Abstract
Background
Both coronavirus disease-2019 (COVID-19) and cancer place a heavy burden on the society and mental health of patients. Spiritual health may play a prominent role in coping with stressful conditions. Considering the existing controversy regarding the correlation between spiritual health and stress related to the COVID-19 pandemic in cancer patients, this study aimed to assess the correlation between spiritual health and COVID-19 stress in cancer patients.
Methods
This cross-sectional study was conducted on cancer patients presenting to Rasoul and Firouzgar Hospitals, affiliated with Iran University of Medical Sciences, in 2022. After obtaining written informed consent, eligible patients filled out the spiritual health questionnaire and COVID Stress Scale (CSS). Data were analyzed by the Pearson and Spearman correlation coefficients and one-way ANOVA.
Results
The mean (SD) levels of COVID-19 stress and spiritual health were equal to 106.5 (44.5) and 26.2 (10.9), respectively, which are regarded as moderate levels. An inverse correlation of -0.48 was found between spiritual health and COVID-19 stress (P < 0.001). Spiritual health decreased by an increase in the stage of cancer (P < 0.001). The mean COVID-19 total stress score and its domain scores [except for the post-traumatic stress syndrome (PTSD) domain] were significantly higher in patients with poor spiritual health compared with those with good spiritual health. However, the difference in this regard was not significant between patients with poor and moderate spiritual health (P > 0.05).
Conclusion
This study confirmed the prominent role of spiritual health in the reduction of COVID-19 stress. Promotion of spiritual health in cancer patients should be considered as an inseparable part of patient care to prevent disease aggravation and decrease the stress level of cancer patients, particularly during the COVID-19 pandemic.
Keywords: Cancer, COVID-19, Health, Pandemics
↑What is “already known” in this topic:
Spiritual health may play an important role in coping with stressful conditions caused by diseases. Therefore, depression, hopelessness, and aggression have been more commonly reported in cancer patients.
→What this article adds:
An inverse correlation was found between spiritual health and COVID-19 stress. Spiritual health promotion should be considered for cancer patients as an inseparable part of their care to combat the disease, especially during the COVID-19 pandemic.
Introduction
Coronavirus disease-2019 (COVID-19) affected almost all important economic, political, social, and military aspects of different countries worldwide (1, 2). Considering the pathogenesis, speed of transmission, and the percentage of morbidity and mortality caused by severe acute respiratory syndrome coronavirus 2, it can compromise the mental health of people at different socioeconomic levels (3, 4). It can not only cause public health concerns but can also lead to the development of some psychological disorders such as anxiety, fear, depression, avoidance behaviors, irritability, sleep disorders, and post-traumatic stress disorder (PTSD) (5, 6).
In recent decades, despite the achievements in the prevention and control of communicable diseases, the incidence and prevalence of non-communicable diseases have significantly increased (7). Cancer is the second most common cause of morbidity and mortality after cardiovascular diseases in most countries (8-11). Affliction with cancer affects all aspects of patients’ life and their families (12, 13). In the past, the burden of cancer was greater in developed countries. However, this pattern has changed, and currently, 56% of new cancer cases and related deaths occur in developing countries (14). In Iran, cancer is the third most common cause of death after cardiovascular diseases and accidents (15).
A number of factors, such as long-term stress, can play a role in the development of leukemia (16-18). On the other hand, cancer patients are at higher risk of COVID-19 than other individuals since they are under chemotherapy and receive immunosuppressive drugs (19). Since the correlation between PTSD and cancer has been mentioned in some studies (20, 21), such patients may require psychological interventions and screening for such disorders (22). It has been reported that young female patients with lymphoma are more likely to develop depression and PTSD when afflicted with COVID-19 (23). Also, immunosuppression associated with COVID-19 can make the patients susceptible to PTSD (24). Furthermore, stress is a known factor that can cause psychiatric disorders in cancer patients and adversely affect their quality of life (25-27). The COVID-19 pandemic can also cause psychiatric disorders in patients. However, COVID-19 peaks can cause postponement of some procedures. COVID-19 related stress is among such disorders which can adversely affect the emotional and psychological function of cancer patients (28-30). COVID-19 can affect different aspects of patients’ life. Also, due to the novelty of SARS-CoV-2, its management is highly challenging for oncologists since it can delay the treatment course of cancer patients, and this delay can adversely affect the emotional and psychological health and well-being of patients (31, 32).
