty, OA: osteoarthritis, BIO: biological agents, JAKi: Janus kinase inhibitors.
Tsushima et al.22) reported a decrease in performance of RA-THA in 2013-2019 compared to 1998-2003. The current changes in the hip joint observed in RA patients are similar to the primary changes in OA that were characterized radiographically by the development of capital drop and decreased central migration.
Regarding RA-knee, a deep learning model for classifying anteroposterior knee radiographs according to “RA” and “OA-like RA” groups was developed by Takeda et al.23). They reported that the percentage of “OA-like RA” showed a significant increase from 20.9% in 2006 to 67.7% in 2020. However, it appears that RA-knee is not the same as OA-knee. Nejima et al.24) reported that the entire lower limb alignment was more valgus in patients with RA-knee compared to those with OA-knee. In addition, Jensen et al.25) reported that the histological findings of the femoral head in RA, which they termed secondary OA, differed from those of the femoral head in OA.
The complications affecting patients who had undergone RA-THA differed from those of patients who underwent OA-THA. According to a single large center study conducted in Australia, increasing rates of dislocation were reported, similar rates of infection and aseptic loosening were observed, and decreasing rates of revision and PPF were observed for RA-THA compared to OA-THA26). Although higher rates of dislocation were observed, a higher prevalence of PPF was not observed in this study. These results might be explained by the primary use of composite beam stems in performance of RA-THA27-29). In addition, although aseptic loosening was the most common reason for THA revision, it may not detect the sources of infection in cases of THA revision30). In fact, use of antibiotic bone cement during performance of primary THA was reported to decrease the rate of THA revision31,32).
3. Elderly Patients with RA and Late-onset of RA
The global prevalence of elderly patients with RA and late-onset RA is increasing33). The population of Japan is increasing faster than that of any other country34). Fractures caused by osteoporosis are a significant problem for the elderly. In the IORRA study, it was reported as a significant risk factor for fractures in Japanese patients with RA35). In Cox regression models, risk factors for fracture in patients with RA included a health assessment questionnaire (HAQ), age, history of fractures, and orthopedic surgeries. The reported rate of PPF in patients with RA ranged from 0.3% to 2.5%26,35). According to the general practitioner database, the risks of pelvic and vertebral fractures tend be higher for patients with RA compared with control subjects in the UK36). Ravi et al.37) reported that the surgeon’s experience in performance of total joint arthroplasties for treatment of patients with RA influenced a direct decline in surgical complications. In addition, efforts to improve our surgical strategies and techniques for management of patients with RA should continue.
4. Limitations
This study has several limitations. First, some patients living outside our local area visited our institutes to undergo THA. Any complications of THA occurring in a patient who lives outside our local area might be treated at secondary and tertiary care facilities located in their area. Therefore, some cases are not included in our registry. Second, we collected information on cases of infection following THA on patients who underwent THA revision, but not all cases. We were not able to investigate cases involving patients who chose conservative therapy or debridement of infectious THA. Last, we were not able to obtain clinical data on RA, including disease activity score and history of medication. Considering the limitations of this study, conduct of additional research will be required to confirm our findings.
CONCLUSION
Prior to the era of BIO and JAKi, joint arthroplasty performed within 10 years after the onset of RA was associated with a high level of disease activity and mortality. Significant advancements in RA therapy were reported around 2003, and disease activity showed improvement over the long term in Japan.
Due to early and aggressive drug therapy for treatment of RA in the era of BIO and JAKi, a decrease in the annual number of THAs performed on patients with RA may occur. Even in the era of BIO and JAKi, patients with RA undergoing THA have several unmet needs, including secondary OA, dislocation, PPF with osteoporosis, and periprosthetic joint infection.
