Abstract
Background
Chronic diseases are a global health challenge, and therefore, more attention should be paid to improving self-efficacy in people with chronic diseases. This study examined the relationship between family health and self-efficacy, and explored the mediating role of perceived social support and the moderating role of health literacy. The aim is to enhance the self-efficacy of chronic patients by improving family health, social support, and health literacy, thereby improving their physical and mental state.
Methods
A cross-sectional study based on psychological and behavioural factors was conducted, namely, the 2022 China Residents Survey, which included 5150 Chinese patients with chronic diseases. The General Self-Efficacy Scale-Short Form was used to assess self-efficacy, the Health Literacy Questionnaire-short form was used to assess health literacy, the Perceived Social Support Scale–Short Form was used to evaluate perceived social support, and the Chinese version of the Family Health Scale-Short Form was used to assess family health status.
Results
Family health of patients with chronic diseases had a significant positive effect on self-efficacy. Perceived social support was identified as a partial mediator between family health and self-efficacy, accounting for 59.39% of the total effect. Health literacy moderated the impact of family health on perceived social support and self-efficacy.
Conclusions
Chronic diseases have become a global health challenge, and more attention should be paid to improving the self-efficacy of the chronically ill population. Our results not only facilitate the understanding of the relationship mechanisms between family health and self-efficacy in chronic patients but can also serve as a guide for healthcare workers and policymakers who wish to provide better care for patients.
Keywords: Chronic diseases, Family health, Self-efficacy, Health literacy, Perceived social support, Mediating effect with regulation
Background
Chronic diseases such as cardiovascular disease and diabetes have become major global health threats and are a burden to the medical system and economy. As the largest developing country, China has a vast number of patients with chronic diseases. Simultaneously, with dramatic changes in lifestyle and an increase in population aging, the incidence of chronic diseases is increasing annually [1]. According the Sixth National Health Service Statistical Survey in 2018, major chronic diseases such as cardiovascular and cerebrovascular diseases, diabetes, and cancer account for more than 90% of China's disease economic burden, with the prevalence of chronic diseases among people aged 55–64 years reaching 48.4% and that among older adults aged 65 years and above reaching 62.3%. Thus, it is crucial to prevent and manage chronic diseases and provide effective ways to improve the physical and mental health of the affected population.
Self-efficacy (SE) is the belief that a person can successfully perform the behaviours required to produce an outcome. In other words, it is confidence in a person’s ability to accomplish something. Bandura states that it determines whether an individual views their emotional health in a self-helping or self-defeating manner [2]. As a crucial psychosocial concept, SE is closely related to the health and well-being of a population. For chronic patients, self-health management is crucial for chronic disease control and management, and SE is an important prerequisite for self-health management [3]. Studies have shown that older adults with higher SE can enhance their confidence in their ability to manage symptoms related to chronic diseases and consistently treat their illness over the long term [4] and improve their skills to better cope with diseases [5]. However, current levels of SE in chronic patients are generally low [6]. Physical and mental distress due to illness and social alienation are reasons for a decrease in SE [7]. Patients experience negative emotions owing to the disease, and SE is reduced. A decrease in SE is not conducive to good self-health management, thereby aggravating disease. In the long run, this leads to a vicious cycle. Therefore, it is important to improve SE in chronic patients to overcome this dilemma.
Societies and families play important roles in managing chronic diseases. Family is the core of society, providing not only material support but also spiritual and emotional support. Owing to a decline in psychological and physical function, chronic patients may become dependent on others, while the family, as a social system to which they are most likely to receive support, plays a vital role in providing primary healthcare for patients. Studies have shown that family functioning in patients with chronic diseases affects their physical health and behavioural compliance [8]. Family members help chronically ill patients manage their conditions [9], playing an important role in guiding primary care for chronic diseases [10].
The concept of family health (FH) has gradually drawn attention in the control and management of chronic diseases. FH refers to resources at the family unit level, which are developed from the intersection of the internal interactions of each family member's health, abilities, behaviours, personalities, and members, as well as their physical, social, emotional, economic, and medical resources [11]. It integrates the key elements of previous concepts, such as family structure, family function, and family social network; strengthens the ability and sociability of the family to obtain external resources; and emphasises health-related elements, linking individual health with social group health [12]. FH is more important for chronic patients, especially in Chinese families in the context of Confucian culture. Under the influence of Confucianism, Chinese culture is collectivist, and Chinese families maintain the health of their members through mutual assistance and collective action within family [13, 14]. Currently, the FH level of Chinese families with chronic diseases is relatively good [15]. Given the interdependence of Chinese family culture, a higher level of FH can help maintain a healthful family environment and improve patients' health behaviors [15].
There is a close correlation between FH and SE levels. Good family support significantly affects patient recovery and SE. As the main source of support for chronic patients, the family can enhance their SE and improve self-care behaviors [16, 17]. Secondly, a broad network of psychosocial family structures may influence SE [18]. Individuals with larger family support networks are more likely to have higher SE [19]. In addition, there is a statistically significant correlation between family functioning and SE [20]. Puspasari et al. showed that family functioning can improve SE [21]. A functioning family provides strong support for its members and can improve self-confidence and problem-solving skills. Subsequently, it enhances overall SE [22]. Meanwhile, previous studies have shown a positive correlation between family environment and SE [23]. Individuals are more likely to have higher SE when an unhealthy family environment transforms into a healthy and productive one [24]. In conclusion, FH and SE are related. Thus, we hypothesized: FH may have a positive effect on SE, and good FH is conducive to improving SE.
Perceived social support (PSS) is an individual's subjective perception of their own level of social support. Previous studies have shown that PSS is closely related to an individual’s FH level, and social support has therefore been regarded as an important resource for improving individual FH. Patients with higher PSS have been shown to have higher FH levels and better family functioning [25]. Likewise, chronic disease patients with high FH levels typically have a good family atmosphere, high PSS, and can actively face negative emotions. Perceived family and social support has also been found to be closely related with SE [17, 26]. Other studies have revealed a positive correlation between PSS and SE [27, 28], and that PSS is an important indicator of medication adherence SE in patients [29]. Some cohort studies have also shown that increases in specific types of PSS lead to increased SE [30–32]. Therefore, we hypothesized: PSS may be a vital mediating factor in the relationship between FH and SE for patients with chronic diseases.
Health literacy (HL) is defined as the ability to obtain, process, understand, and communicate health-related information that contributes to health decision-making and the management of health conditions [33, 34]. Considering HL as a resource, a higher level of HL is conducive to a positive environment for the self-management of patients with chronic diseases. Studies have shown that patients with high levels of HL can effectively use their social support systems and receive material and psychological support [35], while maintaining a positive perception of their illness [36, 37]. This means that the higher the HL, the stronger the patient’s ability to cope with illness, and the less dependence on family members to cope with health problems and access support [38]. This indicates that high levels of HL may enhance the positive effect of FH on PSS and diminish the negative impact of FH on PSS. HL in patients with chronic diseases may moderate the relationship between FH and PSS. Research also suggests that HL and SE are closely related. High levels of HL contribute to the improvement of patients' SE, which leads to the control and improvement of disease [39]. Further improvements in SE in the family environment, family structure, and well-functioning individuals may occur when the level of HL is high [40]. This indicates that high levels of HL may enhance the positive effect of FH on SE and diminish the negative impact of FH on SE. HL may moderate the relationship between FH and SE. In addition, previous studies have shown that HL plays a crucial moderating role in similar contexts [41]. In terms of patient emotions, HL moderates the relationship between health anxiety and emotional regulation. High levels of HL can buffer the negative effects of health anxiety on emotional regulation [42], thereby maintaining the stability of patients' SE. In terms of patient medication, medication literacy plays a moderating role between family functioning and patient medication adherence [43], and good literacy can enhance the positive impact of family functioning on patient medication adherence. Meanwhile, according to the protective factor-protective factor model [44], interactions may occur between different protective factors, and the effect of one protective factor on the outcome variable may change depending on the level of the other one. In this study, both HL and FH served as protective factors. The enhancement or weakening of HL may lead to changes in the relationship between FH and PSS, as well as between FH and SE. Based on the above evidence, we hypothesized: HL may have a moderating effect on FH and PSS relationships, as well as the moderating effect on FH and SE relationships.
