Abstract
Purpose:
To compare the analgesic efficacy of orally administered Curcuma longa (curcumin) and mefenamic acid (MA) after surgical periodontal therapy (SPT).
Materials and Methods:
Seventy-six periodontitis patients were randomly divided into two groups. In the test group, patients received curcumin capsules (200 mg), and in the control group, patients received MA (500 mg). All patients underwent post-operative antibiotic therapy using 500 mg amoxicillin and 400 mg metronidazole for 7 days. Post-operative pain and discomfort were evaluated using the numerical rating scale (NRS) and verbal rating scale (VRS), respectively. Evaluation were performed after 24 (T1), 48 (T2), and 72 h (T3). Group comparisons were done using Student’s t-test and the Mann-Whitney U-test. The level of statistical significance was established at p < 0.05.
Results:
All patients had stage 3/grade C periodontitis. The mean age of individuals in the test and control groups were 58.4 ± 7.3 and 57.2 ± 5.2 years, respectively. A family history of periodontal diseases was reported by 37.5% and 47.4% individuals in the test and control groups, respectively. In the test and control groups, the total mean duration of periodontal surgery was 168.2 ± 12.2 and 173.4 ± 10.7 min, respectively. There was no statistically significant difference in the mean NRS and VRS scores among patients in the test and control groups. In both groups, there was no statistically significant difference in the change in NRS scores at any time point.
Conclusions:
Compared with MA, curcumin is ineffective for pain and discomfort management after SPT. The possibility of the results being biased due to lack of operator blinding cannot be overlooked.
Key words: curcumin, mefenamic acid, pain, periodontal flap surgery
Post-operative pain after oral surgical interventions such as tooth extraction and periodontal flap procedures is often disquieting for patients.33,34 Traditionally, non-steroidal anti-inflammatory drugs (NSAIDs) such as diclofenac, mefenamic acid (MA), acetyl salicylic acid and propionic acid derivatives are prescribed to patients for the management of post-operative pain.16,20 The NSAIDs inhibit cyclooxygenase-2 (COX-2), thereby blocking production of prostaglandins,12 and are beneficial for the management of mild to moderate levels of pain.18 However, the analgesic efficacy of NSAIDs is often compromised in patients experiencing severe pain.44 The NSAIDs should not be prescribed to patients using anticoagulants such as warfarin and clopidogrel,7 and their potential side-effects include gastrointestinal- and hepatotoxicity.7,9 The global use of herbal medications for pain relief has increased over the years;2,30,41 their consumers often perceive that medications derived from medicinal plants are safe and have no undesirable side-effects compared with synthetic pharmacological drugs.6,29
Curcumin is an organic polyphenol present in the roots of Curcuma species, such as turmeric.3 It adjusts the inflammatory response by down-regulating the activity of lipoxygenase and COX-2. Moreover, curcumin retards the production of inflammatory cytokines such as interleukin (IL)-1, IL-6, IL-12 and tumor necrosis factor-alpha (TNF-α).28 It has also been reported that curcumin is a potent anti-oxidant and anti-inflammatory agent,35 and is claimed to relieve pain, e.g. arthritis, burn pain and neuropathic pain.43 In a randomised controlled clinical trial, the effectiveness of curcumin (test group) was compared with MA (control group) for managing post-operative pain after surgical extraction of impacted third molars.33 In that study, self-perceived post-operative pain was assessed using the numerical rating scale (NRS). The results showed that although patients in both groups perceived less pain than baseline pain levels, individuals in the test group perceived significantly less post-operative pain compared with the control group. The authors concluded that curcumin is useful in the management of pain following surgical extraction of impacted wisdom teeth.33 A limited number of clinical studies have assessed the analgesic efficacy of a curcumin-based gel following periodontal flap surgical procedures.5,34 Their results showed that curcumin-containing mucoadhesive films are useful in reducing postoperative pain and swelling following periodontal surgical interventions.5,34 A thorough review of the relevant literature yielded no studies which compared the analgesic efficacy of orally administered Curcuma longa (curcumin) and MA after surgical periodontal therapy (SPT). Thus, the aim of this study was to compare the analgesic efficacy of curcumin and MA after SPT. The authors hypothesise that compared with MA, curcumin is not effective for pain management after SPT.