Funding Statement
Funding No funding to declare.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79:685–99. doi: 10.1136/annrheumdis-2019-216655. https://doi.org/10.1136/annrheumdis-2019-216655. [DOI] [PubMed] [Google Scholar]
- 2.Tanaka S, Kobayashi M, Saito K, Takita A. Impact of denosumab discontinuation on changes in bone mineral density and bone erosion in rheumatoid arthritis patients. Mod Rheumatol. 2022;32:284–91. doi: 10.1093/mr/roab022. https://doi.org/10.1093/mr/roab022. [DOI] [PubMed] [Google Scholar]
- 3.Takakubo Y, Takagi M, Tamaki Y, et al. Mid-term results of joint-preserving procedures by a modified Mann method for big toe deformities in rheumatoid patients undergoing forefoot surgeries. Mod Rheumatol. 2010;20:147–53. doi: 10.1007/s10165-009-0253-2. https://doi.org/10.1007/s10165-009-0253-2. [DOI] [PubMed] [Google Scholar]
- 4.Mochida Y, Saito I, Akamatsu Y, Taki N, Mitsugi N, Saito T. Clinical and radiological results of non-cement impaction bone-graft method of total hip arthroplasty for rheumatoid arthritis. Mod Rheumatol. 2007;17:235–8. doi: 10.1007/s10165-007-0571-1. https://doi.org/10.1007/s10165-007-0571-1. [DOI] [PubMed] [Google Scholar]
- 5.Massardo L, Gabriel SE, Crowson CS, O'Fallon WM, Matteson EL. A population based assessment of the use of orthopedic surgery in patients with rheumatoid arthritis. J Rheumatol. 2002;29:52–6. [PubMed] [Google Scholar]
- 6.Shourt CA, Crowson CS, Gabriel SE, Matteson EL. Orthopedic surgery among patients with rheumatoid arthritis 1980-2007: a population-based study focused on surgery rates, sex, and mortality. J Rheumatol. 2012;39:481–5. doi: 10.3899/jrheum.111056. https://doi.org/10.3899/jrheum.111056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pincus T, Sokka T, Chung CP, Cawkwell G. Declines in number of tender and swollen joints in patients with rheumatoid arthritis seen in standard care in 1985 versus 2001: possible considerations for revision of inclusion criteria for clinical trials. Ann Rheum Dis. 2006;65:878–83. doi: 10.1136/ard.2005.044131. https://doi.org/10.1136/ard.2005.044131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993;14:231–42. doi: 10.1016/8756-3282(93)90146-2. https://doi.org/10.1016/8756-3282(93)90146-2. [DOI] [PubMed] [Google Scholar]
- 9.Momohara S, Yano K, Sakuma Y, Ikari K. Recent orthopedic surgeries aiming to improve quality of life for patients with rheumatoid arthritis. J Rheumatol. 2016;43:245. doi: 10.3899/jrheum.150238. https://doi.org/10.3899/jrheum.150238. [DOI] [PubMed] [Google Scholar]
- 10.Takakubo Y, Ito J, Momma R, et al. Trend of orthopaedic surgeries for the patients with rheumatoid arthritis who are received biologic agents in our institute. Jpn Soc Replace Arthroplast. 2022;52:675–6. Japanese. [Google Scholar]
- 11.Yamanaka H, Seto Y, Tanaka E, et al. Management of rheumatoid arthritis: the 2012 perspective. Mod Rheumatol. 2013;23:1–7. doi: 10.1007/s10165-012-0702-1. https://doi.org/10.1007/s10165-012-0702-1. [DOI] [PubMed] [Google Scholar]
- 12.Yamanaka H, Tanaka E, Nakajima A, et al. A large observational cohort study of rheumatoid arthritis, IORRA: providing context for today's treatment options. Mod Rheumatol. 2020;30:1–6. doi: 10.1080/14397595.2019.1660028. https://doi.org/10.1080/14397595.2019.1660028. [DOI] [PubMed] [Google Scholar]
- 13.da Silva E, Doran MF, Crowson CS, O'Fallon WM, Matteson EL. Declining use of orthopedic surgery in patients with rheumatoid arthritis? Results of a long-term, population-based assessment. Arthritis Rheum. 2003;49:216–20. doi: 10.1002/art.10998. https://doi.org/10.1002/art.10998. [DOI] [PubMed] [Google Scholar]
- 14.Momohara S, Inoue E, Ikari K, et al. Recent trends in orthopedic surgery aiming to improve quality of life for those with rheumatoid arthritis: data from a large observational cohort. J Rheumatol. 2014;41:862–6. doi: 10.3899/jrheum.131018. https://doi.org/10.3899/jrheum.131018. [DOI] [PubMed] [Google Scholar]