Spirituality is a unique phenomenon and is correlated with health, good feeling, and recovery(33). Spiritual health is a health domain that results in integrity of physical, mental, and social health (34). Many physicians believe that faith and spirituality are important parameters in the recovery of patients and consider it imperative to pay attention to them during the treatment course (35). Evidence shows that spiritual health may play an important role in coping with stressful conditions caused by diseases. On the other hand, depression, hopelessness, and sometimes a tendency to suicide have been more commonly reported in cancer patients (36- 41).
Controversy exists regarding the correlation of spiritual health with mental health and also COVID-19 stress in cancer patients. Considering the significant burden of the pandemic on different aspects of health and high stress levels in cancer patients, this study aimed to assess the correlation of spiritual health and COVID-19 pandemic stress in cancer patients to take a step forward to improve their quality of life.
Methods
This descriptive cross-sectional study was conducted on eligible cancer patients presenting to Firouzgar and Rasoul Hospitals affiliated with Iran University of Medical Sciences from April to December 2022. The inclusion criteria were signing informed consent forms, definite diagnosis of cancer, age over 18 years, and a minimum of 6 months had to be passed since the definite cancer diagnosis. The exclusion criteria were duration of disease < 6 months, cognitive disorders, history of malignancy, pregnancy ,age over 85 years, and incomplete patient records.
The participants were recruited through convenience sampling. The sample size was calculated using the G*Power software, considering the standard deviation of 9.1 reported by Amiri et al. (42), the significance level of 0.05, the power level of 0.8, and the effect size of 0.15.
Data were collected by using two standard questionnaires, namely the spiritual health questionnaire and the COVID Stress Scale (CSS). To consider the potential bias of attrition, as the participants were cancer patients, a trained interviewer was responsible for gathering the data and filling the questionnaires in person in the shortest time. The questions were asked of the patients themselves, and some variables were extracted from the medical records of patients. Also, some questions were answered by the attending physicians. The spiritual health of patients was evaluated by using the comprehensive spiritual health assessment scale for the Iranian population, which has 48 questions, including 28 cognitive/emotional and 20 behavioral questions. Moreover, Amiri et al. (42) confirmed the validity and reliability of this questionnaire in an Iranian urban population. The questions have 5-point Likert scale answer choices, and the total spiritual health score between 48-102 indicates poor, 103-167 indicates moderate, and 168-240 indicates good spiritual health (38).
The CSS has 36 items to assess stress reactions stemming from COVID-19 across sub-dimensions, including (I) danger and contamination(mysophobia), (II) socioeconomic consequences, (III) xenophobia, (IV) PTSD, and (V) compulsive checking. Items are rated on a 5-point Likert scale, scoring from 0 (never) to 4 (always/extremely). This scale was validated in an Iranian population of patients with obsessive-compulsive disorder (Khosravani et al., 2021). In the present study, Cronbach's alpha of the CSS was 0.95.
Statistical analysis
Data were analyzed using the Pearson and Spearman correlation coefficients, regression model, one-way ANOVA, and Tukey post-hoc test. The analyses were performed using the statistical software SPSS (ver. 22). The significance level was set at 0.05.
Results
Demographic and clinical variables of 300 patients, including 149 females (49.67%) and 151 males (50.33%) with a mean age of 50.21±15.92 years, were evaluated. The frequency of stage I, II, III, and IV was 2.7% (n=8), 17% (n=51), 47% (n=141), and 33.3% (n=100). The cancer types included Breast, Prostate, Lung, and Kidney cancers (percentages of 45.3, 39.2, 11.6, and 3.9, respectively).
The mean score of spiritual health was 106.45±44.5. The results indicated moderate spiritual health of patients. The mean COVID-19 stress score was 44.2±33.36. The mean scores were 9.72±1.74 for stress-related virus dangers, 6.48±1.49 for stress-related socioeconomic consequences, 8.82±2.06 for xenophobia, 10.93±2.36 for mysophobia, 4.91±1.10 for compulsive checking, and 7.74±1.26 for PTSD.
After controlling for the effect of other variables, spiritual health showed significant correlations with self-reported health and stage of cancer. Also, the behavior domain of spiritual health had significant correlations with self-reported health and stage of cancer. However, the correlation coefficient was negative for the correlation of spiritual health with the stage of cancer, indicating an inverse correlation (Table 1).
