Abstract
Background/Objectives: The Ministry of Health, Labor and Welfare in Japan has been promoting physicians’ working style reforms since 2019. This study aimed to update the relationship between working hours, depressive symptoms, and suicidal ideation among obstetricians and gynecologists, based on the physicians’ working style reforms. Methods: A questionnaire-based survey was conducted among obstetricians and gynecologists, and valid responses were obtained from 1164 physicians. Multivariable logistic regression analysis was performed to identify significant associations. Results: Of the respondents, 49.8% were female, and most physicians were aged 30–39 (32.1%). Precisely, 57.4% worked in public hospitals, and 47.9% worked in urban areas. Physicians working 40 ≤ x < 60 h per week accounted for the largest proportion of physicians. Depressive symptoms and suicidal ideation accounted for 16.4% and 3.6% of participants, respectively. The following factors were significantly associated with depressive symptoms as a dependent variable: other occupation, having two or three children, working 60–80 h or >100 h per week, and working in rural areas. None of these variables was significantly associated with suicidal ideation. Conclusions: The physicians’ working style reforms have reduced the number of working hours for obstetricians and gynecologists. However, rates of depressive symptoms and suicidal ideation have not improved.
Keywords: Karōshi, working hour, depressive symptoms, suicide ideation, Japan
1. Introduction
The number of working hours among laborers in Japan is relatively high compared to international levels [1]. A comparison between occupations shows that physicians have particularly long working hours [2]. Among physicians, those working in obstetrics and gynecology hospitals tend to work longer hours [3].
In 2016, the Ministry of Health, Labor and Welfare established the Study Group on Physicians’ Working Style Reform, which investigated measures to promote physicians’ working style reforms and published a report in 2019 [4]. The report states that the maximum overtime hours for physicians will begin in April 2024, starting at 960 h per year for Level A and 1860 h per year for Level B (provisional special level for securing regional medical care). It outlines concrete measures to reduce working hours, including specific regulations on physicians’ overtime, proper management of working hours, utilization of existing industrial health systems, and promotion of task shifting.
There is a wide range of national and international evidence regarding the adverse health effects of long working hours. According to a systematic review by Bannai et al., long working hours are associated with depressive state, anxiety, sleep conditions, and coronary heart disease [5]. Suicide due to depression caused by excessive workload and death from ischemic heart disease and cerebrovascular disease are called “Karōshi” or “overwork death” and have become a public health issue unique to China and other East Asian countries [6].
Medicine is a stressful profession, and residents are especially prone to depression and burnout [7,8,9]. According to a review of factors associated with physician burnout, younger age, female sex, negative marital status, long working hours, and low reported job satisfaction are predictors of burnout [10]. Long working hours negatively affect residents’ health and medical safety [11,12].
In 2019, we conducted a study that, for the first time, revealed the extent of overwork among obstetricians and gynecologists in Japan and demonstrated that long working hours among physicians may lead to depressive symptoms and suicidal ideation [13].
Following the implementation of the physicians’ working style reforms in 2019, it was hoped that working hours would be reduced, leading to a decrease in the proportion of doctors suffering from depression or suicidal thoughts. However, no studies have examined the improvements in depressive symptoms and suicidal ideation after the reform.
This study aimed to update the understanding of the relationship between working hours, depressive symptoms, and suicidal ideation among obstetricians and gynecologists in light of the physicians’ working style reforms implemented in 2019.
2. Materials and Methods
2.1. Participants
We selected 1170 hospitals across Japan with obstetrics and gynecology departments whose hospital names were disclosed through the hospital bed function reporting system [14]. In November 2023, we sent survey request forms to managers and physicians of the obstetrics and gynecology departments. An online questionnaire survey was conducted, taking approximately 10 min to complete, and responses were collected via Google Forms. No special follow-up was conducted, and respondents who did not complete the survey were excluded. In addition, no incentives or compensation were offered to participants.
2.2. Measurements
2.2.1. Depressive Symptoms
To assess the respondents’ depressive state, we used the Japanese version (QIDS-SR-J) [15] of the 16-Item Quick Inventory of Depressive Symptomatology Self-Report Version (QIDS-SR) [16], used worldwide to assess the severity of depression and defined depression, as moderate or high on the scale. The QIDS-SR is a 16-item self-administered rating scale that evaluates depression severity and aligns with the diagnostic criteria for major depressive disorder in the DSM-IV of the American Psychiatric Association [16]. The QIDS-SR-J is the validated Japanese version of this tool.
