Abstract
Background
Dissecting intracranial aneurysms (DIAs) have been treated through endovascular reconstructive manners, such as flow diverters (FDs) and stent-assisted coiling (SAC). Notably, no robust evidence has compared both approaches. Hence, the authors conducted a meta-analysis to compare their outcomes.
Methods
PubMed, Embase and Web of Science were searched for studies employing SAC and FD treatment for DIAs. The following outcomes were considered for extraction: procedure-related mortality, total mortality, postoperative and follow-up complete aneurysm occlusion, complications, good clinical outcomes, recurrence, and retreatment. Odds ratio (OR) with random effects was employed for statistical comparison.
Results
The meta-analysis included 10 studies. A total of 195 and 222 patients were included in the FD and the SAC group, respectively. Stent-assisted coiling had higher postoperative complete aneurysm occlusion rates (OR 0.03; 95% CI 0.01–0.08). Flow diverter retreatment rate was lower, but without statistical significance (OR 0.35; 95% CI 0.11–1.10). No significant differences were found in follow-up complete aneurysm occlusion (OR 1.18; 95% CI 0.35–3.99); total mortality (OR 0.44; 95% CI 0.09–2.08); intraoperative complications (OR 0.30; 95% CI 0.06–1.45); postoperative complication (OR 0.77; 95% CI 0.35–1.70); good clinical outcomes (OR 0.97; 95% CI 0.43–2.20); and recurrence (OR 0.38; 95% CI 0.13–1.10) between the two groups.
Conclusion
Stent-assisted coiling shows higher postoperative complete aneurysmal occlusion rates, but both techniques achieve similar rates in angiographic follow-up. Flow diverter has lower, but not statistically significant, retreatment rates than SAC. Both techniques have similar complication rates. Future randomized, multicenter, and prospective studies with larger sample sizes are needed for more conclusive findings.
Keywords: Stent-assisted coiling, coil, flow diverter, dissecting, aneurysm, systematic review, meta-analysis
Introduction
Dissecting intracranial aneurysms (DIAs) are a rare subtype of aneurysms that occur when the continuity of the intima layer of an artery breaches leading to the formation of a false lumen, and the development of an intramural hematoma and aneurysm. 1 The primary location for DIAs is the vertebrobasilar system, which can result in significant morbidity and mortality upon aneurysm growth, rupture, or artery thrombosis.1–3 Presentation can include asymptomatic patients, brainstem compression syndrome, and severe subarachnoid hemorrhage. 1 Epidemiologically, DIAs are reported more frequently in young Asian populations. 4
Endovascular therapies have become preferred over open surgery given the elevated morbidity and mortality related to surgical treatment; moreover, reconstructive techniques could be done in a less invasive way.2–5 These therapies encompass a range of options, including stent-assisted coiling (SAC), flow diverter (FD), sole stenting, coiling, and parent vessel occlusion.3–6 Stent-assisted coiling has been utilized for the last two decades, proving to be an effective and safe therapy. 5 Notably, the landscape is evolving with the experience acquired with FD for other indications.
A recent meta-analysis has demonstrated the safety and efficacy of FDs in treating DIAs. 7 Flow diverters are gaining prominence in neurovascular surgery as the go-to devices, ushering in what some call the “FD era.”8,9 Despite the demonstrated feasibility of FDs in DIAs,6,7 no comparative systematic analysis has been conducted to establish the superiority of one therapy over the other. We aim to review the outcomes of DIA treatment and compare the two endovascular treatment cohorts SAC and FD therapies.
Methods
This systematic review and meta-analysis adhered to the guidelines set by the Cochrane Handbook and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement.10,11 A prospective registration was not performed.
Search strategy
PubMed, Embase, and Web of Science databases were systematically searched from inception to January 2024 with the following search strategy: “(dissecting OR dissection) AND aneurysm AND (intracranial OR cerebral) NOT (aorta OR aortic).” The authors searched broadly to ensure complete coverage of the DIA literature.
Selection process and eligibility criteria
Two authors independently undertook the selection of studies (C.S. and M.Z.P.). In cases of disagreement, senior investigators were consulted. Full-text analysis was performed in all studies of endovascular treatment of DIAs. After segregating the therapies employed for each study, the following eligibility criteria were applied: (1) retrospective and prospective consecutive cohorts or randomized clinical trials evaluating patients submitted to FD or SAC in the same study; (2) reporting on at least one outcome related to both procedures in different populations, and (3) published from the year 2000 onwards. Conference abstracts were excluded. Only studies involving consecutive patients with a clear inclusion process were considered to diminish the selection bias of small sample sizes. Studies encompassing only one patient for any treatment group were excluded.
Outcomes assessed
Outcomes included procedure-related mortality, total mortality, postoperative and follow-up complete aneurysm occlusion, complications (total, ischemic, hemorrhagic), good clinical outcomes, recurrence, and retreatment.
Data extraction
The data extraction process aimed to organize information for each treatment method into online spreadsheets. Three authors participated in this process, which covered various dimensions, including publication details (first author, publication year, study design, country), and baseline patient characteristics (number of patients, number of aneurysms, ruptured aneurysms, aneurysm location, patient age, gender, and follow-up duration).