Materials and Methods
Ethics Statement
The present study was performed following guidelines recognized by the Declaration of Helsinki as revised in 2013 for experimentation involving human patients. All volunteer participants were requested to read and sign a consent form written in simple English and Arabic. All participants were informed that they could withdraw at any phase of the study without consequences. Ethical approval was obtained from the research ethics committee of the Centre for Specialist Dental Practice and Clinical Research (UDCRC/025-16).
Eligibility Criteria
Patients with periodontitis were included. Self-reported smokers,25 habitual consumers of alcohol19 and patients with systemic illnesses, including but not limited to self-reported oral and systemic cancer, HIV/AIDS, diabetes mellitus (DM), prediabetes, hepatic and renal diseases, and cardiovascular diseases, were excluded.8,22,27,39 Moreover, overweight and obese individuals, pregnant and/or lactating females, and patients who had consumed probiotics, corticosteroids/steroids, or bisphosphonates within the past 90 days were excluded. Likewise, subjects who were undergoing dental prophylaxis or any form of oral or craniofacial surgery were also eliminated.
Preoperative Staging and Grading of Periodontitis
Patients diagnosed with periodontitis were included. Periodontitis was defined using the following parameters: horizontal marginal bone loss (MBL), probing depth (PD) of ≥ 4 mm, and clinical attachment loss (AL) of at least 1–2 mm.38 Pre-operative patient records were evaluated to determine the staging and grading of periodontitis by one trained investigator (Kappa 0.89).
Design, Randomisation, and Allocation Concealment
A parallel-arm trial design as described elsewhere37 was applied in the current investigation. For randomisation, a computer program (www.random.org, Randomness and Integrity Services; Dublin, Ireland) was used, and allocation to the study-groups was done via block randomisation.11
Surgical Procedure
All surgical procedures were performed in one session by a trained and experienced periodontist. Under local anesthesia, all patients underwent full-mouth dental prophylaxis using an ultrasonic hand scaler (Woodpecker Uds-J Ultrasonic Scaler, EMS Compatible Original; Guangzhou, China). In both arches, gingival sulcular incisions were maed around the affected teeth using a sterile No. 15 surgical blade (iSmile Dental Products, Prehma #15 sterile stainless steel surgical scalpel blade; Sacramento, CA, USA), and buccal and lingual/palatal flaps were elevated using sterile periosteal elevators (Syze UK, DS-1004; London, UK) as described elsewhere.14 Mechanical curettage of teeth and root surfaces was performed using sterile curettes (Hu-Friedy; Chicago, IL, USA) to remove subgingival plaque, calculus, diseased granulation tissue and pocket epithelium. The flaps were repositioned and sutured using 3-0 interrupted sutures (Unify PGA Surgical Sutures, Henry Schein; Berlin, Germany). The duration of the surgical intervention was also retrieved from patients’ dental records.
Grouping
The principal investigator communicated with participants of the assigned treatment group. Post-operatively, participants were divided into 2 groups. 1. Test group: patients received curcumin capsules (200 mg) (Terry Natural Products, CuraMed; Green Bay, WI, USA); 2. control group: patients received one tablet of MA (500 mg). In both groups, participants were prescribed antibiotics (amoxicillin 500 mg and metronidazole 400 mg) 3x daily (every 8 h) for 7 days. In the present trial, the dosage of curcumin was based on results from previous reviews.15,28 The participants in the test and control groups were advised to orally take 1 MA tablet and 2 curcumin capsules, respectively, immediately after the procedure and then every 8 h for 3 days. After the third day, participants in the test and control groups were advised to take the respective analgesics as needed for pain.