Previous research has primarily focused on chronic patients’ SE from the perspectives of family function, family members’ health, and family support; however, there is a lack of research on the SE of patients with chronic diseases from the perspective of FH. Second, when considering the influence of family factors, most studies have been conducted only on family caregivers or family members, and few studies have been conducted separately on chronic patients. Third, empirical studies on the mental health of chronic patients tend to focus on the impact of factors such as family function, structure, and social support on mental health but rarely focus on how these influencing factors interact and connect. The prevention and treatment of chronic diseases has always been an important issue in China and abroad, and the physical and mental health of people with chronic diseases should receive full attention. Exploring the relationship between FH and the SE of patients can help improve patients’ SE and enhance the self-health management of patients, enrich the relevant theoretical framework of chronic disease management and control, and provide a basis for local authorities to formulate policies and interventions. Therefore, this study aimed to explore the impact of FH on SE in chronic patients and provide a theoretical basis for the improvement of patients’ SE in China. Based on the literature review, we propose the following hypotheses:
Hypothesis 1 [H1]: FH positively correlates with SE in patients with chronic diseases.
Hypothesis 2 [H2]: There is a mediating effect between PSS, FH, and SE.
Hypothesis 3 [H3]: HL can moderate the association between FH and PSS, as well as the association between FH and SE. High levels of HL will buffer against the effects of FH on PSS and the effects of FH on SE.
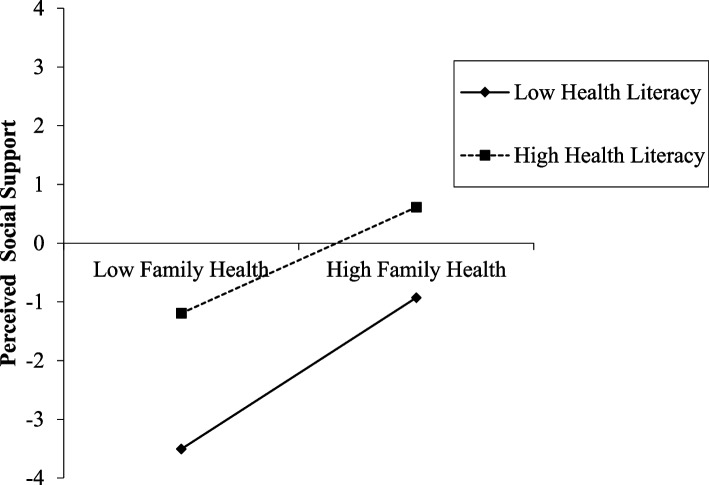
Our proposed model for these relationships is shown in Fig. 1.
Fig. 1.
Hypothetical model of family health, perceived social support, health literacy, and self-efficacy
Methods
Samples and participants
The study data were obtained from a cross-sectional survey conducted from 20 June to 31 August, 2022 that focused on the psychology and behaviour of Chinese residents [45]. The sample was selected from a comprehensive range of locations across China, including 148 cities, 202 districts, 390 townships, and 780 villages. These locations were chosen to represent the diverse population distribution across the 23 provinces of China, five autonomous regions, and four municipalities directly under the Central Government [46, 47].
For study eligibility, participants had to be at least 12 years old, hold Chinese nationality as a permanent resident, and have a limited travel history in the past year (less than one month). The participants were required to express their willingness to participate in the study and provide informed consent. Additionally, they were required to be capable of independently completing an online questionnaire or with the assistance of an investigator, while comprehending the meaning of each question. Exclusion criteria encompassed individuals presenting with delirium, abnormal symptoms, and cognitive impairment; participants concurrently engaged in other similar research endeavors; and those displaying unwillingness to participate.
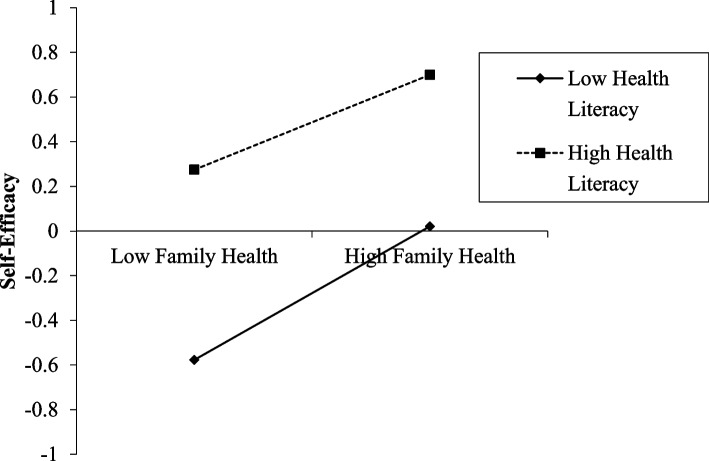
Initially, we collected 30 505 questionnaires, from which we selected a subset of 5684 patients with chronic diseases based on clear rejection criteria, where the response time was less than or equal to 240 s. After checking the questionnaires for logical errors, such as selection contradictions and discrepancies, 5150 valid questionnaires were retained, comprising 2547 women and 2603 men. Our screening process for respondents is shown in Fig. 2.
Fig. 2.
Screening process for respondents
Variables
Independent variable: Family Health (FH)
This study considered FH as an independent variable, taking into account family structure, function, and social networks. It emphasises the ability to obtain external resources and establish social connections while also focussing on health factors and establishing a connection between individual and social group health [15]. The Family Health Scale—Short Form (FHS-SF) was developed in Chinese by Crandall et al. [48], translated by members of the China Family News Research Centre. The FHS-SF summarises four dimensions related to family social and emotional health: 1) FH social processes, 2) FH social styles, 3) FH resources, and 4) external family social support. There are 10 specific items, each scored using a 5-point Likert scale during the assessment. Items 6, 9, and 10 are scored inversely. According to a literature review, the clinical cut-off points of the scale for assessing FH are as follows: < 25% for poor FH, between 25 and 75% for moderate FH, and ≥ 75% for good FH. A final score of 10–12 therefore indicates poor FH, a score of 13–37 indicates moderate FH, and a score of 38–50 indicates good FH.
Dependent variable: Self-Efficacy (SE)
SE is the dependent variable in this study and was measured using the novel General Self-Efficacy Scale (NGSES), developed by Chen et al. [49] and revised by Feng and Chen [50], which comprises eight items. The reliability and validity analysis of the NGLES-SF by Wang et al. [51] determined that the three items were measured from three dimensions: level or degree, intensity, and universality. A 5-point Likert scale ranging from 0 (strongly disagree) to 4 (strongly agree) was used to measure SE. Higher scores indicate higher SE. A low SE was defined as a total score between 3 and 11, while a high SE was defined as a total score between 12 and 15 [52].
Mediating variable: Perceived Social Support (PSS)
PSS emphasises an individually subjective perception of how much social support is received, including three dimensions, namely: family support (receiving emotional help and support from family members), friend support, and other support (leaders, relatives, colleagues), and the questionnaire uses three items, each of which ranges from 0 (strongly agree) to 6 (strongly agree). A final total score between 3 and 7 is considered low support. This study defined high support status as a total score between 15 and 28, whereas a total score between 8 and 14 indicates moderate support status.
Moderating variable: Health Literacy (HL)
According to the World Health Organization (WHO), HL refers to the ability to access, comprehend, recognise, and transfer health information for different health conditions to promote and sustain good health across one’s lifespan [53]. The Health Literacy Questionnaire-Short Form 12 (HLS-SF12) was used to assess applicability in the Chinese population. This study employed a condensed version of the Health Literacy Scale comprising nine items. Each item is rated on a 4-point Likert scale, with higher scores indicating elevated levels of HL. According to the European Health Literacy Project, patients with an HL index of 33 or less are considered to have limited HL [54]. Based on the literature, the population was divided into two groups: a high HL group (34–36 points) and a middle and low HL group (9–33 points).