Clinical outcomes were extracted based on the modified Rankin Scale (mRS) and the Glasgow Outcome Scale (GOS). Favorable outcomes were defined as an mRS score between 0 and 2 or a GOS of 4 or 5. Complications, which included adverse events during or after surgery related to the procedure, encompassed ischemia, hemorrhage, infections, and others. The term “postprocedure” was applicable if confirmed until discharge or explicitly stated by the author.
Complete occlusion was considered as Raymond–Roy grading scale class I or when the study stated it as “complete occlusion.” Recurrence was considered as aneurysm regrowth or aneurysm recanalization. Retreatment was considered when the authors explained the patient needed to undergo a second procedure due to an unsuccessful first approach or complications, such as rebleeding or recanalization.
Methodological assessment
The included studies were submitted to evaluate their methodological quality through the ROBINS I tool by two authors (S.B. and L.O.B). The purpose was to determine the overall quality of the literature through the analysis of individual studies. This tool is segmented into seven domains of biases: confounding, selection of participants, classification of interventions, deviations of intended intervention, missing data, measurement of outcomes, and selection of the reported result. 12
Statistical analysis
Review Manager (version 5.4.1) was utilized to analyze outcomes associated with both techniques. Treatment effects were compared using Odds ratio (OR) with 95% confidence intervals, employing a random-effect model. Heterogeneity was assessed using I² statistics.
Results
Study selection and baseline characteristics of the included studies
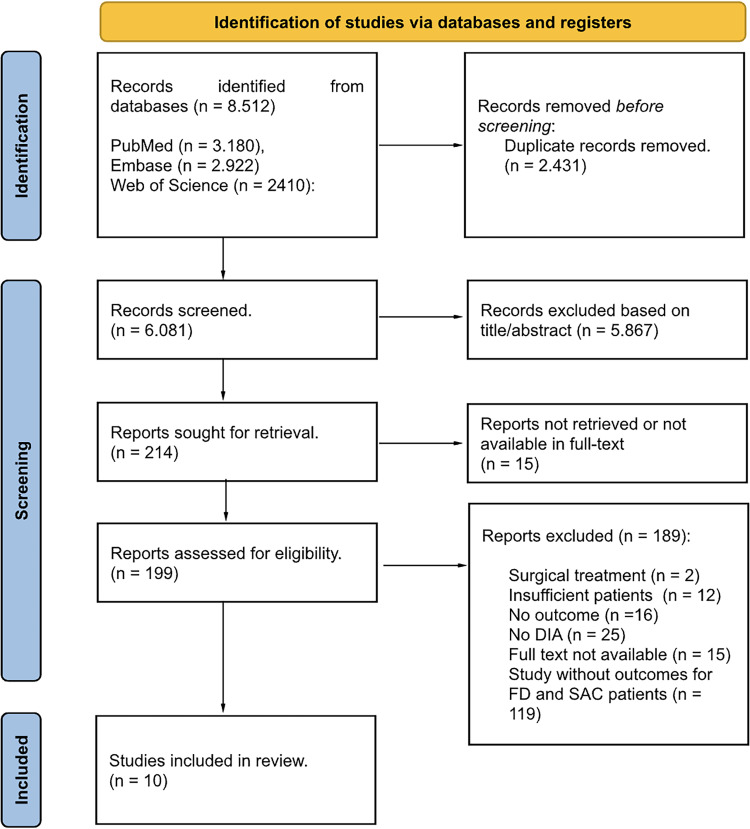
We identified 8512 articles in the initial search. Of those, 6081 were fully reviewed based on inclusion criteria, and 10 studies were included in the final analysis (Figure 1).3,5,13–20 The included studies were conducted in the United States, South Korea, Germany, China, and Thailand between 2010 and 2023. Importantly, four studies were Chinese. All articles evaluated had a retrospective methodological design. The studies comprised 195 patients for the FD group and 222 for the SAC group. The mean age of participants ranged from 31 to 58 years. In the FD group, 29.9% of patients with available data on sex were female, whereas, in the SAC group, the corresponding percentage was slightly higher at 34.9%.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flow diagram.
Only one patient had an aneurysm in the anterior circulation (internal carotid artery). All other aneurysms included were in the vertebrobasilar system. Five studies analyzed only unruptured aneurysms, while two analyzed only ruptured. Three studies had both ruptured and unruptured aneurysms. A total of 28/202 (13.8%) aneurysms were ruptured in the FD group, while 21/230 (9.1%) were in the SAC. Other characteristics of the included studies are shown in Table 1.
Table 1.
Baseline characteristics of the included studies (FD/SAC).