Questionnaire, Evaluation of Post-operative Pain and Discomfort Scores, Blinding
A standardised questionnaire was given to all participants to collect information regarding age, gender, family history of periodontal diseases, drug allergies, and intensity of post-operative pain. The questionnaire was administered to all participants by a trained investigator (SM). In both groups, evaluation of post-operative pain was performed using the numerical rating scale (NRS) and discomfort using a 4-point verbal rating scale (VRS) (1 = none; 2 = mild; 3 = moderate; 4 = severe).5,42 Three pain evaluations were performed by phone calls with the patients after 24 (T1), 48 (T2), and 72 h post-operatively. This procedure was performed by one trained and calibrated investigator (Kappa 0.92) who was blinded to the study groups.
Statistical Analysis
Statistical analysis was conducted using a software program (SPSS v.18, IBM; Chicago, IL, USA). Group comparisons were performed using Student’s t-test and the Mann-Whitney U-test. Power analysis was calculated based on results obtained from a pilot investigation using a software program (G*Power version 3.1.5., University of Kiel; Kiel, Germany). A t-test of independent means (test and control groups) was set as the statistical test to perform power analysis using an effect size of 1 and alpha of 5%. Bonferroni’s post-hoc adjustment was used for multiple comparisons. It was estimated that inclusion of at least 38 individuals per group was necessary to attain a study power of 91.5%. p-values below 0.05 were considere statistically significant.
Results
Recruitment of Study Participants
Ninety-one individuals were initially invited to the present study. Fifteen individuals (11 females and 4 males) refused to participate in the present study. These individuals (n = 15) refused to sign the written informed consent form. In total, 76 individuals (38 per group) were included (Fig 1).
Fig 1.
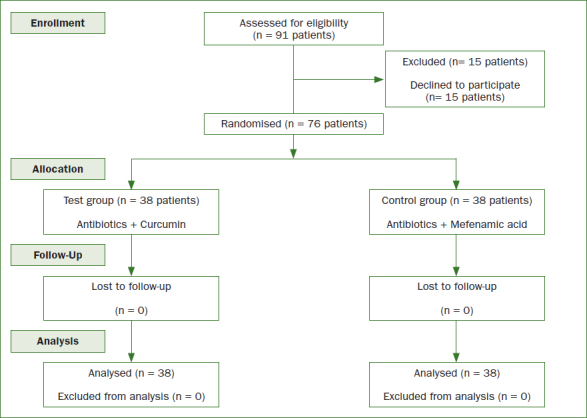
CONSORT flow diagram for patient recruitment.
Characteristics of the Study Cohort
In the test and control groups, 26 and 28 individuals, respectively, were males. The mean ages of individuals in the test group was 58.4 ± 7.3 and 57.2 ± 5.2 years in the control group. There was no statistically significant difference in the mean age of males and females in the test and control groups. A family history of periodontal diseases was reported by 37.5% in the test group and 47.4% in the control group. None of the patients reported drug allergies (Table 1). There was no statistically significant difference in the preoperative periodontal inflammatory parameters in both groups (Table 1). As per the periodontal diagnostic records, all patients had stage 3/grade C periodontitis. In the test and control groups, the total mean duration of periodontal surgery was 168.2 ± 12.2 min in the test group and 173.4 ± 10.7 min in the control group. None of the participants in the test and control group reported allergic reactions or complications associated with their prescription medication.
Table 1.