Covariates
This study employed personal, family, and social characteristics as control variables. The personal characteristics surveyed include gender (1 = male, 2 = female), age (1 = 12–17 years old, 2 = 18–59 years old, 3 = 60 years old and above), type of household registration (1 = non-agricultural, 2 = agricultural), highest level of education (1 = below primary school, 2 = junior high school, 3 = high school, 4 = technical secondary school, 5 = bachelor's degree or above), and subsidy as a binary variable (1 = yes, 0 = no); Family characteristics refer to different types of families, including 1 = nuclear family, 2 = backbone family (parents and married children), 3 = single-parent family, 4 = other types of families. Other types of families include conjugal families, joint families (consisting of parents and two or more married children, or a group of unmarried siblings), dink families (consisting of two couples who have chosen not to have children), intergenerational families, single families (a family that chooses not to marry or remarry after divorce but lives independently), reformed families (in which at least one couple has marriage experience and may have children from previous marriages), cohabiting families (in which two romantically involved people live together on a continuous and stable basis but are not married), families with same-sex couples, etc. The per-capita monthly income of the family is categorised into three groups: 1–3 represents income less than or equal to ¥1500, ¥1501– ¥6000, and greater than ¥6000, respectively. Social characteristics were measured by social status on a scale of 1–7, with 1 being the lowest and 7 the highest. The term "social status" is employed herein to signify subjective social status, which may be defined as the subject's own perception and self-evaluation of the social class to which their family belongs [55, 56].
Statistical analysis
The data for this study were processed and analysed using SPSS 25.0 and the PROCESS v2.16.3 plug-in. The social and demographic characteristics of the participants were analysed using frequency (percentage) statistics. A univariate analysis was performed for continuous variables. An independent samples t-test was used to differentiate categorical variables and discuss the effects of the three primary control variables (individual, family, and society) on the dependent variables. Descriptive statistics and Pearson correlation tests were used to assess correlations between FH, SE, HL, and PSS, with P < 0.05 considered statistically significant. This study used a bootstrap program to analyse the significance of PSS in the mediating role of FH and SE. A total of 5000 bootstrap samples with a 95% confidence interval (CI) were selected. The mediating effect of PSS on the FH and SE of patients with chronic diseases, after controlling for variables, was tested using Model 4 with the PROCESS macro program. Finally, to examine the moderating effect of HL on the relationship between FH and PSS and FH and SE, Model 8 of the PROCESS macro program was used.
Results
Common method bias test
An exploratory factor analysis was conducted using Harman's single-factor test. The results showed that there were seven factors with special values greater than 1, and the factor with the highest explained variation rate was 32.791%, which was less than the critical value of 40%, indicating that there was no serious common method bias.
Personal, family and social statistics of the participants
Among the 5150 valid questionnaires for patients with chronic diseases, 50.5% were male and 49.5% were female. The majority were young and middle-aged people aged 18–59 years (55.6%) and older people aged 60 years and over (42.9%). Most respondents were registered as non-agricultural households (52.4%) and lived in urban areas (66.8%). The highest number of respondents had a university education or higher (35.8%), of which 76.3% received some sort of financial aid. Of the participants, 38.0% came from nuclear families, and 40.7% of the patients with chronic diseases had an average monthly income of 3001–6000 yuan. Most participants rated their social status as roughly in the middle of the scale (34.7%) (Table 1).
Table 1.
Personal, family, and social statistics of participants (N = 5150)
| Characteristics | Number | Percentage |
|---|---|---|
| Personal characteristics | ||
| Gender | ||
| Men | 2603 | 50.5 |
| Women | 2547 | 49.5 |
| Age | ||
| 12–17 | 82 | 1.6 |
| 18–59 | 2861 | 55.6 |
| ≥ 60 | 2207 | 42.9 |
| Household registration type | ||
| Non-agricultural | 2701 | 52.4 |
| Agriculture | 2449 | 47.6 |
| Permanent residence | ||
| Urban | 3439 | 66.8 |
| Rural | 1711 | 33.2 |
| Education | ||
| Primary school and below | 1467 | 28.4 |
| Junior high school | 876 | 17.0 |
| Technical secondary school or high school | 961 | 18.6 |
| College degree or above | 1846 | 35.8 |
| Subsidised | ||
| Have | 3927 | 76.3 |
| Nothing | 1223 | 23.7 |
| Family characteristics | ||
| Family type | ||
| Nuclear family | 1957 | 38.0 |
| Stem family | 1582 | 30.7 |
| Single-parent family | 216 | 4.1 |
| Other forms of family | 1395 | 27.0 |
| Family per capita monthly income | ||
| ≤ 3000 | 1912 | 37.1 |
| 3001–6000 | 2099 | 40.7 |
| > 6000 | 1139 | 22.1 |
| Social characteristics | ||
| Social status | ||
| 1 | 80 | 1.6 |
| 2 | 293 | 5.7 |
| 3 | 856 | 16.6 |
| 4 | 1787 | 34.7 |
| 5 | 1322 | 25.7 |
| 6 | 553 | 10.7 |
| 7 | 259 | 5.0 |
Single factor analysis of self-efficacy in chronic disease patients
There were significant differences in SE between patients with chronic disease according to gender, age, type of household registration, permanent residence, highest level of education, subsidy enjoyment situation, family type, family income, and social status (P < 0.01). Therefore, we adjusted for these factors as control variables in subsequent analyses (Table 2).
Table 2.
Single factor analysis of self-efficacy in chronic patient population (N = 5150)
| Self-efficacy(SE) | |||
|---|---|---|---|
| M ± SD | t/F | ||
| Gender | Men | 7.73 ± 2.390 | 2.785** |
| Women | 7.47 ± 2.414 | ||
| Age | 12–17 | 6.61 ± 2.693 | 28.774** |
| 18–59 | 7.81 ± 2.340 | ||
| ≥ 60 | 7.37 ± 2.447 | ||
| Household registration type | Non-agricultural | 7.85 ± 2.363 | 4.209** |
| Agriculture | 7.33 ± 2.421 | ||
| Permanent residence | Town | 7.81 ± 2.393 | 0.018** |
| Countryside | 7.19 ± 2.377 | ||
| Education | Primary school and below | 7.07 ± 2.338 | 37.250** |
| Junior high school | 7.65 ± 2.482 | ||
| Technical secondary school or high school | 7.80 ± 2.331 | ||
| College degree or above | 7.91 ± 2.390 | ||
| Subsidy enjoyment situation | Have | 7.30 ± 2.653 | 54.451** |
| Nothing | 7.70 ± 2.314 | ||
| Family type | Nuclear family | 7.84 ± 2.325 | 13.306** |
| Stem family | 7.58 ± 2.367 | ||
| Single-parent family | 7.13 ± 2.623 | ||
| Other forms of family | 7.38 ± 2.490 | ||
| Family per capita monthly income | ≤ 3000 | 7.40 ± 2.365 | 12.864** |
| 3001–6000 | 7.66 ± 2.446 | ||
| > 6000 | 7.85 ± 2.371 | ||
| Social status | 1 | 6.74 ± 3.404 | 14.903** |
| 2 | 7.05 ± 2.605 | ||
| 3 | 7.22 ± 2.275 | ||
| 4 | 7.55 ± 2.349 | ||
| 5 | 7.85 ± 2.321 | ||
| 6 | 7.90 ± 2.348 | ||
| 7 | 8.23 ± 2.740 | ||
** P < 0.01
Descriptive statistics and correlation analysis of primary research variables
Descriptive statistics and Pearson’s correlation tests were performed for FH, SE, HL, and PSS. The results showed that the score of FH in the chronic patients’ group was 26.35 ± 6.241, the total score of SE was 8.60 ± 2.40, the total score of PSS was 12.76 ± 3.635, and the total score of HL was 18.42 ± 5.329. There was a significant positive correlation between the variables (P < 0.01), indicating that there was no collinearity problem among the four variables, which was suitable for further exploration using path analysis (Table 3).
Table 3.
Statistical and Pearson correlation analysis results (N = 5150)
| Variable | Basic statistics | The correlation coefficient between variables | |||||
|---|---|---|---|---|---|---|---|
| M | SD | Min–max | 1 | 2 | 3 | 4 | |
| Family health(FH) | 26.35 | 6.241 | 10–50 | 1 | |||
| Self-efficacy(SE) | 8.60 | 2.405 | 3–15 | 0.415** | 1 | ||
| Perceived social support(PSS) | 12.76 | 3.635 | 3–21 | 0.437** | 0.635** | 1 | |
| Health literacy(HL) | 18.42 | 5.329 | 9–36 | 0.446** | 0.423** | 0.384** | 1 |
** P < 0.01
The mediating role of perceived social support
Model 4 of the PROCESS macro procedure was used to examine the mediating effect of PSS on the FH and SE of patients with chronic illness, after controlling for variables. As shown in Table 4 and Fig. 3, H1 was established and FH significantly positively predicted SE (β = 0.1514; P < 0.001). FH significantly and positively predicted PSS (β = 0.2461, P < 0.001). Both PSS and FH significantly positively affected SE (β = 0.3653, P < 0.001; β = 0.0615, P < 0.001).