Table 1. Spearman correlation of spiritual health total score and its domain score with other variables.
| Variable | Spearman correlation coefficient (P value)* | |||
|---|---|---|---|---|
| Spiritual health | Ideology | Attitude | Behavior | |
| Age | 0.074 (0.594) | 0.921 (-0.013) | 0.705 (0.049) | 0.891 (-0.018) |
| Self-reported health | 0.021 (0.476) | 0.082 (0.180) | 0.156 (0.153) | 0.033 (0.373) |
| Stage of cancer | 0.038 (-0.289) | 0.098 (-0.161) | 0.103 (-0.166) | 0.042 (-0.240) |
*P values were calculated using the Spearman correlation coefficients.
COVID-19 stress score had significant inverse correlations with insurance coverage, self-reported health, and BMI, such that having health insurance, higher levels of self-reported health, and higher BMI were associated with significantly lower COVID-19 stress (Table 2). However, a higher stage of cancer was significantly correlated with a higher level of COVID-19 stress and a greater stress-related virus dangers domain score. The stress-related socioeconomic consequences domain score had a significant direct correlation with age and gender, such that the stress-related socioeconomic consequences domain score was higher in males and in older patients.
Table 2. Spearman correlation of xenophobia , mysophobia , compulsive checking , and PTSD with other variables.
| Variable | Spearman correlation coefficient (P value)* | |||
|---|---|---|---|---|
| Xenophobia | Mysophobia | Compulsive checking | PTSD | |
| Age | 0.562 (-0.069) | 0.971 (0.005) | 0.191 (0.181) | 0.645 (0.060) |
| Self-reported health | 0.004 (-0.286) | 0.208 (-0.135) | 0.001 (-0.399) | 0.021 (-0.241) |
| Stage of cancer | 0.179 (0.127) | 0.340 (0.097) | 0.385 (0.097 ) | 0.714 (0.036) |
*P values were calculated using the Spearman correlation coefficients.
Gender and xenophobia had a direct correlation, and males acquired a higher xenophobia score than females. Self-reported health and BMI had significant inverse correlations with xenophobia and compulsive checking. Also, self-reported health had a significant inverse correlation with PTSD (Table 3).
Table 3. Spearman correlation of COVID-19 stress score, stress-related virus dangers, and stress-related socioeconomic consequences domain scores with other variables.
| Variable | Spearman correlation coefficient (P value)* | ||
|---|---|---|---|
| Dangers | Related socioeconomic consequences | COVID-19 stress score | Related virus stress |
| Age | 0.204 (0.214) | 0.688 (0.064) | 0.048 (0.218) |
| Self-reported health | 0.008 (-0.385) | 0.146 (-0.189) | 0.003 (-0.278) |
| Stage of cancer | 0.049 (0.222) | 0.048 (0.223) | 0.501 (0.059 ) |
*P values were calculated using the Spearman correlation coefficients.
A significant inverse correlation was found between spiritual health and COVID-19 stress score and also stress-related socioeconomic consequences domain score, such that by an increase in spiritual health, the COVID-19 stress and stress-related its consequences decreased. The spiritual health ideology domain had significant inverse correlations with stress-related socioeconomicconsequences and mysophobia. COVID-19 stress and stress-related socioeconomic consequences had significant inverse correlations with the behavior domain of spiritual health (Table 4).
Table 4. Spearman correlation of spiritual health total and domain scores with COVID-19 stress and its domains.
| Variable | Spearman correlation coefficient (P value)* | |||
|---|---|---|---|---|
| Spiritual health | Ideology | Attitude | Behavior | |
| COVID-19 stress | 0.003 (-0.342) | 0.091 (-0.107) | 0.101 (-0.098) | 0.015 (-0.258) |
| Related virus dangers | 0.061 (-0.112) | 0.864 (-0.018) | 0.0984 (-0.010) | 0.055 (-0.103) |
| Stress related socioeconomic Consequences | 0.017 (-0.199) | 0.038 (-0.162) | 0.003 (-0.203) | 0.004 (-0.226) |
| Xenophobia | 0.761 (0.025) | 0.963 (-0.04) | 0.763 (-0.024) | 0.813 (-0.028) |
| Mysophobia | 0.989 (-0.007) | 0.037 (-0.168) | 0.784 (-0.02) | 0.689 (-0.011) |
| Compulsive checking | 0.258 ( 0.116) | 0.311 (0.107) | 0.334 (-0.090) | 0.329 (-0.093) |
| PTSD | 0.447 (0.064) | 0.302 (0.101) | 0.394 (0.066) | 0.674 (0.033) |
*P values were calculated using the Spearman correlation coefficients.