Characteristics of the study groups
| Parameters | Test group | Control group |
|---|---|---|
| Number of patients | 38 | 38 |
| Gender (male:female) | 26:12 | 28:10 |
| Age in years (all patients) | 58.4 ± 7.3 years | 57.2 ± 5.2 years |
| Age of males in years | 61.2 ± 4.3 years | 62.4 ± 5.1 years |
| Age of females in years | 56.1 ± 2.9 years | 55.7 ± 4.1 years |
| Periodontal parameters | ||
| Plaque index | 2.7 ± 0.3 | 2.8 ± 0.2 |
| Gingival index | 3.02 ± 0.2 | 2.9 ± 0.05 |
| Probing depth | 4.2 ± 0.07 mm | 4.3 ± 0.02 mm |
| Clinical attachment loss | 6.1 ± 0.2 mm | 5.9 ± 0.03 mm |
| Marginal bone loss (mesial surface) | 4.7 ± 0.06 mm | 4.6 ± 0.03 mm |
| Marginal bone loss (distal surface) | 4.6 ± 0.04 mm | 4.5 ± 0.05 mm |
| Number of missing teeth | 16.2 ± 2.5 teeth | 16.6 ± 1.6 teeth |
| Family history of periodontal diseases | ||
| Yes | 15 (37.5%) | 18 (47.4%) |
| No | 5 (13.2%) | 10 (26.3%) |
| I don’t know | 15 (49.3%) | 10 (26.3%) |
| Allergies to antibiotics (penicillin) | None | None |
| Allergies to NSAIDs | None | None |
NSAIDs: non-steroidal anti-inflammatory drugs.
Numerical Rating Scale and Verbal Rating Scale Scores
The mean NRS and VRS scores assessed at different post-operative time points (T1, T2 and T3) were comparable (p > 0.05) among patients in the test and control groups (Figs 2a and 2b). There was no statistically significant difference in the mean NRS and VRS scores assessed at the 3 different post-operative time points among males and females in either group (data not shown).
Fig 2.
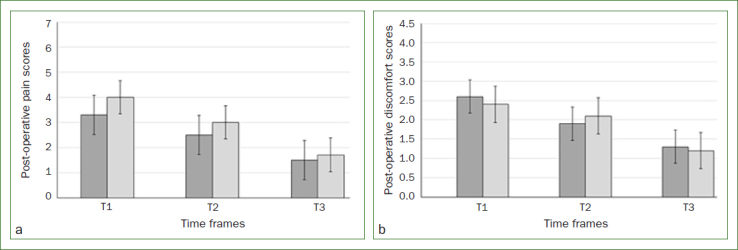
a. Mean numerical rating scale scores in the test (dark grey bars) and control groups (light grey bars) after 24 h (T1), 48 h (T2) and 72 h (T3); b. Mean verbal rating scores in the test (dark grey bars) and control groups (light grey bars) after 24 h (T1), 48 h (T2) and 72 h (T3).
Change in Numerical Rating Scale and Verbal Rating Scale Scores at Different Time Intervals
In the test and control groups, there was no statistically significant change in the NRS scores assessed at the 3 different post-operative time points (Tables 2 and 3). There was no statistically significant difference in the change in mean NRS and VRS scores assessed at any of the post-operative time points among males and females in either group (data not shown).
Table 2.
Comparison of change in numerical rating scale scores in the test and control groups at different time intervals
| Time interval | Groups | Change in mean NRS score | p-value |
|---|---|---|---|
| T1 vs T2 | Test group | 0.8 | 0.13 |
| Control group | 1 | ||
| T1 vs T3 | Test group | 1.8 | 0.06 |
| Control group | 2.3 | ||
| T2 vs T3 | Test group | 1 | 0.15 |
| Control group | 1.3 |
NRS: numerical rating scale; T1: 24 h after periodontal surgery; T2: 48 h after periodontal surgery; T3: 72 h after periodontal surgery.
Table 3.
Comparison of change in verbal rating scale scores in the test and control groups at different time intervals
| Time interval | Groups | Change in mean VRS score | p-value |
|---|---|---|---|
| T1 vs T2 | Test group | 0.7 | 0.15 |
| Control group | 0.3 | ||
| T1 vs T3 | Test group | 1.3 | 0.22 |
| Control group | 1.2 | ||
| T2 vs T3 | Test group | 0.6 | 0.21 |
| Control group | 0.9 |
VRS: verbal rating scale; T1: 24 h after periodontal surgery; T2: 48 h after periodontal surgery; T3: 72 h after periodontal surgery.
