Abstract
Background and Purpose
High quality clinical documentation is a fundamental skill for practicing physicians and important for quality improvement. However, documentation and coding are rarely integrated into medical education curricula and there is a lack of standard neurology curriculum on this topic. We developed and evaluated a teaching session on clinical documentation for neurology resident physicians.
Methods
The education consisted of a didactic session designed by a neurologist with content about risk-adjusted mortality, clinical documentation integrity (CDI), impact of documentation on patients, and neurology-specific documentation guidance. A pre-post survey design was used to compare baseline and post-intervention self-reported knowledge and attitudes.
Results
61 responses were collected (37 pre- and 24 post-intervention). Residents had increased understanding of the impact of documentation on quality metrics (P = 0.004), risk-adjusted mortality (P < 0.0001), and impact on patients (P = 0.02). Attitude towards CDI education improved significantly (P = 0.0016), as well as agreement that CDI is important to resident physicians (P = 0.003). The portion of residents who agreed training on CDI is useful and valuable increased significantly (P = 0.004). 92% agreed this curriculum was useful, and 96% agreed they understood the role of CDI better after the session.
Conclusions
In this study of a teaching session for neurology residents on clinical documentation, we found this format of teaching was well-received and highly effective in improving resident attitudes and self-reported knowledge.
Keywords: general neurology, clinical specialty, outcomes, techniques, quality, techniques, neurohospitalist, clinical specialty
Introduction
Accurate clinical documentation impacts patient care, affects reimbursement, and influences quality metrics. As value-based care becomes more standard, there is increasing focus on the quality and completeness of physician documentation to include specific diagnoses, comorbidities, and complications. Although documentation has been traditionally linked with payor reimbursement, it has substantial impact on evaluating care quality and patient outcomes. 1 Metrics such as the mortality index or length of stay index rely on accurate clinical documentation. Mortality index is a computed ratio of observed to expected mortality. Observed mortality reflects how many deaths occurred, whereas expected mortality is calculated via risk-adjustment methods from diagnoses and comorbidities captured from physician clinical documentation. Incomplete documentation yields falsely low expected mortality, leading to a higher service-line mortality index than is truly reflective of the quality of care provided. Thus, physician documentation has substantial impact on quality metrics and hospital specialty-specific rankings.
Accurate coding is an important function of neurologic practice 2 but many resident physicians do not have formal training in documentation, coding, or quality metrics. 3 There is a gap between the documentation language used in clinical practice and International Classification of Diseases-10th revision (ICD-10) codes, which is the language used by coders. To bridge this gap, many hospitals have implemented clinical documentation integrity (CDI) specialists to ensure patient complexity is accurately captured in physician notes. CDI specialists have a clinical nursing background and review documentation in real-time for accuracy, errors, missing diagnoses, and proper terminology. They commonly send queries to the clinical team, including to resident physicians, to clarify or include a diagnosis that is clinically supported by chart review but has not been properly documented. In addition, there are diagnoses and comorbidities specific to neuroscience that heavily impact expected mortality, for example, “cerebral edema” and “brain compression”. Medical coders are not permitted to assume a diagnosis without clear documentation. For example, “midline shift” cannot be translated to “brain compression” in coding without corresponding physician documentation. Neuroscience-trained CDI specialists will query to clarify documentation for these and other high-complexity diagnoses when they have not been captured by the clinical team.
Physicians may view accurate documentation as an additional administrative burden or overly complex. 4 However, they must stay up to date with evolving documentation and coding guidelines. Learning systems-based practices, effective exchange of information, and maintenance of medical records are domains of the ACGME core competencies, thus the topic must be integrated into residency training. The guidelines and framework used by CDI specialists and coding are often not familiar to clinicians which may result in frustration and a lack of teamwork with CDI specialists. 5 With expanding patient volume, higher complexity of care, and increasing features in the electronic medical record, any perception of extra time spent documenting may hinder a positive working relationship with the CDI team. 5 In addition, there are misunderstandings that clinical documentation integrity serves a primarily financial purpose without any impact on patient care or ability to evaluate the quality of patient care delivered.