| Study (year) | Country | Enrollment Period | n Patients | n Aneurysms | R | Mean age (SD) [range] | F | VA | BA | VBA | VA-PICA | PCA | ICA | Follow-up time (SD) [range] mo |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catapano et al. (2021) 13 | USA | January 1, 1999– December 31, 2019 | 29/15 | 29/15 | 7/8 | NA | NA | 24/13 | 0 | 1/2 | 4/0 | 0 | 0 | NA |
| Cho et al. (2019) 14 | South Korea | January 2009–December 2017 | 7/9 | 7/9 | 0/0 | 47.6 (22.1) / 54.3 (14.7) | 5/6 | 5/9 | 2/0 | 0 | 0 | 0 | 0 | 16.3 (13.1) / 27 (23.4) |
| Kaschner et al. (2019) 15 | Germany | January 2004–July 2018 | 8/4 | 9/4 | 7/4 | 46.625 / 48.25 | 2/1 | 5/4 | 1/0 | 1/0 | 0 | 1/0 | 1/0 | 9.66 / 2.98 |
| Li et al. (2020) 16 | China | January 2010–September 2018 | 4/10 | 4/10 | 0/0 | 31.5 / 54.1 | 2/0 | 3/10 | 0 | 1/0 | 0 | 0 | 0 | 12.5 / 14.5 |
| Schob et al. (2019) 17 | Germany | January 2010–May 2018 | 3/4 | 3/4 | 3/4 | 59.33 / 58.25 | 3/2 | 3/4 | 0 | 0 | 0 | 0 | 0 | 4 / 17.75 |
| Zhang et al. (2020) 18 | China | January 2009–December 2018 | 8/15 | 12/21 | 0/2 | NA | NA | 2/17 | 0 | 0 | 10/4 | 0 | 0 | 6.375 / 13 |
| Duangprasert et al. (2023) 19 | Thailand | March 2015–May 2022 | 11/3 | 11/3 | 11/3 | NA | NA | 9/3 | 0 | 0 | 2/0 | 0 | 0 | NA |
| Han et al. (2023) 5 | China | January 2016–December 2020 | 65/59 | 65/59 | 0/0 | 53 [47–58] / 53 [48–61] | 11/11 | 49/46 | 0 | 2/3 | 14/10 | 0 | 0 | 11 [6–28] / 10 [6–30] |
| Oh et al. (2023) 3 | Korea | April 2009–September 2021 | 24/48 | 24/48 | 0/0 | 54.7 (10.9) / 57.6 (10.7) | 12/28 | 17/41 | 0 | 0 | 7/7 | 0 | 0 | 13.5 [6–60] / 32.13 [6–120] |
| Wu et al. (2023) 20 | China | January 2014–March 2022 | 36/55 | 38/57 | 0/0 | 55.1 (8.9) / 58.3 (9.6) | 9/18 | 24/46 | 0 | 14/11 | 0 | 0 | 0 | 7 [6–10] / 9 [6–14] |
NA: not available; SD: standard deviation; n: number; F: female; R: ruptured; Ret: retrospective; mo: months.
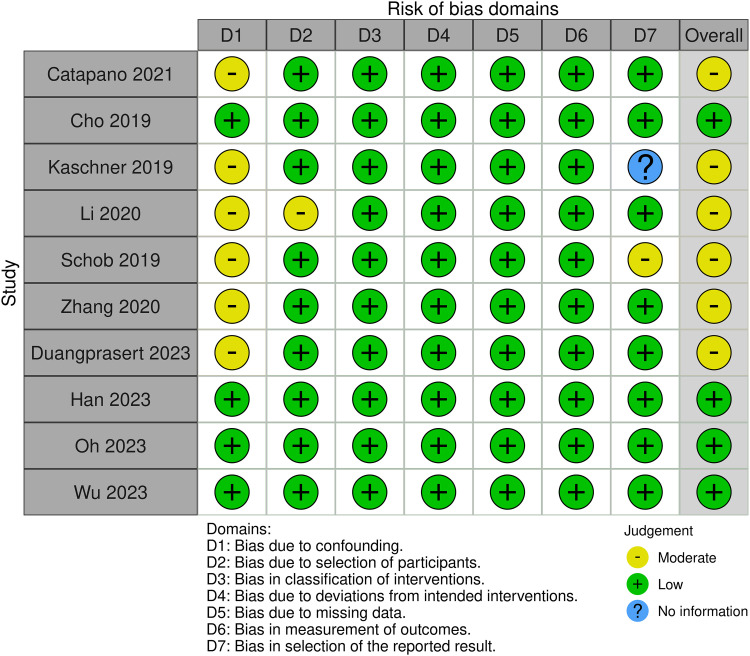
Methodological assessment of the included studies
After employing the ROBINS-I tool, it was found that four studies exhibited a low risk of bias,3,5,14,20 while six were categorized as having a moderate risk (Figure 2).13,15–19 A noteworthy observation is that confounding factors were neither adequately controlled nor compared among the six studies with a moderate risk of bias. Furthermore, factors contributing to this moderate risk included imprecise descriptions of the patient selection process, 16 and a lack of clarity regarding the outcomes analyzed in the methods section.15,17 An overall risk of bias by each domain is depicted in Figure 3.
Figure 2.
Traffic-light plot demonstrating the methodological assessment of each study.
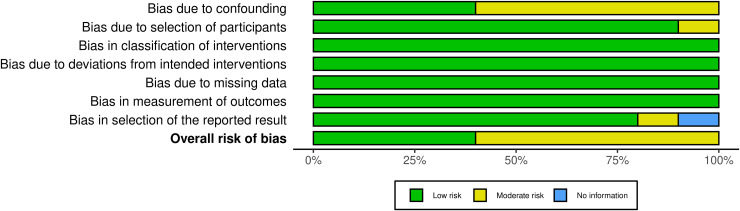
Figure 3.
Summary plot illustrating the overall quality of the literature by each domain.