Inverse correlation between spiritual health and COVID-19 stress (Figure 1). Except for PTSD, the mean scores of other CSS domains were significantly different in patients with different spiritual health levels (Table 5).
Figure 1.
Scatter plot of spiritual health versus COVID-19 stress
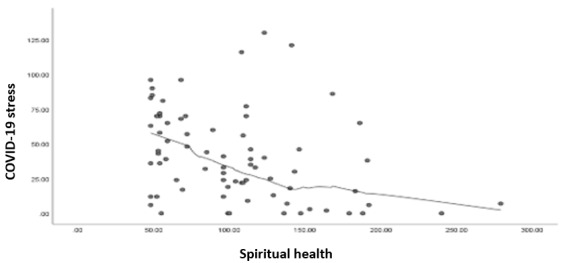
Table 5. Mean COVID-19 stress score according to the level of spiritual health.
| Variable | Spearman correlation coefficient (P value)* | |||
|---|---|---|---|---|
| Poor | Moderate | Good | *P value | |
| COVID-19 stress | 7.9±51.1 | 11.3±42.2 | 6.1±33.1 | 0.001> |
| Related virus dangers | 1.1±11.9 | 1.2±8.9 | 1.4±5.5 | 0.001> |
| Stress related socioecoNomic consequences | 1.2±8.6 | 1.0±7.6 | 1.6±4.7 | 0.017 |
| Xenophobia | 1.04±10.8 | 1.1±8.1 | 1.6±7.7 | 0.020 |
| Mysophobia | 1.3±13.7 | 1.1±9.6 | 1.3±8.9 | 0.031 |
| Compulsive checking | 1.7±7.4 | 1.1±5.7 | 1.5±4.3 | 0.041 |
| PTSD | 1.1±9.2 | 1.2±7.6 | 1.2±6.6 | 0.051 |
*P values were calculated using ANOVA*
The ANOVA assumptions, including Normal distribution and homoscedasticity, were assessed graphically and using statistical tests and no serious violation was detected. The mean COVID-19 stress total and domain scores, except for PTSD, were significantly different between patients with poor, moderate, and good spiritual health. Moreover, for all variables, Tukey post-hoc tests indicated significantly higher scores in patients with poor spiritual health compared with those with moderate spiritual health and in patients with moderate spiritual health compared with those with good spiritual health. Merely the difference in Xenophobia was not significant between patients with moderate and good spiritual health (P = 0.341).
Finally, considering the significant correlations between COVID-19 stress and the covariates including self-reported health, stage of cancer, and spiritual health in Table 3 and Table 4, a regression model was fitted on these covariates, taking COVID-19 stress as the response variable. The findings are presented in Table 6. Accordingly, adjusted for the stage of cancer and spiritual health, spiritual health had a borderline reverse association with COVID-19 stress.
Table 6. Linear regression model findings taking COVID-19 stress as the response variable.
| Variable | Unstandardized regression coefficient | |||
|---|---|---|---|---|
| Coefficient | 95% confidence | Interval | P value | |
| Spiritual health | -0.092 | -0.184 | 0.001 | 0.047 |
| Self-reported health | 1.037 | -0.338 | 2.412 | 0.139 |
|
Stage of cancer;
1 |
-12.906 | -37.899 | -37.899 | -0.310 |
| 2 | -7.631 | -31.615 | 16.353 | 0.532 |
| 3 | -7.716 | -31.907 | 16.47 | 0.531 |
Discussion
The COVID-19 pandemic caused several economic problems, posed a general and public health threat, and imposed severe restrictions on the social life of people. Diagnosis, treatment, and follow-up of cancer patients are usually associated with increased levels of psychological stress. Thus, affliction with both COVID-19 and cancer would pose a heavy psychological burden on patients (37). Therefore, psychosocial support is imperative for cancer patients to maintain their quality of life and mental health (39).