Problem Statement
There is no published formal curriculum for neurology residents about CDI, risk-adjusted mortality and metrics, or the impact of documentation on quality metrics. Common formats for delivering CDI education include standardized web-based modules or large-group webinars as part of onboarding. However, we hypothesized that an effective education curriculum would be delivered by a physician in the same specialty and would focus on patient outcomes and neurology specific diagnoses rather than primarily on billing, financial implications, or reimbursement. We created a physician-led neurology-specific education session on CDI for neurology residents, hypothesizing it would improve knowledge and attitudes about CDI.
Methods
Curriculum Design
The educational session was developed by a neurologist with the following learning objectives:
1) Describe how risk-adjusted mortality is derived using neurology-specific case examples.
2) Identify how physician clinical documentation impacts mortality index and quality metrics.
3) Understand the role of CDI specialists.
4) Outline high-yield neurology documentation tips.
5) Analyze impact of documentation on hospital financial survival via case-study.
Curriculum Content and Implementation
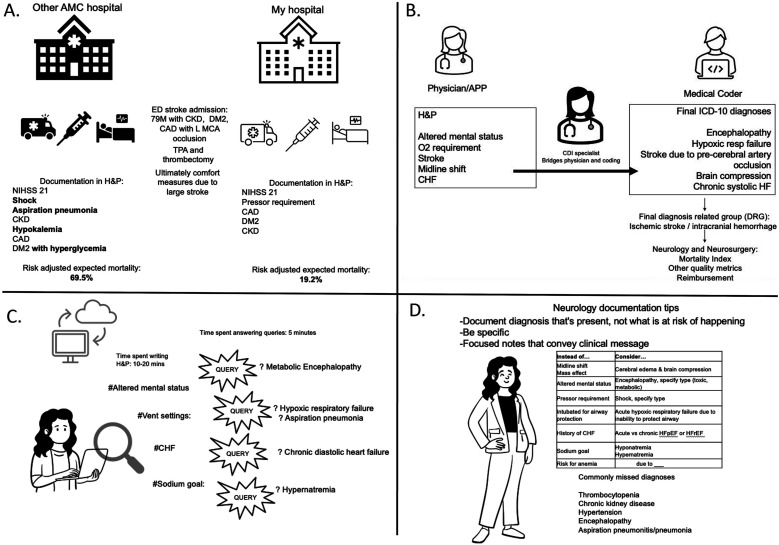
The lecture content was designed in a story-telling format and is divided into five topics: risk-adjusted mortality, clinical documentation integrity, neurology documentation improvement, and impact on patients. Examples of the curriculum material are shown in Figure 1 with additional outline of educational content in supplemental material 1. With the approval of the neurology residency program directors, the education session was held over one hour as part of a residency-wide didactic lecture.
Figure 1.
Examples of curriculum content (A) Impact of documentation on risk-adjusted expected mortality. (B) Introducing CDI specialist and coding, diagnosis related groups (DRGs). (C) Examples of documentation clarification. (D) Neurology documentation tip chart.
Participants
Neurology residents and residents from other specialties (e.g., psychiatry) rotating on the inpatient neurology service in PGY-1 to PGY-4 years of training were included.
Outcomes Assessments
Neurology residents were asked to complete an anonymous survey prior to the education session (intervention) to assess their attitude towards CDI via five questions using a 5-point Likert scale (1-strongly disagree, 2-disagree, 3-neutral, 4-agree, 5-strongly agree) and knowledge of certain topics via six questions using categorical responses (1-disagree, 2-unsure, 3-agree). Using the Kirkpatrick model of learning evaluation, 6 we evaluated the intervention’s impact on resident attitude (Kirkpatrick Level 1, reaction) and knowledge (Kirkpatrick Level 2, learning). Survey responses were collected in REDCap, a secure data collection application.
Statistical Analysis
Descriptive statistics were calculated for survey responses. As survey data was anonymous, responses were not matched and thus were unpaired in analysis. Pre- and post-responses were analyzed via Mann Whitney test (for analysis of significance between ordinal ranks) comparing median responses and distribution of ranks where appropriate. Statistical significance was reported at a P value of 0.05. Mann Whitney U value is reported as well. Analyses were performed in GraphPad Prism (Version 10.0.0).
Standard Protocols, Informed Consent, and Data Availability
The study was approved under exempt status by the Mass General Brigham Institutional Review Board and granted waiver of signed informed consent (IRB protocol 2023P001786).