Table 4.
Testing the mediating effect of perceived social support
| Dependent variable | Independent variable | β | 95% CI | R2 | F | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Self-efficacy(SE) | Family health(FH) | 0.1514*** | 0.1418 | 0.1610 | 0.1951 | 124.568*** |
| Perceived social support(PSS) | Family health(FH) | 0.2461*** | 0.2317 | 0.2606 | 0.2048 | 132.361*** |
| Self-efficacy(SE) | Perceived social support(PSS) | 0.3653*** | 0.3501 | 0.3805 | 0.4375 | 363.330*** |
| Family health(FH) | 0.0615*** | 0.0526 | 0.0704 | |||
*** P < 0.001
Fig. 3.
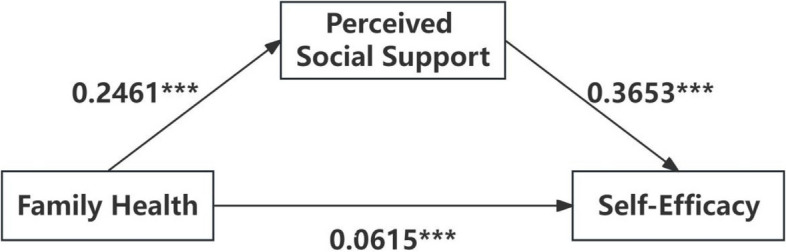
Pathways of influence of the mediating role of perceived social support
A bootstrap procedure was used to test the significance of the mediating effects of PSS on FH and SE. The bootstrap sampling frequency was selected 5000 times and a 95% CI was set. Table 5 shows that the total effect value was 0.1514 (95% CI: 0.1417–0.1610), the direct effect value of FH on SE was 0.0615 (95% CI: 0.0526–0.0704), and the mediating effect value of PSS was 0.0899 (95% CI: 0.0820–0.0985), accounting for 59.39% of the total effect, indicating that PSS partially mediated the relationship between FH and SE. Thus, H2 is supported.
Table 5.
Decomposition table of total effect, direct effect, and indirect effect
| Point estimate | 95% CI | Ratio of effect | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Total effect | 0.1514*** | 0.1418 | 0.1610 | |
| Direct effect | 0.0615*** | 0.0526 | 0.0704 | 0.4061 |
| Indirect effect | 0.0899*** | 0.0820 | 0.0985 | 0.5939 |
*** P < 0.001
Moderated mediation effects
Model 8 of the PROCESS macro program was used to test the moderating effect of HL status. The results showed that after controlling for variables, the product term of FH × HL was a significant predictor of PSS (β = −0.0058, P < 0.001, 95% CI: −0.0077– −0.0039) and interaction was a significant predictor of SE (β = −0.0013, P < 0.001, 95% CI: −0.0024 – −0.0002), suggesting that HL moderated both the prediction of PSS and SE by FH. Thus, H3 was confirmed (see Table 6). Although the moderating effect of health literacy was statistically significant, the β values of these results were relatively small, which means the actual impact may be limited. This is because the large sample size could detect smaller effects, thereby increasing the likelihood of statistical significance in the results.
Table 6.
Path-coefficients of the moderated mediating model
| Dependent variable | Independent variable | B | 95% CI | R2 | F | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Perceived Social Support(PSS) | Family health(FH) | 0.1758*** | 0.1600 | 0.1916 | 0.2555 | 5137.0000*** |
| Health literacy(HL) | 0.1808*** | 0.1606 | 0.2010 | |||
| Int-1 | −0.0058*** | −0.0077 | −0.0039 | |||
| Self-efficacy(SE) | Perceived social support(PSS) | 0.3412*** | 0.3257 | 0.3567 | 0.4533 | 5136.0000*** |
| Family health(FH) | 0.0410*** | 0.0316 | 0.0503 | |||
| Health literacy(HL) | 0.0718*** | 0.0600 | 0.0836 | |||
| Int-2 | −0.0013*** | −0.0024 | −0.0002 | |||
Note: Int-1 Family health × Health literacy, Int-2 Family health × Health literacy
*** P < 0.001
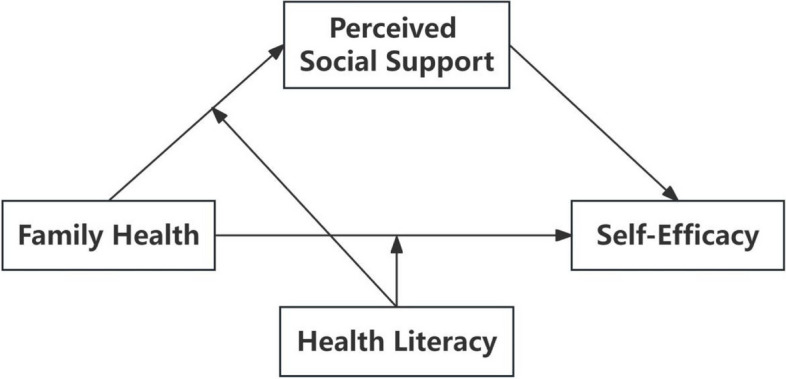
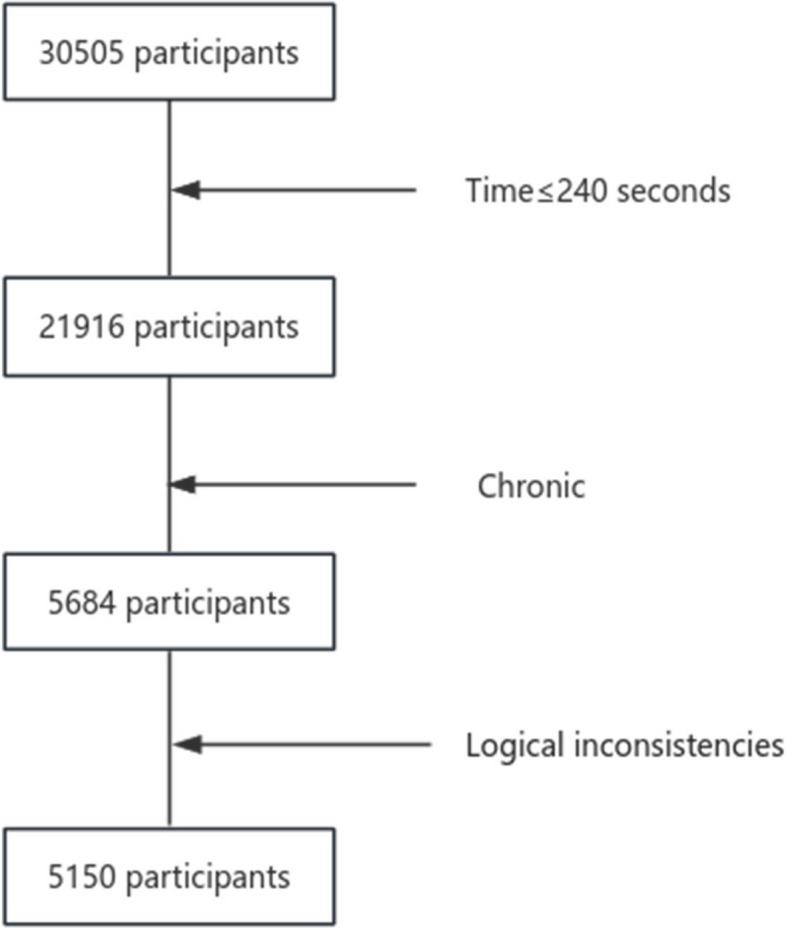
To further analyse the moderating effect of HL, the total HL score was divided into high and low groups according to the mean score plus or minus one standard deviation for a simple slope test. The results showed (Fig. 4) that in the low-HL group (M-1SD), FH had a significant positive predictive effect on PSS (simple slope = 0.0705, 95% CI: 0.0613–0. 0779); in the high-HL group (M + 1SD), the positive predictive effect of FH on PSS was significantly attenuated (simple slope = 0.0494, 95% CI: 0.0397–0.0593), indicating that the positive predictive effect of FH on PSS decreased with increasing individual HL levels. The results showed (Fig. 5) that FH had a significant positive predictive effect on SE in the low-HL group (simple slope = 0.0478, 95% CI: 0.0374–0. 0581); for patients with chronic disease and higher HL, the positive predictive effect of FH on SE was significantly attenuated (simple slope = 0.0342, 95% CI: 0.0225–0.0458), indicating that as individual HL increased, the positive predictive effect of FH on SE decreased (see Table 7).