Discussion
In the present study, stringent eligibility criteria, such as exclusion of self-reported tobacco-product users and immunosuppressed patients, were adopted. It is well known that tobacco smoking and systemic diseases such as poorly-controlled DM and habits such as cigarette smoking are risk factors for periodontitis.24,27 Although patients included in the present investigation were presumably systemically healthy and were non-smokers, it is imperative to interpret this information with caution, as laboratory-based investigations such as assessment of serum glycemic and salivary cotinine levels were not assessed. However, other factors, e.g. as advancing age, compromised routine oral hygiene maintenance, low socioeconomic status and low educational level, are also associated with the occurrence and progression of periodontitis.10,27,31 According to Lertpimonchai et al,31 the risk of periodontitis is nearly 5 times higher in patients with a poor oral hygiene. Such factors may have contributed to the progression of periodontitis in the patient population assessed.
The present results showed no statistically significant difference in the postoperative NRS and VAS scores in the test and control groups. It is therefore tempting to speculate that curcumin and MA are equally effective in reducing self-perceived pain after oral surgical interventions. However, it is important to cautiously interpret such a conclusion, as a number of factors may have biased the results. Firstly, the principal investigator was aware of the medications prescribed to patients in the test and control groups. Although the study was power adjusted, the possibility of bias cannot be overlooked. One justification for this is that patients using curcumin were advised to use 2 capsules whereas those in the control group were taking one tablet of MA. In this regard, patients were possibly aware of which group they belonged to. Furthermore, from an ethical standpoint, the authors could not conceal the objectives of the present study from the participants. Furthermore, to the authors’ knowledge from indexed literature, a consensus has yet to be reached regarding the oral dosage of curcumin that is most effective for the management of post-operative pain and discomfort following oral surgical interventions. In this context, the authors relied upon data from indexed literature to estimate the most effective dosage of curcumin. Results of a clinical trial showed that in contrast to NSAIDs, curcumin demonstrates superior post-surgical anti-inflammatory effect when orally consumed at a dose of 1.2 g daily for 6 days.21 Nevertheless, it is difficult to predict the precise role of curcumin or MA in reducing post-operative discomfort or pain as all participants were prescribed antibiotics. From a biomedical ethics perspective, the authors were unable to include additional treatment groups (patients prescribed curcumin or MA only). This was done to minimise the risk of post-surgical infections that could have otherwise influenced pain and discomfort scores after the procedure. In the present study, none of the participants reported any side-effects after consuming any of the prescribed medications. These results suggest that curcumin is a safe herbal medication for the management of post-operative pain and discomfort. This is supported by the results of a phase-I clinical trial in which oral intake of curcumin at doses up to 8 g/day induced no side-effects or complications.13 However, in order to declare curcumin a reliable replacement for traditional NSAIDs warrants further studies.
Conclusion
Compared with MA, curcumin is ineffective for pain and discomfort management after surgical periodontal debridement in patients with periodontitis. The possibility of the results being biased due to lack of operator blinding cannot be overlooked.