Results
Demographic and Baseline Data
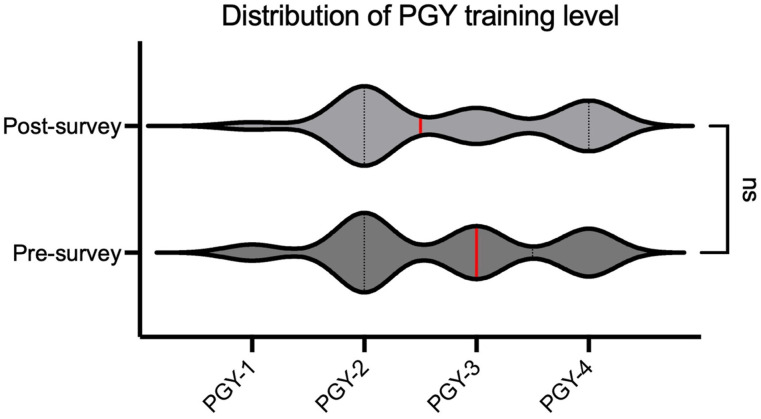
A total of 61 survey responses were collected (37 pre-intervention, 24 post-intervention). Post-graduate year (PGY) training level distribution was evenly matched between pre- and post-respondents (Figure 2, U = 428.5, P = 0.83) with total distribution PGY-1 (6.5%, n = 4), PGY-2 (43%, n = 26), PGY-3 (25%, n = 15), and PGY-4 (26%, n = 16). All respondents were neurology residents except four psychiatry residents (PGY-1) rotating on the neurology inpatient service. Most of the participants (86%, n = 32) responded in the pre-intervention survey that they had not received or were unsure if they ever had previous training about CDI.
Figure 2.
PGY-training distribution. Distribution of PGY-training level does not differ significantly between groups. (Mdnpre = 3.0, Mdnpost = 2.5, P = 0.83, U = 428.5) Pre-intervention n = 37 and post-intervention n = 24.
Knowledge Data
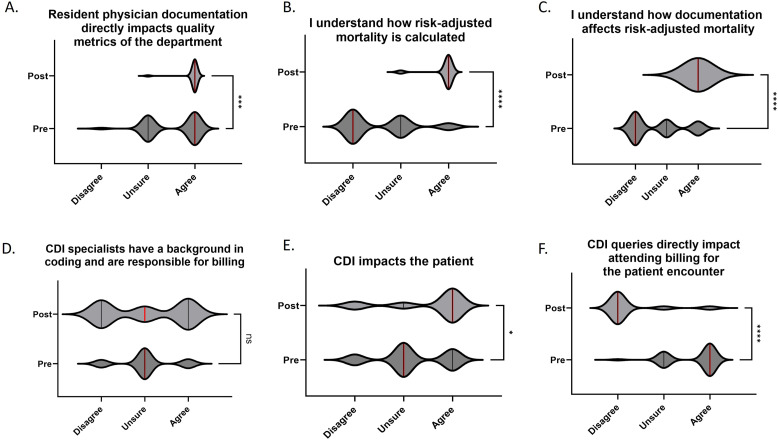
The portion of residents who agreed that resident physician documentation has a direct impact on neurology department quality metrics increased from 54% to 96% with a significant positive shift in agreement (Figure 3A, U = 258, P = 0.004).
Figure 3.
Survey results in knowledge domains. Median values (red line) represent data from a 3-point Likert scale (Disagree = 1, Unsure = 2, Agree = 3). Pre-intervention n = 37 and post-intervention n = 24. (A) Significant increase in agreement that resident documentation impacts quality metrics, Mdnpre = 3.0, Mdnpost = 3.0, U = 258, P = 0.004. (B) Significant increase in agreement of understanding how risk-adjusted mortality is calculated, Mdnpre = 1.0, Mdnpost = 3.0, U = 65, P < 0.0001. (C) Significant increase in understanding how documentation affects risk-adjusted mortality, Mdnpre = 1.0, Mdnpost = 3.0, U = 96, P < 0.0001. (D) No change in belief that CDI specialists have a background in coding and are responsible for billing, Mdnpre = 2.0, Mdnpost = 2.0, U = 436, P = 0.86. (E) Increase in agreement that CDI impacts the patient, Mdnpre = 2.0, Mdnpost = 3.0, U = 302.5, P = 0.0220. (F) Significant decrease in belief that CDI queries directly impact attending billing for the encounter, Mdnpre = 3.0, Mdnpost = 1.0, U = 74, P < 0.0001.