We also determined whether those who were depressed also had suicidal ideation, which tended to be higher among physicians in previous studies [17]. As in previous studies, we considered as having suicidal ideation those who responded as follows: “I think about suicide or death for several minutes several times a week” and “I have thought about suicide or death in great detail several times a day or made specific suicide plans or actually attempted to die”.
2.2.2. Working Hours and Risk Factors
We first described the physician attributes (sex, age, occupation, weekly working hours, foundational entity of the workplace, total number of hospital beds, and region) for all the respondents and for those with and without depressive symptoms, with the cutoff set at moderate or higher on the QIDS-SR-J (Table 1). Age was classified into six groups: <30 years, 30s, 40s, 50s, 60s, and ≥70 years. The foundational entities of the workplace were classified into four groups: public, national universities, private universities, and private (excluding private universities). Occupation was classified into four groups: department manager, staff, specialized physician, and others. The weekly working hours were classified into five groups: x < 40 h, 40 ≤ x < 60 h, 60 ≤ x < 80, 80 ≤ x < 100 h, and x ≥ 100 h. The total number of hospital beds was classified into five groups: x < 200 beds, 200 ≤ x < 400 beds, 400 ≤ x < 600 beds, 600 ≤ x < 800 beds, and x ≥ 800 beds. In Japan, 344 secondary medical areas were classified into three categories based on the combination of population size and population density in 2023: the first group (urban), the second group (intermediate), and the third group (rural) [18].
Table 1.
Characteristics of participants.
| Total | Without Depressive Symptoms | Depressive Symptoms | Suicide Ideation | |||||
|---|---|---|---|---|---|---|---|---|
| Total number of participants, n | 1164 | 973 | 191 | 42 | ||||
| % of all participants | 100.0% | 83.6% | 16.4% | 3.6% | ||||
| Sex, n, % | ||||||||
| Female | 580 | 49.8% | 475 | 48.8% | 105 | 55.0% | 25 | 59.5% |
| Male | 584 | 50.2% | 498 | 51.2% | 86 | 45.0% | 17 | 40.5% |
| Age, n, % | ||||||||
| <30 | 130 | 11.2% | 104 | 10.7% | 26 | 13.6% | 7 | 16.7% |
| 30–39 | 374 | 32.1% | 301 | 30.9% | 73 | 38.2% | 18 | 42.9% |
| 40–49 | 318 | 27.3% | 263 | 27.0% | 55 | 28.8% | 9 | 21.4% |
| 50–59 | 187 | 16.1% | 162 | 16.6% | 25 | 13.1% | 5 | 11.9% |
| 60–69 | 141 | 12.1% | 130 | 13.4% | 11 | 5.8% | 2 | 4.8% |
| ≧70 | 14 | 1.2% | 13 | 1.3% | 1 | 0.5% | 1 | 2.4% |
| Occupation | ||||||||
| Department manager | 325 | 27.9% | 291 | 29.9% | 34 | 17.8% | 9 | 21.4% |
| Staff | 582 | 50.0% | 477 | 49.0% | 105 | 55.0% | 20 | 47.6% |
| Specialized physician | 223 | 19.2% | 179 | 18.4% | 44 | 23.0% | 12 | 28.6% |
| Other | 34 | 2.9% | 26 | 2.7% | 8 | 4.2% | 1 | 2.4% |
| Delivery-related work | ||||||||
| Yes | 1060 | 91.1% | 880 | 90.4% | 180 | 94.2% | 37 | 88.1% |
| No | 104 | 8.9% | 93 | 9.6% | 11 | 5.8% | 5 | 11.9% |