- 15.Jämsen E, Virta LJ, Hakala M, Kauppi MJ, Malmivaara A, Lehto MU. The decline in joint replacement surgery in rheumatoid arthritis is associated with a concomitant increase in the intensity of anti-rheumatic therapy: a nationwide register-based study from 1995 through 2010. Acta Orthop. 2013;84:331–7. doi: 10.3109/17453674.2013.810519. https://doi.org/10.3109/17453674.2013.810519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matsumoto T, Nishino J, Izawa N, et al. Trends in treatment, outcomes, and incidence of orthopedic surgery in patients with rheumatoid arthritis: an observational cohort study using the Japanese national database of rheumatic diseases. J Rheumatol. 2017;44:1575–82. doi: 10.3899/jrheum.170046. https://doi.org/10.3899/jrheum.170046. [DOI] [PubMed] [Google Scholar]
- 17.Nikiphorou E, Carpenter L, Morris S, et al. Hand and foot surgery rates in rheumatoid arthritis have declined from 1986 to 2011, but large-joint replacement rates remain unchanged: results from two UK inception cohorts. Arthritis Rheumatol. 2014;66:1081–9. doi: 10.1002/art.38344. https://doi.org/10.1002/art.38344. [DOI] [PubMed] [Google Scholar]
- 18.Goodman SM, Springer BD, Chen AF, et al. 2022 American College of Rheumatology/American Association of Hip and Knee Surgeons guideline for the perioperative management of antirheumatic medication in patients with rheumatic diseases undergoing elective total hip or total knee arthroplasty. Arthritis Rheumatol. 2022;74:1464–73. doi: 10.1002/art.42140. https://doi.org/10.1002/art.42140. [DOI] [PubMed] [Google Scholar]
- 19.Zhou VY, Lacaille D, Lu N, et al. Has the incidence of total joint arthroplasty in rheumatoid arthritis decreased in the era of biologics use? A population-based cohort study. Rheumatology (Oxford) 2022;61:1819–30. doi: 10.1093/rheumatology/keab643. https://doi.org/10.1093/rheumatology/keab643. [DOI] [PubMed] [Google Scholar]
- 20.Matsushita I, Motomura H, Seki E, Kimura T. Radiographic changes and factors associated with subsequent progression of damage in weight-bearing joints of patients with rheumatoid arthritis under TNF-blocking therapies-three-year observational study. Mod Rheumatol. 2017;27:570–5. doi: 10.1080/14397595.2016.1227235. https://doi.org/10.1080/14397595.2016.1227235. [DOI] [PubMed] [Google Scholar]
- 21.Nystad TW, Fenstad AM, Furnes O, Havelin LI, Skredderstuen AK, Fevang BT. Reduction in orthopaedic surgery in patients with rheumatoid arthritis: a Norwegian register-based study. Scand J Rheumatol. 2016;45:1–7. doi: 10.3109/03009742.2015.1050451. https://doi.org/10.3109/03009742.2015.1050451. [DOI] [PubMed] [Google Scholar]
- 22.Tsushima H, Takahide S, Akasaki Y, et al. Is there a reduction in hip destruction under a treat-to-target strategy in patients with rheumatoid arthritis? Mod Rheumatol. doi: 10.1093/mr/road021. Published online February 14, 2023; https://doi.org/10.1093/mr/road021 . [DOI] [PubMed] [Google Scholar]
- 23.Takeda R, Matsumoto T, Maenohara Y, et al. Increasing trend of radiographic features of knee osteoarthritis in rheumatoid arthritis patients before total knee arthroplasty. Sci Rep. 2022;12:10452. doi: 10.1038/s41598-022-14440-2. https://doi.org/10.1038/s41598-022-14440-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nejima S, Fujimaki H, Kumagai K, et al. Deformity analysis of the lower limb on the coronal plane in patients with rheumatoid arthritis and osteoarthritis. Mod Rheumatol. 2022;32:741–5. doi: 10.1093/mr/roab046. https://doi.org/10.1093/mr/roab046. [DOI] [PubMed] [Google Scholar]
- 25.Jensen R, Christensen AF, Hartlev LB, et al. Calcified cartilage differs in patients with end-stage primary osteoarthritis and secondary osteoarthritis due to rheumatoid arthritis of the hip joint. Scand J Rheumatol. 2022;51:441–51. doi: 10.1080/03009742.2021.1952754. https://doi.org/10.1080/03009742.2021.1952754. [DOI] [PubMed] [Google Scholar]