Fig. 4.
The moderating effect of health literacy on the relationship between family health and perceived social support
Fig. 5.
The moderating effect of health literacy on the direct relationship between family health and self-efficacy
Table 7.
Analysis of the regulatory role of health literacy
| Path | Health literacy(HL) | Effect | Boot SE | 95% CI | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Family Health – Perceived Social support(FH-PSS) | −5.3288 (M-1SD) | 0.0705 | 0.0047 | 0.0613 | 0.0799 |
| 0.0000 (M) | 0.0600 | 0.0039 | 0.0526 | 0.0677 | |
| 5.3388 (M + 1SD) | 0.0494 | 0.0049 | 0.0397 | 0.0593 | |
| Family Health—Self Efficacy(FH-SE) | −5.3288 (M-1SD) | 0.0478 | 0.0053 | 0.0374 | 0.0581 |
| 0.0000 (M) | 0.0410 | 0.0048 | 0.0316 | 0.0503 | |
| 5.3388 (M + 1SD) | 0.0342 | 0.0059 | 0.0225 | 0.0458 | |
Discussion
The study results showed that patients with chronic diseases had an average SE of 8.60, indicating a low SE level. This score was lower than those reported by Ge et al. [52] and Jianrong et al. [57] in their studies on the general population using the same scale. These findings suggest that low SE among chronic patients requires urgent attention and measures by all stakeholders to improve SE. This study found that self-efficacy was lower among women, minors aged 12–17 years, agricultural households, living in countryside, low education level, receiving government assistance and subsidies, single-parent family, low income and low social status patients with chronic illness, which is similar to the findings of previous studies [58, 59]. These characteristics mostly coincide with the socially vulnerable groups, which are often disadvantaged in social development in terms of economic income, competitiveness, social status, rights and interests, etc., and have to bear great material and mental pressure, and there are limitations due to their own cultural, political or their own conditions [60], which make it more difficult to obtain and use adequate and abundant resources compared to other groups. Because of their own economic, cultural, political or other conditions [60], they are less likely than other groups to have access to and use sufficient and abundant resources, have less confidence in themselves to achieve [61, 62], and have a lower sense of self-efficacy. We hope that all sectors of society will pay more attention to chronic disease patients with these characteristics to ensure that their needs are met and that they receive appropriate support in various aspects such as health care and safety.
This study examined the relationship between FH and SE in patients with chronic disease. The results indicated that FH has a significantly positive impact on SE among those living with chronic illnesses. The healthier the family, the greater the SE of patients to control their behaviour, as supported by previous research [18, 63]. Over time, individuals with chronic diseases are more likely to experience negative emotions such as weakness, depression [63], and anxiety [64]. People with chronic illness and their families form strong bonds with each other. Such support may be helpful in building and reinforcing self-confidence, coping with disease, and managing their emotions [65]. Additionally, family plays a crucial role in the adoption and maintenance of health-promoting behaviours as part of the social support system [66]. Consequently, they can enhance patient SE by providing positive social support, including emotional and informational support [67]. It is important to note that self-management is crucial for controlling and managing chronic diseases as it can reduce hospitalisation rates and improve prognosis. SE is a key factor in successful self-management. It thus follows that the construction of a healthy family should be the focus of this study. The improvement of family health is dependent upon the efforts of family members and the participation of the wider society, with the objective of helping patients with chronic diseases to improve their confidence in disease control.
The results showed that after controlling for variables related to individual, family, and basic social characteristics, PSS played a positive mediating role in FH and SE in people with chronic diseases. During treatment, chronic patients receive a high level of social support, which expands their problem-solving pathways and enhances their personal abilities, thereby enhancing their SE [7]. FH promotes the improvement of social support systems for patients with chronic diseases. A good family environment and rich network of family resources can make it easier for patients to access other social resources, thereby improving the level of social support. Previous research has also shown that family cohesion and subjective socioeconomic status are strongly related to social support [68, 69]. In addition, a functioning family, along with good family support, can increase patients' self-confidence, which in turn enhances their SE [21, 22, 70, 71]. This suggests that FH levels affect the level of patients’ PSS, and thus affect SE. High levels of social support and SE can improve patients' quality of life [72–74] and reduce negative emotions such as depression [26]. Therefore, in the process of treatment and management, community health service organizations can develop health intervention plans, such as forming community health support groups and chronic family management groups to help patients establish an effective social support system with family at the core, thereby improving patients’ PSS to increase their SE.
Additional studies have shown that HL plays a crucial role in moderating the relationship among FH, PSS, and SE in chronic patients. As HL levels increased, the positive predictive effects of FH on PSS and SE decreased. The positive relationship between FH and PSS weakened in the HL group. That is, chronic disease patients with high HL have a lower level of FH due to a poor FH lifestyle and a lack of FH resources [75]. This in turn leads to a lower level of PSS [76]. However, higher HL may result in greater health knowledge, correct health cognition and mindset, and higher self-care abilities [77]. Patients with chronic diseases can actively seek health-related help and use resources to deal with difficult situations [78]. HL positively correlates with PSS [79]. Interventions aimed at regulating high HL can improve low PSS scores to some extent [80]. Therefore, PSS scores of patients with chronic diseases may not be as low. HL also moderated the direct effect of FH on SE in chronic patients. As individual HL improved, the positive predictive effect of FH on SE decreased. If a patient with a chronic disease has high HL but poor FH owing to inadequate social and emotional health processes and insufficient external social support, their SE may be low [81]. However, if they have critical HL, they can communicate better [82] and actively use information to improve their situation [15, 83], eventually increasing their SE [84, 85]. Therefore, the SE of patients with chronic diseases may not be as low; in 2022, the HL level of Chinese residents was 27.78% [86], indicating significant room for improvement.
Given this context, along with our results, there is an urgent need to increase the HL levels in patients with chronic diseases and the entire population. In the future, in health strategies at the national level, national public health services should extend their focus from individual health to the larger family context. Especially in China, with the accelerated rate of urbanisation and the aging of the population, family structures are becoming increasingly complex and the social determinants of health are more diverse, which poses a number of challenges to health strategies, and makes it all the more necessary to develop family-centred health promotion strategies, and also to comprehensively take into account the complex characteristics of different families, such as the type of family, the per capita monthly income of the family, the number of children, the social status, and to take into account the development of medical technology At the same time, it is also necessary to take into full consideration the complex characteristics of different families, such as family type, per capita monthly income, number of children, social status, and the development of medical technology, and to take into full consideration the characteristics of the family and its impact on society, so as to formulate a scientific strategy for health promotion and management in accordance with local conditions. For example, healthcare workers should not only provide health education to patients with chronic diseases but also extend HL efforts to include family members. To effectively improve HL in patients with chronic diseases, it is important to situate HL efforts within the context of FH rather than just individual care. This approach aligns with the increasing commitment to shared roles and active family-centred care, and allows patients to manage their health better and ultimately achieve their health promotion goals. At the same time, public health policies and interventions should emphasise the positive impact of family health and health literacy on the self-efficacy of patients with chronic diseases, and establish a better social support network to promote family-based chronic disease management, and gradually build a collaborative management model of “individual-family-community service system” to improve the efficiency of chronic disease management. For example, using family physician contracting services as a means to strengthen communication between medical professionals and patients with chronic diseases and their caregivers, guiding patients and their caregivers to understand relevant knowledge about chronic disease prevention, control and management, and improving the overall health literacy of the family, as well as enhancing patients' self-efficacy and self-management skills. Finally, governments must adopt a more comprehensive view of the health system in order to support this strategy, concentrating on issues such as the distribution of healthcare resources, the ability of medical professionals to communicate, and institutional elements that encourage patients and their families to actively participate in their care. Governments ought to focus more on creating more all-encompassing interventions, training medical staff to carry them out, educating and preparing the public, and constructing a public health infrastructure and healthcare system that supports and enables this shift.