Dehghan et al. (3) reported that 61% of patients with moderate to advanced stages of cancer were anxious about COVID-19, and 26% believed that the COVID-19 pandemic affected their treatment course. In the Kim et al. study, (4) cancer patients reported experiencing depression, anxiety, and behavioral disorders during the COVID-19 pandemic. Vicinanza (5) and Grajek et al. (6) confirmed the anxiety of cancer patients under radiotherapy during the COVID-19 pandemic. The side effects of cancer treatment can cause psychosocial disorders (37). Concerns regarding COVID-19 are associated with anxiety and depression (7), and are among the reasons for treatment postponement (8, 9). Several studies have evaluated the correlation between stress and spiritual health. However, the present study was the first to assess the correlation between spiritual health and COVID-19 stress in cancer patients and revealed that cancer patients in the present study had moderate to high spiritual health, which is probably due to the cultural and religious conditions of the study population.
Our result was in line with Li (15) and Amirmohamadi et al. studies (10). Nonetheless, Kavak et al. (11) reported that patients with advanced stomach cancer had a high level of spiritual well-being. Variations in the results can be attributed to different study designs and the type and stage of cancer.
Khiyali et al. (38) found no significant correlation between age, marital status, and level of education with spiritual health, which was in agreement with us and other investigations (12, 13). Another study reported no significant correlation between spiritual health with age, gender, race, stage of cancer, metastasis, insurance coverage, and marital status (14); whereas another study indicated the effect of demographic factors and clinical data on the spiritual health of advanced cancer patients had higher spiritual health (39). In line with their results, the present study showed a significant correlation between the stage of cancer and spiritual health. Consistent with the present results, Khiyali et al. (38) reported a moderate level of COVID-19 stress in cancer patients. However, the stress level of males and those with a negative history of COVID-19 was significantly higher than others while age and gender had no significant correlation with stress level in this study.
The correlation between spiritual health and mental health has been reported in different populations. Dehghan et al. (40) demonstrated that COVID-19 stress was common in hemodialysis patients, and spiritual health may effectively decrease their COVID-19 stress (40). Another study conducted revealed that mental health was influenced by spiritual well-being, and the promotion of spiritual health increased self-esteem and decreased the level of stress and anxiety. According to Zhai et al. study (41), life experiences can empower individuals to expand their personal strategies for better coping with stress and promotion of their mental health. Thus, attention to spiritual needs is imperative for a patient-oriented intervention. Addressing the psychosocial and spiritual needs of patients can improve their quality of life (18).
Findings of Esmaeili et al. study (19) consistent with our results, demonstrated that improved resilience and higher spiritual health can decrease psychological susceptibility. This study was conducted on cancer patients who are already susceptible to higher levels of stress and anxiety, irrespective of the COVID-19 pandemic; nonetheless, the role of the COVID-19 pandemic in generating higher levels of stress in patients is undeniable. Farahati et al. (20) statements were in agreement with the results of Shi (21) and Wen et al. (22) who showed that the COVID-19 pandemic caused significant psychological problems in different populations.
Moradijou (23) and Yousefi et al. (24) confirmed our results regarding the significant correlation between spiritual health and stress. Thus, spiritual health can aid in promoting mental health by offering a framework for the interpretation and description of life experiences and creating a sense of existential coherence (25). Spirituality supports human and divine aspects of life and leads to positive thinking and motivation. It also improves the personal ability to accept and endure pain and suffering and cope with stresses and problems (26).
In line with the present results, Khiyali et al. (38) showed that the promotion of spiritual well-being and resilience in cancer patients under chemotherapy should be an inseparable part of their care because these qualities are valuable sources to combat cancer and decrease the stress and anxiety of patients especially during the COVID-19 pandemic.
The present findings revealed a significant inverse correlation between spiritual health and COVID-19 stress in chemotherapy patients. Mihic-Gongora (27) and Turke et al. (28) pointed to the significant inverse correlation of stress with spirituality and added that spirituality in cancer patients decreases their level of stress and anxiety during periods of social seclusion and helps the patients to comply with cancer treatment during the COVID-19 pandemic. Moeini et al. (29) found that a spiritual care program can decrease the anxiety and stress levels of leukemia patients. Thus, for hard-to-cure diseases, nurses are recommended to use comprehensive care programs with special emphasis on spiritual care.