| Number of children | ||||||||
| None | 409 | 35.1% | 319 | 32.8% | 90 | 47.1% | 20 | 47.6% |
| 1 | 189 | 16.2% | 152 | 15.6% | 37 | 19.4% | 6 | 14.3% |
| 2 | 363 | 31.2% | 320 | 32.9% | 43 | 22.5% | 10 | 23.8% |
| 3 | 168 | 14.4% | 150 | 15.4% | 18 | 9.4% | 4 | 9.5% |
| ≥4 | 35 | 3.0% | 32 | 3.3% | 3 | 1.6% | 2 | 4.8% |
| Working hours per week, n, % | ||||||||
| <40 | 148 | 12.7% | 135 | 13.9% | 13 | 6.8% | 5 | 11.9% |
| 40–59 | 710 | 61.0% | 614 | 63.1% | 96 | 50.3% | 20 | 47.6% |
| 60–79 | 240 | 20.6% | 180 | 18.5% | 60 | 31.4% | 13 | 31.0% |
| 80–99 | 46 | 4.0% | 31 | 3.2% | 15 | 7.9% | 3 | 7.1% |
| ≧100 | 17 | 1.5% | 10 | 1.0% | 7 | 3.7% | 1 | 2.4% |
| Entity of employer | ||||||||
| Public | 668 | 57.4% | 565 | 58.1% | 103 | 53.9% | 21 | 50.0% |
| National University | 121 | 10.4% | 91 | 9.4% | 30 | 15.7% | 3 | 7.1% |
| Private University | 69 | 5.9% | 55 | 5.7% | 14 | 7.3% | 5 | 11.9% |
| Private | 306 | 26.3% | 262 | 26.9% | 44 | 23.0% | 13 | 31.0% |
| Employer’s total no. of beds | ||||||||
| <200 beds | 90 | 7.7% | 80 | 8.2% | 10 | 5.2% | 4 | 9.5% |
| ≥200–<400 beds | 320 | 27.5% | 271 | 27.9% | 49 | 25.7% | 9 | 21.4% |
| ≥400–<600 beds | 399 | 34.3% | 340 | 34.9% | 59 | 30.9% | 14 | 33.3% |
| ≥600–<800 beds | 203 | 17.4% | 163 | 16.8% | 40 | 20.9% | 6 | 14.3% |
| ≥800 beds | 152 | 13.1% | 119 | 12.2% | 33 | 17.3% | 9 | 21.4% |
| Area, n, % | ||||||||
| Urban | 558 | 47.9% | 472 | 48.5% | 86 | 45.0% | 21 | 50.0% |
| Intermediate | 489 | 42.0% | 412 | 42.3% | 77 | 40.3% | 18 | 42.9% |
| Rural | 10.1% | 89 | 9.1% | 28 | 14.7% | 3 | 7.1% | |
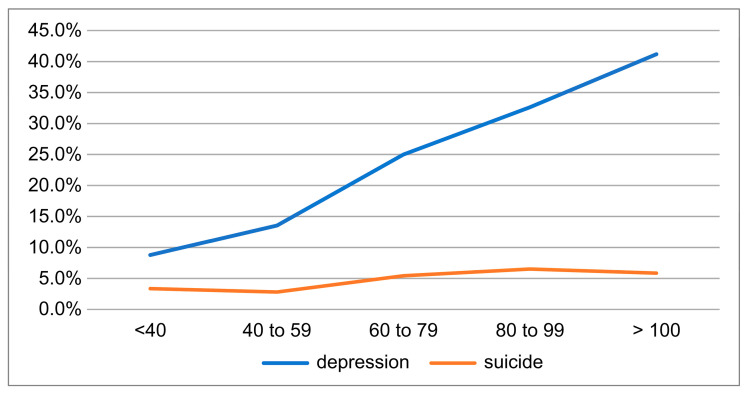
Figure 1 shows the percentage of depressive symptoms and suicidal ideation for each category of working hours per week.
Figure 1.
Relationship between working hours and depression symptoms/suicide ideation.
2.3. Statistical Analysis
To examine the relationship between depressive symptoms, working hours, and other risk factors among obstetricians and gynecologists, we performed a multivariable logistic regression analysis, with the cutoff set at moderate or higher on the QIDS-SR-J (Table 2). Depressive symptoms were set as the dependent variable, and physician attributes (sex, age, occupation, weekly working hours, whether to perform delivery, number of children, foundational entity of the workplace, total number of beds, and region) were set as independent variables. We also conducted a multivariate logistic regression analysis with suicidal ideation as the dependent variable and the other variables as independent variables (Table 2). The QIDS-SR16 has proven to be a popular choice given that it was developed to align with the Diagnostic and Statistical Manual of Mental Disorders-IV criteria and is quick and simple to administer [19]. The required sample size for logistic regression analysis is typically 10 times the number of explanatory variables (9), thus requiring a minimum of 90 samples; our sample size of 1164 is therefore sufficient [20].
Table 2.