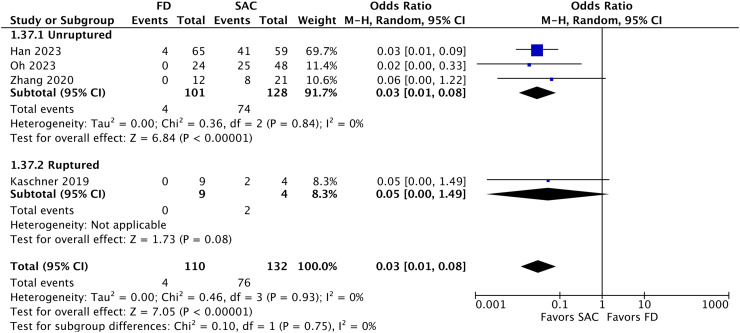
Pooled analysis of all studies
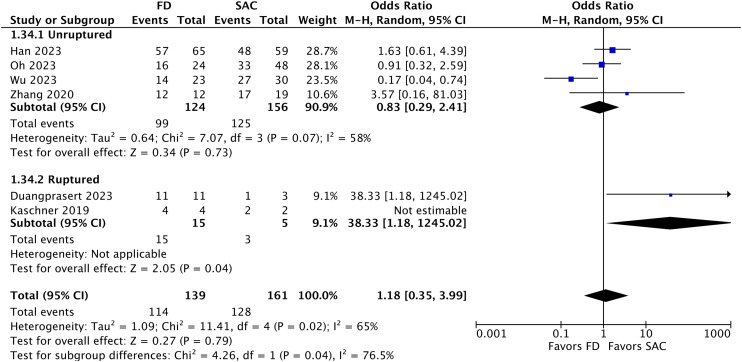
In a pooled analysis of 10 studies, comprising 195 FD and 222 SAC patients with cerebral aneurysm, SAC has significantly higher postoperative complete aneurysm occlusion rates (OR 0.03; 95% CI 0.01–0.08; p < 0.01; Figure 4). Nonetheless, no significant differences were found in follow-up complete aneurysm occlusion (OR 1.18; 95% CI 0.35–3.99; p > 0.5; Figure 5). In the ruptured subgroup, Duangprasert et al. significantly favored the FD group. 19
Figure 4.
Forest plot illustrating the comparison of postoperative complete aneurysmal occlusion.
Figure 5.
Forest plot depicting the comparison of follow-up complete aneurysm occlusion.
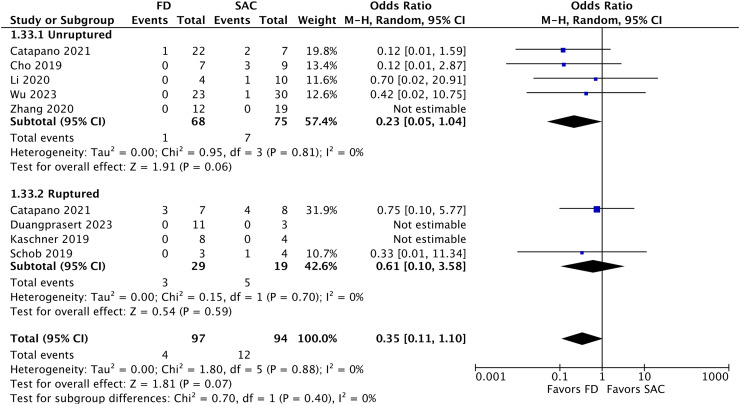
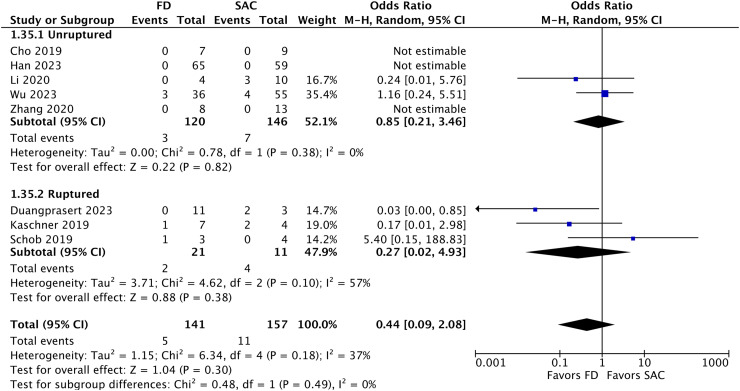
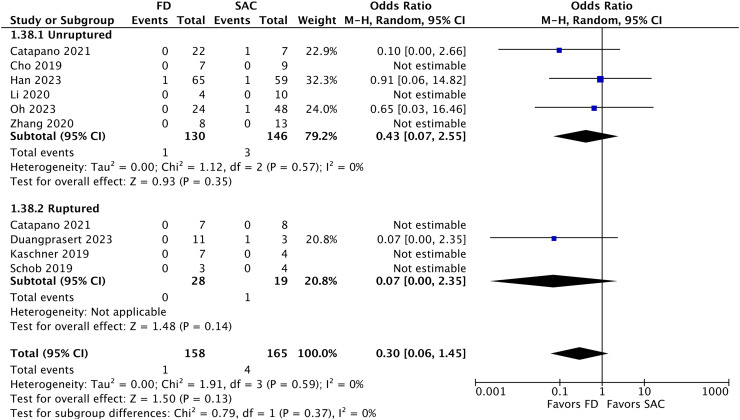
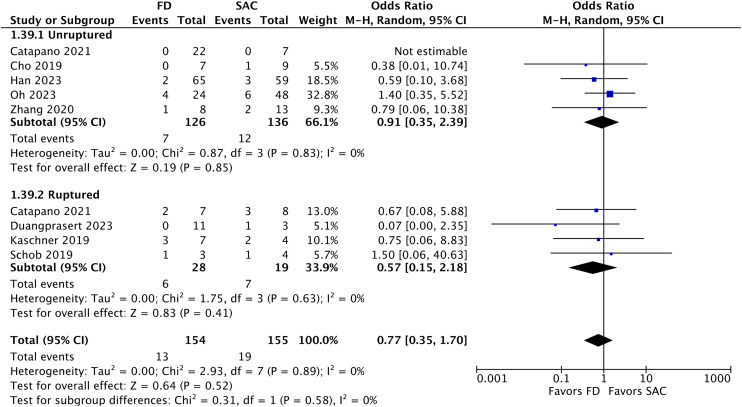
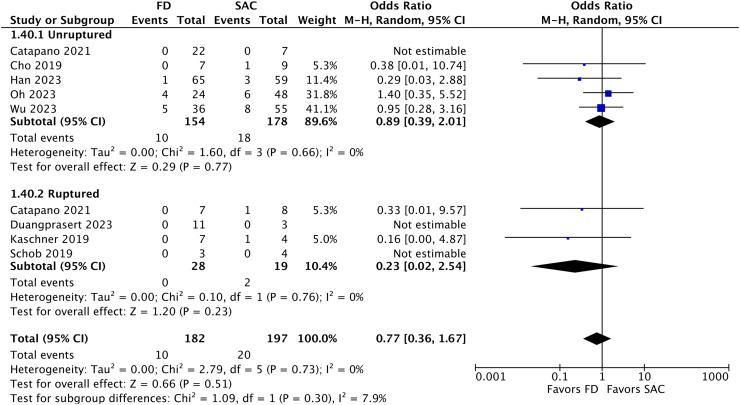
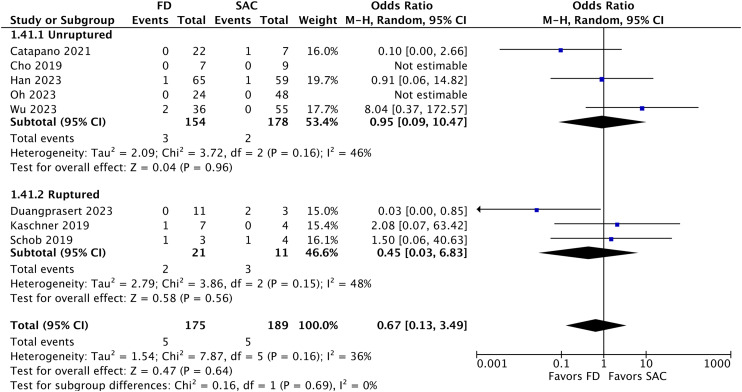