As the main strength, our research was the first study to address the correlation of spiritual health with COVID-19 stress in cancer patients. These findings can help health policymakers in strategy planning to improve the spiritual health and resilience of patients as effective mechanisms to combat cancer. Additionally, the limitations of this study include sample size, data collection and cross-sectional design. The convenience sampling which was applied due to complexities in random recruiting of participants, narrows the generalizability of the finding to the target population. Future studies are recommended to use other methods of data collection with interventional study designs.
Conclusion
The COVID-19 stress and spiritual health levels of cancer patients were moderate in this study. An inverse correlation was found between spiritual health and COVID-19 stress. These results highlighted the prominent role of spiritual health in the reduction of COVID-19 stress. Spiritual health promotion should be considered for cancer patients as their care is a valuable quality to combat the disease and decrease stress, especially during the COVID-19 pandemic.
Ethical Considerations
This study was approved by the research ethics committee of Iran University of Medical Sciences (IR.IUMS.FMD.REC.1400.447).
Conflict of Interests
The authors declare that they have no competing interests.
Acknowledgment
The authors would like to thank the Oncology Department of Firoozgar Hospital, Iran University of Medical Sciences.
Authors’ Contributions
All authors have contributed equally to developing the concept, implementation, processing of results, and writing the article. We declare that this material has not been published before and is not under consideration by other publishers.
Cite this article as : Anoushirvani AA, Tabaeian SP, Maarefi M, Basir Shabestari S. Correlation of Spiritual Health and Stress Related to the COVID-19 Pandemic in Cancer Patients. Med J Islam Repub Iran. 2024 (24 Jul);38:85. https://doi.org/10.47176/mjiri.38.85
References
- 1.Chen W, Lv X, Xu X, Gao X, Wang B. Meta-analysis for psychological impact of breast reconstruction in patients with breast cancer. Breast Cancer. 2018;25(4):464–469. doi: 10.1007/s12282-018-0846-8. [DOI] [PubMed] [Google Scholar]
- 2.Bargon CA, Batenburg MCT, van Stam, Mink van, van Dam, van der. et al. Impact of the COVID-19 Pandemic on Patient-Reported Outcomes of Breast Cancer Patients and Survivors. JNCI Cancer Spectr. 2021;5(1):pkaa104. doi: 10.1093/jncics/pkaa104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dehghan M, Namjoo Z, Zarei A, Tajedini H, Bahrami A, Zakeri MA. The relationship between coronavirus anxiety, mindfulness and spiritual health in patients with cancer: a survey in Southeast Iran. Psychiatry Investig. 2021;18(5):443–452. doi: 10.30773/pi.2020.0441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim K, Kim H, Lee J, Cho IK, Ahn MH, Son KY. et al. Functional impairments in the mental health, depression and anxiety related to the viral epidemic, and disruption in healthcare service utilization among cancer patients in the COVID-19 pandemic era. Cancer Res Treat. 2022;54(3):671–679. doi: 10.4143/crt.2021.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vicinanza F, Ippolito E, Sisto A, Santo B, Fiore M, Trodella LE. et al. The psychological impact of the covid-19 pan-demic on radiotherapy cancer patients. Transl Oncol. 2022;22:101457. doi: 10.1016/j.tranon.2022.101457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grajek M, Krupa-Kotara K, Rozmiarek M, Sobczyk K, Działach E, Górski M. et al. The level of COVID-19 anxiety among oncology patients in Poland. Int J Environ Res Public Health. 2022;19(18):11418. doi: 10.3390/ijerph191811418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murata S, Rezeppa T, Thoma B, Marengo L, Krancevich K, Chiyka E. et al. The psychiatric sequelae of the COVID‐19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021;38(2):233. doi: 10.1002/da.23120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Albano D, Feraca M, Nemesure B. An assessment of distress levels of patients undergoing lung cancer treatment and surveillance during the COVID-19 pandemic. J Nurse Pract. 