Logistic regression analysis of factors associated with depressive symptoms and suicidal ideation.
| Depressive Symptoms | OR | 95% CI | p-Value | Suicidal Ideation | OR | 95% CI | p-Value |
|---|---|---|---|---|---|---|---|
| Sex | Sex | ||||||
| Female | Reference | Female | Reference | ||||
| Male | 1.05 | 0.73–1.51 | 0.80 | Male | 0.72 | 0.3–1.48 | 0.37 |
| Age | Age | ||||||
| <30 years | Reference | <30 years | Reference | ||||
| 30 s | 1.13 | 0.58–2.19 | 0.72 | 30 s | 0.97 | 0.28–3.37 | 0.96 |
| 40 s | 1.35 | 0.64–2.88 | 0.43 | 40 s | 0.49 | 0.11–2.20 | 0.36 |
| 50 s | 1.06 | 0.44–2.56 | 0.89 | 50 s | 0.29 | 0.47–1.79 | 0.18 |
| 60 s | 0.68 | 0.24–1.92 | 0.46 | 60 s | 0.21 | 0.02–1.80 | 0.16 |
| ≥70 years | 0.82 | 0.09–7.86 | 0.87 | ≥70 years | 1.62 | 0.11–24.48 | 0.73 |
| Occupation | Occupation | ||||||
| Department manager | Reference | Department manager | Reference | ||||
| Staff | 1.34 | 0.78–2.31 | 0.29 | Staff | 0.73 | 0.24–2.23 | 0.58 |
| Specialized physician | 1.13 | 0.54–2.37 | 0.74 | Specialized physician | 0.61 | 0.14–2.74 | 0.52 |
| Other | 3.06 | 1.08–8.62 | 0.04 | Other | 0.63 | 0.06–6.34 | 0.69 |
| Delivery-related work | Delivery-related work | ||||||
| No | Reference | No | Reference | ||||
| Yes | 1.39 | 0.69–2.78 | 0.36 | Yes | 0.69 | 0.22–2.16 | 0.53 |
| Number of children | Number of children | ||||||
| None | Reference | None | Reference | ||||
| 1 | 0.75 | 0.46–1.22 | 0.26 | 1 | 1.00 | 0.38–2.67 | 0.98 |
| 2 | 0.47 | 0.29–0.75 | 0.00 | 2 | 1.90 | 0.33–2.17 | 0.74 |
| 3 | 0.44 | 0.24–0.83 | 0.01 | 3 | 2.37 | 0.25–3.05 | 0.84 |
| ≥4 | 0.39 | 0.11–1.38 | 0.14 | ≥4 | 2.14 | 0.52–14.67 | 0.24 |
| Working Hours per Week | Working Hours per Week | ||||||
| <40 h per week | Reference | <40 h per week | Reference | ||||
| 40~60 h per week | 1.43 | 0.76–2.70 | 0.27 | 40~60 h per week | 1.00 | 0.34–2.91 | 1.00 |
| 60~80 h per week | 2.51 | 1.26–5.00 | 0.01 | 60~80 h per week | 1.90 | 0.60–6.06 | 0.28 |
| 80~100 h per week | 6.88 | 2.88–16.45 | 0.00 | 80~100 h per week | 2.37 | 0.48–1168 | 0.29 |
| ≥100 h per week | 5.93 | 1.80–19.57 | 0.00 | ≥100 h per week | 2.15 | 0.21–21.92 | 0.52 |
| Foundational Entity of Employer | Foundational Entity of Employer | ||||||
| Public | Reference | Public | Reference | ||||
| National University | 1.43 | 0.77–2.64 | 0.25 | National University | 0.58 | 0.15–2.29 | 0.44 |
| Private University | 0.87 | 0.36–2.06 | 0.74 | Private University | 0.60 | 0.13–2.72 | 0.50 |
| Private | 1.08 | 0.69–1.70 | 0.74 | Private | 1.29 | 0.57–2.92 | 0.54 |
| Employer’s Total No. of Beds | Employer’s Total No. of Beds | ||||||
| <200 beds | Reference | <200 beds | Reference | ||||
| ≥200–<400 beds | 0.92 | 0.41–2.03 | 0.83 | ≥200–<400 beds | 0.54 | 0.14–2.01 | 0.36 |
| ≥400–<600 beds | 1.03 | 0.46–2.31 | 0.94 | ≥400–<600 beds | 0.84 | 0.23–3.06 | 0.80 |
| ≥600–<800 beds | 1.20 | 0.50–2.92 | 0.68 | ≥600–<800 beds | 0.63 | 0.13–3.00 | 0.56 |
| ≥800 beds | 1.62 | 0.62–4.20 | 0.32 | ≥800 beds | 2.03 | 0.44–9.38 | 0.37 |
| Workplace | Workplace | ||||||
| Urban | Reference | Urban | Reference | ||||
| Intermediate | 1.16 | 0.81–1.67 | 0.41 | Intermediate | 0.93 | 0.47–1.85 | 0.84 |
| Rural | 1.97 | 1.11–3.49 | 0.02 | Rural | 1.06 | 0.33–3.43 | 0.93 |
p < 0.05. OR, odds ratio; CI, confidence interval.