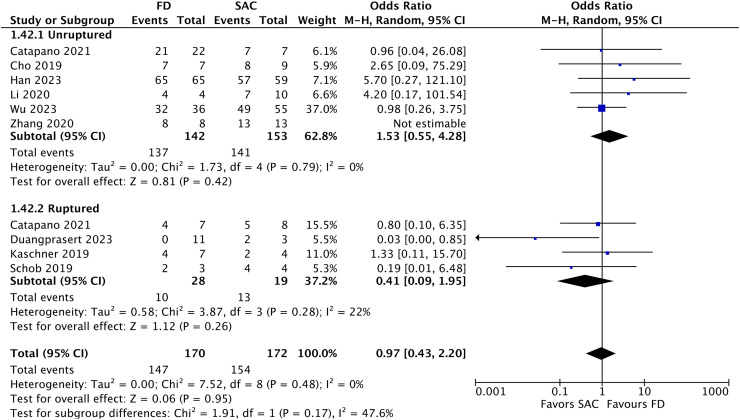
Flow diverter had lower retreatment rates, but there was no significant statistical significance (OR 0.35; 95% CI 0.11–1.10; p = 0.07; Figure 6). There was also no significant statistical difference for total mortality (OR 0.44; 95% CI 0.09–2.08; p = 0.30; Figure 7); related mortality (OR 0.47; 95% CI 0.07–3.26; p = 0.44; Supplementary Digital Material); intraoperative complications (OR 0.30; 95% CI 0.06–1.45; p = 0.13; Figure 8); postoperative complication (OR 0.77; 95% CI 0.35–1.70; p = 0.52; Figure 9); ischemic complications (OR 0.77; 95% CI 0.36–1.67; p = 0.51; Figure 10); hemorrhagic complications (OR 0.67; 95% CI 0.13–3.49; p = 0.64; Figure 11); good clinical outcomes (OR 0.97; 95% CI 0.43–2.20; p = 0.95; Figure 12); and recurrence (OR 0.38; 95% CI 0.13–1.10; p = 0.08; Supplementary Digital Material). Funnel plots are available in the Supplementary Digital Material.
Figure 6.
Forest plot demonstrating the comparison of retreatment.