Acknowledgements
The authors are grateful to the Researchers supporting project at King Saud University for funding through Researchers supporting project No. (RSP-2021-44)
Funding Statement
The authors are grateful to the Researchers supporting project at King Saud University for funding through Researchers supporting project No. (RSP-2021-44)
References
- Abduljabbar T, Vohra F, Kellesarian SV, Javed F. Efficacy of scaling and root planning with and without adjunct Nd: YAG laser therapy on clinical periodontal parameters and gingival crevicular fluid interleukin 1-beta and tumor necrosis factor-alpha levels among patients with periodontal disease: A prospective randomized split-mouth clinical study. J Photochem Photobiol B. 2017;169:70–74. doi: 10.1016/j.jphotobiol.2017.03.001. [DOI] [PubMed] [Google Scholar]
- Abebe W. Herbal medication: potential for adverse interactions with analgesic drugs. J Clin Pharm Ther. 2002;27:391–401. doi: 10.1046/j.1365-2710.2002.00444.x. [DOI] [PubMed] [Google Scholar]
- Aggarwal BB, Kumar A, Bharti AC. Anticancer potential of curcumin: preclinical and clinical studies. Anticancer Res. 2003;23:363–398. [PubMed] [Google Scholar]
- Al-Hamoudi N, Alsahhaf A, Al Deeb M, Alrabiah M, Vohra F, Abduljabbar T. Effect of scaling and root planing on the expression of anti-inflammatory cytokines (IL-4, IL-9, IL-10, and IL-13) in the gingival crevicular fluid of electronic cigarette users and non-smokers with moderate chronic periodontitis. J Periodontal Implant Sci. 2020;50:74–82. doi: 10.5051/jpis.2020.50.2.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anil A, Gujjari SK, Venkatesh MP. Evaluation of a curcumin-containing mucoadhesive film for periodontal postsurgical pain control. J Indian Soc Periodontol. 2019;23:461–468. doi: 10.4103/jisp.jisp_700_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer BA, Tilburt JC, Sood A, Li GX, Wang SH. Complementary and alternative medicine therapies for chronic pain. Chin J Integr Med. 2016;22:403–411. doi: 10.1007/s11655-016-2258-y. [DOI] [PubMed] [Google Scholar]
- Becker DE. Pain management: Part 1: Managing acute and postoperative dental pain. Anesth Prog. 2010;57:67–78. doi: 10.2344/0003-3006-57.2.67. quiz 79–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berlin-Broner Y, Febbraio M, Levin L. Association between apical periodontitis and cardiovascular diseases: a systematic review of the literature. Int Endod J. 2017;50:847–859. doi: 10.1111/iej.12710. [DOI] [PubMed] [Google Scholar]
- Bessone F. Non-steroidal anti-inflammatory drugs: What is the actual risk of liver damage? World J Gastroenterol. 2010;16:5651–5661. doi: 10.3748/wjg.v16.i45.5651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boillot A, El Halabi B, Batty GD, Rangé H, Czernichow S, Bouchard P. Education as a predictor of chronic periodontitis: a systematic review with meta-analysis population-based studies. PLoS One. 2011;6:e21508. doi: 10.1371/journal.pone.0021508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broglio K. Randomization in clinical trials: permuted blocks and stratification. JAMA. 2018;319:2223–2224. doi: 10.1001/jama.2018.6360. [DOI] [PubMed] [Google Scholar]
- Cashman JN. The mechanisms of action of NSAIDs in analgesia. Drugs. 1996;52(suppl 5):13–23. doi: 10.2165/00003495-199600525-00004. [DOI] [PubMed] [Google Scholar]
- Cheng AL, Hsu CH, Lin JK, Hsu MM, Ho YF, Shen TS, et al. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res. 2001;21:2895–2900. [PubMed] [Google Scholar]
- Cortellini P, Tonetti MS. A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intra-bony defects: a novel approach to limit morbidity. J Clin Periodontol. 2007;34:87–93. doi: 10.1111/j.1600-051X.2006.01020.x. [DOI] [PubMed] [Google Scholar]