At baseline, only 15% of residents responded they understood how risk-adjusted mortality is calculated which increased to 92% after the intervention with a positive shift in agreement (Figure 3B, U = 65, P < 0.0001). Similarly, the portion of residents who self-reported understanding of how documentation affects risk-adjusted mortality increased from 22% to 100% (Figure 3C, U = 96, P < 0.0001).
There was no significant change in the percentage of residents who thought CDI specialists have a coding background and are responsible for billing (Figure 3D, U-435, P = 0.86). There was a significant increase in agreement that CDI impacts the patient (Figure 3E, U = 302.5, P = 0.0220). The portion who agreed CDI queries directly impact attending physician billing for the encounter decreased from 65% to 8% (Figure 3F, U = 74, P < 0.0001).
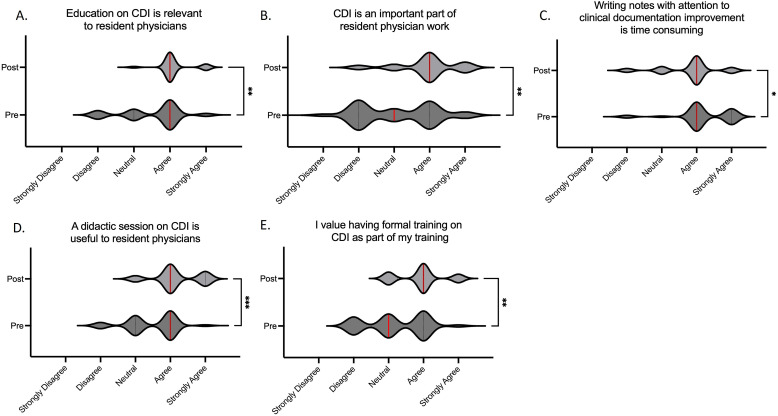
Attitudes Data
The portion of residents who agreed or strongly agreed that education on CDI is relevant to resident physicians increased from 62% to 96% (Figure 4A, U = 268.5, P = 0.0016). The portion who agreed or strongly agreed that CDI is an important part of resident physician work increased from 43% to 79% (Figure 4B, U = 255.5, P = 0.0027).
Figure 4.
Survey results in attitude domains. Median values (red line) represent data from a 5-point Likert scale (Strongly Disagree = 1, Disagree = 2, Neutral = 3, Agree = 4, Strongly Agree = 5). Pre-intervention n = 37 and post-intervention n = 24. (A) Increase in agreement that education on CDI is relevant to resident physicians, Mdnpre = 4.0, Mdnpost = 4.0, U = 268.5, P = 0.0016. (B) Increase in agreement that CDI is an important part of resident physician work, Mdnpre = 3.0, Mdnpost = 4.0, U = 255.5, P = 0.0027. (C) Decrease in agreement that writing notes with attention to clinical documentation is time consuming, Mdnpre = 4.0, Mdnpost = 4.0, U = 315, P = 0.031. (D) Increase in agreement that a didactic session on CDI is useful to resident physicians, Mdnpre = 4.0, Mdnpost = 4.0, U = 230, P = 0.0004. (E) Increased portion of residents who valued having formal training on CDI, Mdnpre = 3.0, Mdnpost = 4.0, U = 253, P = 0.0021.
At baseline, 92% agreed or strongly agreed that writing notes with attention to clinical documentation improvement is time consuming; after the session this percentage decreased to 75% (Figure 4C, U = 315, P = 0.03).
There was a significant increase from 54% to 86% of residents who agreed or strongly agreed that a didactic session on CDI is useful to residents and trainees (Figure 4D, U = 230, P = 0.0004). Likewise, significantly more residents agreed or strongly agreed that they value having formal training on CDI (43% to 75%, Figure 4E, U = 253, P = 0.002).
Feedback on the format of education was generally positive, as 92% agreed or strongly agreed this curriculum was useful, and 96% agreed or strongly agreed they understood the role of CDI better after the session.