This study has some limitations. First, the cross-sectional design used limited the establishment of a causal relationship between FH and SE. Future studies should use longitudinal designs to determine the direction of these associations. Second, as information was collected from the study participants, there may have been reporting bias, social desirability bias and recall bias, which could have affected the accuracy and reliability of the findings. Future research could include objective measures or ecological momentary assessment(EMA) to validate the accuracy and reliability of self-reported data. Third, this study focused solely on the mediating role of PSS and moderating role of HL, disregarding other potential mechanisms between FH and SE in individuals with chronic illnesses. Future research should investigate additional individual, family, social, and other factors that are beyond the scope of this study. Finally, statistical significance may be overestimated due to large sample sizes, which may have some impact on the actual significance of the results. Statistical significance does not necessarily imply that the results are of equal importance or impact in practice, and it is recommended that when reporting statistical results, future researchers should not assess the practical significance of the results based on statistical significance alone, but should combine it with effect sizes to understand the value of the research findings in practice.
Conclusions
In a context where chronic diseases have become one of the global health challenges, more attention should be paid to improving the SE of the chronically ill population. Our results not only facilitate the understanding of the relationship mechanisms between FH and SE in chronic patients but can also serve as a guide for healthcare workers and policymakers who wish to provide better care for patients. To support this, the government can formulate a series of measures to improve the self-efficacy of patients with chronic diseases; improve the family health of patients by focusing on the construction of a healthy family environment and adherence to family values; and at the same time, establish a family-centred and effective social support system to improve the external social support network of patients. Medical workers can extend the health literacy work from the patient’s personal care relationship to the improvement of family health, to more effectively improve the health literacy of the chronic disease population. This will result in managing self-health better, and ultimately, in achieving the purpose of health promotion.
Acknowledgements
The authors would like to thank all those who generously allocated their time to this study. We would also like to thank Editage (www.editage.cn) for English language editing.
Abbreviations
- FH
Family health
- SE
Self-efficacy
- PSS
Perceived social support
- HL
Health literacy
- NGESES-SF
General Self-Efficacy Scale-Short Form
- HLS-SF12
Health Literacy Questionnaire-Short Form 12
- PSSS-SF
Perceived Social Support Scale-Short Form
- FHS-SF
Family Health Scale-Short Form
Authors' contributions
Conceived and designed the research: K.L., AQ.C., YC.Q., and ZN.L. Manuscript drafting: K.L., AQ.C., YC.Q., and XX.Y. Conceptualization: AQ.C. and WZ.L. Methodology: YC.Q. and JH.L. Data Analysis: K.L. Manuscript Editing: ZN.L and JY.C. Resources: ZN.L., YB.W. and JY.C.
Funding
This project received support from Guangzhou Public Health Service System Construction Research Foundation (Grant No. 2021–2023), the Characteristic New Think Tank of university in Guangdong Province (Grant No. 2024TSZK016), the Social Science Key Laboratory of Guangdong Higher Education Institutes for Health Governance Based on Big Data Utilization (Grant No. 2023WSY007), the Health Economics Association of Guangdong Province (Grant No. 2023-WJMZ-51) and the Accredited Scientiffc Research Project (Featured Innovation Project) of Universities in Guangdong Province (grant number 2021WTSCX072).
Data availability
Data are available, upon reasonable request, by e-mailing: wuyibo@bjmu.edu.cn.
Declarations
Ethics approval and consent to participate
An ethical review (JKWH-2022–02) of the study protocol has been published in Psychosomatic Medicine Research. Before completing the questionnaire, each participant voluntarily participated and provided informed consent. Informed consent for minors was provided by a parent or legal guardian.To protect the privacy of the participants, data were collected and analysed anonymously. The researchers received ethical approval from the Shaanxi Academy of International Trade and Commerce (JKWH-2022–02) to treat the results of the study fairly and equally, independent of the characteristics of the participants, and to take measures in the data analysis and interpretation of the results to ensure that no discriminatory conclusions were drawn.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhen-ni Luo and Kun Li these authors contributed equally to this work.
References
- 1.National Health Commission of the People's Republic of China. China health statistics yearbook. Beijing: Peking Union Medical College Press; 2020.
- 2.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. [DOI] [PubMed] [Google Scholar]
- 3.Baljani E, Rahimi J, Amanpour E, Salimi S, Parkhashjoo M. Effects of a nursing intervention on improving self-efficacy and reducing cardiovascular risk factors in patients with cardiovascular diseases. J Hayat. 2011;17:45–54. [Google Scholar]
- 4.Han K, Lee P, Lee S, Park E. Factors influencing quality of life in people with chronic illness in Korea. J Nurs Scholarsh. 2003;35:139–44. [DOI] [PubMed] [Google Scholar]
- 5.Afendy A, Kallman JB, Stepanova M, Younoszai Z, Aquino RD, Bianchi G, et al. Predictors of health-related quality of life in patients with chronic liver disease. Aliment Pharmacol Ther. 2009;30:469–76. [DOI] [PubMed] [Google Scholar]
- 6.Peters M, Potter CM, Kelly L, Fitzpatrick R. Self-efficacy and health-related quality of life: a cross-sectional study of primary care patients with multi-morbidity. Health Qual Life Outcomes. 2019;17:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chu HH, Lee KS, Ho Lee K, Chung JH, Shin KC, Hwang TY. Association of physical and psychological health status between chronic obstructive pulmonary disease patients and their family caregivers. Health Care Women Int. 2019;40:1019–30. [DOI] [PubMed] [Google Scholar]
- 8.Chae YR, Lee SH, Jo YM, Kang HY. Factors related to family support for hemodialysis patients: A systematic review and meta-analysis. Korean J Adult Nurs. 2019;31:123–35. [Google Scholar]
- 9.Kim O, Yeom EY, Jeon HO. Relationships between depression, family function, physical symptoms, and illness uncertainty in female patients with chronic kidney disease. Nurs Health Sci. 2020;22:548–56. [DOI] [PubMed] [Google Scholar]
- 10.Alizadeh F, Addepalli A, Chaudhuri SR, Budongo AM, Owembabazi I, Chaw GF, et al. Family health sheets: a vital instrument for village health workers providing comprehensive healthcare. BMC Health Serv Res. 2021;21:1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiss-Laxer NS, Crandall A, Okano L, Riley AW. Building a Foundation for Family Health Measurement in National Surveys: A Modified Delphi Expert Process. Matern Child Health J. 2020;24:259–66. [DOI] [PubMed] [Google Scholar]
- 12.Haomiao L, Ju S, Qiang Y, Yibo W. Family health: concept, measurement, and current situation in China (in Chinese). Res Health Policy China. 2022;15:1–7. [Google Scholar]
- 13.Hsiao FH, Klimidis S, Minas H, Tan ES. Cultural attribution of mental health suffering in Chinese societies: the views of Chinese patients with mental illness and their caregivers. J Clin Nurs. 2006;15(8):998–1006. [DOI] [PubMed] [Google Scholar]
- 14.Ying L. Cross cultural comparative study of health concepts between China and the West (in Chinese)[D]. Hei Longjiang: Harbin University of Science and Technology; 2015. [Google Scholar]
- 15.Haomiao L, Yibo W, Ju S, Qiang Y. Family health and chronic disease control: the mediating role of health literacy, health behavior, and trust in grassroots services (in Chinese). Popul Dev. 2023;29:145–60. [Google Scholar]
- 16.Coffman MJ. Effects of tangible social support and depression on diabetes self-efficacy. J Gerontol Nurs. 2008;34(4):32–9. [DOI] [PubMed] [Google Scholar]