- 26.Taylor-Williams O, Nossent J, Inderjeeth CA. Incidence and complication rates for total hip arthroplasty in rheumatoid arthritis: a systematic review and meta-analysis across four decades. Rheumatol Ther. 2020;7:685–702. doi: 10.1007/s40744-020-00238-z. https://doi.org/10.1007/s40744-020-00238-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sasaki K, Momma R, Takakubo Y, et al. The influence of cement stem concept on the incidence and treatment of periprosthetic fracture. Rinsyoseikei. 2020;55:1015–20. Japanese. [Google Scholar]
- 28.Kaneuji A, Chen M, Takahashi E, et al. Collarless polished tapered stems of identical shape provide differing outcomes for stainless steel and cobalt chrome: a biomechanical study. J Funct Biomater. 2023;14:262. doi: 10.3390/jfb14050262. https://doi.org/10.3390/jfb14050262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carli AV, Negus JJ, Haddad FS. Periprosthetic femoral fractures and trying to avoid them: what is the contribution of femoral component design to the increased risk of periprosthetic femoral fracture? Bone Joint J. 2017;99-B(1 Supple A):50–9. doi: 10.1302/0301-620X.99B1.BJJ-2016-0220.R1. https://doi.org/10.1302/0301-620X.99B1.BJJ-2016-0220.R1. [DOI] [PubMed] [Google Scholar]
- 30.Naganuma Y, Takakubo Y, Hirayama T, et al. Lipoteichoic acid modulates inflammatory response in macrophages after phagocytosis of titanium particles through Toll-like receptor 2 cascade and inflammasomes. J Biomed Mater Res A. 2016;104:435–44. doi: 10.1002/jbm.a.35581. https://doi.org/10.1002/jbm.a.35581. [DOI] [PubMed] [Google Scholar]
- 31.Leta TH, Fenstad AM, Lygre SHL, et al. The use of antibiotic-loaded bone cement and systemic antibiotic prophylactic use in 2,971,357 primary total knee arthroplasties from 2010 to 2020: an international register-based observational study among countries in Africa, Europe, North America, and Oceania. Acta Orthop. 2023;94:416–25. doi: 10.2340/17453674.2023.17737. https://doi.org/10.2340/17453674.2023.17737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hirayama T, Tamaki Y, Takakubo Y, et al. Toll-like receptors and their adaptors are regulated in macrophages after phagocytosis of lipopolysaccharide-coated titanium particles. J Orthop Res. 2011;29:984–92. doi: 10.1002/jor.21369. https://doi.org/10.1002/jor.21369. [DOI] [PubMed] [Google Scholar]
- 33.Safiri S, Kolahi AA, Hoy D, et al. Global, regional and national burden of rheumatoid arthritis 1990-2017: a systematic analysis of the Global Burden of Disease study 2017. Ann Rheum Dis. 2019;78:1463–71. doi: 10.1136/annrheumdis-2019-215920. https://doi.org/10.1136/annrheumdis-2019-215920. [DOI] [PubMed] [Google Scholar]
- 34.Nakajima A, Sakai R, Inoue E, Harigai M. Prevalence of patients with rheumatoid arthritis and age-stratified trends in clinical characteristics and treatment, based on the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Int J Rheum Dis. 2020;23:1676–84. doi: 10.1111/1756-185X.13974. https://doi.org/10.1111/1756-185X.13974. [DOI] [PubMed] [Google Scholar]
- 35.Furuya T, Inoue E, Hosoi T, Taniguchi A, Momohara S, Yamanaka H. Risk factors associated with the occurrence of hip fracture in Japanese patients with rheumatoid arthritis: a prospective observational cohort study. Osteoporos Int. 2013;24:1257–65. doi: 10.1007/s00198-012-2080-0. https://doi.org/10.1007/s00198-012-2080-0. [DOI] [PubMed] [Google Scholar]
- 36.van Staa TP, Geusens P, Bijlsma JW, Leufkens HG, Cooper C. Clinical assessment of the long-term risk of fracture in patients with rheumatoid arthritis. Arthritis Rheum. 2006;54:3104–12. doi: 10.1002/art.22117. https://doi.org/10.1002/art.22117. [DOI] [PubMed] [Google Scholar]
- 37.Ravi B, Croxford R, Austin PC, et al. Increased surgeon experience with rheumatoid arthritis reduces the risk of complications following total joint arthroplasty. Arthritis Rheumatol. 2014;66:488–96. doi: 10.1002/art.38205. https://doi.org/10.1002/art.38205. [DOI] [PubMed] [Google Scholar]