2021;17(4):489. doi: 10.1016/j.nurpra.2020.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sigorski D, Sobczuk P, Osmola M, Kuć K, Walerzak A, Wilk M. et al. Impact of COVID-19 on anxiety levels among patients with cancer actively treated with systemic therapy. ESMO Open. 2020;5(5):e000970. doi: 10.1136/esmoopen-2020-000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amirmohamadi M, Borhani F, Kiani M. et al. The correlation between spiritual wellbeing and depression in elderly patients with cancer in Iran. Middle East J. 2017;7(10):9. [Google Scholar]
- 11.Kavak F, Özdemir A, Dural G. The Relation between spiritual wellbeing and psychological resilience among patients diagnosed with advanced gastrointestinal cancer. Current Psychol. 2021;40(4):1788. [Google Scholar]
- 12.Martins H, Dias Domingues, Caldeira S. Spiritual well-being in cancer patients undergoing chemotherapy in an outpatient setting: a cross-sectional study. J Holist Nurs. 2020;38(1):68–77. doi: 10.1177/0898010119858269. [DOI] [PubMed] [Google Scholar]
- 13.Mendonça AB, Pereira ER, Magnago C, da Silva, Morett Leão, Costa Rosa. et al. Distress and Spiritual Well-Being in Brazilian Patients Initiating Chemotherapy during the COVID-19 Pandemic—A Cross-Sectional Study. Int J Environ Res Public Health. 2021;18(24):13200. doi: 10.3390/ijerph182413200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rabow MW, Knish S. Spiritual well-being among outpatients with cancer receiving concurrent oncologic and palliative care. Support Care Cancer. 2015;23(4):919. doi: 10.1007/s00520-014-2428-4. [DOI] [PubMed] [Google Scholar]
- 15.Li CC, Rew L, Hwang SL. The relationship between spiritual well-being and psychosocial adjustment in Taiwanese patients with colorectal cancer and a colostomy. J Wound Ostomy Continence Nurs. 2012;39(2):161. doi: 10.1097/WON.0b013e318244afe0. [DOI] [PubMed] [Google Scholar]
- 16.Caldeira S, Timmins F, de Carvalho, Vieira M. Clinical Validation of the Nursing Diagnosis Spiritual Distress in Cancer Patients Undergoing Chemotherapy. Int J Nurs Know. 2017;28(1):44–52. doi: 10.1111/2047-3095.12105. [DOI] [PubMed] [Google Scholar]
- 17.Timmins F, Caldeira S. Assessing the spiritual needs of patients. Nurs Stand. 2017;31(29):47–53. doi: 10.7748/ns.2017.e10312. [DOI] [PubMed] [Google Scholar]
- 18.Morocutti P. Positive correlations between spirituality and health: results from some surveys. Medicina E Morale. 2019;68(1):41–54. [Google Scholar]
- 19.Esmaeili Darmian, Javadi SV. Study the role of spiritual health and resilience in pandemic COVID- 19 on psychological vulnerability. J Fundament Mental Health. 2022;24(5):349. [Google Scholar]
- 20.Farahati M. Psychological consequences of the coronavirus outbreak in the community. J Social Impact Asses. 2020;1(2):207. [Google Scholar]
- 21.Shi YR, Rong DG, Ye LC. Fear can be more harmful than the severe acute respiratory syndrome coronavirus 2 in controlling the corona virus disease 2019 epidemic. World J Clin Cases. 2020;8(4):52–70. doi: 10.12998/wjcc.v8.i4.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L. et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16(10):1732. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noroozi M, Mohebbi-Dehnavi Z. Investigating the relationship between religious orientation and spiritual intelligence with general health dimensions in women with breast cancer. J Educ Health Promot. 2023;12:40. doi: 10.4103/jehp.jehp_1744_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yousefi F, Rafiei S, Tayeri F. Investigating the spiritual health and its relationship with the mental health of new students of Kurdistan University of Medical Sciences. Shenakht Journal of Psychology and Psychiatry. 2019;6(4):100. [Google Scholar]
- 25.Wind TR, Rijkeboer M, Andersson G, Riper H. The COVID-19 pandemic: The ‘black swan’for mental health care and a turning point for e-health. Internet Interv. 2020;20:100317. doi: 10.1016/j.invent.2020.100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jafari A, Hajiloo N, Faghani R, Khazan K. The relationship between spiritual well-being and psychological hardiness with mental health of the elderly. Behav Sci Res. 2012;10(6):431. [Google Scholar]