- 17.Bahari G, Scafide K, Krall J, Mallinson RK, Weinstein AA. Mediating role of self-efficacy in the relationship between family social support and hypertension self-care behaviours: A cross-sectional study of Saudi men with hypertension. Int J Nurs Pract. 2019;25(6):e12785. [DOI] [PubMed] [Google Scholar]
- 18.Zakiei A, Norouzi E, Ghasemi SR, Komasi S, Rostampour M, Khazaie H. Controlling risky behavior associated with AIDS: the role of social support, family functioning, self-efficacy and AIDS risk perception. BMC Psychol. 2022;10:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chang C-W, Chen F-P. Family social networks and personal recovery among Chinese people with mental illness in Hong Kong: The mediating effects of self-esteem and self-efficacy. Psychiatr Rehabil J. 2020;45(3):247–54. [DOI] [PubMed] [Google Scholar]
- 20.Wensu Z, Xidi Z, Shaojie L, Baohua Z, Yunhan Y, Huilan X, et al. Does the presence of anxiety and depression symptoms mediate the association between family functions and self-efficacy in pregnant women in the third trimester?: a community-based cross-sectional survey. Front Psychiatry. 2021;12: 726093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Puspasari J, Nur Rachmawati IN, Budiati T. Family support and maternal self-efficacy of adolescent mothers. Enfirm Clin. 2018;28:227–31. [Google Scholar]
- 22.Mei YX, Xiang DD, Zhang ZX, Twumwaah Budu J, Lin BL, Chen SY. Family function, self-efficacy, care hours per day, closeness and benefit finding among stroke caregivers in China: A moderated mediation model. J Clin Nurs. 2023;32:506–16. [DOI] [PubMed] [Google Scholar]
- 23.Mahmoudi A. Effect of self-esteem and self-efficacy in family dynamics. Proc Soc Behav Sci. 2012;46:53–6. [Google Scholar]
- 24.Hemati Z, Abbasi S, Oujian P, Kiani D. Relationship between parental communication patterns and self-efficacy in adolescents with parental substance abuse. Iran J Child Neurol. 2020;14:49–56. [PMC free article] [PubMed] [Google Scholar]
- 25.Shamali M, Konradsen H, Stas L, Østergaard B. Dyadic effects of perceived social support on family health and family functioning in patients with heart failure and their nearest relatives: using the Actor-Partner Interdependence Mediation Model. PLoS ONE. 2019;14:e0217970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Iovino P, Nolan A, De Maria M, Ausili D, Matarese M, Vellone E, et al. The influence of social support on self-care is mediated by self-efficacy and depression in chronic illness: key findings from the ‘SODALITY’ observational study. Aging Ment Health. 2023;27:820–8. [DOI] [PubMed] [Google Scholar]
- 27.Gurbuz IZ, Akin S. Relationship between quality of life, self-efficacy and social support in patients with multiple sclerosis. Int J Palliat Nurs. 2023;29:598–612. [DOI] [PubMed] [Google Scholar]
- 28.Safi F, Areshtanab HN, Ghafourifard M, Ebrahimi H. The association between self-efficacy, perceived social support, and family resilience in patients undergoing hemodialysis: a cross-sectional study. BMC Nephrol. 2024;25(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hacihasanoglu Asilar R, Yildirim A, Saglam R, Demirturk Selcuk E, Erduran Y, Sarihan O. The effect of loneliness and perceived social support on medication adherence self-efficacy in hypertensive patients: an example of Turkey. J Vasc Nurs. 2020;38:183–90. [DOI] [PubMed] [Google Scholar]
- 30.Benson PR. The longitudinal effects of network characteristics on the mental health of mothers of children with ASD: the mediating role of parent cognitions. J Autism Dev Disord. 2016;46:1699–715. [DOI] [PubMed] [Google Scholar]
- 31.Saleh OA, Halperin O, Baron-Epel O. Predictors of maternal self-efficacy and the mediating role of postpartum fatigue for Jewish and Arab women in Northern Israel. Midwifery. 2022;107: 103281. [DOI] [PubMed] [Google Scholar]
- 32.Fierloos IN, Windhorst DA, Fang Y, Hosman CMH, Jonkman H, Crone MR, et al. The association between perceived social support and parenting self-efficacy among parents of children aged 0–8 years. BMC Public Health. 2023;23(1):1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berkman ND, Davis TC, McCormack L. Health literacy: what is it? J Health Commun. 2010;15(Suppl 2):9–19. [DOI] [PubMed] [Google Scholar]
- 34.Duong TV, Aringazina A, Kayupova G, Nurjanah Pham TV, Pham KM, Truong TQ, et al. Development and validation of a new short-form health literacy instrument (HLS-SF12) for the general public in six Asian countries. Health Lit Res Pract. 2019. 10.3928/24748307-20190225-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu W, Yang W, Qian S. The mediating effect of self-efficacy on health literacy and social support in young and middle-aged patients with coronary heart disease after PCI. Vasc Health Risk Manag. 2023;19:341–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Suarilah I, Lin CC. Factors influencing self-management among Indonesian patients with early-stage chronic kidney disease: a cross-sectional study. J Clin Nurs. 2022;31:703–15. [DOI] [PubMed] [Google Scholar]
- 37.Shiyanbola OO, Unni E, Huang Y-M, Lanier C. The association of health literacy with illness perceptions, medication beliefs, and medication adherence among individuals with type 2 diabetes. Res Social Adm Pharm. 2018;14:824–30. [DOI] [PubMed] [Google Scholar]
- 38.Ishikawa H, Kiuchi T. Association of health literacy levels between family members. Front Public Health. 2019;7:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nasiri S, Heydari N, Rafiee S, Paran M. Effect of family centered education on Patient’s self-care. Sadra Med J. 2020;8:311–20. [Google Scholar]
- 40.Ong-Artborirak P, Seangpraw K, Boonyathee S, Auttama N, Winaiprasert P. Health literacy, self-efficacy, self-care behaviors, and glycemic control among older adults with type 2 diabetes mellitus: a cross-sectional study in Thai communities. BMC Geriatr. 2023;23:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pelikan JM, Ganahl K, Roethlin F. Health literacy as a determinant, mediator and/or moderator of health: empirical models using the European Health Literacy Survey dataset. Glob Health Promot. 2018;25(4):57–66. [DOI] [PubMed] [Google Scholar]
- 42.Fang S, Mushtaque I. The Moderating Role of Health Literacy and Health Promoting Behavior in the Relationship Among Health Anxiety, Emotional Regulation, and Cyberchondria. Psychol Res Behav Manag. 2024;17:51–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ni H, Lin Y, Peng Y, Li S, Huang X, Chen L. Relationship Between Family Functioning and Medication Adherence in Chinese Patients With Mechanical Heart Valve Replacement: A Moderated Mediation Model. Front Pharmacol. 2022;13: 817406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hollister-Wagner GH, Foshee VA, Jackson C. Adolescent aggression: models of resiliency 1. J Applied Social Pyschol. 2021;31:445–66. [Google Scholar]
- 45.Wang YJ, Kaierdebieke A, Fan SY, Zhang RF, Huang MJ, Li H, et al. Study protocol: a cross-sectional study on psychology and behavior investigation of Chinese residents. PBICR Psychosom Med Res. 2022;4:19. [Google Scholar]
- 46.Yang Y, Fan S, Chen W, Wu Y. Broader Open Data Needed in Psychiatry: Practice from the Psychology and Behavior Investigation of Chinese Residents. Alpha Psychiatry. 2024;25(4):564–5. https://doi.org/10.5152/alphapsychiatry.2024.241804. Published 2024 Aug 1. [DOI] [PMC free article] [PubMed]
- 47.Wu Y, Fan S, Liu D, Sun X. Psychology and Behavior Investigation of Chinese Residents: Concepts, Practices and Prospects[J]. Chinese General Practice. 2024;27(25):3069–75. 10.12114/j.issn.1007-9572.2024.0075. [Google Scholar]
- 48.Crandall A, Weiss-Laxer NS, Broadbent E, Holmes EK, Magnusson BM, Okano L, et al. The family health scale: reliability and validity of a short- and long-form. Front Public Health. 2020;8: 587125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen G, Gully SM, Eden D. Validation of a new general self-efficacy scale. Organ Res Methods. 2001;4:62–83. [Google Scholar]
- 50.Feng X, Chen XY. Reliability and Validity of New General Self-efficacy Scale (NGSSE)[J]. J Mudanjiang Normal Univ (Philosophy Social Sciences Edition). 2012;4:127–9. [Google Scholar]
- 51.Wang F, Chen K, Du Z, Wu Y, Tang J, Sun X, et al. Reliability and validity analysis and Mokken model of New General Self-Efficacy Scale-Short Form. 2022; 10.13140/RG.2.2.23191.04006.