Statistical analyses were considered significant at p-values < 0.05. STATA 17.0 was used for all statistical analyses.
2.4. Ethical Considerations
This study was approved by the Human Research Ethics Committee of the Tokyo Healthcare University (approval number: Education 023-03B). The study objective and measures to ensure secure data management were stated on the first page of the questionnaire. We also explained to the potential participants that their involvement in the study was voluntary. Informed consent was obtained from all participants. The results were analyzed separately from personal information to ensure anonymity and confidentiality of personal information.
3. Results
Questionnaires were sent to 1170 hospitals across Japan, and valid responses were received from 423 hospitals (valid response rate: 36.2%) and 1164 physicians. The 1164 OBGYNs who responded accounted for 16.3% of the 7127 hospital-based obstetricians and gynecologists in the 2020 Statistics on Physicians, Dentists, and Pharmacists conducted by the Ministry of Health, Labor and Welfare [21].
As shown in Table 1, 49.8% of the respondents were female, and most physicians were aged 30–39, accounting for 32.1% of the population. A total of 57.4% of the physicians worked in public hospitals, and 47.9% worked in urban areas.
Physicians working 40 ≤ x < 60 h per week accounted for the largest proportion of physicians (61.6%), followed by 20.6% in the 60–79 h per week group, 12.7% in the <40 h per week group, 4.0% in the 80 ≤ x < 100 h per week group and 1.5% in the x ≥ 100 h per week group. In our study in 2019, physicians working 60–80 h per week accounted for the largest proportion of physicians (37.5%), followed by 27.1% in the x ≥ 100 h per week group and 19.5% in the 80–100 h/week group.
Precisely 16.4% of respondents were rated as having moderate-to-severe depression on the QIDS-SR-J. As shown in Figure 1, the proportion of patients with depressive symptoms was higher in the group that worked longer hours. It was 25.0% in the 60 ≤ x < 80 h per week group and 32.6% in the 80 ≤ x < 100 h per week group. Suicidal ideation was present in 3.6% of respondents and was higher in the group with 80–100 h per week (6.5%).
Table 2 shows the results of the multivariate logistic regression analysis. With depressive symptoms as the dependent variable, the following showed significant associations: other occupation (control: department manager); having two children (control: no children); having three children (control: no children); 60–80 h per week (control: <40 h per week); 80–100 h per week (control: <40 h per week); >100 h per week (control: <40 h per week); and rural areas (control: urban).
In the analysis with suicidal ideation as the dependent variable, no significant association was found for any of the variables.
4. Discussion
In this study, physicians working > 60 h per week accounted for 26.0% of the respondents, revealing the excessive workload of obstetricians and gynecologists working in Japanese hospitals. Weekly working hours of 60 h correspond to 4 h of overtime work per day compared to the legal working hours of 8 h per day and 40 h per week, as stipulated by the Labor Standards Act, and the number of overtime hours exceeds approximately 80 h per month. Such long working hours are referred to as “death-from-overwork level” since they are strongly associated with the development of mental disorders and cardiovascular diseases due to psychological stress, and they meet the certification criteria for occupational hazards [22,23]. Since 49.1% of the respondents seem to have working conditions that exceed “Karōshi’s criteria”, there is an urgent need to improve the working environment for obstetricians and gynecologists in the development of a sustainable obstetric and gynecological medical system.
In contrast, 84.1% of physicians in the 2019 survey worked over 60 h per week; thus, working hours were found to have decreased considerably in the current survey [13]. This may be due to progress in physicians’ working style reforms, such as task shifting. However, the Ministry of Health, Labor and Welfare has given guidance that hours for “physician’s study” are not to be added to working hours, which was unclear in 2019. Additionally, the hours that were previously considered working hours have been made clear to employees as a result of the acquisition of “the permission of night and day shifts”, and much of the time during night and day shifts is now considered to be break time. These points may have impacted the above comparison [24,25].