Figure 7.
Forest plot illustrating the comparison of total mortality.
Figure 8.
Forest plot depicting the comparison of intraoperative complications.
Figure 9.
Forest plot illustrating the comparison of postoperative complications.
Figure 10.
Forest plot illustrating the comparison of ischemic complications.
Figure 11.
Forest plot illustrating the comparison of hemorrhagic complications.
Figure 12.
Forest plot demonstrating the comparison of good clinical outcomes.
Discussion
Overview
This systematic review and meta-analysis aimed to compare the efficacy of FD and SAC in treating DIAs. The study included 10 articles and involved 417 patients, with most patients enrolled in China. The analysis revealed that FD had lower, but not statistically significant, retreatment rates compared to SAC, although postoperative complete occlusion significantly favored SAC. Importantly, the two treatments had no significant differences in complete occlusion rates at the last follow-up. Additionally, no significant disparities were observed regarding recurrence, good clinical outcomes, complications, or mortality rates. Subanalyses based on the rupture status of the aneurysm were conducted. Future studies are required to expand sample sizes, enhance methodological design, and confirm whether or not FD has statistical lower retreatment rates compared with SAC.
Complete occlusion and recanalization
Immediate complete occlusion rates for aneurysms were significantly higher in SAC compared to FD, which was anticipated given the nature of the SAC procedure and results seen in previous studies.3,5 However, FD achieved similar occlusion rates during follow-up, indicating a relative similarity in outcomes between the two procedures. After one year, FD demonstrates promising occlusion rates, 5 highlighting possible favorable long-term outcomes. Only one study significantly favored SAC over FD for this outcome. Nevertheless, the authors acknowledge that both techniques yielded comparable adequate occlusion and safety outcomes, highlighting the need for further investigation. 20
Duangprasert et al. demonstrated that all 11 patients who underwent FD had complete aneurysm occlusion at follow-up, compared to one out of three patients in the SAC group. 19 Still, Zhang et al. reported a higher rate of follow-up complete occlusion for FD placement compared to SAC (90% vs. 72.5%), with significantly more obliteration over time in aneurysms treated with FDs than in those treated with SAC. 18
Our study achieved no statistical significance regarding the disparity in FD and SAC recanalization/recurrence, even though it came close. The close-to-significant differences in the analysis of retreatment rates can also demonstrate this. In their study, Oh et al. observed that major recanalization at six months was significantly lower in the subset of patients undergoing FD placement compared to SAC (OR = 0.196; p = 0.027). Additionally, they noted a more favorable cumulative rate of major recanalization with FD placement (hazard ratio = 0.291; p = 0.048). However, the two modalities had no significant differences regarding overall recanalization rates or procedural and delayed complication rates. 3
As per existing literature, recanalization after placement of FDs is influenced by factors such as aneurysm size, involvement of major branches, and fusiform configuration.21–24 Conversely, recanalization of vertebrobasilar artery dissecting aneurysms following SAC correlates with postprocedural occlusive outcomes and involvement of major branches. 25 Han et al. emphasized the need for future studies investigating those factors and others associated with recurrence, such as endothelialization and hemodynamic environment. 5
Mortality and clinical outcomes
Based on the analysis, both procedures demonstrated no significant difference in mortality. Li et al. reported higher mortality rates for SAC when treating unruptured aneurysms (0% for FD and 30% for SAC) but did not describe the reasons for deaths. 16 However, when analyzing larger samples, such as those in the studies by Wu et al. 20 and Han et al., 5 no difference was observed, indicating the need for further research. Regarding ruptured aneurysms, some results also appeared to favor FD, but with small sample sizes and no statistical significance.15,19 Duangprasert et al. provided an example of two deaths related to the SAC, compared to no death in the FD group. 19 Special attention should be given to the aneurysm after rupture, especially regarding the chance of rerupture. 13 Narata et al. found a 69–71.4% incidence of rebleeding after initial rupture, with 57% of bleedings occurring during the first day. After rerupture, the mortality rate is up to 46.7% compared with 8.3% of the aneurysm without rebleeding. 26
Regarding clinical outcomes, studies involving larger populations have shown similar results for FD and SAC.20,5 Catapano et al. slightly favored FD, with 86.2% achieving an mRS score of 0–2 compared to 80% for SAC. However, when analyzing outcomes based on the rupture status, there is controversy, with FD showing a good clinical outcome in 57.1% of cases versus 62.5% for SAC. 13
Complications
Upon analysis, both procedures demonstrated no significant differences. Hemorrhagic complications included rerupture and rebleeding. Ischemic complications mainly involved in-stent stenosis and thrombosis. Despite no statistical significance, Catapano et al. yielded better complication rates with FD than SAC (7% vs. 27%), demonstrating rebleeding in both cases of FD complications, justified by antiplatelet to avoid thrombosis. 13 Our analysis for hemorrhagic complications did not show a difference for both techniques.