Discussion
We developed education for neurology residents on clinical documentation integrity and found this format of teaching was effective in improving learner attitudes and self-reported knowledge. Although half of the residents were in upper years (PGY-3 or PGY-4) of their training, most (86%) had little previous education on CDI. Among the subgroup of PGY-4 residents, 67% responded they had not received or were unsure if they received prior training on documentation. Residents approaching their final year of neurology residency lack adequate exposure to the key concepts behind clinical documentation, billing, and coding. This finding is consistent with the published literature about the overall lack of education on billing in medical training.3,5,7,8 In a published survey of neurology residents and fellows, 75% responded their medical training did not prepare them to understand the business aspect of clinical practice. 7 The lack of a curriculum transcends specialties; a study of surgical residents found 82% had not received adequate training and 85% felt they were novices at coding and billing. 9
Education in billing and coding benefits neurology trainees and academic departments. 7 In a study of neurology residents, 71% felt that the business of medicine should be a part of the residency curriculum. 7 However, lectures on billing and financial issues are sometimes met with hesitance from trainees who have immediate focus on medical decision making rather than the requirement to bill for care provided. Frustrations with CDI can exist along the process including from queries, mismatch between clinical and coding terminologies, and a lack of understanding of the role of CDI specialists. 5 We sought to promote understanding and a culture of collaboration with CDI specialists. In this session, we outlined the distinction between the billing and coding department and CDI department by emphasizing the role of CDI specialists as part of the clinical team with a patient-centered focus. Attitudes towards CDI improved significantly after the education, with an increase 62% to 96% of residents agreeing education on CDI is relevant to them. 75% of residents valued having formal training in CDI after the study, compared with 43% at baseline. Improvement in attitudes towards CDI were seen in all domains, specifically in its relevance, importance, and value to residents.
One of the common barriers to engaging in CDI from physicians and trainees is the perception that it increases time spent documenting.5,10 In our study, 92% of residents at baseline responded that writing notes with attention to clinical documentation improvement is time consuming. After the session, there were significantly fewer residents who felt this way (75%), though we note this is still the majority, suggesting a need for strategies to streamline quality documentation. Certainly, residents’ primary focus is on patient care. Although billing is a required part of physician practice, the curriculum focused on patient and quality-outcomes, including the importance of documentation in preventing insurance denial and financial survival to continue to provide high-quality care. Residents held a misconception that answering CDI queries financially impacts the billing provider directly, which was dispelled by education on how documentation affects the department quality metrics and financial reimbursement. We found only 67% of residents at baseline agreed that CDI impacts the patient, which increased to 81% after the intervention. 11
The mortality index, which reflects the ratio of observed to expected mortalities in the inpatient setting, is widely utilized to assess the quality of care delivered to inpatients with neurologic disease. However, its utility and accuracy is greatly impacted by the specific documentation that underlies the calculation of expected mortality. One focus of the study was education surrounding quality metrics including the mortality index. Most residents did not know how risk-adjusted mortality is calculated or how documentation affects risk-adjusted mortality. The session was highly successful in improving understanding of these important topics. When coding and documentation is taught in residency education, the focus is often largely on reimbursement. 3 It is paramount that residents recognize the impact their documentation has on inpatient mortality index and how documentation directly influences a reflection of the quality of patient care delivered rather than reimbursement alone. If physicians realize the impact their documentation has on quality metrics reflective of the care they provide, they may be more likely to engage in documentation improvement efforts.
Limitations
The limitations of this study include its single-center design in a small sample size. In addition, the intervention represents a single time point, thus ongoing study is required to prove sustainability of the effect. We recognize that continued medical education on this topic is key, as a single session is unlikely to suffice full adaptation of the skills and material. The group of residents who responded to the pre-survey was not individually matched to the post-survey cohort, but we felt this was necessary to protect anonymity. A minority of the residents surveyed were from a different specialty (eg, psychiatry), and some residents had prior CDI training which may confound the results. Another limitation of our paper is that the knowledge domains were self-reported, which is a limitation of this type of study; further research to measure changes in resident documentation practices before and after intervention would solidify the primary results.
Future Directions
Incorporating documentation curricula into medical education will benefit trainees during residency and result in an easier transition into independent practice. 7 The optimum form of delivering this education to residents is not well established, but likely would consist of in-person seminars, 3 CDI specialist presence on rounds, 5 skills sessions, and documentation resources such as documentation cards 12 provided in a longitudinal fashion rather than at a single time point. We emphasize the importance of specialty-specific documentation training rather than generic online delivery of the material. Replication and modification of this teaching could easily be adapted within other programs and is a low-cost intervention. Based on the results of this study, future research would aim to assess the impact of this curriculum on neurology resident documentation behaviors and directly measure outcomes such as increased comorbidity capture, decreased CDI queries, or improved mortality and length-of-stay indices.