There are a few points to note regarding whether obstetricians and gynecologists really work fewer hours. First, the definition of a physician’s study time has been defined by the Ministry of Health, Labor, and Welfare; however, in some cases, the distinction between labor and self-study is not always straightforward [26]. Additionally, the following can be said regarding “the permission of night and day shifts” and whether the workload during the on-call day shift is greater or less than that during the night and day shift. In a study of Japanese obstetricians and gynecologists, 17% answered that their workload was very heavy, and 31% answered that their workload was somewhat heavy; thus, it should be noted that the criteria for night and day shift permits may be loose [27].
Precisely 16.4% of respondents were rated as having moderate-to-severe depression on the QIDS-SR-J, and suicidal ideation was present in 3.6% of respondents, which was approximately the same as in the 2019 survey (16.4% for depressive symptoms and 3.3% for suicidal ideation). In other words, there was no improvement in the rates of depressive symptoms and suicidal ideation despite the reduction in working hours compared with 2019. As pointed out in the previous paragraph, this may be related to the fact that the definition of working hours has changed so that the actual time spent in the hospital has not changed or to factors other than working hours, such as people relationships [28].
Compared to previous studies, a study of employed Japanese physicians found the prevalence of depressive symptoms to be 6.5% and suicidal ideation to 3.6%, both lower than the results of this study [17]. One possible reason for this is that the working hours of obstetricians and gynecologists are longer than those of other medical departments [3]. There are no other studies on obstetricians and gynecologists worldwide, with the exception of ours; therefore, it is difficult to make comparisons.
In multiple logistic regression analysis with depressive symptoms as the dependent variable, depressive symptoms were significantly lower for those with two or three children (control: no children) and significantly higher for those who worked 60–80 h/week, 80–100 h/week, more than 100 h/week (control: under 40 h/week), and rural areas (control: urban areas). The odds ratio for an 80–100 h per h/week was the highest among the independent variables. In the analysis with suicidal ideation as the dependent variable, no significant association was found for any of the variables.
According to previous studies, younger physician age, female sex, negative marital status, and long working hours have been said to be predictors of burnout [10]. A previous study conducted in 2019 showed a significant positive association between depressive symptoms and negative marital status, long working hours, being male, and aged 30–49 years. In the present study, long working hours were significantly associated with depressive symptoms; however, the other factors were not consistent with those in previous studies. Having children may reduce the likelihood of depressive symptoms, possibly because of reduced working hours resulting from time spent on childcare and education.
Regarding the relationship between depressive symptoms and factors such as the characteristics of the hospital where the physicians work and the region in which the hospital is located, only rural areas were significantly associated with the independent variables in this study. Physician shortages are a problem in underpopulated areas, leading to longer working hours, which can lead to depression [18].
Among obstetricians and gynecologists, physicians who perform deliveries have longer working hours and lower career satisfaction [29]. A more detailed survey of physicians’ practice would enable a more elaborate discussion.
Study Limitations
This study had some limitations. First, only 423 of the 1170 hospitals (36.2%) and 1164 physicians participated in the study, which is a relatively small number because participation was voluntary. It is possible that physicians who responded to our questionnaire were interested in issues such as working conditions, mental health, or depressive symptoms. Additionally, severely depressed physicians may not have responded to the survey.
Second, we used a self-administered questionnaire and defined residents who had a QIDS-SR-J score of ≥16 as screening-positive for depressive symptoms. In addition, the QIDS-SR is based on DSM-IV criteria rather than DSM-5, so this algorithm may not fully align with current diagnostic standards or detect all cases of depressive symptoms. For assessing suicidal ideation, quantitative measures such as the Suicide Intent Scale were not used, which may limit the assessment’s thoroughness.
Third, the relationship between working hours, depressive symptoms, and suicidal ideation was statistical rather than causal. This may be related to factors that were not measured, such as job satisfaction, support systems, underlying diseases, alcoholism, economic background, and sleep status [28].
Fourth, in defining suicidal ideation, this study did not examine details such as the full spectrum of ideation severity, frequency, and intent—as were performed in previous studies—which remains an area for future research [30].
Fifth, with regard to working hours, responses were provided in 20 h increments to increase the response rate. Using narrower categories or continuous analysis of hours could have yielded more precise insights.
5. Conclusions
Following a study conducted in 2019, this study sheds light on the relationship between overwork and mental health among obstetricians and gynecologists in Japan. Although working hours decreased, the rates of depressive symptoms and suicidal ideation have remained unchanged, suggesting that factors other than working hours, as well as changes in the definition of working hours, may contribute to depressive symptoms and suicidal ideation. Physician working-style reforms need to be vigorously promoted to improve the mental health of obstetricians and gynecologists.