Conversely, Han et al. demonstrated that thromboembolic complications were more common than hemorrhagic complications in their study. 5 This is a matter of heightened relevance once considering future perspectives of anticoagulation therapy. As per Wu et al., who also achieved heightened ischemia rates, potential causes of ischemic events following endovascular treatment include inadequate stent expansion, hyporesponsiveness to antiplatelet drugs, acute or delayed occlusion of perforating vessels, delayed cobalt allergic reactions, and detachment of intraluminal thrombus during stenting or coiling procedures. 20 Zhang et al. emphasized the significance of utilizing antiplatelet medications and closely monitoring platelet function, with adjustments to medication and dosage based on individual response, as crucial factors for successful FD placement. 18
Future perspectives
Cost-effectiveness studies can shed light on whether different materials, lengths of hospitalization, and retreatment rates impact financially the treatment. Radiation burden can also be studied. More DIAs studies are being published,27–30 and the understanding of the pathology is improving. We hope this analysis further enhances the comprehensiveness of the literature.
Limitations
Although the ROBINS I assessment yielded a relatively favorable level of bias, large randomized, prospective, multicenter studies are currently missing. Larger sample sizes are required to confirm the results and address the limitations imposed by TSA. Further studies focusing solely on comparing both techniques instead of reporting institutional experiences with DIAs could provide useful evidence. Lastly, retrospective studies should be mentioned as a significant limitation.
Conclusion
The present meta-analysis comparing FD and SAC for treating DIAs demonstrated that SAC has significantly higher rates of complete aneurysm occlusion. However, both techniques achieved similar complete occlusion rates in the follow-up analysis. Flow diverter is accompanied by lower, but not statistically significant, retreatment rates than SAC. Notwithstanding, the results should be evaluated considering significant limitations, such as the lack of randomization and small sample sizes. Further randomized, multicenter, and prospective studies with robust sample sizes are warranted for more conclusive clinical recommendations.
Supplemental Material
Supplemental material, sj-docx-1-ine-10.1177_15910199241301820 for Flow diverter versus stent-assisted coiling treatment for managing dissecting intracranial aneurysms: A systematic review and meta-analysis by Leonardo O. Brenner, Milena Zadra Prestes, Cid Soares, Pedro Romeiro, Victor A. Gomez, Nicollas Nunes Rabelo, Leonardo C. Welling, Stefan W. Koester, Agostinho C. Pinheiro, Sávio Batista, Raphael Bertani, Eberval Gadelha Figueiredo and Daniel Dutra Cavalcanti in Interventional Neuroradiology
Acknowledgements
The authors thank the professionals who work at each included institution.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Leonardo O. Brenner https://orcid.org/0009-0009-5612-556X
Cid Soares https://orcid.org/0009-0003-4476-2357
Agostinho C. Pinheiro https://orcid.org/0000-0002-2496-9479
Supplemental material: Supplemental material for this article is available online.
References
- 1.Bond KM, Krings T, Lanzino Get al. et al. Intracranial dissections: a pictorial review of pathophysiology, imaging features, and natural history. J Neuroradiol 2021; 48: 176–188. [DOI] [PubMed] [Google Scholar]
- 2.Han J, Liu F, Chen J, et al. Periprocedural cerebrovascular complications and 30-day outcomes of endovascular treatment for intracranial vertebral artery dissecting aneurysms. J Neurosurg 2022: 1–9. Published online November 18, 2022. DOI: 10.3171/2022.10.JNS221953. [DOI] [PubMed] [Google Scholar]
- 3.Oh HS, Bae JW, Hong CE, et al. Stent-assisted coil embolization versus flow-diverting stent in unruptured vertebral artery dissecting aneurysms: efficacy and safety comparison. Neurosurgery 2023; 93: 120–127. [DOI] [PubMed] [Google Scholar]
- 4.Liu P, Li Z, Hu L, et al. Clinical characteristics, endovascular choices, and surgical outcomes of intracranial vertebral artery dissecting aneurysms: a consecutive series of 196 patients. J Neurosurg 2022; 138: 215–222. Published June 3, 2022. [DOI] [PubMed] [Google Scholar]
- 5.Han J, Tong X, Han M, et al. Flow diverters versus stent-assisted coiling in unruptured intracranial vertebral artery dissecting aneurysms. J Neurosurg 2024; 140: 1064–1070. Published online October 13, 2023. [DOI] [PubMed] [Google Scholar]
- 6.Lu X, Zhang Y, Zhou H, et al. Flow diverters in the treatment of unruptured vertebral artery dissecting aneurysm: a single-center experience. Front Neurol 2023; 14: 1050619. Published February 22, 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amoukhteh M, Hassankhani A, Valizadeh P, et al. Flow diverters in the treatment of intracranial dissecting aneurysms: a systematic review and meta-analysis of safety and efficacy. J Neurointerv Surg 2024; 16: 1005–1012. Published online January 11, 2024. [DOI] [PubMed] [Google Scholar]
- 8.Petr O, Brinjikji W, Cloft H, et al. Current trends and results of endovascular treatment of unruptured intracranial aneurysms at a single institution in the flow-diverter era. AJNR Am J Neuroradiol 2016; 37: 1106–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gozal YM, Abou-Al-Shaar H, Alzhrani G, et al. Complications of endovascular and open aneurysm surgery in the era of flow diversion. Acta Neurochir Suppl 2023; 130: 85–94. [DOI] [PubMed] [Google Scholar]
- 10.Higgins JPT, Thomas J, Chandler J, (eds), et al. Cochrane handbook for systematic reviews of interventions version 6.4 (updated August 2023). Cochrane, https://www.training.cochrane.org/handbook (2023).