- 27.Mihic-Gongora L, Jiménez-Fonseca P, Hernandez R, Gil-Raga M, Pacheco-Barcia V, Manzano-Fernández A. et al. Psychological distress and resilience in patients with advanced cancer during the Covid-19 pandemic: the mediating role of spirituality. BMC Palliat Care. 2022;21(1):146. doi: 10.1186/s12904-022-01034-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turke KC, Canonaco JS, Artioli T, Lima MSS, Batlle AR, Oliveira FCP. et al. Depression, anxiety and spirituality in oncology patients. Rev Assoc Med Bras. 2020;66(7):960. doi: 10.1590/1806-9282.66.7.960. [DOI] [PubMed] [Google Scholar]
- 29.Moeini M, Taleghani F, Mehrabi T, Musarezaie A. Effect of a spiritual care program on levels of anxiety in patients with leukemia. Iran J Nurs Midwifery Res. 2014;19(1):88–93. [PMC free article] [PubMed] [Google Scholar]
- 30.Alipour A, Ghadami A, Alipour Z, Abdollahzadeh H. Preliminary validation of the Corona Disease Anxiety Scale (CDAS) in the Iranian sample. Quart J Health Psychol. 2020;8:163. [Google Scholar]
- 31.Frey MK, Ellis AE, Zeligs K, Chapman-Davis E, Thomas C, Christos PJ. et al. Impact of the coronavirus disease 2019 pandemic on the quality of life for women with ovarian cancer. Am J Obstet Gynecol. 2020;223(5):725.e1–725.e9. doi: 10.1016/j.ajog.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roman NV, Mthembu TG, Hoosein M. Spiritual care–‘A deeper immunity’–A response to Covid-19 pandemic. Afr J Prim Health Care Fam Med. 2020;12(1):2456. doi: 10.4102/phcfm.v12i1.2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mazaheri M, Fallahi Khoshknab, MaddahSB, Rahgozar M. Nursing attitude to spirituality and spiritual care. Health Monitor J Iran Inst Health Sci Res. 2009;8(1):31. [Google Scholar]
- 34.Akbari M, Hossaini SM. The relationship of spiritual health with quality of life, mental health, and burnout: The mediating role of emotional regulation. Iran J Psych. 2018;13(1):31. [PMC free article] [PubMed] [Google Scholar]
- 35.Rezaei M, Seyedfatemi N, Hosseini F. Spiritual Well-being in Cancer Patients who Undergo Chemotherapy. Journal of Hayat. 2009;14(4 and 3):33–39. [Google Scholar]
- 36.Bekelman DB, Dy SM, Becker DM, Wittstein IS, Hendricks DE, Yamashita TE. et al. Spiritual well-being and depression in patients with heart failure. J Gen Intern Med. 2007;22(4):470. doi: 10.1007/s11606-006-0044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moraes Filho, Khoury HT. Uso do coping religioso/espiritual diante das toxicidades da quimioterapia no paciente oncológico. Rev Bras Cancerol. 2018;64(1):27–33. [Google Scholar]
- 38.Khiyali Z, Naderi Z, Vakil M, Ghasemi H, Dehghan A, Bijani M. A study of COVID anxiety, spiritual well-being and resilience levels in patients with cancer undergoing chemotherapy during the COVID-19 pandemic: a cross-sectional study in the south of Iran. BMC Psychology. 2023;11:75. doi: 10.1186/s40359-023-01126-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sun XH, Liu X, Zhang B, Wang YM, Fan L. Impact of spiritual care on the spiritual and mental health and quality of life of patients with advanced cancer. World J Psychiatry. 2021;11(8):449–462. doi: 10.5498/wjp.v11.i8.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dehghan M, Namjoo Z, Mohammadi Akbarabadi, Fooladi Z, Zakeri MA. The relationship between anxiety, stress, spiritual health, and mindfulness among patients undergoing hemodialysis: A survey during the COVID‐19 outbreak in Southeast Iran. Health Sci Rep. 2021;4(4):e461. doi: 10.1002/hsr2.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhai Y, Du X. Loss and grief amidst COVID-19: A path to adaptation and resilience. Brain Behav Immun. 2020;87:80. doi: 10.1016/j.bbi.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amiri P, Abbasi M, Garibzadeh S, Asghari Jafarabadi, Hamzavi Zarghani, Azizi F. Designation and psychometric assessment of a comprehensive spiritual health questionnaire for Iranian populations. Medical Ethics Journal. 2015;9(30):25–56. [Google Scholar]