Acknowledgments
The authors would like to thank all the participants of the study.
Author Contributions
M.I. contributed to all aspects of the study. R.S. and M.O. contributed by supervising the study. Y.S. was responsible for project administration. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was approved by the Human Research Ethics Committee of the Tokyo Healthcare University (approval number: Education 023-03B and date of approval: 28 March 2023).
Informed Consent Statement
Informed consent was obtained from all participants in this study. The results were analyzed separately from personal information to ensure anonymity and confidentiality of personal information.
Data Availability Statement
Some data are unavailable due to ethical restrictions.
Conflicts of Interest
Author Yoshino Sato was employed by the company Okoge Co., Ltd. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding Statement
This study was supported by the Ministry of Education, Culture, Sports, Science, and Technology Grant-in-Aid for Scientific Research (22K10436 Empirical Research on Progress and Issues of Work Style Reform to Address the Harsh Working Environments of Obstetricians and Gynecologists across Japan).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Ogura K. Long working hours in Japan; an international comparison and research topics. Jpn. Econ. 2009;36:23–45. [Google Scholar]
- 2.Ministry of Internal Affairs and Communications Employment Structure Basic Survey; Volume 2013. [(accessed on 10 August 2024)];2012 Available online: https://www.stat.go.jp/data/shugyou/2012/index2.html. (In Japanese)
- 3.Ministry of Health, Labour and Welfare Regarding Ideal Paths Forward for Overtime Work Regulations. [(accessed on 10 August 2024)];2019 Available online: https://www.mhlw.go.jp/content/10800000/000481338.pdf. (In Japanese)
- 4.Ministry of Health, Labour and Welfare Report of the Study Group on Physicians’ Working Style Reform. [(accessed on 10 August 2024)];2019 Available online: https://www.mhlw.go.jp/stf/newpage_04273.html. (In Japanese)
- 5.Bannai A., Tamakoshi A. The association between long working hours and health: A systematic review of epidemiological evidence. Scand. J. Work. Environ. Health. 2014;40:5–18. doi: 10.5271/sjweh.3388. [DOI] [PubMed] [Google Scholar]
- 6.Eguchi H., Wada K., Smith D.R. Recognition, compensation, and prevention of Karoshi, or death due to overwork. J. Occup. Environ. Med. 2016;58:e313–e314. doi: 10.1097/JOM.0000000000000797. [DOI] [PubMed] [Google Scholar]
- 7.Thomas N.K. Resident burnout. JAMA. 2004;292:2880–2889. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- 8.Dyrbye L., Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med. Educ. 2016;50:132–149. doi: 10.1111/medu.12927. [DOI] [PubMed] [Google Scholar]
- 9.Dyrbye L.N., West C.P., Satele D., Boone S., Tan L., Sloan J., Shanafelt T.D. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad. Med. 2014;89:443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 10.Amoafo E., Hanbali N., Patel A., Singh P. What are the significant factors associated with burnout in doctors? Occup. Med. 2015;65:117–121. doi: 10.1093/occmed/kqu144. [DOI] [PubMed] [Google Scholar]
- 11.Lockley S.W., Cronin J.W., Evans E.E., Cade B.E., Lee C.J., Landrigan C.P., Rothschild J.M., Katz J.T., Lilly C.M., Stone P.H., et al. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N. Engl. J. Med. 2004;351:1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 12.Landrigan C.P., Rothschild J.M., Cronin J.W., Kaushal R., Burdick E., Katz J.T., Lilly C.M., Stone P.H., Lockley S.W., Bates D.W., et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N. Engl. J. Med. 2004;351:1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 13.Ishikawa M. Long working hours, depression and suicidality among OB/GYNs in Japan. Occup. Med. 2022;72:200–206. doi: 10.1093/occmed/kqab191. [DOI] [PubMed] [Google Scholar]
- 14.Ministry of Health, Labour and Welfare Hospital Bed Function Reporting System. [(accessed on 2 January 2024)]; Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000055891.html. (In Japanese)