- 52.Ge P, Li Q, Dong M, Niu Y, Han X, Xiong P, et al. Self-medication in Chinese residents and the related factors of whether or not they would take suggestions from medical staff as an important consideration during self-medication. Front Public Health. 2022;10:1074559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Health promotion glossary of terms. Geneva: World Health Organization; 2021. Licence: CC BY-NC-SA 3.0IGO.
- 54.HLS-EU Consortium Comparative Report of Health Literacy in Eight EU Member States. The European Health Literacy Project 2009–2012. http://cpme.dyndns.org:591/adopted/2015/Comparative_report_on_health_literacy_in_eight_EU_member_states.pdf. Accessed 15 Aug 2021.
- 55.Ferreira WA, Camelo L, Viana MC, Giatti L, Barreto SM. Is subjective social status a summary of life-course socioeconomic position? Cad Saude Publica. 2018;34(5): e00024317. [DOI] [PubMed] [Google Scholar]
- 56.Ross CE, Mirowsky J. Age and the gender gap in the sense of personal control. Soc Psychol Q. 2002;65(2):125–45. [Google Scholar]
- 57.Jianrong M, Lina L, Ling Z, Yibo W, Xinying S. Effects of self-efficacy on health literacy among Chinese residents. China Health Educ (in Chinese). 2022;38:579–82+588.
- 58.Bartlett SJ, Lambert SD, McCusker J, Yaffe M, de Raad M, Belzile E, et al. Self-management across chronic diseases: Targeting education and support needs. Patient Educ Couns. 2020;103(2):398–404. [DOI] [PubMed] [Google Scholar]
- 59.García-Ovejero E, Pisano-González M, Salcedo-Diego I, Serrano-Gallardo P. Impact of Chronic Disease Self-Management Program on the Self-Perceived Health of People in Areas of Social Vulnerability in Asturias, Spain. Healthcare (Basel). 2024;12(8):811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Munari SC, Wilson AN, Blow NJ, Homer CSE, Ward JE. Rethinking the use of “vulnerable.” Aust N Z J Public Health. 2021;45(3):197–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mace Firebaugh C, Wojtyna A, Rich D, Beeson T. Examining self-efficacy and COVID-19 disease prevention behaviors among socially vulnerable populations. J Community Psychol. 2023;51(3):1427–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dzerounian J, Pirrie M, AlShenaiber L, Angeles R, Marzanek F, Agarwal G. Health knowledge and self-efficacy to make health behaviour changes: a survey of older adults living in Ontario social housing. BMC Geriatr. 2022;22(1):473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cui Y, Zhao QP, Zhang XY, Zhu JY, Wang FL, Zhang P. The relationship between frailty and depression in middle-aged and elderly people with chronic diseases: the chain mediating effect of perceived social support and resilience. [J] Nurse Continuing Educ. 2024;39(03):236–40.
- 64.Liqin Z, Zhiquan X, Li Y, Lanfang Z, Cailian R. Cognitive function status and its relationship with frailty in hospitalized elderly patients with comorbidities of chronic diseases (in Chinese). Guangdong Med J. 2023;44:1061–6. [Google Scholar]
- 65.Yuan Y, Xu HW, Zhang S, Wang Y, Kitayama A, Takashi E, et al. The mediating effect of self-efficacy on the relationship between family functioning and quality of life among elders with chronic diseases. Nurs Open. 2021;8:3566–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cene CW, Haymore B, Dolon-Soto DR, Lin FC, Pignone M, DeWalt D, et al. Perceived social support operates through self-efficacy to positively influence heart failure self care management. Circulation. 2011;124(21 Suppl 1):A18299. [Google Scholar]
- 67.Kline KS, Scott LD, Britton AS. The use of supportive-educative and mutual goal-setting strategies to improve self-management for patients with heart failure. Home Healthc Nurse. 2007;25:502–10. [DOI] [PubMed] [Google Scholar]
- 68.Wu S, Zheng X. The effect of family adaptation and cohesion on the well-being of married women: A multiple mediation effect. J Gen Psychol. 2020;147:90–107. [DOI] [PubMed] [Google Scholar]
- 69.Yan W, Zhang L, Li W, You X, Kong F. Associations of family subjective socioeconomic status with hedonic and eudaimonic well-being in emerging adulthood: A daily diary study. Soc Sci Med. 2022;298: 114867. [DOI] [PubMed] [Google Scholar]
- 70.Konradsen H, Dieperink KB, Lauridsen J, Sorknaes AD, Ostergaard B. Validity and reliability of the Danish version of the ice expressive family functioning and ice family perceived support questionnaires. Scand J Caring Sci. 2018;32:1447–57. [DOI] [PubMed] [Google Scholar]
- 71.Wu F, Sheng Y. Social support network, social support, self-efficacy, health-promoting behavior and healthy aging among older adults: a pathway analysis. Arch Gerontol Geriatr. 2019;85: 103934. [DOI] [PubMed] [Google Scholar]
- 72.Feng Z, Cramm JM, Nieboer AP. Social participation is an important health behaviour for health and quality of life among chronically ill older Chinese people. BMC Geriatr. 2020;20:299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ayalon R, Bachner YG. Medical, social, and personal factors as correlates of quality of life among older cancer patients with permanent stoma. Eur J Oncol Nurs. 2019;38:50–6. [DOI] [PubMed] [Google Scholar]
- 74.Lara R, Vázquez ML, Ogallar A, Godoy-Izquierdo D. Psychosocial resources for hedonic balance, life satisfaction and happiness in the elderly: a path analysis. Int J Environ Res Public Health. 2020;17:56–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang F, Wu Y, Sun X, Wang D, Ming WK, Sun X, et al. Reliability and validity of the Chinese version of a short form of the family health scale. BMC Prim Care. 2022;23:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lima-Rodríguez JS, Domínguez-Sánchez I, Lima-Serrano MM. Family and social variables associated with family health. West J Nurs Res. 2022;44:920–31. [DOI] [PubMed] [Google Scholar]
- 77.Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. J Gen Intern Med. 2006;21:806–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.White S, Chen J, Atchison R. Relationship of preventive health practices and health literacy: a national study. Am J Health Behav. 2008;32:227–42. [DOI] [PubMed] [Google Scholar]
- 79.Kobayashi R, Ishizaki M. Relationship between health literacy and social support and the quality of life in patients with cancer: questionnaire study. J Particip Med. 2020;12: e17163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lee SD, Arozullah AM, Cho YI, Crittenden K, Vicencio D. Health literacy, social support, and health status among older adults. Educ Gerontol. 2009;35:191–201. [Google Scholar]
- 81.Zakiei A, Vafapoor H, Alikhani M, Farnia V, Radmehr F. The relationship between family function and personality traits with general self-efficacy (parallel samples studies). BMC Psychol. 2020;8:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Inoue M, Takahashi M, Kai I. Impact of communicative and critical health literacy on understanding of diabetes care and self-efficacy in diabetes management: a cross-sectional study of primary care in Japan. BMC Fam Pract. 2013;14:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ishikawa H, Takeuchi T, Yano E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care. 2008;31:874–9. [DOI] [PubMed] [Google Scholar]
- 84.Maleki Chollou K, Gaffari-Fam S, Babazadeh T, Daemi A, Bahadori A, Heidari S. The association of health literacy level with self-care behaviors and glycemic control in a low education population with type 2 diabetes mellitus: a cross-sectional study in Iran. Diabetes Metab Syndr Obes. 2020;13:1685–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lee YJ, Shin SJ, Wang RH, Lin KD, Lee YL, Wang YH. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ Couns. 2016;99:287–94. [DOI] [PubMed] [Google Scholar]
- 86.China.gov. Health Literacy Level of the Nation's Residents to Reach. 2023. https://www.gov.cn/govweb/lianbo/bumen/202308/content_6899405.htm. Accessed 22 Feb 2024.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available, upon reasonable request, by e-mailing: wuyibo@bjmu.edu.cn.