Conclusions
A curriculum on documentation developed for neurology residents resulted in improved self-reported knowledge and attitudes towards clinical documentation. This topic is of increasing importance, with rising emphasis on documentation and quality measures. Formal curriculum on this topic should be integrated into neurology residency and inpatient fellowship programs. 13
Supplemental Material
Supplemental Material for Curriculum Innovation: Clinical Documentation Improvement Education for Neurology Trainees by Yasmin Aghajan, and Bradley J. Molyneaux in The Neurohospitalist.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Yasmin Aghajan https://orcid.org/0000-0003-3608-3568
Bradley J. Molyneaux https://orcid.org/0000-0002-3377-1229
References
- 1.Aiello FA, Judelson DR, Durgin JM, et al. A physician-led initiative to improve clinical documentation results in improved health care documentation, case mix index, and increased contribution margin. J Vasc Surg. 2018;68(5):1524-1532. [DOI] [PubMed] [Google Scholar]
- 2.Powers LB. Coding issues in critical care patients with an emphasis on encephalopathy. Continuum. 2012;18(3):669-677. doi: 10.1212/01.CON.0000415435.73845.9b [DOI] [PubMed] [Google Scholar]
- 3.Gay LJ, Lin D, Colah Z, Raynaldo G. Inpatient coding system and opportunities for documentation optimization: an interactive session for internal medicine residents. MedEdPORTAL. 2022;18:11219. doi: 10.15766/mep_2374-8265.11219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zalatimo O, Ranasinghe M, Harbaugh RE, Iantosca M. Impact of improved documentation on an academic neurosurgical practice. J Neurosurg. 2014;120(3):756-763. [DOI] [PubMed] [Google Scholar]
- 5.Rouse M, Jones M, Zogleman B, May R, Ekilah T, Gibson C. Resident integration with inpatient clinical documentation improvement: a quality improvement project. BMJ Open Qual. 2022;11(2):e001300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirkpatrick JD, Kirkpatrick WK. Kirkpatrick’s Four Levels of Training Evaluation. Alexandria: ATD Press; 2016. [Google Scholar]
- 7.Waugh JL. Education in medical billing benefits both neurology trainees and academic departments. Neurology. 2014;83(20):1856-1861. [DOI] [PubMed] [Google Scholar]
- 8.Varacallo MA, Wolf M, Herman MJ. Improving orthopedic resident knowledge of documentation, coding, and Medicare fraud. J Surg Educ. 2017;74(5):794-798. doi: 10.1016/j.jsurg.2017.02.003 [DOI] [PubMed] [Google Scholar]
- 9.Fakhry SM, Robinson L, Hendershot K, Reines HD. Surgical residents’ knowledge of documentation and coding for professional services: an opportunity for a focused educational offering. Am J Surg. 2007;194(2):263-267. doi: 10.1016/j.amjsurg.2006.11.031 [DOI] [PubMed] [Google Scholar]
- 10.Christino MA, Matson AP, Fischer SA, Reinert SE, Digiovanni CW, Fadale PD. Paperwork versus patient care: a nationwide survey of residents’ perceptions of clinical documentation requirements and patient care. J Grad Med Educ. 2013;5:600-604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Villanueva R, Busis NA, Cohen BH, Ciccarelli L. The transformation of documenting and coding for neurologic hospital inpatient and observation services. Continuum. 2023;29(2):628-640. doi: 10.1212/CON.0000000000001301 [DOI] [PubMed] [Google Scholar]
- 12.Spellberg B, Harrington D, Black S, Sue D, Stringer W, Witt M. Capturing the diagnosis: an internal medicine education program to improve documentation. Am J Med. 2013;126(8):739-743. doi: 10.1016/j.amjmed.2012.11.035 [DOI] [PubMed] [Google Scholar]
- 13.Dawson B, Carter K, Brewer K, et al. Chart smart: a need for documentation and billing education among emergency medicine residents. West J Emerg Med. 2010;11:116-119. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Curriculum Innovation: Clinical Documentation Improvement Education for Neurology Trainees by Yasmin Aghajan, and Bradley J. Molyneaux in The Neurohospitalist.