- 15.Fujisawa D., Nakagawa A., Tajima M., Sado M., Kikuchi T., Iba M.K. Cross-cultural adaptation of the quick inventory of depressive symptomatology-self report (QIDS-SR) Jpn. J. Stress. Sci. 2010;25:43–52. [Google Scholar]
- 16.Trujols J., de Diego-Adeliño J., Feliu-Soler A., Iraurgi I., Puigdemont D., Álvarez E., Pérez V., Portella M.J. Looking into the effect of multi-item symptom domains on psychometric characteristics of the Quick Inventory of Depressive Symptomatology-Self Report (QIDS-SR16) Psychiatry Res. 2018;267:126–130. doi: 10.1016/j.psychres.2018.05.076. [DOI] [PubMed] [Google Scholar]
- 17.Review Committee on Health Support for Employed Physicians Affiliated with the Japan Medical Association. Report of a Questionnaire-Based Survey on the Current State of Health and Support for Employed Physicians. 2016. [(accessed on 10 August 2024)]. Available online: http://dl.med.or.jp/dl-med/kinmu/kshien28.pdf. (In Japanese)
- 18.Fukuda S., Watanabe T., Takahashi T. Research on regional disparity of the number of physicians by clinical departments. J. Jpn. Soc. Healthc. Admin. 2018;55:9–18. (In Japanese) [Google Scholar]
- 19.Rush A.J., Trivedi M.H., Ibrahim H.M., Carmody T.J., Arnow B., Klein D.N., Markowitz J.C., Ninan P.T., Kornstein S., Manber R., et al. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biol. Psychiatry. 2003;54:573–583. doi: 10.1016/S0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 20.Peduzzi P., Concato J., Kemper E., Holford T.R., Feinstein A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996;49:1373–1379. doi: 10.1016/S0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 21.Ministry of Health, Labour and Welfare Overview of Statistics on Physicians, Dentists, and Pharmacists. [(accessed on 10 August 2024)];2022 Available online: https://www.mhlw.go.jp/toukei/saikin/hw/ishi/20/index.html. (In Japanese)
- 22.Ministry of Health, Labour and Welfare . Regarding Certification Criteria for Mental Disorders Due to Psychological Stress. Ministry of Health, Labour and Welfare; Tokyo, Japan: 2011. (In Japanese) [Google Scholar]
- 23.Ministry of Health, Labour and Welfare . Regarding Certification Criteria for Cerebrovascular Disease and Ischemic Heart Disease, Etc. (Excluding Those Caused by Injury) Ministry of Health, Labour and Welfare; Tokyo, Japan: 2001. (In Japanese) [Google Scholar]
- 24.Ministry of Health, Labour and Welfare Views on Physician’s Study and Working Hours. [(accessed on 19 November 2018)]; Available online: https://www.mhlw.go.jp/content/10800000/000404613.pdf. (In Japanese)
- 25.Dr. Part-Time Job Navigation [Website]. Survey on the Status of Obtaining “the Permission of Night and Day Shift” by Medical Institutions! How Do You Check Which Hospitals Have Acquired the Permit and What Should What Do You Need to Be Aware of? 2023. [(accessed on 10 August 2024)]. Available online: https://arbeit.doctor-navi.jp/blog/20230316/11552/ (In Japanese)
- 26.Ishikawa M. Should the time physicians spend for self-directed learning be considered as working hours?: A nationwide opinion survey of physicians working for obstetric and gynecology clinics. J. Jpn. Assoc. Health Care Admin. 2024;15:5–13. (In Japanese) [Google Scholar]
- 27.Ministry of Health, Labor and Welfare For Proper Labor Management After Obtaining the Permission of Night and Day Shift. [(accessed on 10 August 2024)];2023 Available online: https://www.mhlw.go.jp/content/001237735.pdf. (In Japanese)
- 28.Eckleberry-Hunt J., Lick D. Physician depression and suicide: A shared responsibility. Teach. Learn. Med. 2015;27:341–345. doi: 10.1080/10401334.2015.1044751. [DOI] [PubMed] [Google Scholar]
- 29.Bettes B.A., Chalas E., Coleman V.H., Schulkin J. Heavier workload, less personal control: Impact of delivery on obstetrician/gynecologists’ career satisfaction. Am. J. Obstet. Gynecol. 2004;190:851–857. doi: 10.1016/j.ajog.2003.10.695. [DOI] [PubMed] [Google Scholar]
- 30.Menon N.K., Shanafelt T.D., Sinsky C.A., Linzer M., Carlasare L., Brady K.J.S., Stillman M.J., Trockel M.T. Association of Physician Burnout With Suicidal Ideation and Medical Errors. JAMA Netw. Open. 2020;3:e2028780. doi: 10.1001/jamanetworkopen.2020.28780. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Some data are unavailable due to ethical restrictions.