- Daily JW, Yang M, Park S. Efficacy of turmeric extracts and curcumin for alleviating the symptoms of joint arthritis: a systematic review and meta-analysis of randomized clinical trials. J Med Food. 2016;19:717–729. doi: 10.1089/jmf.2016.3705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SW, McCahon RA. Management of postoperative pain in maxillofacial surgery. Br J Oral Maxillofac Surg. 2019;57:4–11. doi: 10.1016/j.bjoms.2018.11.010. [DOI] [PubMed] [Google Scholar]
- Gadicherla S, Smriti K, Roy S, Pentapati KC, Rajan J, Walia A. Comparison of extraction socket healing in non-diabetic, prediabetic, and type 2 diabetic patients. Clin Cosmet Investig Dent. 2020;12:291–296. doi: 10.2147/CCIDE.S264196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garimella V, Cellini C. Postoperative pain control. Clin Colon Rectal Surg. 2013;26:191–196. doi: 10.1055/s-0033-1351138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay IC, Tran DT, Paquette DW. Alcohol intake and periodontitis in adults aged ≥ 30 years: NHANES 2009–2012. J Periodontol. 2018;89:625–634. doi: 10.1002/JPER.17-0276. [DOI] [PubMed] [Google Scholar]
- Gupta A, Bah M. NSAIDs in the treatment of postoperative pain. Curr Pain Headache Rep. 2016;20:62. doi: 10.1007/s11916-016-0591-7. [DOI] [PubMed] [Google Scholar]
- Gupta SC, Patchva S, Aggarwal BB. Therapeutic roles of curcumin: lessons learned from clinical trials. Aaps j. 2013;15:195–218. doi: 10.1208/s12248-012-9432-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey NA, Shalamanova L, Whitehead KA, Dempsey-Hibbert N, van der Gast C, Taylor RL. Exploring the putative interactions between chronic kidney disease and chronic periodontitis. Crit Rev Microbiol. 2020:1–17. doi: 10.1080/1040841x.2020.1724872. [DOI] [PubMed] [Google Scholar]
- Iacopino AM. Diabetic periodontitis: possible lipid-induced defect in tissue repair through alteration of macrophage phenotype and function. Oral Dis. 1995;1:214–229. doi: 10.1111/j.1601-0825.1995.tb00187.x. [DOI] [PubMed] [Google Scholar]
- Javed F, Abduljabbar T, Vohra F, Malmstrom H, Rahman I, Romanos GE. Comparison of periodontal parameters and self-perceived oral symptoms among cigarette smokers, individuals vaping electronic cigarettes, and never-smokers. J Periodontol. 2017;88:1059–1065. doi: 10.1902/jop.2017.170197. [DOI] [PubMed] [Google Scholar]
- Javed F, Al-Kheraif AA, Al Amri MD, Mikami T, Vohra F, Warnakulasuriya S, et al. Periodontal parameters and whole salivary cytokine profiles among habitual gutka chewers and non-chewers. J Periodontol. 2015;86:689–695. doi: 10.1902/jop.2015.140556. [DOI] [PubMed] [Google Scholar]
- Javed F, Al-Rasheed A, Almas K, Romanos GE, Al-Hezaimi K. Effect of cigarette smoking on the clinical outcomes of periodontal surgical procedures. Am J Med Sci. 2012;343:78–84. doi: 10.1097/MAJ.0b013e318228283b. [DOI] [PubMed] [Google Scholar]
- Javed F, Näsström K, Benchimol D, Altamash M, Klinge B, Engström PE. Comparison of periodontal and socioeconomic status between subjects with type 2 diabetes mellitus and non-diabetic controls. J Periodontol. 2007;78:2112–2119. doi: 10.1902/jop.2007.070186. [DOI] [PubMed] [Google Scholar]
- Jurenka JS. Anti-inflammatory properties of curcumin, a major constituent of Curcuma longa: a review of preclinical and clinical research. Altern Med Rev. 2009;14:141–153. [PubMed] [Google Scholar]
- Karimi A, Majlesi M, Rafieian-Kopaei M. Herbal versus synthetic drugs; beliefs and facts. J Nephropharmacol. 2015;4:27–30. [PMC free article] [PubMed] [Google Scholar]