- 11.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J 2021; 372: n71. Published March 29, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Br Med J 2016; 355: i4919. Published Octobet 12, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Catapano JS, Ducruet AF, Cadigan MS, et al. Endovascular treatment of vertebral artery dissecting aneurysms: a 20-year institutional experience. J Neurointerv Surg 2022; 14: 257–261. [DOI] [PubMed] [Google Scholar]
- 14.Cho DY, Kim BS, Choi JH, et al. The fate of unruptured intracranial vertebrobasilar dissecting aneurysm with brain stem compression according to different treatment modalities. AJNR Am J Neuroradiol 2019; 40: 1924–1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaschner MG, Kraus B, Petridis Aet al. et al. Endovascular treatment of intracranial ‘blister’ and dissecting aneurysms. Neuroradiol J 2019; 32: 353–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li M, Liang H, Wang J. Unfavorable outcomes related to endovascular treatment of giant vertebrobasilar aneurysms. Front Neurol 2020; 11: 748. Published August 11, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schob S, Becher A, Bhogal P, et al. Segment occlusion vs. reconstruction-a single center experience with endovascular strategies for ruptured vertebrobasilar dissecting aneurysms. Front Neurol 2019; 10: 207. Published March 13, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang Y, Tian Z, Zhu W, et al. Endovascular treatment of bilateral intracranial vertebral artery aneurysms: an algorithm based on a 10-year neurointerventional experience. Stroke Vasc Neurol 2020; 5: 291–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duangprasert G, Noiphithak R, Sukhor Set al. et al. Efficacy and predicting factors of multimodal treatment for ruptured intracranial vertebral artery dissecting aneurysms. Neurosurg Rev 2023; 46: 321. Published December 1, 2023. [DOI] [PubMed] [Google Scholar]
- 20.Wu Q, Wang C, Xu S, et al. Low-profile visualized intraluminal support-within-enterprise overlapping-stent technique versus flow diversion in the treatment of intracranial vertebrobasilar trunk dissecting aneurysms. Quant Imaging Med Surg 2023; 13: 3536–3546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bender MT, Colby GP, Lin LM, et al. Predictors of cerebral aneurysm persistence and occlusion after flow diversion: a single-institution series of 445 cases with angiographic follow-up. J Neurosurg 2018; 130: 259–267. [DOI] [PubMed] [Google Scholar]
- 22.Moshayedi H, Omofoye OA, Yap E, et al. Factors affecting the obliteration rate of intracranial aneurysms treated with a single pipeline embolization device. World Neurosurg 2017; 104: 205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maragkos GA, Ascanio LC, Salem MM, et al. Predictive factors of incomplete aneurysm occlusion after endovascular treatment with the pipeline embolization device. J Neurosurg 2019; 132: 1598–1605. Published April 26, 2019. [DOI] [PubMed] [Google Scholar]
- 24.Hanel RA, Monteiro A, Nelson PK, et al. Predictors of incomplete aneurysm occlusion after treatment with the pipeline embolization device: PREMIER trial 1 year analysis. J Neurointerv Surg 2022; 14: 1014–1017. [DOI] [PubMed] [Google Scholar]
- 25.Jeon JP, Cho YD, Rhim JK, et al. Stent-assisted coil embolization of vertebrobasilar dissecting aneurysms: procedural outcomes and factors for recanalization. Korean J Radiol 2016; 17: 801–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Narata AP, Yilmaz H, Schaller K, et al. Flow-diverting stent for ruptured intracranial dissecting aneurysm of vertebral artery. Neurosurgery 2012; 70: 982–989. [DOI] [PubMed] [Google Scholar]
- 27.Dmytriw AA, Alrashed A, Enriquez-Marulanda A, et al. Unruptured intradural posterior circulation dissecting/fusiform aneurysms natural history and treatment outcome. Interv Neuroradiol 2023; 29: 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen L, Leng X, Zheng C, et al. Computational fluid dynamics (CFD) analysis in a ruptured vertebral artery dissecting aneurysm implanted by pipeline when recurrent after LVIS-assisted coiling treatment: case report and review of the literatures. Interv Neuroradiol 2023; 29: 442–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu Y, Yu J, Zhang T, et al. Endovascular treatment of distal internal carotid artery aneurysms and vertebral artery dissecting aneurysms with the Willis covered stent: a single-center, retrospective study. Interv Neuroradiol 2023; 29: 63–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amoukhteh M, Hassankhani A, Jannatdoust P, et al. Comparative meta-analysis of endovascular strategies for intracranial dissecting aneurysms: flow diverters versus stents with or without coiling. Interv Neuroradiol 2024. Published online June 14, 2024. DOI: 10.1177/15910199241262070. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-ine-10.1177_15910199241301820 for Flow diverter versus stent-assisted coiling treatment for managing dissecting intracranial aneurysms: A systematic review and meta-analysis by Leonardo O. Brenner, Milena Zadra Prestes, Cid Soares, Pedro Romeiro, Victor A. Gomez, Nicollas Nunes Rabelo, Leonardo C. Welling, Stefan W. Koester, Agostinho C. Pinheiro, Sávio Batista, Raphael Bertani, Eberval Gadelha Figueiredo and Daniel Dutra Cavalcanti in Interventional Neuroradiology