- Kumarswamy A. Multimodal management of dental pain with focus on alternative medicine: A novel herbal dental gel. Contemp Clin Dent. 2016;7:131–139. doi: 10.4103/0976-237X.183066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lertpimonchai A, Rattanasiri S, Arj-Ong Vallibhakara S, Attia J, Thakkinstian A. The association between oral hygiene and periodontitis: a systematic review and meta-analysis. Int Dent J. 2017;67:332–343. doi: 10.1111/idj.12317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundmark A, Hu YOO, Huss M, Johannsen G, Andersson AF, Yucel-Lindberg T. Identification of salivary microbiota and its association with host inflammatory mediators in periodontitis. Front Cell Infect Microbiol. 2019;9:216. doi: 10.3389/fcimb.2019.00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulina T, Diana H, Cahyanto A, Amaliya A. The efficacy of curcumin in managing acute inflammation pain on the post-surgical removal of impacted third molars patients: A randomised controlled trial. J Oral Rehabil. 2018;45:677–683. doi: 10.1111/joor.12679. [DOI] [PubMed] [Google Scholar]
- Meghana MVS, Deshmukh J, Devarathanamma MV, Asif K, Jyothi L, Sindhura H. Comparison of effect of curcumin gel and noneugenol periodontal dressing in tissue response, early wound healing, and pain assessment following periodontal flap surgery in chronic periodontitis patients. J Indian Soc Periodontol. 2020;24:54–59. doi: 10.4103/jisp.jisp_105_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon VP, Sudheer AR. Antioxidant and anti-inflammatory properties of curcumin. Adv Exp Med Biol. 2007;595:105–125. doi: 10.1007/978-0-387-46401-5_3. [DOI] [PubMed] [Google Scholar]
- Nagpal M, Sood S. Role of curcumin in systemic and oral health: An overview. J Nat Sci Biol Med. 2013;4:3–7. doi: 10.4103/0976-9668.107253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair B. Clinical Trial Designs. Indian Dermatol Online J. 2019;10:193–201. doi: 10.4103/idoj.IDOJ_475_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(suppl 1):S173–182. doi: 10.1002/JPER.17-0721. [DOI] [PubMed] [Google Scholar]
- Polvora TLS, Nobre AVV, Tirapelli C, Taba M, Macedo LD, Jr, Santana RC, et al. Relationship between human immunodeficiency virus (HIV-1) infection and chronic periodontitis. Expert Rev Clin Immunol. 2018;14:315–327. doi: 10.1080/1744666X.2018.1459571. [DOI] [PubMed] [Google Scholar]
- Rajamäki TJ, Jämsen E, Puolakka PA, Nevalainen PI, Moilanen T. Diabetes is associated with persistent pain after hip and knee replacement. Acta Orthop. 2015;86:586–593. doi: 10.3109/17453674.2015.1044389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rayati F, Hajmanouchehri F, Najafi E. Comparison of anti-inflammatory and analgesic effects of Ginger powder and Ibuprofen in postsurgical pain model: A randomized, double-blind, case-control clinical trial. Dent Res J (Isfahan) 2017;14:1–7. doi: 10.4103/1735-3327.201135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosas S, Paço M, Lemos C, Pinho T. Comparison between the Visual Analog Scale and the Numerical Rating Scale in the perception of esthetics and pain. Int Orthod. 2017;15:543–560. doi: 10.1016/j.ortho.2017.09.027. [DOI] [PubMed] [Google Scholar]
- Sun J, Chen F, Braun C, Zhou YQ, Rittner H, Tian YK, et al. Role of curcumin in the management of pathological pain. Phytomedicine. 2018;48:129–140. doi: 10.1016/j.phymed.2018.04.045. [DOI] [PubMed] [Google Scholar]
- Tobias JD. Weak analgesics and nonsteroidal anti-inflammatory agents in the management of children with acute pain. Pediatr Clin North Am. 2000;47:527–543. doi: 10.1016/s0031-3955(05)70224-8. [DOI] [PubMed] [Google Scholar]


